Abstract
Objective
Purification and characterization of cancer stem cells (CSCs) can lead to the identification of targets for therapeutic interventions of cancer. With regard to gastric cancer, studies have not yet defined and characterized CSCs.
Methods
The expression of the cell surface markers CD44 and CD24 was examined in gastric cell lines AGS and gastric cancer tissues from five patients with fluorescence-activated cell sorting analysis (FACS). The tumorigenic properties, self-renewal, and differentiated progeny in the two distinct cell populations CD44+CD24+ and CD44−CD24− were identified in vivo serial transplantation and in vitro culture. Real-time RT-PCR was used to assess the expression of sonic hedgehog (SHH), patched 1 (PTCH1), and GLI3 signaling molecules in CD44+CD24+ and CD44−CD24− cells.
Results
As few as 200 CD44+CD24+ cells injected in NOD–SCID mice were able to generate tumors in 50% of mice (6 of 12), while tumors did not form in mice until at least 10,000 CD44−CD24− cells were injected, where only one of 12 mice formed a tumor, further verifying that CD44+CD24+ gastric cancer cells have the capacity to both self-renew and produce differentiated progeny. Moreover, SHH, PTCH1, and GLI3 mRNA expression increased significantly in the CD44+CD24+ subpopulation when compared with the CD44−CD24− subpopulation.
Conclusions
These studies strongly suggest that the CD44+CD24+ subpopulation of human gastric cancer cell lines, AGS, is gastric cancer stem cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the one of the most common cancers and the second leading cause of cancer-related death from cancer worldwide. It is estimated that about 700,000 people died of gastric cancer annually, and 42% of gastric cancer cases worldwide are recorded in China (Parkin et al. 2005). Significant advancements have been achieved over the past two decades in elucidating important molecular pathways that are involved in gastric carcinoma (Wu et al. 2009). However, these advancements have not improved the treatment of gastric cancer. Hence, the understanding of the mechanism underlying gastric carcinogenesis is essential for the management of gastric cancer.
Recent studies have shown that tumor cells are heterogeneous, but only cancer stem cells are able to proliferate extensively and form new tumors. These cells are termed cancer stem cells (CSCs). The existence of CSCs was first observed in hematopoietic malignancies by Dick et al, in 1997, and they found that rare subpopulations of cells within leukemia are able to generate leukemia in nonobese diabetic–severe combined immunodeficient (NOD–SCID) mice (Bonnet and Dick 1997), These cells displayed the cell surface marker phenotype of CD34+CD38− and have properties of self-renewal and multilineage differentiation along with potent proliferative capacity. The technique of sorting cells based on cell surface marker expression and assessing their ability to initiate tumor growth in immunocompromised mice was also applied to investigate any possible existence of solid-organ CSCs. Using these techniques, cancer stem cells have now been identified in several tumor types, including breast, brain, colon, prostate, head, neck, and liver cancers, melanoma, and multiple myeloma (Al-Hajj et al. 2003; Singh et al. 2004; O’Brien et al. 2007; Collins et al. 2005; Prince et al. 2007; Yang et al. 2008; Fang et al. 2005; Matsui et al. 2004).
Cancer stem cells in pancreatic cancer have been identified recently using a xenograft model in which primary human pancreatic adenocarcinomas were grown in immunocompromised mice. Tumorigenic subpopulation of pancreatic cancer cells expressing the cell surface markers CD44, CD24, and epithelial-specific antigen (ESA) has been identified (Li et al. 2007). Pancreatic cancer stem cells with the CD44+CD24+ESA+ phenotype had a significant increase in tumorigenic potential when compared with nontumorigenic cancer cells. The CD44+CD24+ESA+ pancreatic cancer cells showed stem cell properties of self-renewal.
Several studies have shown the presence of gastric CSCs in gastric cell line NUGC3, MKN1, MKN7, and MKN28, and the cancer stem cells (i.e., SP cells) are about 0.6–2.2% (Haraguchi et al. 2006). Yet, the growth characteristics and pathway signaling in the regulation of these stem cells currently remain unclear. Recently, CD44 was reported as a cell surface marker to identify gastric CSCs in gastric cancer cell lines. CD44+ cells formed spherical colonies in serum-free media in vitro and showed tumorigenic ability when injected into the stomach and skin of SCID mice in vivo. This supported that the CD44+ gastric cancer cells have the stem cell properties of self-regeneration and the ability to form differentiated progenies when compared with CD44− cells (Takaishi et al. 2009). Based on the above findings, we examined gastric cell lines AGS and human gastric tissue for the potential stem cell populations using multiple known stem cell markers. In AGS gastric cancer cell lines, cancer stem cell population expressing the CD44+CD24+ showed the properties of self-regeneration and the ability to produce differentiated progenies. Our data strongly suggest that the existence of gastric CSCs with CD44+CD24+ as a promising cell surface marker to be identified.
Materials and methods
Cell culture
Human gastric cancer cell lines AGS were purchased from American Type Culture Collection and cultured in DMEM (HyClone, Logan, UT), supplemented with 10% fetal bovine serum (FBS; HyClone, Logan, UT).
Preparation of the single-cell suspensions of tumor cells
Before digestion with collagenase, xenograft tumors or primary human tumors were cut up into small pieces with scissors and then minced completely using sterile scalpel blades. To obtain single-cell suspension, the resultant minced tumor pieces were mixed with ultrapure collagenase IV (Worthington Biochemicals, Freehold, NJ) in medium 199 (200 units of collagenase per ml) and allowed to incubate at 37°C for 2.5–3 h for enzymatic dissociation. The specimens were further mechanically dissociated every 15–20 min through pipetting with a 10-ml pipette. At the end of the incubation, cells were filtered through a 40-μm nylon mesh, washed with HBSS/20% fetal bovine serum (FBS), and finally washed twice with HBSS (Li et al. 2007).
Flow cytometry
Dissociated cells were counted and transferred to a 5-ml tube, then washed twice with HBSS containing 2% heat-inactivated FBS, and resuspended in HBSS with 2% FBS at the concentration of 106 per 100 μl Sandoglobin solution. The mix was then added to the sample at a dilution of 1:20, and then the sample was incubated on ice for 20 min. Finally, the sample was washed twice with HBSS/2% FBS and resuspended in HBSS/2% FBS. After adding antibodies, the sample was incubated on ice for 20 min and then washed twice with HBSS/2% FBS. When needed, a secondary antibody was added by resuspending the cells in HBSS/2%FBS followed by a 20-min incubation. After another washing, cells were resuspended in HBSS/2% FBS containing 4′,6-diamidino-2-phenylindole (DAPI; 1 μg/mL final concentration).The antibodies used were anti-CD44 allophycocyanin, anti-CD24 (phycoerythrin), anti-H2K (PharMingen, Franklin Lakes, NJ), and anti–ESA-FITC (Biomeda, Foster City, CA), each at a dilution of 1:40. In all experiments using human xenograft tissue, infiltrating mouse cells were eliminated by discarding H2K (mouse histocompatibility class I) cells during flow cytometry. Dead cells were excluded by using the viability dye DAPI. Flow cytometry was done using a FACSAria (BD Immunocytometry Systems, Franklin Lakes, NJ). Side scatter and forward scatter profiles were used to eliminate cell doublets. Cells were routinely sorted twice, and the cells were reanalyzed for purity, which typically was >97% (Li et al. 2007).
Sorted cell implantation into NOD/SCID mice
All studies were conducted in an AAALAC (Association for Assessment and Accreditation of Laboratory Animal Care International) accredited facility, in compliance with the US Public Health Service guidelines for the care and use of animals in research. Sorted cells were washed with serum-free HBSS after flow cytometry and suspended in serum-free RPMI/Matrigel mixture (1:1 volume) followed by injecting s.c. into the right and left midabdominal area of 6- to 8-week-old male NOD/SCID mice using a 23-gauge needle. Animals underwent autopsy at 3–6 weeks after cell implantation, and tumor growth was assessed. Tissues were fixed in formaldehyde and examined histologically.
Tumorsphere culture
Cells were suspended in serum-free culture medium DMEM containing 1% N2 supplement, 2% B27 supplement, 1% antibiotic–antimycotic (Invitrogen), 10 ng/ml human FGF-2 (Sigma, Saint Louis, MO), and 20 ng/ml EGF (Invitrogen) and then plated in 48-well ultra-low attachment plates (Corning, Corning, NY) at 100 cells per well. Seven to ten days later, plates were quantified using an inverted microscope (Olympus) at 100×, 200×, and 400× magnification. For subsequent quantification of cell numbers per tumorsphere, tumorspheres were collected and filtered through a 40-μm sieve (BD Biosciences, San Jose, CA) and disassociated with 2.5% trypsin, while the viable cells were counted with trypan blue exclusion.
RNA extraction and analysis of Hh signaling components expression in gastric tumor stem cells
Total RNA from these cells was collected using an RNeasy Mini Kit (Qiagen, Valencia, CA) according to the manufacturer’s protocol followed by DNAse treatment and RNA clean-up (RNeasy Mini Kit; Qiagen, Valencia, CA, USA). RNA concentration and integrity were determined using the RNA 6000 Nano LabChip Kit (Qiagen) on Agilent 2100 Bioanalyzer. The mRNA levels of SHH, PTCH1, and GLI3 genes were quantitated by real-time PCR. Primers were designed by using an optimization program (Lasergene 6; DNAStar, Madison, WI). RNA (250–500 ng) was reverse-transcribed using the First Strand Synthesis Kit (Qiagen), and cDNA was subjected to real-time PCR using SYBR green/ROX Master Mix (Qiagen). Real-time PCR (RT-PCR) was performed using a Rotor-Gene 6000 (Corbett Life Science, Sydney, Australia), and β-actin was used as an internal control for normalization. Fold changes of target genes were calculated using comparative quantification of β-actin. Results were analyzed using Rotor-Gene 6000 Software.
Statistical analysis
Data are reported as mean ± standard deviation (SD). Results were analyzed using t test for comparison of two means. The chi square test was used for categorical data (Prism software; GraphPad Software, Inc., San Diego, CA). A value of P < 0.05 was considered to be statistically significant.
Results
Expression of CD44 and CD24 from cells derived from gastric cancer lines AGS, and gastric cancer tissues
To evaluate the possibility of the expression of candidate cell surface markers as gastric CSCs, putative stem cell markers (CD184, CD44, CD24, CD133, CD163, ESA, etc.) were used to screen the cell surface marker of gastric CSCs by fluorescence-activated cell sorting analysis. Expression of CD44 and CD24 was only positive in AGS gastric cancer lines; the expression of other multiple putative stem cell markers was negative. The percentage of cells with CD44+ and CD24+ was 4–15% and 5–13%, respectively (Fig. 1a, b), and the percentage of cells with CD44 and CD24 markers is 1.8–6.3% (Fig. 2). Because the properties of cell lines adapted to long-term growth in vitro can differ from those of tumors growing in vivo, the expression of cell surface markers in the cancer cell line may be distinct from primary gastric adenocarcinoma cells. We also investigated the expression of CD44, CD24, and epithelial-specific antigen (ESA) in fresh human primary gastric adenocarcinoma tissues; our results showed that subpopulation of gastric cancer cells expressing the cell surface markers CD44, CD24, and epithelial-specific antigen (ESA) was 29.69, 23.28, and 45.93%, respectively (Fig. 3).
Expression of putative stem cell markers from cells derived from gastric cancer lines AGS by fluorescence-activated cell sorting (FACS) analysis. a, b Expression of cell surface markers CD44 and CD24 in AGS gastric cancer lines was shown (top left and right, respectively). The percentage of cells with CD44+ and CD24+ was 4–15% and 5–13%, respectively. One of more than three independent experiments is shown here
Tumor-initiating capacity of cells bearing stem cell markers
To determine whether cells expressing distinct cancer stem cell markers are tumorigenic in vivo, two populations were purified by FACS and injected back into the skin and stomach of the NOD/SCID mice (Fig. 4a, b). The results showed a substantial difference in tumorigenic properties. Tumors frequently arose on the injection of 200–500 CD44+CD24+ gastric cancer cells, whereas 104 CD44−CD24− cells consistently only one out of the 12 mice form tumors (Table 1). Most importantly, tumors grown from CD44+CD24+ cells maintained a differentiated phenotype while reproduced the morphologic and phenotypic heterogeneity of human gastric adenocarcinoma lesions, formation of epithelial gland-like structures. Moreover, when analyzed by flow cytometry, it contained both CD44+CD24+ and CD44−CD24− populations in proportions similar to those of their parent gastric cancer cell. Taken together, these observations suggested that in human gastric cancer cell line xenografts, a population with stem cell–like properties can be reproducibly and consistently isolated based on CD24 and CD44. Further assessment of the capacity of generating differentiated progeny of CD44+CD24+ human gastric cancer cells was verified by histology method. Hematoxylin and eosin staining (H&E) of tumors originated from CD44+CD24+ cells showed epithelial cancer cells, which were remarkably similar to the appearance of the human gastric tumor (Fig. 5).
a Tumor formation in nonobese diabetic–severe combined immuno deficient mice injected with gastric cancer stem cells. CD44+CD24+ cells and CD44−CD24− cells were isolated by flow cytometry as described and assayed for the ability to form tumors after injecting subcutaneously into the NOD/SCID mice (n = 12) at 200, 500, 103, 5,000, and 104 cells per injection. Mice were examined for tumor formation by palpation and subsequent autopsy. The analysis was completed 16 weeks following injection. Data are expressed as number of tumors formed/number of injections. b Orthotopic in NOD/SCID mice after 2 weeks. Gastric tumor formation in NOD–SCID mice injected with gastric cancer stem cells. Implantation of 200 CD44+CD24+ gastric CSCs resulted in the tumor formation
Tumoroid spheres formation in CD44+CD24+ cells isolated from gastric cancer cell lines
Since tumorsphere culture has been widely used to assess the self-renewal potential of stem cells and cancer stem cells (Yu et al. 2007; Dontu et al. 2004; Phillips et al. 2006; Liu et al. 2006), in the current study, we employed tumorsphere culture to explore the CD44+CD24+ and CD44−CD24− subpopulations from human gastric cancer cell lines AGS produced spheroid colonies after in vitro culture for 3–4 weeks in serum-free media under nonadherent conditions. CD44+CD24+ cells showed spherical colony formation (Fig. 6a), while CD44−CD24− gastric cancer cells formed few colonies (Fig. 6b). Then, we cultured FACS-sorted CD44+CD24+ and CD44−CD24− populations separately with the regular medium of DMEM supplemented with 10% FBS in the regular cell culture plates. After a few weeks of culture, the CD44+CD24+ populations contain not only CD44+CD24+ but also CD44−CD24− subpopulations, whereas CD44−CD24− populations only have CD44−CD24− subpopulations. This suggested that the CD44+CD24+ populations have multipotential differentiation capability in in vitro culture.
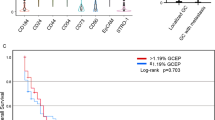
The expression of Hh signaling components mRNA in CD44+CD24+ gastric cancer cells and CD44−CD24− cells isolated from gastric cancer cell lines AGS
It has been reported that hedgehog signaling pathway is involved in the regulation of self-renewal of multiple solid-organ cancer stem cells (Liu et al. 2006; Hatsell and Frost 2007). To evaluate whether upregulation of molecules is important in self-renewal pathways in gastric CSCs, real-time reverse transcription-polymerase chain reaction was used to investigate the expression of Hh signaling molecules in CD44+CD24+ gastric cancer cells and CD44−CD24− cells isolated from gastric cancer cell lines. We found that the SHH, PTCH1, and GLI3 mRNA expression increased significantly in CD44+CD24+ subpopulation when compared with CD44−CD24− subpopulation. Noticeably, the SHH transcript was elevated ninefold in CD44+CD24+ gastric cancer cells, when compared with CD44−CD24− nontumorigenic gastric cancer cells (Fig. 7).
The upregulation of the expression of Hh signaling molecules SHH, PTCH1, and GLI3 mRNA in gastric CSCs. The expression of SHH, PTCH1, and GLI3 mRNA in total gastric cancer cells was quantitated by real-time RT-PCR. Data are expressed as the mean ± SD. *P < 0.05, comparing CD44−CD24− with CD44+CD24+ cells
Discussion
Cancer stem cells in human gastric cancer cell lines were identified in this study. We found that CD44+CD24+ cells comprised 1.8–6.3% of human gastric cancer cells. These cells have been shown to define a highly tumorigenic cancer cell population in gastric cancer cells with properties of self-regeneration and multilineage differentiation. Just 200 CD44+CD24+ cells injected in NOD–SCID mice were enough to generate tumors in 50% of mice (six of 12), while tumors did not form in mice until at least 10,000 CD44−CD24− cells were injected, where only one of 12 mice formed a tumor, reflecting at least a 50-fold greater tumor-initiating potential. In vitro study demonstrated that CD44+CD24+ cells showed spherical colony formation in serum-free conditions, while CD44−CD24− gastric cancer cells formed few or no colonies. Our data strongly suggest that CD44+CD24+ cells are defined as putative cancer stem cells in human gastric cancer cell lines AGS.
Former studies suggested that several stem cell markers, such as CD133, may be shared by cancer stem cells in different tumor types; in human brain tumors, prostate cancer, and colon cancer, expression of CD133+ defined a subpopulation of cancer cells with high tumorigenic potential (Singh et al. 2004; O’Brien et al. 2007; Collins et al. 2005); this indicated that the same cell marker can act as a CSC marker in multitype human cancer. Based on our former studies in pancreatic cancer, in which CD44+CD24+ESA+ cells were identified as putative cancer stem cells (Li et al. 2007), CD44 and CD24 markers were used to identify gastric cancer stem sells in AGS cell line. We found that the expression of CD44 and CD24 was only positive in AGS gastric cancer lines. No other putative stem cell markers were found in gastric CSCs.
In tumor tissues, a significant CD44 is an adhesion molecule that regulates cell proliferation, migration, and invasion, through interacting with its ligands, heparanase, and hyaluronan, and thus plays an important role in tumor progression and metastasis (Hsu et al. 2007). CD24 may regulate cell adhesion by downregulation of CXCR4, an important receptor in stem cell homing and tumor metastasis (Charafe-Jauffret et al. 2008). Previous studies have shown that gastric cancer stem cells express the cell surface marker CD44 and represent 0.5–1.0% of all gastric cancer cells (Takaishi et al. 2009). Along with the properties of self-renewal and multilineage differentiation, CD44+ cells also have been shown to define a highly tumorigenic cancer cell population in prostate cancer cells with stem cell–like characteristics (Collins et al. 2005). Our study of human gastric cancer cell lines AGS has revealed a CD44+CD24+ subpopulation of cancer cells that possess the characteristics of CSCs. Our finding suggests that more than one set of specific cell surface markers may exist for gastric cancer stem cell populations. To identify gastric cancer stem cell, a more distinguishing expression marker or set of markers may yet need to be discovered.
We also investigated the expression of CD44 and CD24 in fresh human gastric adenocarcinoma cells. Our preliminary results showed that the percentage of cells with CD44+ and CD24+ in fresh gastric cancer cells was 29.69 ± 2.32% and 23.28 ± 2.15%, respectively. These results could help to further isolate gastric cancer stem cells from the human gastric adenocarcinoma tissue.
Self-renewal and differentiation potential are the features of stem cells. CSCs can both self-renew and produce differentiated progeny like normal stem cells. Normal stem cells’ self-renewal signaling pathways that have been implicated in solid-organ malignancies include Notch, Wnt/β-catenin, phosphatase and tensin homologue deleted from chromosome 10, sonic hedgehog (SHH), and BMI-1 (Yu et al. 2007; Dontu et al. 2004; Phillips et al. 2006; Liu et al. 2006). Several reports have shown that hedgehog signaling is important for the maintenance of cancer stem cells and the proliferation of tissue progenitor cells (Watkins et al. 2003; Peacock et al. 2007; Karhadkar et al. 2004). It has been reported that SHH signaling plays an important role in the progression of gastric cancer. The activation of the hedgehog pathway was increased in human gastric adenocarcinomas and gastric cancer precursor; inhibition of hedgehog signaling by cyclopamine inhibited gastric cancer growth both in vitro and in vivo, suggesting that this signaling pathway has an early and critical role in gastric cancer development (Ma et al. 2005; Katoh and Katoh 2005; Lee et al. 2007). To assess whether upregulation of molecules is important in self-renewal pathways in gastric CSCs, we performed real-time reverse transcription-polymerase chain reaction to assess the expression of developmental signaling molecules. We observed that the SHH transcript was elevated ninefold in CD44+CD24+ gastric cancer cells when compared with CD44−CD24− nontumorigenic gastric cancer cells. These data suggested that there is a significant upregulation of SHH expression in gastric CSCs.
Our results showed that CSCs exist in AGS cell lines. These cells were discriminated by the expression of CD44 and CD24 markers and displayed the properties of self-renewal and multilineage differentiation along with potent proliferative capacity because these cells drive tumor development. Thus, further identification of the signaling pathways that regulate the key properties of self-renewal and differentiation of the gastric CSCs will ultimately aid in designing strategies to target this population; this may lead to more effective therapies for gastric cancer.
References
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF (2003) Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA 100:3983–3988
Bonnet D, Dick JE (1997) Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med 3:730–737
Charafe-Jauffret E, Monville F, Ginestier C, Dontu G, Birnbaum D, Wicha MS (2008) Cancer stem cells in breast: current opinion and future challenges. Pathobiology 75:75–84
Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ (2005) Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res 65:10946–10951
Dontu G, Jackson KW, McNicholas E, Kawamura MJ, Abdallah WM, Wicha MS (2004) Role of Notch signaling in cell-fate determination of human mammary stem/progenitor cells. Breast Cancer Res 6:R605–R615
Fang D, Nguyen TK, Leishear K, Finko R, Kulp AN, Hotz S et al (2005) A tumorigenic subpopulation with stem cell properties in melanomas. Cancer Res 65:9328–9337
Haraguchi N, Utsunomiya T, Inoue H, Tanaka F, Mimori K, Barnard GF, Mori M (2006) Characterization of a side population of cancer cells from human gastrointestinal system. Stem Cells 24:506–513
Hatsell S, Frost AR (2007) Hedgehog signaling in mammary gland development and breast cancer. J Mammary Gland Biol Neoplasia 129:163–173
Hsu KH, Tsai HW, Shan YS, Lin PW (2007) Significance of CD44 expression in gastrointestinal stromal tumors in relation to disease progression and survival. World J Surg 31:1438–1444
Karhadkar SS, Bova GS, Abdallah N, Dhara S et al (2004) Hedgehog signalling in prostate regeneration, neoplasia and metastasis. Nature 431:707–712
Katoh Y, Katoh M (2005) Hedgehog signaling pathway and gastric cancer. Cancer Biol Therapy 4:1050–1054
Lee SY, Han HS, Lee KY, Hwang TS et al (2007) Sonic hedgehog expression in gastric cancer and gastric adenoma. Oncol Rep 17:1051–1055
Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, Wicha M, Clarke MF, Simeone DM (2007) Identification of pancreatic cancer stem cells. Cancer Res 67:1030–1037
Liu S, Dontu G, Mantle ID, Patel S, Ahn NS, Jackson KW, Suri P, Wicha MS (2006) Hedgehog signaling and Bmi-1 regulate self-renewal of normal and malignant human mammary stem cells. Cancer Res 66:6063–6071
Ma X, Chen K, Huang S, Zhang X, Adegboyega PA et al (2005) Frequent activation of the hedgehog pathway in advanced gastric adenocarcinomas. Carcinogenesis 26:1698–1705
Matsui W, Huff CA, Wang Q, Malehorn MT, Barber J, Tanhehco Y, Smith BD, Civin CI, Jones RJ (2004) Characterization of clonogenic multiple myeloma cells. Blood 103:2332–2336
O’Brien CA, Pollett A, Gallinger S, Dick JE (2007) A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature 445:106–110
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Peacock CD, Wang Q, Gesell GS et al (2007) Hedgehog signaling maintains a tumor stem cell compartment in multiple myeloma. Proc Natl Acad Sci USA 104:4048–4053
Phillips TM, McBride WH, Pajonk F (2006) The response of CD24(-/low)/CD44+ breast cancer-initiating cells to radiation. J Natl Cancer Inst 98:1777–1785
Prince ME, Sivanandan R, Kaczorowski A, Wolf GT, Kaplan MJ, Dalerba P et al (2007) Identification of a subpopulation of cells with cancer stem cell properties in head and neck squamous cell carcinoma. Proc Natl Acad Sci USA 104:973–978
Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB (2004) Identification of human brain tumour initiating cells. Nature 432:396–401
Takaishi S, Okumura T, Tu S, Wang SS, Shibata W, Vigneshwaran R, Gordon SA, Shimada Y, Wang TC (2009) Identification of gastric cancer stem cells using the cell surface marker CD44. Stem Cells 27:1006–1020
Watkins DN, Berman DM, Burkholder SG, Wang B, Beachy PA, Baylin SB (2003) Hedgehog signalling within airway epithelial progenitors and in small-cell lung cancer. Nature 422:313–317
Wu K, Nie Y, Guo C, Chen Y, Ding J, Fan D (2009) Molecular basis of therapeutic approaches to gastric cancer. J Gastroenterol Hepatol 24:37–41
Yang ZF, Ho DW, Ng MN, Lau CK, Yu WC, Ngai P et al (2008) Significance of CD90+ cancer stem cells in human liver cancer. Cancer Cell 13:153–166
Yu F, Yao H, Zhu P, Zhang X, Pan Q, Gong C, Huang Y, Hu X, Su F, Lieberman J, Song E (2007) let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell 131:1109–1123
Acknowledgments
This research was supported by grants from National Natural Science Foundation of China No. 81071978 (to C-J.Z) and No. 30973113 (to H.Y), Chongqing Science & Technology Commission Project No. 2009BB5017 (to C-J.Z), and Natural Science Foundation of Third Military Medical University No. 2009XHG12 (to C-J. Z).
Conflict of interest
The authors do not have any conflicts of interest to report with for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, C., Li, C., He, F. et al. Identification of CD44+CD24+ gastric cancer stem cells. J Cancer Res Clin Oncol 137, 1679–1686 (2011). https://doi.org/10.1007/s00432-011-1038-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-011-1038-5