Abstract
Introduction
The special types of breast cancer seem to have not only distinct morphological features but also distinct biological features.
Materials and methods
Women diagnosed with a first primary invasive breast cancer in the 2004–2005 period were identified through Tuscan Cancer Registry. Information on age, tumor size, lymph node status, histological type and grade, hormonal receptors, HER2 immunohistochemical expression were collected. Five subtypes were defined: luminal A, luminal B HER2+, luminal B HER2−, triple negative, and HER2 positive. The association between the histological type and molecular subgroups was assessed by a Fisher’s exact test, and a multinomial logistic regression model was used.
Results
Out of 1,487 patients, 34 % were luminal A subtype, 25 % luminal B HER2−, 11 % luminal B HER2+, 19 % triple negative, and 10.2 % HER2+; 58.5 % of cancers were ductal NOS types. With luminal A as reference, histological types distribution was significantly different between the subgroups. Mucinous, tubular, and cribriform histotypes were found among luminal A cancers more than in other subgroups; all medullary carcinomas were triple negative cancers. Pathological stage at diagnosis was more advanced, and histological grade was lower among subgroups other than luminal A.
Conclusions
Significant association between breast cancer histotypes and molecular subgroups was found.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive breast cancer is a heterogeneous disease in its presentation, pathological classification, and clinical course: female breast carcinomas are extremely different in clinical and histopathological features (Anderson et al. 2006).
These tumors can be categorized in several ways, according to histological type or according to molecular type based on expression of tumor markers. Up to 75 % of the diagnosed invasive carcinomas are defined as invasive ductal carcinoma, not otherwise specified (NOS). The 5–15 % of invasive carcinomas are represented by invasive lobular carcinoma; however, numerous other less common variants are defined by the WHO classification (Yerushalmi et al. 2009, Li et al. 2005, Lakhani et al. 2012). These special types of breast cancer display a distinct morphology and might exhibit a distinct prognostic and predictive profile from ductal carcinoma NOS.
Molecular subtyping has been developed based on the gene expression profiles of largely ductal carcinoma NOS and a few lobular breast cancer: some studies recently suggested an association between special types of breast cancers and distinct biological features (Weigelt and Reis-Filho 2009). However, the relative rarity of each special type makes molecular analysis difficult (Weigelt and Reis-Filho 2009) and whether it is useful to apply molecular classification to understand these rare tumors are unclear (Yerushalmi et al. 2009). Moreover, the molecular subclassification has been largely developed through studies based on ductal carcinoma NOS (Weigelt et al. 2008).
The aim of this study was to evaluate the correlation between histological type and molecular subgroups in a population-based series of female breast cancer patients.
Materials and methods
Women diagnosed with a first primary invasive breast cancer between January 2004 and December 2005 were identified through Tuscan Cancer Registry, a population-based cancer registry that collects all cancer cases diagnosed in residents in the provinces of Florence and Prato, central Italy, from 1985. Women whose cancers were not histologically confirmed were excluded. Information on age at diagnosis, tumor size, lymph node status, histological type, histological grade, pathological stage, immunohistochemical expression of hormonal receptors, ki-67, and HER2 were collected. A review of already existing pathology reports was made to collect information, for each case, on the percentage of positive cells for immunohistochemical estrogen (ER) and progesterone (PR) receptors expression, on the score for human epidermal growth factor 2 (HER2) and on proliferation index, through the Ki-67 expression. Moreover, data on HER2 fluorescence in situ hybridization (FISH) testing were also collected.
Ki-67 immunohistochemical expression was considered high, and ER and PR were categorized as positive in case of ≥14 and >1 % immunoreactive tumor cells were reported, respectively (Goldrisch et al. 2011). Tumors were considered positive for hormone receptors if found positive for at least one receptor.
HER2 expression was assessed through immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH) as previously described (Caldarella et al. 2011).
We evaluated the distribution of breast subtypes which have been identified to have different prognosis and different therapeutic response in morphologically similar breast cancer patients (Goldrisch et al. 2011); through immunohistochemical analysis currently reported in routine pathology reports, five subtypes of breast cancer were defined on the expression of ER or PR, HER2 and Ki67: luminal A if ER/PR+, low Ki67 and HER2−, luminal B (HER2 positive) if ER/PR+ and HER2+, luminal B (HER2 negative) if ER/PR+, high Ki67, and HER2−, triple negative if ER/PR– and HER2−, HER2 positive if ER/PR– and HER2+.
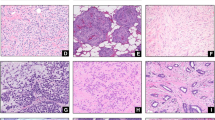
Tumor histotypes were coded using the International Classification of Diseases for Oncology (ICD-O) codes according to World Health Organization criteria (Fritz et al. 2000); they were categorized as ductal NOS, lobular, mixed, tubular, mucinous, cribriform, papillary, medullary, other rare histotypes (metaplastic, adenoid cystic, apocrine, neuroendocrine). Tumors were graded according to Elston-Ellis modification of the Bloom and Richardson grading system (Elston and Ellis 1991). All breast cancer patients were staged according to the TNM classification.
Clinicopathological characteristics of molecular subgroup as histological type, age (<50 and 50+ years), pathological T (T1-4, unknown) and N (N0-2, unknown), histological grade (G1, G2, G3, unknown), tumor size (<20, ≥20 mm, unknown) were compared to luminal A subgroup separately. p value is calculated using the chi-square test.
Multinomial logistic regression model including histological type (ductal NOS, lobular, mixed, mucinous, tubular, and other) (model a) and including histological type (ductal, lobular, mixed, mucinous, tubular, and other), age (<50 years, 50+ years), and size of tumor (<20, 20+ mm) (model b) was used to evaluate probability of each histological type of belonging to a specific molecular subtype.
Results
Out of the 1,984 women with first primary breast cancer collected by registry, 1,487 patients had available immunohistochemical results: 34.1 % were luminal A subtype, 25.2 % luminal B HER2−, 11.5 % luminal B HER2+, 19 % triple negative, and 10.2 % HER2+.
Invasive ductal carcinoma NOS was the most frequent histotype (58.6 % of total), followed by lobular (13.9 %), mixed (ductal and lobular or invasive ductal carcinoma NOS+ other histotype) (12.4 %), mucinous (3 %), tubular (2.9 %), and cribriform (2.6 %) types. Papillary (1.4 %) and medullary (0.3 %) carcinomas were very uncommon types.
Tumors were G1 (well differentiated) in 157 cases (11 % of total), G2 (moderately differentiated) in 513 (34 %), and G3 (poorly differentiated) in 308 (21 %). In 509 cases (34 %), information on histological grade was not available.
By age, most patients were 50 years older (77 %). About 60 % of cancer had tumor size smaller than 20 mm at diagnosis. About 25 % of patients had lymph node positive at diagnosis; however, for 40 % of the patients’ cases, the lymph node status was not available in the registry (Table 1).
With luminal A subgroup as reference, histological type and pathological stage at diagnosis distribution were significantly different between the subgroups. Ductal NOS was more frequent among subgroups other than luminal A, particularly when HER2+ subgroup was considered. Lobular, mucinous, tubular, and cribriform types were more represented among luminal A subgroup, while all medullary tumors were in the triple negative subgroup. No medullary was diagnosed in luminal A subgroup, and no tubular neither cribriform types were diagnosed in HER2+ subgroup.
Moreover, at diagnosis, the pathological T was more advanced, particularly for triple negative subgroup (p = 0.001), and lymph nodes were more frequently positive. G3 (poorly differentiated) histological grade was found, particularly when HER2+ subgroup was considered (p = 0.000).
A multinomial logistic regression model (Table 2, model a) showed that probability of belonging to luminal A subgroup was higher for special types than for ductal NOS cancer; when tumor size and age of patients were included, probability of belonging to luminal B HER2−, luminal B HER2+, triple negative, and HER2+ subgroups was higher for ductal NOS type and increased with increasing tumor size (Table 2, model b).
Discussion
The special types of breast cancer have not only distinct morphological features but also distinct clinical presentations and prognostic implications (Weigelt and Reis-Filho 2009).
They were recognized as other entities than ductal NOS carcinoma (Louwman et al. 2007), with differences in age at diagnosis, stage, histological grade. Moreover, differences between various histological types of breast cancer have been noted in previous studies: papillary and mucinous carcinoma frequency tend to increase with age, on the contrary medullary carcinoma frequency decreases (Li et al. 2005).
The question of whether molecular classification can be applied to special types of breast cancer and whether it can be useful to understand their clinical presentation and outcome has been recently investigated (Weigelt and Reis-Filho 2009). Few previous studies have evaluated differences in clinical and pathologic tumor characteristics by histological types; recently, the utility, for treatment decision, of identification of special types particularly in luminal breast cancer has been shown (Colleoni et al. 2012).
Our data from a population-based cancer registry found a significantly different distribution of special type according to molecular subtypes in invasive breast cancers. Compared to ductal carcinoma NOS, lobular, mucinous, tubular, and cribriform carcinomas often displayed a luminal phenotype, confirming data from literature which reported that lobular, mixed, and mucinous carcinomas have been shown to be more likely hormonal receptors positive compared to ductal carcinomas NOS (Li et al. 2005).
Many studies reported that tubular and cribriform tumors, which in our data were more frequent in luminal A and in luminal B HER2− subgroups, have excellent prognosis and are characterized by patterns of genetic aberrations found in G1 (low histological grade) luminal breast cancers (Yerushalmi et al. 2009, Weigelt et al. 2008, Colleoni et al. 2012). Some authors suggest that tubular and cribriform carcinomas are tumors with distinct morphological features but similar clinical presentation and natural history, with the same precursors and preinvasive lesions, representing a spectrum of lesions of a single family (Weigelt and Reis-Filho 2009; Colleoni et al. 2012). Immunohistochemical analysis showed for some histological special types similar protein expression patterns; this feature may suggest a common etiological background or the involvement of common genetic pathways during cancerogenesis (Weigelt et al. 2008). Moreover, recent studies suggested that several histological subtypes may not represent specific biological entities (Gruver et al. 2011).
Molecular and immunohistochemical analysis showed that each special type of breast cancer is composed of tumors that are more homogeneous than ductal NOS and lobular carcinomas, and it has been recently suggested that each histological special subtype pertained to only one molecular subtype (Weigelt et al. 2008).
We found that medullary carcinoma shows a triple negative phenotype. Medullary carcinomas, although cluster as poor prognosis triple negative tumor, are reported to be associated with a favorable outcome (Yerushalmi et al. 2009; Weigelt et al. 2008; Vu-Nishino et al. 2005; Vincent-Salomon et al. 2007; Metzger-Filho et al. 2012); however, the small number of patients could hamper studies on this type of breast cancer (Yerushalmi et al. 2009). Some authors recently underlined that prognosis among triple negative cancers varies according to histological type and suggested that triple negative cancers probably constitute a heterogeneous group of tumors (Metzger-Filho et al. 2012).
Our data found that luminal A cases tend to be diagnosed at a more early stage, particularly when compare to triple negative and HER2+ subtypes; histological grade, moreover, was found to be lower among HER2+ than among luminal A carcinomas. These results justify the well-known favorable prognosis of luminal subgroup (Caldarella et al. 2011). In our study, we did not analyze the outcome; however, we found that lobular type seems to belong more frequently to prognostically favorable molecular subgroups. In literature, conflicting results are reported on the outcome of lobular breast cancers: some studies reported a worse outcome and others a prognosis similar to ductal NOS cancers (Colleoni et al. 2012; Cristofanilli et al. 2005; Rakha et al. 2008). It is well known that lobular tumors are more difficult to detect with mammography compared to ductal NOS tumors (Li et al. 2005).The differences in biological characteristics observed by histological type may reflect the different etiologies of these tumors and may influence the utility of screening approaches to detect different histological types of cancer.
Recently, the role of histopathological evaluation in order to detect special types of cancer with particular regard to the need for adjuvant systemic treatment has been underlined. The response to neoadjuvant chemotherapy and the prognosis has been recently found varying for each histological type: a good prognosis for mucinous carcinoma was found, although the poor response to treatment (Nagao et al. 2012). Recently, it has been suggested that the identification of special types of breast cancer within the luminal subgroup should be considered in therapeutic algorithms (Li et al. 2005; Colleoni et al. 2012) and that molecular mechanism could represent targets for the development of individualized therapy (Simpson et al. 2010).
Because the limitation in sample size of rare histological types of breast cancer, further larger studies are needed to evaluate the impact of molecular characterization on histological classification system of breast cancer.
However, our data suggest that molecular and immunohistochemical analysis can be useful to refine the biological knowledge; an alliance of morphology with molecular analysis could improve the care of patients with breast cancer (Simpson et al. 2010; Schnitt 2010).
References
Anderson WF, Pfeiffer RM, Dores GM, Sherman ME (2006) Comparison of age distribution patterns for different histopathologic types of breast carcinoma. Cancer Epidemiol Biomarkers 15(10):1899–1905
Caldarella A, Crocetti E, Bianchi S, Vezzosi V, Urso C, Biancalani M, Zappa M (2011) Female breast cancer status according to ER, PR and HER2 expression: a population based analysis. Pathol Oncol Res 17(3):753–758
Colleoni M, Rotmensz N, Maisonneuve P, Mastropasqua MG, Luini A, Veronesi P, Intra M, Montagna E, Cancello G, Cardillo A, Mazza M, Perri G, Iorfida M, Pruneri G, Goldhirsch A, Viale G (2012) Outcome of special types of luminal breast cancer. Annals Oncol 23(6):1428–1436
Cristofanilli M, Gonzalez-Angulo A, Sneige N, Kau SW, Broglio K, Theriault RL, Valero V, Buzdar AU, Kuerer H, Buccholz TA, Hortobagyi GN (2005) Invasive lobular carcinoma classic type: response to primary chemotherapy and survival outcomes. J Clin Oncol 23(1):41–48
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow up. Histopathology 19:403–410
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S (2000) International classification of diseases for oncology, 3rd edn. World Health Organization, Geneva
Goldrisch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ, Panel members (2011) Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747
Gruver AM, Portier BP, Tubbs RR (2011) Molecualr pathology of breast cancer. Arch Pathol Lab Med 135:544–557
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ (2012) WHO classification of tumours, vol 4. IARC WHO Classification of Tumours, no 4
Li CI, Uribe DJ, Daling JR (2005) Clinical characteristics of different histologic types of breast cancer. Br J Cancer 93:1046–1052
Louwman MWJ, Vriezen M, van Beek MWPM, Tutein Nolthenius-Puylaert CBJE, van der Sangen MJC, Roumen RM, Kiemeney LALM, Coebergh JWW (2007) Uncommon breast tumors in perspective: incidence, treatment and survival in the Netherlands. Int J Cancer 121:127–135
Metzger-Filho O, Tutt A, de Azambuja E, Saini KS, Viale G, Loi S, Bradbury I, Bliss JM, Azim HA Jr, Di Leo A, Baselga J, Sotiriou C, Piccard-Gebhart M (2012) Dissecting the heterogeneity of triple-negative breast cancer. JCO 30:1879–1887
Nagao T, Kinoshita T, Hojo T, Tsuda K, Fujimara Y (2012) The differences in the histological types of breast cancer and the response to neoadjuvant chemotherapy: the relationship between the outcome and the clinicopathological characteristics. Breast 21(3):289–295
Rakha EA, El-Sayed ME, Powe DG, Green AR, Habashy H, Grainge MJ, Robertson JF, Blamey R, Gee J, Nicholson RI, Lee AH, Ellis IO (2008) Invasive lobular carcinoma of the breast: response to hormonal therapy and outcomes. Eur J Cancer 44:73–83
Schnitt SJ (2010) Classification and prognosis of invasive breast cancer: from morphology to molecular taxonomy. Mod Pathol 23:S60–S64
Simpson PT, Reis Filho JS, Lakhani SR (2010) Breast pathology: beyond morphology. Sem Diagn Pathol 27:91–96
Vincent-Salomon A, Gruel N, Lucchesi C, MacGrogan G, Dendale R, Sigal-Zafrani B, Longy M, Raynal V, Pierron G, de Mascarel I, Taris C, Stopp-Lyonnel D, Pierga JY, Salmon R, Sastre-Garau X, Fourquet A, Delattre O, de Cremoux P, Aurias A (2007) Identification of typical medullary breast carcinoma as a genomic sub-group of basal-like carcinomas, a heterogeneous new molecular entity. Breast Cancer Res 9(2):R24
Vu-Nishino H, Tavassoli FA, Ahrens WA, Haffty BG (2005) Clinicopathologic features and log-term outcome of patients with medullary breast carcinoma managed with breast-conserving therapy (BCT). Int J Radiat Oncol Biol Phys 62(4):1040–1047
Weigelt R, Reis-Filho JS (2009) Histological and molecular types of breast cancer: is there a unifying taxonomy? Nat Rev Clin Oncol 6(12):718–730
Weigelt B, Horlings HM, Kreike B, Hayes MM, Hauptmann M, Wessels LFA, de Jong D, Van de Vijver MJ, Van’t Veer LJ, Peterse JL (2008) Refinement of breast cancer classification by molecular characterization of histological special types. J Pathol 216:141–150
Yerushalmi R, Hayes MM, Gelmon KA (2009) Breast carcinoma-rare types: review of the literature. Annals Oncol 20:1763–1770
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caldarella, A., Buzzoni, C., Crocetti, E. et al. Invasive breast cancer: a significant correlation between histological types and molecular subgroups. J Cancer Res Clin Oncol 139, 617–623 (2013). https://doi.org/10.1007/s00432-012-1365-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-012-1365-1