Abstract
Introduction
Nivolumab is the first checkpoint-inhibitor approved for the treatment of advanced HCC patients. Real-life experience data of nivolumab treatment in HCC patients, especially those with advanced liver disease, is scarce.
Materials and methods
All patients with confirmed advanced HCC and nivolumab treatment from three large German centers were retrospectively analyzed. Clinical parameters and outcome were assessed.
Results
A total of 34 patients were included. At the time of treatment initiation 5 patients (14.7%) were classified as stage BCLC B and 29 (85.3%) BCLC C, respectively. 25 (73.5) patients had received prior sorafenib treatment. All patients presented with cirrhosis, namely Child–Pugh stages A (56%) or B (41%), respectively. At time of patient’s assessment, 20 out of 34 (58.8%) patients had died. Grade 3 toxicities occurred in two patients (5.9%). Best overall responses were partial response in four patients (11.8%) and stable disease in eight patients (23.5%). The median overall survival of the whole cohort was 7.5 weeks (range 0–46). Child–Pugh B stage disease at treatment start was significantly associated with poor outcome.
Discussion
Nivolumab treatment seems safe and clinical efficacious. Patients with advanced liver disease require further prospective evaluation due to probable limited efficacy of nivolumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most common malignant primary liver cancer affecting more than half a million patients annually (El-Serag 2011). HCC mainly develops on the basis of chronic liver injury caused by chronic viral hepatitis, alcohol abuse or metabolic disorders. The constant liver damage and concomitant inflammation results in an impaired tissue remodeling and, ultimately, in liver cirrhosis, which is the predominant risk factor for HCC development. Curative HCC treatment is only available in early stages involving local ablative procedures, surgical resection or liver transplantation. In patients not amenable to curative or local therapy as well as patients with metastatic disease, systemic treatment is the therapy of choice (El-Serag 2011). Until recently, only tyrosinkinase-inhibitors (TKI) were approved for these patients, i.e. sorafenib in first and regorafenib in a second line setting. Sorafenib was approved in 2008 and demonstrated a survival benefit of 10.7 months versus 7.9 months in placebo-treated Western world patients (Llovet et al. 2008). More recently regorafenib was approved for second-line treatment after progression during sorafenib treatment with comparable survival benefits (10.6 versus 7.8 months) (Bruix et al. 2017). In the last 2 years, two additional TKIs, namely Cabozantinib and Lenvatinib, also demonstrated survival benefit in advanced HCC (Raoul et al. 2018). Furthermore, the VEGF-R2 antibody Ramucirumab improved survival compared to placebo in high-risk patients with high AFP levels (Zhu et al. 2018).
Since HCC is a hallmark of inflammation-induced cancers, several preclinical and early-phase studies investigated the efficacy of immunotherapeutic approaches for advanced HCCs. While results of studies on oncolytic viruses, vaccines or cytokine-activated killer cells have not yet fulfilled the expectations, clinical trials on the safety and efficacy of checkpoint inhibitors were particularly promising (El-Khoueiry et al. 2017). Blockage of the checkpoints programmed cell death-1/programmed cell death ligand 1 (PD-1/PD-L1) and cytotoxic T lymphocyte-associated protein 4 (CTLA-4) disrupts acquired immunosuppressive mechanisms of cancer cells and activates natural anti-tumor effects of immune cells. Nivolumab is one of the first human immunoglobulin G4 (IgG4) monoclonal antibodies, which binds to the PD-1 receptor. Nivolumab targets an epitope of PD-1 with high affinity and specificity. PD-1 is expressed on different immune cells and especially on T-cells (Keir et al. 2008). Specialized cytotoxic CD8 + T-cells take the key role in adaptive anti-tumor immune responses. The concept of interrupting the activation of PD1 by targeting PD-1 or its ligand PD-L1 in cancer patients and thereby activating the immune system against tumor cells has been successfully proven in several tumor entities including HCC (Brahmer et al. 2012; Topalian et al. 2012). In September 2017 nivolumab was the first checkpoint-inhibitor, granted approval for HCC by the United States Food and Drug Administration (FDA) based on the results of the phase 1–2 dose escalation and expansion trial Checkmate040 (El-Khoueiry et al. 2017). In brief, response rate across all cohorts was reported in about 20% of patients, stable disease was achieved in 45%. Median duration of response was 9.9 months, median time to disease progression 4.1 months. Updated survival data of the Checkmate040 was presented at the end of last year (Sangro et al. 2017). Notably, the subset of sorafenib-naive patients showed a median overall survival of 28 months favoring immunotherapy use as first-line treatment. However, nivolumab has not yet been approved by European Medicines Agency (EMA) and data from the phase 3 trial comparing nivolumab to sorafenib in the first-line setting are urgently awaited [CheckMate-459 trial (NCT02576509)].
As nivolumab has not yet been approved for HCC treatment in Europe, a nivolumab based therapy is only possible in cases if patients do not tolerate TKI treatment or progress under sorafenib and no other tumor-directed therapies are accessible. We here retrospectively analyzed real-life experience of patients treated with nivolumab for advanced HCC from three high-volume German centers.
Methods
Between July 2015 and January 2018 patients with confirmed advanced HCC (BCLC B and C) and nivolumab treatment from three large German university centers were retrospectively identified and included in this study. Patients’ charts and hospital electronic medical records were anonymized and reviewed.
Patients were followed until death or last contact. Dates of treatment start and end of nivolumab were assessed separately. Survival was calculated as the time from initiation of nivolumab until death from any cause or last follow-up. The safety profile was assessed and graded using the Common Toxicity Criteria (CTCAE), version 4.0 (National Cancer Institute (NIH) Division of Cancer Treatment and Diangosis (DCTD) 2009).
HCC was diagnosed according to current guideline recommendations (Galle et al. 2018). Inclusion criteria were a diagnosis of advanced HCC and treatment with nivolumab. The BCLC stage determined the treatment of HCC (Galle et al. 2018). BCLC stage, model of end-stage liver disease (MELD) score, Child–Pugh score and Albumin–Bilirubin (ALBI) grade (Johnson et al. 2015) were assessed by clinical examination, laboratory parameters and the results of ultrasound, CT scans and MRI imaging at the time of treatment start of nivolumab.
Nivolumab was administered as recommended in the official dosing and safety information. Treatment schedules were modified if necessary, according to the treating physician’s discretion.
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee. Written, informed consent was obtained from each patient included in the study. The study was approved by the institutional Review Boards and responsible Ethical Committees at the University Hospitals [Approval numbers: Mainz 837.199.10 (7208), Frankfurt SGI-11-2017, Ulm 317/12, 230/14, 128/15].
Outcome evaluation
Best treatment response was assessed by radiological imaging according to modified RESIST 1.1. criteria (Lencioni and Llovet 2010) based on contrast-enhanced abdominal computed tomography (CT) or magnetic resonance imaging (MRI). Imaging was carried out every 8–12 weeks during nivolumab treatment.
Outcome was assessed as stable disease (SD), progressive disease (PD), partial response (e.g. treatment response of metastasis) (PR), complete response (CR) or not assessable if no radiological staging was done.
Statistical analysis
This study was designed as a retrospective cohort study. Patients were followed till death or last contact. Dates of treatment start and finish with nivolumab were assessed separately. Continuous variables are shown as means ± standard deviation and categorical variables are reported as frequencies and percentages.
Predictors of survival were determined using a univariate Cox regression hazard model. Death was recorded as an event. For the assessment of independent predictors of survival, a multivariate Cox regression hazard model with forward stepwise (likelihood ratio) entry was used. Statistical analyses were performed with SPSS (Version 22.0, IBM, New York, USA) and Prism (7.0, GraphPad, La Jolla, USA).
Results
Baseline patient characteristics
A total of 34 patients were included in the study. 26 male patients (76.5%) and 8 female patients (23.5%) with a median age of 65 years (range 40–77 years). All patients were of Caucasian ethnicity. Most common underlying liver disease was chronic hepatitis C virus (HCV) infection in 10 (29.4%) patients. Seventeen patients (50.0%) were BCLC stage C at initial diagnosis of HCC. The detailed patients´ characteristics are provided in Table 1.
Patients’ characteristics at start of nivolumab treatment
At the time of treatment start with nivolumab 5 patients (14.8%) were classified to BCLC stage B and 29 (85.3%) patients to BCLC stage C. Nineteen patients (55.9%) had extrahepatic metastases and 19 (55.9%) macrovascular invasion. Nineteen patients (55.9%) presented with cirrhosis at Child–Pugh stage A, 14 (41.2%) patients at Child–Pugh stage B and one patient at Child–Pugh stage C (2.9%), respectively.
Nine patients (26.5%) were treatment-naïve to sorafenib and received nivolumab as first systemic treatment. Twenty-five (73.5%) patients had received systemic treatment with sorafenib for a median of 14 weeks (4-432) prior to starting nivolumab. Nine (26.5%) patients had undergone initial surgery/ablation in a curative intent and 15 (44.1%) patients had received local–regional therapies including TACE or SIRT prior to systemic therapy. The detailed patients´ characteristics are provided in Table 1.
Nivolumab treatment and outcome
The median follow-up time after the start of nivolumab was 100 days (range 5–610 days). The median treatment duration was 8 weeks (range 1–80 weeks) with a median of 4 cycles (range 1–42 cycles) administered.
At the time of data analysis in March 2018, 20 out of 34 (58.9%) patients had died. Causes of death were tumor progression in 16 patients (80%), acute liver failure in three patients (15%) and one fatal variceal bleeding (5%). 8 patients (23.5%) were still on nivolumab treatment and 6 patients (17.6%) had stopped treatment for other reasons [patients wish (n = 5), toxicity (n = 1)].
During the treatment, two patients (5.9%) showed grade 3 toxicities probably attributable to nivolumab: One patient developed bullous lichenoid drug eruption and had to stop treatment after 7 cycles. The other patient developed hepatitis grade 2–3 which resolved after steroid treatment.
A total of 8 patients (23.5%) showed an AFP response during the treatment with declining levels.
The best radiological outcomes were a partial response in 4 patients (11.8%) and stable disease in 8 patients (23.5%). Twelve patients had progressive disease (35.3%) at the time of the first radiological evaluation and radiological outcomes were not assessable in 10 patients, who had not undergone imaging at study endpoint. The median overall survival in the whole cohort was 7.5 weeks with a range of 0–46 weeks.
Risk factors for survival
To evaluate risk factors for death of patients receiving nivolumab therapy we first conducted a univariate Cox regression model with the variables male gender, age above 65, BCLC stage at start of nivolumab, previous sorafenib treatment, Child–Pugh stage at beginning of nivolumab treatment, ALBI score at beginning of nivolumab treatment, an ECOG above 0, AFP response after nivolumab and neutrophil/lymphocyte ratio > 2.75 (He et al. 2018). In the univariate analysis Child–Pugh stage (HR 7.742, 95% CI 0.2.619–22.783, p < 0.001) and an ECOG > 0 (HR 3.441, 95% CI 01.049–11.268, p = 0.041) were significant risk factors for survival while previous sorafenib treatment was associated with a risk reduction (HR 0.387, 95% CI 0.152–0.988, p = 0.047). After inclusion of all factors with a p value < 0.1 in a multivariate model only an advanced Child–Pugh stage remained as a significant independent risk factor for survival (HR 7.724, 95% CI 2.619–22.784, p < 0.001) (Table 2).
Discussion
The PD-1 inhibitor nivolumab has recently been approved by the FDA based on the results of the phase I/II CheckMate 040 (El-Khoueiry et al. 2017) trial. The study was composed of two parts, a dose escalation trial with 48 patients and a dose expansion trial with 214 patients. Patients were investigated in four sub-cohorts (HBV or HCV infection and sorafenib naïve or treated), 68% of the cohort was sorafenib pre-treated. Response rate across all cohorts was reported in 20% of patients (14–20% in HBV or HCV infected patients and 21–23% in uninfected patients), stable disease was achieved in 45%.
More than 67% of the patients in the study had extrahepatic metastasis, nearly all patients were Child–Pugh stage A (99%). Updated results were reported at ASCO GI 2018 Annual Meeting for the subgroup of 154 sorafenib experienced patients from both cohorts. Objective response was 14% and median overall survival was 15.1 months leading to the conclusion of the investigators that nivolumab demonstrates a meaningful benefit for pre-treated patients (El-Khoueiry et al. 2018). However, especially sorafenib naïve patients had a favorable prognosis with a median overall survival of 28 months when nivolumab is given as first systemic therapy (Sangro et al. 2017).
So far only one group reported outcomes from 11 real-world patients treated with nivolumab for advanced HCC outside of clinical trials (Feng et al. 2017). All of these patients, hailed from China, had HBV-related cirrhosis and were BCLC stage B or C. They underwent a median of 7.1 cycles nivolumab treatment. The authors reported very promising results with mainly partial responses and stable disease after onset of treatment and one complete response. Only 2 patients had progressive disease and died. Overall survival was not reported. Single case reports described long-lasting complete responses of HCC patients under immunotherapy (Trojan and Sarrazin 2016).
While the checkmate trial included only patients with Child–Pugh stadium A (99%), our cohort involved 19 patients with cirrhosis Child–Pugh stage A at treatment start as well as 14 patients with advanced liver disease classified to stage B and one to stage C. 8 out of 19 Child-Pugh A patients (42%) had died at the time of final analysis and 11 out of 14 (79%) Child–Pugh B patients died.
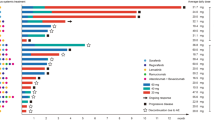
Median OS without treatment in BCLC stages is heterogeneous ranging from 9 to 18 months in BCLC B, 4–8 months in BCLC C and less than 3 months in BCLC D (Cabibbo et al. 2010). As real-life patients tend to be more heterogeneous than patients included in clinical trials, efficacy of new medications needs to be proven in these patients. Survival seems to be poor in patients in these advanced stages of cirrhosis and the benefit of nivolumab for overall survival in this subgroup of patients’ needs to be shown. Especially patients with advanced or decompensated cirrhosis (Child–Pugh stages B and C) are often excluded from trials. However, they are frequently treated in clinical routine. In our cohort, the treatment effect for these patients was limited with a median OS in Child A stage with 7 weeks (1–46) versus 3 weeks (0–14) in Child B stage, respectively. Accordingly, our multivariate analysis revealed Child–Pugh stage as an independent risk factor for survival, underlining that patients with advanced liver disease might not benefit from oncological treatment interventions since survival is determined by the liver function (Fig. 1) (Cabibbo et al. 2017). However, at this point, we cannot rule out a negative selection bias of patients due to the retrospective nature of this study. Just recently an interesting meta-analysis could show the increased efficacy of immunotherapy in male patients independently from other factors. Due to our small cohort and over-representation of male patients we could not find that difference (data not shown), however, this will probably be an important aspect when investigating real life patient cohort in the future (Conforti et al. 2018).
a Overall survival curve (Kaplan–Meier estimator) of patients treated with nivolumab. b Overall survival of patients with hepatocellular carcinoma stratified by BCLC stage (p = 0.126, by log-rank test). c Overall survival of patients with hepatocellular carcinoma stratified by Child–Pugh stage (p < 0.001, by log-rank test). d Overall survival of patients with hepatocellular carcinoma stratified by previous sorafenib treatment (p = 0.186, by log-rank test)
Adverse effects of immunotherapies are different from toxicities caused by “standard” chemotherapy. In a Phase 1 dose escalation trial of nivolumab in different tumor entities grade 3/4 toxicities (treatment-related) occurred in 14% of the patients, most problematic was pneumonitis, which was fatal in three cases (Topalian et al. 2012, 2014). Main side effects the clinician should be aware of are autoimmune phenomena. Increase of liver enzymes without clinical impairment (AST, ALT, even bilirubin) is a common side effect; however, immune-mediated hepatitis (defined as requirement of steroids and no alternate etiology) occurred in 1.1% in the trial. In our cohort, one patient showed hepatitis grade 3 that could effectively be treated with steroids. One other patient had to stop treatment due to bullous lichenoid drug-eruption. This is a rare, but known phenomenon attributable to nivolumab (Vence et al. 2017).
As seen in the clinical trials and previous reports from liver and other cancers, side effects of nivolumab in our cohort were manageable and overall nivolumab appears to be safe in HCC patients even with advanced liver disease. However, elevations in AST and ALT seem to occur more frequently in HCC patients and, therefore, a potential increased risk of liver toxicity has to be taken into account in clinical management (Brown et al. 2017).
There are limitations to this study. The study is of retrospective nature which could bias the patient selection, however, all patients treated with nivolumab at the respective centers were included during the given period of time. Patient’s outcome was assessed as the last contact to the center, not every patient was contacted by phone separately, so the survival may be slightly overestimated.
Taken together our real-life experience with nivolumab therapy in HCC patients confirms the safety of the treatment in patients with advanced HCC stages and even with reduced liver function. However, the prognosis of patients at more advanced stages of cirrhosis and impaired liver function remained very poor and the exact benefit of nivolumab treatment in this setting needs to be shown in the future.
Abbreviations
- ALBI:
-
Albumin–Bilirubin grade
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- CR:
-
Complete response
- CT:
-
Computed tomography
- CTCAE:
-
Common toxicity criteria
- BCLC:
-
Barcelona clinic liver cancer staging
- EMA:
-
European Medicines Agency
- FDA:
-
United States Food and Drug Administration
- HCC:
-
Hepatocellular carcinoma
- MELD:
-
Model of end-stage liver disease
- MRI:
-
Magnetic resonance imaging
- NASH:
-
Non-alcoholic steatohepatitis
- PD:
-
Progressive disease
- PD-1:
-
Programmed cell death protein 1
- PR:
-
Partial response
- OS:
-
Overall survival
- SD:
-
Stable disease
- TACE:
-
Transarterial chemoembolisation
- TKI:
-
Tyrosinkinase-inhibitor
References
Brahmer JR, Tykodi SS, Chow LQM, Hwu W-J, Topalian SL, Hwu P et al (2012) Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med 366(26):2455–2465. https://doi.org/10.1056/NEJMoa1200694
Brown ZJ, Heinrich B, Steinberg SM, Yu SJ, Greten TF (2017) Safety in treatment of hepatocellular carcinoma with immune checkpoint inhibitors as compared to melanoma and non-small cell lung cancer. J ImmunoTher Cancer 5(1):1–10. https://doi.org/10.1186/s40425-017-0298-2
Bruix J, Qin S, Merle P, Granito A, Huang Y-H, Bodoky G et al (2017) Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 389(10064):56–66. https://doi.org/10.1016/S0140-6736(16)32453-9
Cabibbo G, Enea M, Attanasio M, Bruix J, Craxí A, Camm̀a C (2010) A meta-analysis of survival rates of untreated patients in randomized clinical trials of hepatocellular carcinoma. Hepatology 51(4):1274–1283. https://doi.org/10.1002/hep.23485
Cabibbo G, Petta S, Barbara M, Attardo S, Bucci L, Farinati F et al (2017) Hepatic decompensation is the major driver of death in HCV-infected cirrhotic patients with successfully treated early hepatocellular carcinoma. J Hepatol 67(1):65–71. https://doi.org/10.1016/j.jhep.2017.01.033
Conforti F, Pala L, Bagnardi V, De Pas T, Martinetti M, Viale G et al (2018) Cancer immunotherapy efficacy and patients’ sex: a systematic review and meta-analysis. Lancet Oncol 19(6):737–746. https://doi.org/10.1016/S1470-2045(18)30261-4
El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C et al (2017) Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389(10088):2492–2502. https://doi.org/10.1016/S0140-6736(17)31046-2
El-Khoueiry AB, Melero I, Yau TC, Crocenzi TS, Kudo M, Hsu C et al (2018) Impact of antitumor activity on survival outcomes, and nonconventional benefit, with nivolumab (NIVO) in patients with advanced hepatocellular carcinoma (aHCC): Subanalyses of CheckMate-040. In: Abstract presented at the 2018 ASCO GI. https://meetinglibrary.asco.org/record/156075/abstract
El-Serag HB (2011) Hepatocellular carcinoma. N Engl J Med 365(12):1118–1127. https://doi.org/10.1056/NEJMra1001683
Feng D, Hui X, Shi-chun L, Yan-hua B, Li C, Xiao-hui L (2017) Initial experience of anti-PD1 therapy with nivolumab in advanced hepatocellular carcinoma. Oncotarget 8(57):96649–96655
Galle PR, Forner A, Llovet JM, Mazzaferro V, Piscaglia F, Raoul J-L et al (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. https://doi.org/10.1016/j.jhep.2018.03.019
He C, Mao Y, Lao X, Li S, Lin X (2018) Neutrophil-to-lymphocyte ratio predicts overall survival of patients with combined hepatocellular cholangiocarcinoma. Oncol Lett 15(4):4262–4268. https://doi.org/10.3892/ol.2018.7882
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL et al (2015) Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 33(6):550–558. https://doi.org/10.1200/JCO.2014.57.9151
Keir ME, Butte MJ, Freeman GJ, Sharpe AH (2008) PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol 26(1):677–704. https://doi.org/10.1146/annurev.immunol.26.021607.090331
Lencioni R, Llovet J (2010) Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 30(01):052–060. https://doi.org/10.1055/s-0030-1247132
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc J-F et al (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359(4):378–390. https://doi.org/10.1056/NEJMoa0708857
National Cancer Institute (NIH) Division of Cancer Treatment and Diangosis (DCTD) (2009) Common terminology criteria for adverse events (CTCAE) 4.0. https://evs.nci.nih.gov/ftp1/CTC/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf
Raoul J-L, Kudo M, Finn RS, Edeline J, Reig M, Galle PR (2018) Systemic therapy for intermediate and advanced hepatocellular carcinoma: sorafenib and beyond. Cancer Treat Rev 68:16–24. https://doi.org/10.1016/j.ctrv.2018.05.006
Sangro B, Melero I, Yau T, Hsu C, Kudo M, Kim T-Y et al (2017) Nivolumab in sorafenib-naive and experienced patients with advanced hepatocellular carcinoma (HCC): survival, hepatic safety, and biomarker assessments in CheckMate 040. Hepatology 66(S1):1–148. https://doi.org/10.1002/hep.29500
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF et al (2012) Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 366(26):2443–2454. https://doi.org/10.1056/NEJMoa1200690
Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH et al (2014) Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol 32(10):1020–1030. https://doi.org/10.1200/JCO.2013.53.0105
Trojan J, Sarrazin C (2016) Complete response of hepatocellular carcinoma in a patient with end-stage liver disease treated with nivolumab: whishful thinking or possible ? Am J Gastroenterol 111(8):1208–1209. https://doi.org/10.1038/ajg.2016.214
Vence L, Callen J, Burton S, Malone J (2017) Nivolumab-induced bullous lichenoid drug eruption. J Am Acad Dermatol 76(6):AB179. https://doi.org/10.1016/j.jaad.2017.04.697
Zhu AX, Galle PR, Kudo M, Finn RS, Qin S, Xu Y et al (2018) A study of ramucirumab (LY3009806) versus placebo in patients with hepatocellular carcinoma and elevated baseline alpha-fetoprotein (REACH-2). J Clin Oncol 36(4_suppl):TPS538–TPS538. https://doi.org/10.1200/JCO.2018.36.4_suppl.TPS538
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Fabian Finkelmeier received travel grants from AbbVie outside the submitted work. Carolin Czauderna has nothing to report. Lukas Perkhofer received travel grants from Ipsen, Bayer, Sanofi, Novartis outside the submitted work. Thomas J. Ettrich received travel grants from Ipsen outside the submitted work. He acted as consultant for Bayer, BMS, Sanofi, Merck Serono, Roche and Pfizer outside the submitted work. He received lecture fees from Merck Serono, Sanofi, Celgene. One of his research projects is supported by Shire. Jörg Trojan reports personal fees from Amgen, Bayer Healthcare, Bristol Myers-Squibb, Daichi Sankyo, Eisai, Ipsen, Merck Serono, Merck Sharp & Dome, Lilly ImClone, Roche, Shire and research grants from Roche. Arndt Weinmann has nothing to report. Jens Marquardt received honoraria from Roche and Bayer outside the submitted work. Johannes Vermehren reports personal fees from AbbVie, Gilead and MSD outside the submitted work. Oliver Waidmann received travel grants from Abbvie, Bayer, BMS, Gilead, Ipsen, Medac, Novartis, and Servier outside the submitted work. He acted as consultant for Amgen, Bayer, BMS, Celgene, Eisai, Merck, Novartis, Roche, Servier, Shire outside the submitted work. He received lecture fees from Bayer, BMS, Celgene, Ipsen, Novartis, Roche, and Shire.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (approval numbers: Mainz 837.199.10(7208), Frankfurt SGI-11-2017, Ulm 317/12, 230/14, 128/15).
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Finkelmeier, F., Czauderna, C., Perkhofer, L. et al. Feasibility and safety of nivolumab in advanced hepatocellular carcinoma: real-life experience from three German centers. J Cancer Res Clin Oncol 145, 253–259 (2019). https://doi.org/10.1007/s00432-018-2780-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-018-2780-8