Abstract
Purpose
Although several trials have confirmed the treatment efficacy of induction chemotherapy followed by concurrent chemoradiotherapy (CCRT) in locoregionally advanced nasopharyngeal carcinoma (NPC) from endemic area of China, little is known about the best regime for induction chemotherapy in non-endemic region. This study compared the treatment effect of Gemcitabine and cisplatin (GP) versus docetaxel and cisplatin (TP) followed by concurrent chemoradiotherapy in locoregionally advanced NPC from non-endemic area of China.
Materials and methods
A total of 196 locoregionally advanced NPC patients were enrolled in this study, with 142 and 54 patients in TP and GP followed by concurrent chemoradiotherapy groups. The primary endpoint was treatment response of induction chemotherapy. The secondary endpoints included disease-free survival. The Kaplan–Meier method was used to evaluate the efficacy between treatment groups.
Results
The median follow-up time was 45.5 months (range: 6–60.5 months). During induction chemotherapy course, GP contributed higher treatment response rate than TP (68.1% vs. 47.1%, p = 0.007). Patients in GP group had better DFS and LRFS than those in TP group (3-year and 5-year DFS, 86.8% and 82.5% vs. 71.7% and 68%, p = 0.036; 3-year and 5-year LRFS, 96.2% and 96.2% vs. 90.5% and 82.8%, p = 0.03). No significant difference of adverse events was observed between two treatment groups in the whole course.
Conclusion
This study suggested that GP followed by CCRT was better than TP followed by CCRT in improving survival outcomes of locoregionally advanced NPC patients from non-endemic area of China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
About 70% of newly diagnosed nasopharyngeal carcinoma (NPC) patients have locoregionally advanced diseases. (Pan et al. 2016). Radiotherapy combined with chemotherapy has been suggested as recommended treatment model for locoregionally advanced nasopharyngeal carcinoma (LA-NPC) by National Comprehensive Cancer Network (NCCN). However, which combination “cocktail” is the best remains controversial. Since a phase III trial reported the effects of docetaxel, cisplatin and fluorouracil (TPF) induction chemotherapy (IC) plus concurrent radiotherapy (CCRT) was superior to CCRT in LA-NPC, the evidence level of IC + CCRT was elevated from category 3 to category 2A (Sun et al. 2016). Recently, another phase III trial confirms that gemcitabine and cisplatin induction chemotherapy followed by CCRT is a high-effective and low-toxicity regimen for LA-NPC (Zhang et al. 2019). This would be very helpful to further enhance the position of IC + CCRT in treatment selections of LA-NPC.
Docetaxel and cisplatin (TP) induction chemotherapy is also considered as an effective regimen for NPC. Compared with fluorouracil and cisplatin (PF) regimen, several studies indicate that the TP regimen is safer and more effective (Chen et al. 2014; He et al. 2019; Mi et al. 2017). A randomized phase II study reports that neoadjuvant TP followed by CCRT has a trend to improve survival outcomes in LA-NPC when compared with CCRT (Hui et al. 2009). Although it is still unclear which is the better regimen between TP and TPF as induction chemotherapy for LA-NPC, a meta-analysis implies that TP is not inferior to TPF (He et al. 2019). In clinic, physicians may prefer to use TP as induction chemotherapy because it has minor side effects and shorter hospital stays than TPF. At present, with the application of GP followed by CCRT for LA-NPC, the question is whether TP as induction chemotherapy has similar treatment effect with GP in LA-NPC.
In China, the highest incidence of NPC occurs in Southern China; whereas in Northwest China, the incidence is lower. Our previous studies reported the NPC from Northwest China had higher rate of non-keratinizing differentiated subtype (approximate 30%) than endemic NPC (< 5%), and this histological type was a worse prognostic factor for patients survival (Zang et al. 2016, 2018). In view of the potential distinctive pathogenesis and geographical variations for NPC from Northwest China, this study aims to analyze the treatment effects of TP versus GP as induction chemotherapy followed by concurrent chemoradiotherapy in LA-NPC from this area.
Materials and methods
Patients
We retrospectively reviewed patients with NPC at the XiJing Hospital of Forth Military Medical University between January 2006 and December 2015. Selection criteria included: histologically confirmed newly diagnostic nasopharyngeal squamous cell carcinoma; age 18–70 years; stages III–IV without distant metastasis according to the American Joint Committee for Cancer Staging (AJCC) system; Eastern Cooperation Oncology Group (ECOG) performance status ≤ 2; received with TP or GP as induction chemotherapy, followed by cisplatin concurrent with radiotherapy; treated with intensity-modulated radiotherapy (IMRT); patients’ primary residences limited to the Northwest China, which is a typically non-endemic area for NPC. The exclusion criteria included: non-squamous cell carcinoma; AJCC staging T3N0–1; long-term resident history in endemic area; received other regimen as initial treatment except for IC followed by CCRT.
All patients had complete history, physical examination, blood work and imageological examinations of whole body including chest images, abdominal sonography, and whole-body bone scan. Patients were re-staged according to the 8th edition of AJCC system. The precise staging of all patients depended on the magnetic resonance imaging (MRI) of head and neck. The protocol was approved by the appropriate ethical review boards, and the study was conducted in accordance with the principles of the Declaration of Helsinki.
Radiation therapy and chemotherapy
All patients were immobilized in the supine position with head, neck, and shoulder thermoplastic mask. A contrasting CT image was obtained from the simulator for treatment planning. All patients were scanned with serial 3-mm slices from vertex to 5 cm below clavicles. The treatment planning approaches were described by previous studies (Wang et al. 2012; Zhao et al. 2012). The definitions of target delineating were as follows: gross tumor volume (GTV) included nasopharyngeal GTV (GTVnx) and lymph node GTV (GTVnd); high-risk clinical tumor volume (CTVnx) included 5-mm margin of GTVnx, encompassed the entire nasopharyngeal mucosa. CTV1 included the area of high-risk tumor invasion around nasopharyngeal and lymphatic levels of neck. CTV2 covered the low risk of lymphatic levels of neck. Planning target volume (PTV) was created on the basis of CTVs with 3-mm margin. The prescribed radiation doses were defined as follows: a total of 72.6 Gy in 33 fractions at 2.2 Gy per fraction to the PTV of GTVnx, 66–72.6 Gy to metastatic lymph nodes, 64–66 Gy to PTV of CTVnx, 55–60 Gy to PTV of CTV1, and 50 Gy to PTV of CTV2. All patients were treated with 1 fraction daily for 5 days per week. The doses received by each organ at risk (OAR) should be no more than its tolerance (Lee et al. 2009).
In the induction chemotherapy course, all patients received either TP regimen, which consisted of docetaxel (75 mg/m2, day 1) plus cisplatin (75 mg/m2, day 1) or GP regimen, which consisted of gemcitabine (1000 mg/m2, day 1 and day 8) plus cisplatin (75 mg/m2, day 1) every 3 weeks for 2–3 cycles. Radiotherapy began at 3 weeks after the last cycle of induction chemotherapy. Single-drug cisplatin (100 mg/m2) was administrated concurrent with radiotherapy every three weeks. Each chemotherapy cycles interval was 21 days.
Follow-up and evaluation
The follow-up time was calculated from the end of treatment to the last follow-up or death. Patients were regularly evaluated every 3 months during the first two years, every 6 months in the third–fifth years, and then once every year thereafter. Tumor response was assessed using the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0. Treatment-related toxicities were classified according to the National Cancer Institute Common Toxicity Criteria version 3.0. Primary tumor volume was contoured on the planning system according to MRI by a radiation oncologist, and then verified by another radiation oncologist.
Statistical analysis
The primary endpoint of this study was disease-free survival (DFS). The secondary endpoints included overall survival (OS), locoregional recurrence-free survival (LRRFS), distant metastasis-free survival (DMFS), treatment response, variation of tumor volume and treatment-related toxicities. DFS was measured from the end of treatment to the date of disease progression or death from any causes; OS was defined as the time from end of treatment to death; LRRFS, was defined as the time from end of treatment to first local or lymph node regional relapse; DMFS, was defined as the time from end of treatment to first detection of distant metastasis. The Kaplan–Meier method was used to estimate the endpoints, survival curves were compared using the log-rank test. Differences in proportions between groups were assessed using x2 test. The variation of tumor volume were compared by means of Student’s t test. Numerical variable was transformed to categorical variable using median as cut-off if it was not Gaussian distribution, such as tumor volume. Cox proportional hazard model was used to identify potentially independent prognostic factors, and the proportional-hazards assumption was tested with Schoenfeld residuals. The hazard ratio (HR) and its 95% confidence interval (95% CI) were used to indicate the prognostic value of risk factors. We further performed interaction analysis to explore the variation of treatment effect in subgroups, including sex, age, drinking, smoking, histological type, T stage, N stage, clinical staging, primary GTV and primary GTVnd. A two-sided p value of less than 0.05 was considered significant.
Results
Patient characteristics
Patient characteristics are presented in Table 1. The median follow-up time was 60.5 months (range: 6–94 months). A total of 98 of the 155 (63.2%) alive patients were followed for more than 5 years, including 61 (62.2%) in the TP group and 37 (37.8%) in the GP group. The median age of all patients was 47 years (range: 18–69 years). Of all patients included in this study, 58 (29.6%) were female and 138 (70.4%) were male; 82 (41.8%) had history of smoking and 54 (27.6%) had history of drinking; 51 (26%) had WHO histological type II and 145 (74%) had WHO histological type III; 82 (41.8%) had clinical stage III and 114 (58.2%) had clinical stage IV; 54 (27.6%) received GP plus CCRT and 142 (72.4%) received TP plus CCRT. 76 (39.6%) patients data were extracted from our previously terminated clinical trial which randomly assigned patients to receive GP plus CCRT and TP plus CCRT (NCT 01596868). The data of 16 patients received GP plus CCRT were from a recently published trial that randomly assigned patients to receive GP plus CCRT and CCRT (Zhang et al. 2019). Statistical analyses failed to detect any bias of baseline demographic and clinical characteristics between two treatment groups (Table 1).
Treatment responses during induction chemotherapy course
Overall, a total of 104 of 196 patients (53%) had treatment responses in the induction chemotherapy course. The proportion of treatment response was higher in GP group (68.6%) than TP group (47.1%). Patients who received TP had more stable disease after induction chemotherapy (49.3%) (Table 2). Patients who received GP induction chemotherapy experienced higher proportion of more than 30% of decreasing primary tumor volume than those who received TP induction chemotherapy (22.2% vs.7.7%, p = 0.005). However, no significant differences were detected in proportion of more than 50% of decreasing primary tumor volume between two chemotherapy regimens. Moreover, we failed to detect significant differences in proportion of decreasing lymph node volume between two groups (Table 2).
Survival outcomes
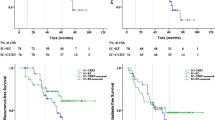
During follow-up period, there were total of 53 events of locoregional recurrence, distant metastasis or deaths (27%), including events in 9 of 54 patients (16.7%) in GP plus CCRT group and in 44 of 142 (31%) in the TP plus CCRT group. The 3-year and 5-year DFS were 86.8% and 84.8% in GP plus CCRT group compared with 71.7% and 68% in TP plus CCRT group (HR, 0.47; 95%CI 0.26–0.85; p = 0.036). Patients receiving GP plus CCRT had a trend in improving 3-year and 5-year OS compared to those receiving TP plus CCRT, but without statistically significant differences (90.6% and 86.7% vs. 83.7% and 74.8%; HR, 0.52; 95%CI 0.26–1.03; p = 0.13). Patients in GP plus CCRT group had significantly better local regional control than those in TP plus CCRT group (3-year and 5-year LRFS, 96.2% and 96.2% vs. 90.5% and 82.8%; HR, 0.23; 95% CI 0.09–0.58; p = 0.03). For DMFS, GP followed by CCRT had a trend to decrease the incidence of distant metastasis, but no statistically significant differences was detected between two groups. The 3-year and 5-year DMFS were 88.7% and 86.7% in GP group versus 77.8% and 77.8% in TP group (HR, 0.55; 95%CI 0.27–1.11; p = 0.12), respectively (Fig. 1).
In subgroup analysis of DFS, GP followed by CCRT contributed better DFS than TP followed by CCRT in patients with specific factors, included male (HR, 0.43; 95%CI 0.19–0.98), histological WHO type III (HR, 0.37; 95%CI 0.24–0.96), T3-4 (HR, 0.27; 95%CI 0.1–0.77), non-smoking history (HR, 0.3; 95%CI 0.26–0.99), AJCC stage IV (HR, 0.38; 95%CI 0.18–0.8) and primary GTVnx > 36.5 cc (HR, 0.15; 95%CI 0.05–0.5). Although no statistically significant differences were detected by subgroups analysis, GP followed by CCRT had a trend to improve DFS in patients with other factors, such as age ≤ 45 (HR, 0.32; 95%CI 0.09–1.07), N2-3 (HR, 0.5; 95%CI 0.24–1.02) and primary GTVnd > 37 cc (HR, 0.36; 95%CI 0.13–1.03) (Fig. 2). In general, the results of subgroup analysis for OS were similar with the results for DFS. GP plus CCRT had a trend to improve OS when compared with TP plus CCRT, except for female, T1–2, AJCC stage III and primary GTV ≤ 36.5 cc (Figure S1). Details regarding subgroup analyses of LRFS and DMFS are provided in figure S2–3 in the supplementary appendix.
Adverse effects
During the whole treatment course, 103 of 196 patients (52.5%) experienced grade 3 or 4 adverse effects. The most common events were nausea (in 59 of 196 patients, 30.1%) and vomiting (in 58 of 196 patients, 29.6%). The incidence of grade 3 or 4 hematologic toxicities was leukopenia (22.4%) and neutropenia (20.9%) in all patients. The incidence of grade 3 or 4 anemia and thrombocytopenia was less than 5% in two groups. Patients in GP group had slightly lower grade 3 or 4 mucositis than those in TP group (20.4% vs. 31%), without significantly statistical differences. Only a few patients had grade 3 or 4 hepatotoxic events (in 4 of 196 patients, 2%) and nephrotoxic events (in 5 of 196 patients, 2.5%) in this study (Table 3).
Multivariate analysis
Multivariate analysis was performed to explore the independent prognostic factors. The covariates included sex (male vs. female), age (≤ 45 vs. > 45), smoking history (yes vs. no), drinking history (yes vs. no), histological WHO types (WHO type II vs. WHO type III), T stage (T1–2 vs. T3–4), N stage (N0–1 vs. N2–3), treatment (GP vs. TP), IC cycles (2 cycles vs. 3 cycles), dose of concomitant chemotherapy (≤ 200 mg/m2 vs. > 200 mg/m2). Chemotherapy regimen (GP vs. TP) was an independent prognostic factor of DFS (HR, 0.448; 95%CI 0.218–0.912; p = 0.029). T stage (T1–2 vs. T3–4) was independent prognostic factors for DFS (HR, 2.016; 95%CI 1.149–3.694; p = 0.015), OS (HR, 2.159; 95%CI 1.112–4.159; p = 0.023) and LRFS (HR, 2.973; 95%CI 1.053–8.395; p = 0.04). Multivariate analysis failed to detect any significant differences of prognostic factors for DMFS (Table 4).
Discussion
Induction chemotherapy plus concurrent chemoradiotherapy is a promising treatment selection for LA-NPC according to two recently published data. Although TPF induction chemotherapy plus CCRT can significantly increase DFS, OS and DMFS than CCRT alone for LA-NPC patients, but patients in TPF group experienced higher grade 4 hematological toxicities (15% vs. 1%)(Sun et al. 2016). Another randomized phase III study found GP plus CCRT had better treatment outcomes than CCRT alone for LA-NPC, with acceptable grade 3 or 4 of toxicities (Zhang et al. 2019). A retrospective study demonstrated that the treatment efficacy of GP plus CCRT is equivalent to TPF plus CCRT in LA-NPC, but with less grade 3–4 acute toxicities (Zhu et al. 2019). Therefore, from the current data, GP plus CCRT is a better choice for LA-NPC patients. Actually, before application of GP as induction chemotherapy in LA-NPC, physicians may prefer TP plus CCRT as initial treatment regimen rather than TPF plus CCRT because of concerns about the high rate of grade 4 toxicities. And a phase II study reported TP plus CCRT had a trend to improve survival outcomes than CCRT alone in LA-NPC (Hui et al. 2009). There are two retrospective studies which failed to detect significant differences of treatment efficacy between TP and GP induction chemotherapy followed by CCRT in LA-NPC patients (Liu et al. 2018; Zheng et al. 2018). These published data above mentioned are from endemic area of China is an important point to be noticed. Little is known about the best regime for induction chemotherapy in non-endemic region of China. This study firstly showed that GP plus CCRT could significantly improve DFS and LRFS, and had a trend to improve OS and DMFS of patients from non-endemic area of China when compared with TP plus CCRT.
There are lack of head-to-head prospective studies to compare TPF with TP induction chemotherapy in NPC. Peng et al. conducted a retrospective study to analyze the efficacy of TPF and TP in patients with LA-NPC, and revealed TPF had relatively better survival benefit than TP in LA-NPC patients who received concurrent cisplatin dose < 200 mg/m2, but no significant differences in patients who received cisplatin dose ≥ 200 mg/m2 (Peng et al. 2018). A meta-analysis reported that TPF as induction chemotherapy did not contribute significant survival benefit in LA-NPC patients when compared with TP (He et al. 2019). A study with small sample from India reported that TPF induction chemotherapy was promising regimen to improve treatment response rate, 2-year failure-free survival and OS than TP in LA-NPC patients, but no statistically significant differences were achieved (Lokesh et al. 2018). According to these data, we speculated that the treatment efficacy of TPF was superior to TP. Meanwhile, according to the recently phase III studies, TPF and GP have almost similar treatment efficacy to improve survival of LA-NPC patients (Sun et al. 2016; Zhang et al. 2019). Therefore, it is not difficult to understand why we detected GP induction chemotherapy had better treatment efficacy than TP in LA-NPC patients from non-endemic area of China.
In this study, we firstly detected that GP plus CCRT could further increase LRFS of LA-NPC. This may be explained by the excellent tumor regression induced by GP induction chemotherapy (76.7% treatment response rate). According to our data, the local control of primary tumor mainly contributed to the LRFS because patients in GP group had much higher 3-year and 5-year local control rate than those in TP group (98.1% and 98.1% vs. 94.1% and 87.6%, p = 0.034) (data were not shown). In the era of IMRT, the total locoregional control rate of NPC has been elevated to 90%, but the local recurrence rate of LA-NPC still remains approximaly 10–20% (Sun et al. 2014; Zhang et al. 2015; Zhao et al. 2019). Re-irradiation still represents the mainstay of treatment for recurrence NPC. However, the salvage rate is less than 40% due to sever late complications and treatment-related deaths, especially with re-irradiation dose up to 60 Gy (Han et al. 2012; Hua et al. 2012). Therefore, decreasing recurrence rate as much as possible in initial radiotherapy course is an important way to further improve survival outcomes of LA-NPC. Our study implies that GP induction chemotherapy followed by CCRT has potential efficacy to increase the LRFS for LA-NPC, but this point still needs to be confirmed by randomized control studies.
In this study, the survival outcomes of patients who received TP plus CCRT were slightly lower than published data from endemic area that investigated induction chemotherapy plus CCRT in LA-NPC (Sun et al. 2016; Zhang et al. 2019). We speculated there were two reasons for this situation. First, the survival outcomes of this study were consistent with those reported by studies from non-endemic area, which investigate the role of taxane-based induction chemotherapy followed by CCRT in LA-NPC (Ghosh-Laskar et al. 2019; Ou et al. 2016). Maybe there are potential distinctive genetic traits to impact the sensitivity of taxane-contained chemotherapy regimen in non-endemic region. Second, a selection bias, which potentially impacted the true treatment effects of TP, could not be avoided in retrospective study. On the other hand, survival outcomes of GP plus CCRT in this study were consistent with data of endemic study suggested GP plus CCRT was an effective treatment regimen for LA-NPC patients from both endemic and nonendemic area of China.
Several of our previous studies found that the rate of histological WHO type II in northwest of China (approximate 30%) was much higher than endemic area of China (< 5%) (Chen et al. 2008; Cheung et al. 2012; Zang et al. 2016, 2018). Many studies demonstrated that WHO type II was a worse prognostic factor for NPC (Cheung et al. 2012; Ghosh-Laskar et al. 2019; Zang et al. 2016; Zhao et al. 2012). In subgroup analysis, GP plus CCRT had no significant benefit to improve survival outcomes than TP plus CCRT in patients with WHO type II. This suggested that there was still lack of effective therapeutic methods to improve survival of patients with WHO type II. Compared with CCRT, we ever reported that IC + CCRT could improve DMFS and OS in LA-NPC patients with WHO type II (Zang et al. 2018). This implied that more intensity treatment model should be explored in these patients.
During the entire treatment course, we did not detect any differences in adverse effects between two regimens. Patients in GP group experienced slightly higher grade 3 or 4 neutropenia (27.8%). This result was consistent with published data (Zhang et al. 2019). In this study, patients in TP group had higher grade 3 or 4 mucositis than those in GP group (31% vs. 20.4%), but the proportion was much lower than TPF (40%) (Sun et al. 2016). In general, the two regimens had same side effects for LA-NPC patients from non-endemic area of China.
Conclusion
GP induction chemotherapy followed by CCRT is better than TP followed by CCRT in DFS and LRFS for locoregionally advanced NPC from northwest of China. Prospective studies should be conducted to confirm these results.
Data availability
Data transparency.
Code availability
Analyses were conducted with the use of SPSS software, version 20.0 (IBM) and GraphPad Prism software, version 8.0.
References
Chen Y et al (2008) Preliminary results of a prospective randomized trial comparing concurrent chemoradiotherapy plus adjuvant chemotherapy with radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma in endemic regions of china. Int J Radiat Oncol Biol Phys 71:1356–1364. https://doi.org/10.1016/j.ijrobp.2007.12.028
Chen X et al (2014) Concurrent chemoradiotherapy comparison of taxanes and platinum versus 5-fluorouracil and platinum in nasopharyngeal carcinoma treatment. Chin Med J 127:142–149
Cheung F, Chan O, Ng WT, Chan L, Lee A, Pang SW (2012) The prognostic value of histological typing in nasopharyngeal carcinoma. Oral Oncol 48:429–433. https://doi.org/10.1016/j.oraloncology.2011.11.017
Ghosh-Laskar S et al (2019) Taxane-based Induction Chemotherapy Plus Concurrent Chemoradiotherapy in Nasopharyngeal Carcinoma: Prospective Results from a Non-endemic Cohort. Clin Oncol. https://doi.org/10.1016/j.clon.2019.06.011(Royal College of Radiologists [Great Britain])
Han F et al (2012) Long-term outcomes and prognostic factors of re-irradiation for locally recurrent nasopharyngeal carcinoma using intensity-modulated radiotherapy. Clin Oncol 24:569–576. https://doi.org/10.1016/j.clon.2011.11.010(Royal College of Radiologists [Great Britain])
He Y, Guo T, Wang J, Sun Y, Guan H, Wu S, Peng X (2019) Which induction chemotherapy regimen followed by cisplatin-based concurrent chemoradiotherapy is the best choice among PF, TP and TPF for locoregionally advanced nasopharyngeal carcinoma? Ann Transl Med 7:104. https://doi.org/10.21037/atm.2019.02.15
Hua YJ et al (2012) Long-term treatment outcome of recurrent nasopharyngeal carcinoma treated with salvage intensity modulated radiotherapy. Eur J Cancer (Oxford England: 1990) 48:3422–3428. https://doi.org/10.1016/j.ejca.2012.06.016
Hui EP et al (2009) Randomized phase II trial of concurrent cisplatin-radiotherapy with or without neoadjuvant docetaxel and cisplatin in advanced nasopharyngeal carcinoma. J Clin Oncol 27:242–249. https://doi.org/10.1200/jco.2008.18.1545
Lee N et al (2009) Intensity-modulated radiation therapy with or without chemotherapy for nasopharyngeal carcinoma: radiation therapy oncology group phase II trial 0225. J Clin Oncol 27:3684–3690. https://doi.org/10.1200/jco.2008.19.9109
Liu T et al (2018) A comparison of neoadjuvant chemotherapy with gemcitabine versus docetaxel plus cisplatin in locoregionally advanced nasopharyngeal carcinoma: a propensity score matching analysis. Cancer Manag Res 10:6237–6245. https://doi.org/10.2147/cmar.S186233
Lokesh KN et al (2018) Induction chemotherapy in locoregionally advanced nasopharyngeal carcinoma in adults: Results from a nonendemic region. Indian J Cancer 55:257–260. https://doi.org/10.4103/ijc.IJC_115_18
Mi JL et al (2017) Chemotherapy regimens containing taxanes or fluorouracil in nasopharyngeal carcinoma: which better? Oral Oncol 74:34–39. https://doi.org/10.1016/j.oraloncology.2017.09.003
Ou D et al (2016) Induction chemotherapy with docetaxel, cisplatin and fluorouracil followed by concurrent chemoradiotherapy or chemoradiotherapy alone in locally advanced non-endemic nasopharyngeal carcinoma. Oral Oncol 62:114–121. https://doi.org/10.1016/j.oraloncology.2016.10.011
Pan JJ et al (2016) Prognostic nomogram for refining the prognostication of the proposed 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer 122:3307–3315. https://doi.org/10.1002/cncr.30198
Peng H et al (2018) Optimizing the induction chemotherapy regimen for patients with locoregionally advanced nasopharyngeal Carcinoma: a big-data intelligence platform-based analysis. Oral Oncol 79:40–46. https://doi.org/10.1016/j.oraloncology.2018.02.011
Sun X et al (2014) Long-term outcomes of intensity-modulated radiotherapy for 868 patients with nasopharyngeal carcinoma: an analysis of survival and treatment toxicities. Radiother Oncol 110:398–403. https://doi.org/10.1016/j.radonc.2013.10.020
Sun Y et al (2016) Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol 17:1509–1520. https://doi.org/10.1016/s1470-2045(16)30410-7
Wang J et al (2012) Failure patterns and survival in patients with nasopharyngeal carcinoma treated with intensity modulated radiation in Northwest China: a pilot study. Radiat Oncol 7:2. https://doi.org/10.1186/1748-717x-7-2
Zang J et al (2016) Prognostic model of death and distant metastasis for nasopharyngeal carcinoma patients receiving 3DCRT/IMRT in nonendemic area of China. Medicine 95:e3794. https://doi.org/10.1097/md.0000000000003794
Zang J et al (2018) Induction chemotherapy followed by concurrent chemoradiotherapy is benefit for advanced stage nasopharyngeal carcinoma with different nonkeratinizing carcinoma subtypes. Sci Rep 8:13318. https://doi.org/10.1038/s41598-018-31050-z
Zhang MX et al (2015) Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: a 10-year experience with a large cohort and long follow-up. Eur J Cancer (Oxford England: 1990) 51:2587–2595. https://doi.org/10.1016/j.ejca.2015.08.006
Zhang Y et al (2019) Gemcitabine and cisplatin induction chemotherapy in nasopharyngeal carcinoma. N Eng J Med. https://doi.org/10.1056/NEJMoa1905287
Zhao LN et al (2012) Clinical outcome for nasopharyngeal carcinoma with predominantly WHO II histology treated with intensity-modulated radiation therapy in non-endemic region of China. Oral Oncol 48:864–869. https://doi.org/10.1016/j.oraloncology.2012.03.001
Zhao C et al (2019) Locoregional control and mild late toxicity after reducing target volumes and radiation doses in patients with locoregionally advanced nasopharyngeal carcinoma treated with induction chemotherapy (IC) followed by concurrent chemoradiotherapy: 10-year results of a phase 2 study. Int J Radiat Oncol Biol Phys 104:836–844. https://doi.org/10.1016/j.ijrobp.2019.03.043
Zheng L, Liao W, Xu P, Li B, Wen H, Zhang S (2018) Tumor volume reduction after gemcitabine plus cisplatin induction chemotherapy in locally advanced nasopharyngeal cancer: comparison with paclitaxel and cisplatin regimens. Med Sci Monit 24:8001–8008. https://doi.org/10.12659/msm.909736
Zhu J, Duan B, Shi H, Li Y, Ai P, Tian J, Chen N (2019) Comparison of GP and TPF induction chemotherapy for locally advanced nasopharyngeal carcinoma. Oral Oncol 97:37–43. https://doi.org/10.1016/j.oraloncology.2019.08.001
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 81372421).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zang, J., Xu, M., Li, C. et al. Gemcitabine and cisplatin versus docetaxel and cisplatin as induction chemotherapy followed by concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma from non-endemic area of China. J Cancer Res Clin Oncol 146, 2369–2378 (2020). https://doi.org/10.1007/s00432-020-03229-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03229-3