Abstract
Objective
To study integrin α6 expression in lung adenocarcinoma tissue through comparison with matching adjacent non-cancerous tissues as well as elucidating the correlation between integrin α6 expression with the clinical parameters of lung adenocarcinoma. We also explore the signal pathways associated with integrin α6 up-regulation.
Methods
The clinical data, cancer tissues, and adjacent non-cancerous tissues of 30 patients diagnosed with lung adenocarcinoma were collected from Taizhou Hospital in Zhejiang Province, China, in 2010. The protein levels of integrin α6 were determined by immunohistochemistry methods. mRNA data of 85 lung adenocarcinoma tissues and 14 normal tissues as well as clinical results were collected from GEO30219. We also collected mRNA data of 533 lung adenocarcinoma tissues and 59 normal tissues as well as the clinical results of 522 patients with lung adenocarcinoma from the Cancer Genome Atlas (TCGA) database. The differences in protein and mRNA levels in cancer tissues and non-cancerous tissues were analyzed, and we subsequently investigated the association between integrin α6 expression and key parameters indicating lung adenocarcinoma progression and overall survival rate. Additionally, the possible pathways involved in the up-regulation of integrin α6 were analyzed by GSEA.
Results
The protein levels of integrin α6 in lung adenocarcinoma tissues were significantly higher than those in adjacent tissues (p < 0.01), and were positively correlated with the grade and T stage of lung adenocarcinoma (p < 0.05). Patients with low integrin α6 protein levels had higher survival rates (p < 0.05). The analysis of gene chip data from the TCGA database also showed that the integrin α6 mRNA level was significantly correlated with T stage (p < 0.05), overall survival (OS) rate (p < 0.01), and disease-free survival (DFS) rate (p = 0.005). GSEA gene enrichment analysis identified a series of pathways that may be associated with integrin α6 up-regulation, including the AGR, PYK2, ECM, and PTEN pathways.
Conclusion
Integrin α6 plays an important role in the occurrence and progression of lung adenocarcinoma and may act as a prognostic predictor of lung adenocarcinoma in patients. Based on the results of the present study, integrin α6 may be a potential target gene for the treatment of lung adenocarcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the most prevalent malignant carcinoma (Acosta et al. 2011) and is the leading cause of cancer-related deaths in China (Chen et al. 2016). Lung adenocarcinoma is the most common type of cancer among women, Asian people, and non-smokers (Toh et al. 2006). Lung adenocarcinoma is often metastatic and has a poor prognosis (Howlader et al. 2014). Traditional treatments for lung adenocarcinoma include preoperative and postoperative chemotherapy, surgery, and radiotherapy (Lynch et al. 2004; Shaw et al. 2013). Analyzing the RNA expression profiles of lung adenocarcinoma patients to screen target genes has become a widely debated research topic in the prognosis of lung adenocarcinoma (Bhattacharjee and Meyerson 2001; Beer et al. 2002; Larsen et al. 2007).
Integrins are obligate heterodimers formed by α and β subunits. Human genome contains 18α subunits and 8β subunits, which form 24 distinct types of integrins through different combinations. As a trans-membrane receptor that connects cells and their external environment, integrin is involved in the process of tumorigenesis and its development (Bartolazzi et al. 2010; Guo and Giancotti 2004; Oshita et al. 2002; Stewart and O’Connor 2015; Takenaka et al. 2001). Integrin can transport the chemical components of extracellular matrix and mechanical body, thereby being involved in the regulation of cell information, signaling, morphology, and movement. Integrin can further biological processes, including cell proliferation, survival, and wound healing (Bachelder et al. 1999; Mainiero et al. 2014; Nikolopoulos et al. 2005). When tumors occur, integrin activates the survival signaling pathways by binding to ECM ligands to prevent apoptosis; when cancer cells metastasize, the affinity of integrin to ECM ligands changes (Huttenlocher et al. 1998).
Integrin α6β4 promotes tissue invasion and metastasis and is involved in tumor angiogenesis (Stewart and O’Connor 2015). It is highly expressed in bladder cancer, cervical cancer, lung cancer, pancreatic cancer, thyroid cancer, and basal-like breast cancer. Both integrin α6 and β4 have been found to be associated with the progression of various carcinomas (Friedrichs et al. 1995; Isaac et al. 2012; Jandova et al. 2015; Stewart and O’Connor 2015; Takeyama et al. 2007; Weinel et al. 2010). Furthermore, the high expression of α6β4 in breast cancer, pancreatic cancer, and head and neck squamous cell carcinoma is considered a marker for a poor prognosis (Stewart and O’Connor 2015). Few studies have explored the role of integrin α6 in lung cancer, especially lung adenocarcinoma. The literature has reported that integrin α6β4 is up-regulated in murine Lewis lung carcinoma variants with high metastasis capacity (Sacchi et al. 1989). Jandova et al.’s (2015) study on various NSCLC cell lines has shown that up-regulation of integrin α6 is associated with elevated invasive potential and metastatic capacity of non-small lung adenocarcinoma cells. In another in vitro study on a lung cancer cell line, integrin α6 was indicated to be related with lung cancer tumor metastasis (Hsu et al. 2013). However, the role of integrin α6 in lung adenocarcinoma is not quite clear yet. In this study, we investigate the potential role of integrin α6 in the occurrence and progression of lung adenocarcinoma, and explore the association of integrin α6 with the prognosis result among patients with adenocarcinoma. In addition, we study the signal pathways associated with integrin α6 up-regulation to determine potential targets in our future study related to integrin α6 in lung adenocarcinoma.
Materials and methods
Patients, clinical data, and sample collection
The cancer tissues, adjacent non-cancerous tissues, and clinical data of 30 patients diagnosed with lung adenocarcinoma were collected in Taizhou Hospital, Enze Healthcare Group of Zhejiang Province in 2010. All tissues were preserved by a central laboratory following standard procedures. The tissue samples were fixed with formaldehyde, and 5 μm sections embedded in paraffin were made following routine procedures. The clinical data included age, gender, tumor position, size, stage, TNM stage, T status and tumor nodes, differentiation, clinical TNM stages, and lymph node metastasis. The project was approved by the Ethics Committee of Taizhou Hospital, and all patients signed informed consent for the samples used in the present research. Two experienced pathologists confirmed the histopathological results. Table 1 shows the patients’ clinicopathological parameters.
Lung adenocarcinoma tissue microarray and immunohistochemistry
The lung adenocarcinoma tissue microarray on our collected tissues was prepared by Shanghai Outdo Biotech Company, Ltd. The microarray was immune-stained by immunohistochemistry methods. Briefly, the microarray was deparaffinized with dimethylbenzene and ultrapure water. To retrieve the antigens, heating treatment was performed in a microwave oven in a citrate buffer until boiling point. Intermediate heating was conducted four to six times to maintain a sub-boiling temperature for 10 min, followed by air cooling for 30 min. Endogenous peroxidase was inactivated with 3% hydrogen peroxide for 10 min, followed by blocking with 10% FBS for 1 h. Microarray was incubated with primary integrin α6 antibody (1:100; code: Ab20142, Cambridge, MA, USA) and a second antibody at room temperature for 2–3 h. The integrin α6 staining results were photographed, and the ROI analysis was performed with IPP software. For each sample, the relative expression level of integrin α6 = ROI (sample)/mean value of ROI (adjacent tissue). Graphpad software was used for data processing and graphics.
GEO and TCGA data retrieval
The GSE30219 (FRANCE, 2013) dataset, including RNA expression data, as well as clinical and prognostic data of 85 patients with lung adenocarcinoma and 14 normal tissues were obtained from the GEO website (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi) using the key terms “prognosis” and “lung cancer”. HTSeq-FPKM and the Clinical Dataset for Lung Adenocarcinoma were downloaded from the TCGA database (https://cancergenome.nih.gov/). In total, we retrieved the mRNA expression data of 533 lung adenocarcinoma tissues and 59 normal tissues, as well as the clinical materials of 522 patients with lung adenocarcinoma. Table 2 presents the clinicopathological parameters of patients with lung adenocarcinoma.
GSEA
We used GSEA3.0 software for our analysis. TMP standardized HTSeq-FPKM mRNA expression data of 533 patients were imported into the GSEA software, and the parameters were set as follows: gene sets database: c2.cp.biocarta.v6.2.symbols.gmt, number of permutations: 1000, collapse dataset to gene symbols: false, enrichment statistic: weighted, metric for ranking genes: Signal2Noise. We defined the top 25% samples in respect of the integrin α6 mRNA level as a high expression group, and the last 25% samples as a low expression group.
Protein expression of PTEN pathway-associated genes and integrin α6 for lung adenocarcinoma obtained from the Human Protein Atlas database
The Human Protein Atlas (http://www.proteinaltas.org) enables a system-level investigation of the transcriptome of the protein-coding genes of over 17 types of tumors. We validated the protein expression of PTEN pathway-associated genes and integrin α6 in lung adenocarcinoma patients. The intensity of antibody staining indicated protein expression.
Data processing and statistical analysis
We adopted SPSS Statistics 20.0 software(IBM Corp., Armonk, NY, USA)for statistical analysis. Continuous variables are shown as mean ± standard deviation (SD). Classified variables are shown as frequency. The best cut-off value is determined by X-Tile software. The relationship between integrin α6 protein or mRNA level and survival rates was obtained with the Kaplan–Meier survival approach, along with the Log-rank (Mantel–Cox) test. Pearson correlation coefficients were used to analyze the relationship between integrin α6 and PTEN pathway-associated genes. TMP standardization was used to process the downloaded HTSeq-FPKM data. During the analysis of the data and clinical parameters of 533 lung adenocarcinoma patients from the TCGA database, the median value was selected for analysis when a patient had repeated integrin α6 expression data. All integrin α6 expression data were normalized with log2. A p value < 0.05 denoted a statistically significant difference. At least five individual tests were applied without ambiguity. In GSEA, FDR < 0.05 was considered to be of significance.
Results
Integrin α6 protein levels in lung adenocarcinoma tissues from hospital patients
Integrin α6 protein levels in lung adenocarcinoma tissues were significantly higher than those of adjacent non-cancerous tissues
To examine the protein levels of integrin α6 in the cancer tissues and adjacent non-cancerous tissues of 30 patients with lung adenocarcinoma, we conducted an immunohistochemical experiment. The clinicopathological features of the protein levels of the patients are shown in Table 1. The analysis results show that integrin α6 protein levels in lung adenocarcinoma tissues were significantly higher than those of adjacent non-cancerous tissues (p < 0.0001) (Figs. 1a, 4a, b).
a The difference of integrin α6 protein levels between lung adenocarcinoma and adjacent non-cancerous lung adenocarcinoma tissues based on hospital patients’ data; b the difference in integrin α6 mRNA levels between lung adenocarcinoma and adjacent non-cancerous lung adenocarcinoma based on GSE30219 data; c the difference in integrin α6 mRNA levels between lung adenocarcinoma and adjacent non-cancerous lung adenocarcinoma based on TCGA data. The error bars represent standard deviation (SD)
Association of integrin α6 protein level in cancer tissue of lung adenocarcinoma patients with clinical parameters
The relationship between integrin α6 protein levels in lung adenocarcinoma tissue and clinical parameters was analyzed (Table 1). The results show that a higher protein level of integrin α6 was closely correlated with tumor size. When tumor size was larger than 3 cm, the integrin α6 protein level was significantly higher (p = 0.034). Integrin α6 protein was also up-regulated in patients with a higher stage (p = 0.031) or T stage (p = 0.039) compared to those with a lower stage or T stage (Figs. 2a, b, 4c, d). In addition, integrin α6 protein levels were also related to gender, with a higher level of integrin α6 among males (p = 0.0005). Other clinical parameters were not significantly associated with integrin α6 protein levels, such as age, location, TMN stage, and lymph node metastasis (p > 0.05).
a The relationship between integrin α6 protein level with different stages, based on hospital patients data; b the relationship between integrin α6 protein level with different T stages, based on hospital patients’ data; c the relationship between integrin α6 mRNA level with different T stages based on GSE30219 data; d the relationship between integrin α6 mRNA level with different T stages based on TCGA data. The error bars represent standard deviation (SD)
The survival rate among patients with a low integrin α6 protein level is significantly higher than that among patients with a high integrin α6 level
The Kaplan–Meier analysis results are shown in Figs. 3a, b and 4e–h. The patients with an integrin α6 mRNA lower than the mean expression were assigned to the low expression group, while the other patients were assigned to the high expression group. The overall survival rate (p = 0.025) was significantly higher in the integrin α6 low expression group, as was their disease-free survival rate (p = 0.0459).
a Kaplan–Meier curve for overall survival rate in lung adenocarcinoma patients grouped by the protein level of integrin α6: based on hospital patients’ data; b Kaplan–Meier curve for disease-free survival rate in lung adenocarcinoma patients grouped by the protein level of integrin α6: based on hospital patients’ data; c Kaplan–Meier curve for overall survival of patients with lung adenocarcinoma grouped by the level of integrin α6 mRNA based on GSE30219 data; d Kaplan–Meier curve for disease-free survival of patients with lung adenocarcinoma grouped by the level of integrin α6 mRNA based on GSE30219 data; e Kaplan–Meier curve for overall survival of patients with lung adenocarcinoma grouped by the level of integrin α6 mRNA based on TCGA data; f Kaplan–Meier curve for disease-free survival of patients with lung adenocarcinoma grouped by the level of integrin α6 mRNA based on TCGA data. Error bars represent standard deviation (SD)
a Example of integrin α6 staining intensity in lung adenocarcinoma tissues (relative expression value = 3.81); b example of integrin α6 staining intensity in adjacent non-cancerous lung adenocarcinoma tissues (relative expression value = 0.49); c example of integrin α6 staining intensity in lung adenocarcinoma tissues with low stages (T1, stage II, relative expression value = 1.69); d example of integrin α6 staining intensity in lung adenocarcinoma tissues with high stages (T2, stage III, relative expression value = 5.81); e example of integrin α6 staining intensity in lung adenocarcinoma tissues with good prognosis (alive at 56 months follow up; relative expression value = 1.93); f example of integrin α6 staining intensity in lung adenocarcinoma tissues with bad prognosis (dead at 14 months follow up; relative expression value = 5.73); g example of integrin α6 staining intensity in lung adenocarcinoma tissues with good prognosis (not relapsed at 57 months follow up; relative expression value = 1.57); h example of integrin α6 staining intensity in lung adenocarcinoma tissues with bad prognosis (relapsed at 8 months follow up; relative expression value = 4.82). Magnification is 10 × 40 for all images
Integrin α6 mRNA levels in lung adenocarcinoma tissues based on the GEO30219 and the TCGA dataset
The integrin α6 mRNA level was down-regulated in lung adenocarcinoma tissues
We downloaded mRNA data and the clinical materials of lung adenocarcinoma patients from the GEO30219 and TCGA databases. The clinical parameters in TCGA are presented in Table 2. The analysis results show that integrin α6 mRNA was lower in carcinoma tissues than that of adjacent non-cancerous tissues in the TCGA database (p < 0.0001) as well as in the GEO30219 database (p < 0.05) (Fig. 1b, c).
Relationships between the integrin α6 mRNA levels in lung adenocarcinoma tissues and clinical parameters
We studied the relationship between integrin α6 mRNA levels and clinical parameters in the TCGA (Table 2). Although the mRNA expression level was significantly associated with T stages in TCGA (p < 0.05), this correlation was not significant in GEO30219 (Fig. 2c). In the cancer tissues of lung adenocarcinoma patients with higher T stages, the integrin α6 mRNA levels were significantly higher in TCGA (Fig. 2d). However, no other clinical parameters were associated with the integrin α6 mRNA levels with statistical significance, including age, gender, race, location, M stage, and lymph node metastasis (p > 0.05).
The survival rate of patients with higher integrin α6 mRNA levels was significantly higher than that of patients with lower levels of integrin α6
The Kaplan–Meier analysis results are shown in Fig. 3c–f. The patients with integrin α6 mRNA lower than the best cut-off value were assigned to the low expression group; the other patients were assigned to the high expression group. The overall survival rate was significantly higher in the integrin α6 low expression group in TCGA (p < 0.0001, cut-off value = 5.948) as well as GEO30219 (p < 0.05, cut-off value = 7.256). What is more, the disease-free survival rate was also significantly higher in the integrin α6 low expression group in TCGA (p < 0.01, cut-off value = 6.022) although there was no significant difference in GEO30219 (p = 0.6167, cut-off = 7.311).
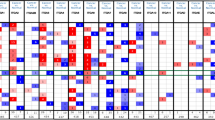
Several pathways may be involved in the up-regulation of integrin α6
We adopted GSEA to analyze the data of the patients in the top 25% with regards to their integrin α6 mRNA levels, and also the data of patients in the bottom 25%. Table 3 shows the results of the GSEA employed to identify the pathways implicated in integrin α6 up-regulation in lung adenocarcinoma. These results include ES, NES, p values, and FDR Q values. The rankings of those pathways are derived from the NES values. The AGR, PYK2, and ECM pathways are ranked in the top three (p < 0.05) (Fig. 5a–c). In addition, the PTEN pathway is enriched in the group with a high expression of integrin α6 (Fig. 5d).
PTEN pathway-associated genes are significantly related to integrin α6
We found that PTEN and other signal pathways were significantly enriched in the group of integrin α6 up-regulation. As shown in Table 4, the genes related to the PTEN signaling pathway, PDPK1, MAPK1, GRB2, ILK, CEAR1, PTEN, PIK3R1, SOS1, ITGB1, FOXO3, and PIK3CA, are more enriched in the group with a higher expression of integrin α6. On the other hand, the correlation analysis between integrin α6 and the related genes are shown in Table 5. We find that all these genes related to the PTEN signaling pathway have a significant correlation with integrin α6 (p < 0.0001) in TCGA. An immunohistochemical stain for the PTEN pathway-associated proteins and integrin α6 is shown in Figs. 6 and 7. The protein expression of the PTEN pathway-related genes and itga6 is primarily consistent.
Protein expression of PTEN pathway-associated genes and integrin α6 as shown in IHC images obtained from the Human Protein Atlas database. a Low staining of integrin α6 in LUAD (Patient ID 2041; antibody CAB009009). b Low staining of integrin α6 in LUAD (Patient ID 2403; antibody CAB009009). c High staining of ITGB1 in LUAD (Patient ID 2041; antibody CAB003434). d High staining of ITGB1 in LUAD (Patient ID 2403; antibody CAB003434). e Not detected staining of SOS1 in LUAD (Patient ID 2041; antibody CAB005396). f Not detected staining of SOS1 in LUAD (Patient ID 2403; antibody CAB005396). g. Not detected staining of ILK in LUAD (Patient ID 2041; antibody CAB004041). h Not detected staining of ILK in LUAD (Patient ID 2403; antibody CAB004041). i Not detected staining of GRB2 in LUAD (Patient ID 2041; antibody CAB002589). j Low staining of GRB2 in LUAD (Patient ID 2403; antibody CAB002589). k Not detected staining of MAPK1 in LUAD (Patient ID 2041; antibody HPA003995). l Low staining of MAPK1 in LUAD (Patient ID 2403; antibody HPA003995). m Not detected staining of PIK3R1 in LUAD (Patient ID 2041; antibody CAB004268). n Low staining of PIK3R1 in LUAD (Patient ID 2403; antibody CAB004268). o Low staining of FOXO3 in LUAD (Patient ID 2041; antibody CAB004074). p Median staining of FOXO3 in LUAD (Patient ID 2403; antibody CAB004074). q Low staining of PDPK1 in LUAD (Patient ID 2041; antibody CAB004272). r Median staining of PDPK1 in LUAD (Patient ID 2403; antibody CAB004272). Magnification is 4 × 10 for all images
Protein expression of PTEN pathway-associated genes and integrin α6 as shown in IHC images obtained from the Human Protein Atlas database. a Low staining of integrin α6 in LUAD (Patient ID 3003; antibody CAB009009; magnification of 4 × 10). b Median staining of integrin α6 in LUAD (Patient ID 3391; antibody CAB009009; magnification of 4 × 10). c Not detected staining of MAPK1 in LUAD (Patient ID 3003; antibody HPA030069). d Low staining of MAPK1 in LUAD (Patient ID 3391; antibody HPA030069). e Low staining of PIK3R1 in LUAD (Patient ID 3003; antibody CAB004268). f Median staining of PIK3R1 in LUAD (Patient ID 3391; antibody CAB004268). g Low staining of FOXO3 in LUAD (Patient ID 3003; antibody CAB004074). h Low staining of FOXO3 in LUAD (Patient ID 3391; antibody CAB004074). Magnification is 4 × 10 for all images
Discussion
Lung adenocarcinoma is a common malignant carcinoma with a poor prognosis (Howlader et al. 2014). Consequently, it is necessary to explore the mechanism of lung adenocarcinoma tumorigenesis and progression to establish effective treatment strategies. In the current study, we explored the association of integrin α6 protein levels and mRNA levels with the occurrence, progression, and prognosis results of lung adenocarcinoma.
According to the results of this study, the protein level of integrin α6 was significantly higher in cancer tissues compared to adjacent non-cancerous tissues in patients with lung adenocarcinoma, which may suggest an association of integrin α6 with the development of lung adenocarcinoma. However, this finding is not consistent with a statistical analysis of the mRNA level of integrin α6 based on the GEO30219 and TCGA dataset. A previous study suggested that other expression regulation mechanisms outside the regulation on the mRNA level have been involved in the regulation of integrin α6 protein expression during the development of lung adenocarcinoma (Frans et al. 1991), which may partially explain the inconsistency.
The results of our study also show that both integrin α6 protein and mRNA levels are significantly associated with the progression of lung adenocarcinoma. In analyzing patients’ data, the expression level of integrin α6 was up-regulated in patients at an advanced stage and T stage of lung adenocarcinoma. The association between integrin α6 and T stage was supported in our analysis of the TCGA data. These results suggest integrin α6 is closely linked to lung adenocarcinoma progression. Earlier studies have revealed an association between integrin α6 and metastasis capacity in lung cancer. It has been reported that integrin α6β4 is up-regulated in murine Lewis lung carcinoma variants with high metastasis capacity (Sacchi et al. 1989). In addition, up-regulation of integrin α6 was shown to be related to the promotion of metastasis in lung cancer or non-small lung adenocarcinoma cell line (Hsu et al. 2013). In our study, the mean value of integrin α6 expression indicated a correlation with parameters related to metastasis, such as the TNM stage and lymph node metastasis in an analysis of patient data, and M and N status in an analysis of the TCGA data. However, the difference is not statistically significant, which may be a result of the relatively small size of the patient group. Thus, further studies with a large cohort of patients are needed in the future.
In addition, high expression levels of integrin α6 predict a poor prognosis for patients with lung adenocarcinoma. The results are consistent for both protein and mRNA of integrin α6. The close relationship between integrin α6 and the prognosis results of lung adenocarcinoma may suggest the potential application of integrin α6 as a predictor of prognoses among patients with lung adenocarcinoma.
Stewart et al. (2016) showed that integrin α6β4 up-regulation is associated with adenocarcinoma tissues compared to normal tissues, with venous invasion and with reduced overall patient survival among non-small lung cancer, including adenocarcinoma and squamous cell carcinoma. Their study and ours suggest that up-regulation of integrin α6 may be associated with the occurrence, progression, and prognosis of lung adenocarcinoma.
The analysis of the signal pathways associated with up-regulation of integrin α6 indicates that the AGR, PYK2, ECM, and PTEN pathways are significantly enriched in the integrin α6 high expression group. Previous studies have shown that Agrin is involved in several receptor signaling pathways of effective oncogenes, such as SFK (Camilleri et al. 2007); ErbB (Trinidad et al. 2000). The PYK2 signaling pathway was reported to be involved in the occurrence and proliferation of non-small cell lung cancer (Wan et al. 2015). Integrins play a regulatory role by binding to ECM or altering their affinity to ECM, while the expression of ECM receptors in lung adenocarcinoma is associated with the growth and metastasis of lung adenocarcinoma cells (Stevens et al. 2017). PTEN, as a tumor suppressor gene, is often mutated in several kinds of tumors, including lung adenocarcinoma (Bi et al. 2017; Li and Sun 1997). PTEN can regulate a variety of cellular physiological processes, including survival, proliferation, growth, and migration, through down-regulating the PI3 kinase signaling pathway, a key carcinogenic signaling pathway. Studies have shown that the PTEN signaling pathway plays an important regulatory role in the invasion and migration of non-small cell lung adenocarcinoma cells (Li et al. 2016; Xia et al. 2016), and has a prognosis predictor value for non-small cell lung cancer patients (Tang et al. 2006). These results of pathway analysis provide clues for the mechanism of integrin α6 regulation and the association of integrin α6 with the progression of lung adenocarcinoma and its prognosis.
To the best of our knowledge, this is the first time integrin alpha 6 subunit has been reported in the progression and prognosis of patients with lung adenocarcinoma. Our study has revealed the important role of integrin α6 in the progression and prognosis of lung adenocarcinoma, which suggests the potential of integrin α6 as a target gene and prognosis predictor in lung adenocarcinoma treatment. However, further studies, especially using a large sample size, are still needed. The mechanism of integrin α6 in lung adenocarcinoma also needs additional experimental verification. In comparison with previous studies, our study has included patient samples from a hospital, thus the result is of more clinical and practical importance. The analysis was based on the medical records of the patients, which can greatly reduce interview bias. Furthermore, we have analyzed the association of integrin α6 with lung adenocarcinoma from both the protein and mRNA levels, and obtained consistent results, thus taking the probability of inconsistency of mRNA and protein into account, thereby reducing the bias that may have been generated by the small sample size.
Conclusion
Integrin α6 plays an important role in the occurrence and progression of lung adenocarcinoma and may act as a prognostic predictor of lung adenocarcinoma patients. Based on the results of the current study, integrin α6 may be a potential target gene and prognosis predictor for the treatment of lung adenocarcinoma patients. However, more studies are needed for further investigation.
References
Acosta D, Suzuki M, Connolly D, Thompson RF, Fazzari MJ, Greally JM, Montagna C (2011) DNA methylation changes in murine breast adenocarcinomas allow the identification of candidate genes for human breast carcinogenesis. Mamm Genome 22:249–259
Bachelder RE, Ribick MJ, Marchetti A, Falcioni R, Soddu S, Davis KR, Mercurio AM (1999) P53 inhibits α6β4 integrin survival signaling by promoting the caspase 3–dependent cleavage of Akt/PKB. J Cell Biol 147:1063–1072
Bartolazzi A, Cerboni C, Flamini G, Bigotti A, Lauriola L, Natali PG (2010) Expression of alpha 3 beta 1 integrin receptor and its ligands in human lung tumors. Int J Cancer 64:248–252
Beer DG et al (2002) Gene-expression profiles predict survival of patients with lung adenocarcinoma. Nat Med 8:816–824
Bhattacharjee A, Meyerson M (2001) Classification of human lung carcinomas by mRNA expression profiling. Proc Natl Acad Sci USA 98:13790–13795
Bi L, Yan X, Yang Y, Qian L, Tian Y, Mao JH, Chen W (2017) The component formula of Salvia miltiorrhiza and Panax ginseng induces apoptosis and inhibits cell invasion and migration through targeting PTEN in lung cancer cells. Oncotarget 8:101599–101613
Camilleri AA, Willmann R, Sadasivam G, Lin S, Rüegg MA, Gesemann M, Fuhrer C (2007) Tyrosine phosphatases such as SHP-2 act in a balance with Src-family kinases in stabilization of postsynaptic clusters of acetylcholine receptors. BMC Neurosci 8(1):46
Chen W et al (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132
Frans H, Ingrid K, Geurts KA, Arnoud S (1991) Molecular cloning of the human α6 integrin subunit. FEBS J 199:425–433
Friedrichs K, Ruiz P, Franke F, Gille I, Terpe HJ, Imhof BA (1995) High expression level of α6 integrin in human breast carcinoma is correlated with reduced survival. Cancer Res 55:901–906
Guo W, Giancotti FG (2004) Integrin signalling during tumour progression. Nat Rev Mol Cell Biol 5:816–826
Howlader N et al (2014) SEER cancer statistics review, 1975–2011. Available from: http://seer.cancer.gov/csr/1975_2011/
Hsu YL, Wu CY, Hung JY, Lin YS, Huang MS, Kuo PL (2013) Galectin-1 promotes lung cancer tumor metastasis by potentiating integrin α6β4 and Notch1/Jagged2 signaling pathway. Carcinogenesis 34:1370–1381
Huttenlocher A, Lakonishok M, Kinder M, Wu S, Truong T, Knudsen KA, Horwitz AF (1998) Integrin and cadherin synergy regulates contact inhibition of migration and motile activity. J Cell Biol 141:515–526
Isaac J, Ying WL, Tarapore P, Ho S (2012) Abstract B48: integrin α6 S-nitrosylation induces prostate cancer cell migration by loss of adhesion to laminin-1. Cancer Res 72:B48–B48
Jandova J, Mason CJ, Pawar SC, Watts GS (2015) Fn14 receptor promotes invasive potential and metastatic capacity of non-small lung adenocarcinoma cells through the up-regulation of integrin α6. Neoplasma 62:41–52
Larsen JE, Pavey SJ, Passmore LH, Bowman RV, Hayward NK, Fong KM (2007) Gene expression signature predicts recurrence in lung adenocarcinoma. Clin Cancer Res 13:2946–2954
Li DM, Sun H (1997) TEP1, encoded by a candidate tumor suppressor locus, is a novel protein tyrosine phosphatase regulated by transforming growth factor beta. Cancer Res 57:2124–2129
Li X et al (2016) Triptolide reduces proliferation and enhances apoptosis of human non-small cell lung cancer cells through PTEN by targeting miR-21. Mol Med Rep 13:2763–2768
Lynch TJ et al (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350:2129–2139
Mainiero F et al (2014) The coupling of alpha6beta4 integrin to Ras-MAP kinase pathways mediated by Shc controls keratinocyte proliferation. EMBO J 16:2365–2375
Nikolopoulos SN, Blaikie P, Yoshioka T, Guo W, Puri C, Tacchetti C, Giancotti FG (2005) Targeted deletion of the integrin beta4 signaling domain suppresses laminin-5-dependent nuclear entry of mitogen-activated protein kinases and NF-kappaB, causing defects in epidermal growth and migration. Mol Cell Biol 25:6090–6102
Oshita F et al (2002) Increased expression of integrin beta1 is a poor prognostic factor in small-cell lung cancer. Anticancer Res 22:1065–1070
Sacchi A, Falcioni R, Piaggio G, Gianfelice MA, Perrotti N, Kennel SJ (1989) Ligand-induced phosphorylation of a murine tumor surface protein (TSP-180) associated with metastatic phenotype. Cancer Res 49:2615
Shaw AT et al (2013) Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med 368:2385–2394
Stevens LE et al (2017) Extracellular matrix receptor expression in subtypes of lung adenocarcinoma potentiates outgrowth of micrometastases. Can Res 77:1905
Stewart RL, O’Connor KL (2015) Clinical significance of the integrin α6β4 in human malignancies. Lab Investig J Tech Methods Pathol 95:976–986
Stewart RL et al (2016) Elevated integrin α6β4 expression is associated with venous invasion and decreased overall survival in non-small cell lung cancer. Hum Pathol 54:174–183
Takenaka K, Shibuya M, Takeda Y, Hibino S, Gemma A, Ono Y, Kudoh S (2001) Altered expression and function of β1 integrins in a highly metastatic human adenocarcinoma cell line. Int J Oncol 17:1187–1194
Takeyama H, Funahashi H, Sawai H, Takahashi H, Yamamotorm M, Akamo Y, Manabe T (2007) Expression of alpha6 integrin subunit is associated with malignancy in gastric gastrointestinal stromal tumors. Med Sci Monit Int Med Jo Exp Clin Res 13:CR51
Tang JM, He QY, Guo RX, Chang XJ (2006) Phosphorylated Akt overexpression and loss of PTEN expression in non-small cell lung cancer confers poor prognosis. Lung Cancer 51:181–191
Toh CK et al (2006) Never-smokers with lung cancer: epidemiologic evidence of a distinct disease entity. J Clin Oncol 24:2245–2251
Trinidad JC, Fischbach GD, Cohen JB (2000) The Agrin/MuSK signaling pathway is spatially segregated from the neuregulin/ErbB receptor signaling pathway at the neuromuscular junction. J Neurosci Off J Soc Neurosci 20:8762
Wan J, Che Y, Kang NN, Chai HP (2015) SOCS3 may regulate HIF-1α expression and cell proliferation by mediating PYK2 signaling pathways in the small cell lung cancer cell line. Oncol Prog 1:79–83
Weinel RJ, Rosendahl A, Neumann K, Chaloupka B, Erb D, Rothmund M, Santoso S (2010) Expression and function of VLA-α2, -α3, -α5 and -α6-integrin receptors in pancreatic carcinoma. Int J Cancer 52:827–833
Xia M, Tong JH, Ji NN, Duan ML, Tan YH, Xu JG (2016) Tramadol regulates proliferation, migration and invasion via PTEN/PI3K/AKT signaling in lung adenocarcinoma cells. Eur Rev Med Pharmacol Sci 20:2573
Funding
This study was funded by Zhejiang Provincial Natural Fund (The Mechanism of Integrin Mediated Wnt/β-catenin Signaling Pathway in Regulating Lymphangiogenesis in Lung Cancer) (grant number LQ18H160029).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest to declare.
Patient study
The study has been approved by the ethics committee and patients gave their informed consent before material was obtained for use in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shen, J., Xu, J., Chen, B. et al. Elevated integrin α6 expression is involved in the occurrence and development of lung adenocarcinoma, and predicts a poor prognosis: a study based on immunohistochemical analysis and bioinformatics. J Cancer Res Clin Oncol 145, 1681–1693 (2019). https://doi.org/10.1007/s00432-019-02907-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-02907-1