Abstract
Purpose
We performed a meta-analysis of three sub-studies of the randomized Tamoxifen Exemestane Adjuvant Multinational (TEAM) trial to determine the effects of exemestane and tamoxifen on bone health.
Methods
Patients received exemestane or tamoxifen as adjuvant therapy for hormone receptor–positive breast cancer. Bone mineral density (BMD) was assessed at baseline and after 12 and 24 months of treatment. Bone turnover markers were also measured.
Results
Patients receiving tamoxifen showed a mean increase from baseline in lumbar spine BMD of 1.2% at month 12 and 0.2% at month 24. Patients receiving exemestane showed a mean decrease from baseline of 2.6% after 12 months and 3.5% after 24 months. There were significant differences in the changes in lumbar spine BMD between treatment groups (P < 0.0001 at both time points). Changes in BMD from baseline at the total hip were also significantly different between exemestane and tamoxifen (P < 0.05 at both time points). Bone turnover markers decreased from baseline with tamoxifen and increased with exemestane.
Conclusions
Exemestane resulted in decreases in BMD and increases in bone turnover markers. BMD increased and bone turnover markers decreased with tamoxifen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tamoxifen is an established adjuvant endocrine treatment for postmenopausal women with hormone receptor–positive breast cancer. The third-generation aromatase inhibitors (AIs), anastrozole, exemestane, and letrozole, have demonstrated superior efficacy as adjuvant therapy compared with tamoxifen in several clinical trials (Coates et al. 2007; Coombes et al. 2007; Forbes et al. 2008) and are now recognized options in this setting (Goldhirsch et al. 2009; National Comprehensive Cancer Network 2009).
The AIs exhibit a tolerability profile distinct from that of tamoxifen, with a lower incidence of gynecological adverse events, thromboembolic events, and endometrial cancer (Coates et al. 2007; Coombes et al. 2007; Forbes et al. 2008; Hadji 2008b). However, while tamoxifen has demonstrated a positive effect on the bone health of postmenopausal women (Love et al. 1992), AI treatment has been associated with a decrease in bone mineral density (BMD) and an increased risk of fracture and osteoporosis (Coates et al. 2007; Coombes et al. 2007; Forbes et al. 2008; Hadji 2007; Hadji and Bundred 2007). This impact on bone is likely to be an indirect consequence of the estrogen-depriving mechanism of action of AIs: estrogen withdrawal favors increased osteoclastic activity and bone resorption (Frenkel et al. 2010).
The efficacy and safety of exemestane for the adjuvant treatment of postmenopausal hormone receptor–positive breast cancer was investigated in the Tamoxifen Exemestane Adjuvant Multinational (TEAM) trial (Jones et al. 2008b). In this large, multinational, phase III, open-label trial, 9,775 postmenopausal patients with hormone receptor–positive breast cancer were randomized to receive 5 years’ exemestane or 2.5–3 years’ tamoxifen followed by 2–2.5 years’ exemestane (Jones et al. 2008b). TEAM was originally designed to investigate 5 years’ exemestane versus 5 years’ tamoxifen. However, the study design was amended following the interim results of the Intergroup Exemestane Study (IES), which showed that switching to exemestane after 2–3 years of tamoxifen improved disease-free survival (DFS) versus continuing tamoxifen (Coombes et al. 2004); subsequent follow-up analyses confirmed that the benefits of exemestane versus tamoxifen are maintained up to more than 5 years post-treatment (Coombes et al. 2009).
In the first analysis of TEAM, a head-to-head comparison of exemestane and tamoxifen after 2.75 years, exemestane was associated with an improvement in DFS compared with tamoxifen (HR 0.89; P = 0.12) and significant improvements in relapse-free survival (HR 0.85; P = 0.02) and time to distant metastases (HR 0.81; P < 0.02) (Jones et al. 2008b). Exemestane was associated with a significant increase in the incidence of osteoporosis, but not fractures, versus tamoxifen (Jones et al. 2008b). At a median follow-up of 5.1 years, TEAM showed no significant differences in efficacy between 5 years’ exemestane and the sequence of tamoxifen followed by exemestane (Rea et al. 2009). Upfront exemestane was associated with a significant increase in osteoporosis, arthralgia, and fractures versus sequential treatment (Rea et al. 2009). Sub-studies of TEAM were conducted to determine the effects of exemestane and tamoxifen on bone health in the United States (Jones et al. 2008a), Germany (Hadji et al. 2009a, b), and the Netherlands/Belgium (van Nes et al. 2008). To increase sample size and power, we performed a meta-analysis of these three sub-studies to determine the effects of exemestane and tamoxifen on BMD and markers of bone turnover after 12 and 24 months of treatment in the TEAM trial.
Methods
The TEAM trial was conducted in compliance with the Declaration of Helsinki and was approved by local ethics committees. All patients provided informed consent.
Study design
These were sub-studies of the randomized, open-label, multicenter TEAM trial, designed to assess the effects of exemestane and tamoxifen on BMD, with or without markers of bone turnover, in postmenopausal women with hormone receptor–positive breast cancer. Methodologies for each sub-study have been reported previously (Hadji et al. 2009a; Jones et al. 2008a; van Nes et al. 2008).
Patients received exemestane for 5 years or tamoxifen for 2.5–3 years followed by 2–2.5 years of exemestane, for a total of 5 years’ endocrine therapy. Patients were assessed for the first 2 years in these bone sub-studies.
Patients
Postmenopausal women with stages I, IIA, IIB, and IIIA T1–3, N0–2, M0, estrogen receptor (ER)-positive and/or progesterone (PR)-positive breast cancer who were candidates for adjuvant endocrine therapy were eligible. All patients were required to have completed primary surgery and/or radiotherapy and/or chemotherapy, if indicated, in accordance with local guidelines. Patients were also required to have adequate renal, hepatic, and hematological function and an Eastern Cooperative Oncology Group performance status 0–2 (van Nes et al. 2010).
Exclusion criteria included one of the following: inflammatory breast cancer, histologically positive supraclavicular nodes, local skin ulceration/infiltration, neoadjuvant chemotherapy, ER- and PR-negative primary tumor or ER/PR-unknown status, or evidence of distant metastasis. Patients were ineligible if they were receiving hormonal adjuvant therapy for prior breast cancer. Patients with uncontrolled cardiac disease, other significant malignancies within the past 3 years, or other serious illnesses were excluded. Patients with diseases requiring chronic intake of drugs that interfere with bone metabolism (e.g., glucocorticosteroids, antiepileptics, bisphosphonates, calcitonin, fluoride, vitamin K antagonists) or metabolic diseases affecting bone metabolism and/or requiring treatment (e.g., primary hyperparathyroidism) were also excluded.
Treatment
Patients received oral treatment with exemestane 25 mg/day or tamoxifen 20 mg/day. Dose modification, escalation, or reduction was not permitted. Treatment was discontinued if the patient withdrew consent, if the investigator considered it was medically necessary, or if there was unacceptable toxicity or relapse of disease. Patients were withdrawn from the bone sub-study if they had a fracture or developed osteoporosis (T-score less than −2.5). All patients were followed up for survival regardless of whether they discontinued treatment prematurely. To document treatment compliance in the US and German sub-studies, patients completed a ‘Drug Administration Record’ at home, which was brought to each clinic visit.
Assessments
Bone mineral density
BMD was measured by dual-energy X-ray absorptiometry (DXA) imaging at the lumbar spine (L1–L4) and total hip (g/cm2 and standardized as T- and Z-scores; Z-scores were not available from the US sub-study) in accordance with the standard operating procedure of the manufacturer. BMD measurements were recorded at baseline. Subsequent measurements were taken 12 and 24 months after treatment initiation with exemestane or tamoxifen.
Markers of bone turnover
Bone turnover markers were assessed in the sub-studies performed in Germany and the Netherlands/Belgium and included the bone formation marker amino terminal propeptide of type I procollagen (PINP) and the bone resorption markers.
C-telopeptide (CTx; the Netherlands/Belgium) and ICTP (carboxyterminal crosslinked telopeptide of type I collagen; Germany). Blood samples (20 mL) were taken at baseline and after 3, 6, 12, and 24 months of treatment. Details of assessments of bone turnover markers have been reported previously (Hadji et al. 2009b).
Primary objective
The primary objective was to compare exemestane and tamoxifen with regard to changes from baseline to months 12 and 24 in BMD (g/cm2) in lumbar spine (integral of L1–L4).
Secondary objectives
Secondary objectives included the comparison of exemestane and tamoxifen with regard to changes from baseline to months 12 and 24 in standardized BMD (T- and Z-scores) in lumbar spine (integral L1–L4) and BMD (g/cm2 and standardized as T- and Z-scores) in total hip. Mean changes from baseline to months 3, 6, 12, and 24 in the markers of bone turnover were also assessed.
Statistical analysis
As this was an analysis of pooled data, a sample size calculation was not indicated. The pooled analysis was performed on patients from the US, German, and Netherlands/Belgium sub-studies. In the US sub-study, only patients who were fully compliant with adjuvant endocrine therapy and had BMD measurements at all time points were included in the analysis. The German and Netherlands/Belgium sub-studies included all patients who had a baseline assessment and at least one post-baseline measurement of BMD or bone turnover (Fig. 1). Patients were analyzed as randomized, irrespective of the treatment actually received.
The analysis was based on observed cases (missing values were not imputed) and covered the period until the visit at month 24 (i.e., before the patients receiving tamoxifen switched to exemestane). All statistical modeling of treatment effects and other possible effects on the target variables was considered exploratory. Consequently, P-values associated with the respective models were not adjusted for multiple testing. All tests were performed two-sided at a significance level of 0.05. Baseline comparability in terms of BMD and bone turnover variables was assessed by analysis of variance (ANOVA) using the baseline value as a dependent variable, and treatment, sub-study and the interaction between treatment and sub-study as model terms. Baseline comparability in terms of demographic variables was also assessed by ANOVA. Baseline comparability in terms of clinical baseline characteristics was assessed by the Cochran–Mantel–Haenszel test. Differences in changes from baseline to the specific time point between exemestane and tamoxifen were assessed by analysis of covariance using the absolute values of the parameter, with treatment, sub-study, and the interaction between treatment and sub-study as model terms and the baseline value as a covariate. All data were analyzed using the Statistical Analysis System, version 9.1.3.
Results
Patient characteristics
In total, data from 412 patients were available for this analysis: 212 patients in the tamoxifen group and 200 in the exemestane group (Fig. 1; Table 1).
In general, the treatment groups were balanced with respect to demographics and baseline characteristics in all three sub-studies (except for weight in the Netherlands/Belgium sub-study; P = 0.0299; Table 1). Chemotherapy rates varied across sub-studies; however, there was no difference in chemotherapy rates between treatment groups in the pooled data. Furthermore, there were no significant differences in the baseline values of BMD (Table 2) or bone turnover markers (Table 3) between treatment groups.
Between sub-studies, significant differences in age (P = 0.0059), tumor stage (P = 0.0002), and the number of positive lymph nodes (P < 0.0001) were observed. There were also significant between-study differences in the baseline values of BMD (Table 2), except for L1–L4 [Z-score].
Primary objective
Across all sub-studies, patients in the tamoxifen group experienced a mean increase in the lumbar spine BMD of 1.2% from baseline to month 12 and 0.2% to month 24. Patients in the exemestane group showed a decrease from baseline of 2.6% after 12 months and 3.5% after 24 months (absolute values are shown in Table 2; mean changes from baseline are illustrated in Fig. 2a). The differences in the changes from baseline to months 12 and 24 between treatment groups were statistically significant (each treatment comparison P < 0.0001). Similar results were obtained in the analyses of individual sub-studies (all treatment comparisons P < 0.01).
Secondary objectives
Standardized BMD measurements in lumbar spine
Changes from baseline in standardized BMD measurements in lumbar spine revealed a similar pattern. Patients receiving tamoxifen had an increase in mean lumbar spine T-score from −0.34 to −0.21 after 12 months and to −0.24 after 24 months. In contrast, patients receiving exemestane showed a decrease from −0.59 to −0.79 after 12 months, remaining at −0.79 after 24 months (each treatment comparison P < 0.0001; Table 2 and Fig. 2b). Patients in the tamoxifen group showed an increase in mean lumbar spine Z-score from 0.59 to 0.76 after 12 months and to 0.81 after 24 months, whereas patients receiving exemestane showed a decrease from 0.53 to 0.34 after 12 months and to 0.28 after 24 months (each treatment comparison P ≤ 0.0001; Table 2 and Fig. 2c).
Changes in BMD in total hip
Significant differences between treatment groups were also found in changes in total hip BMD values. In the tamoxifen group, a mean increase from baseline of 0.8% after 12 months and a mean decrease from baseline of 0.4% after 24 months were observed, when compared with a mean decrease of 1.3% after 12 months and 3.3% after 24 months in the exemestane group (each treatment comparison P < 0.05; Table 2 and Fig. 3a). Mean total hip T-scores remained at −0.41 after 12 months and increased to −0.39 after 24 months in the tamoxifen group. In the exemestane group, a decrease in mean total hip T-scores from −0.43 to −0.60 and to −0.72 after 12 and 24 months, respectively, was observed (each treatment comparison P < 0.01; Table 2 and Fig. 3b). A slight increase was also found in mean total hip Z-scores in the tamoxifen group from 0.54 to 0.63 at month 12 and to 0.62 at month 24 versus a decrease from 0.60 to 0.55 after 12 months and to 0.46 after 24 months in the exemestane group (each treatment comparison P < 0.01; Table 2 and Fig. 3c).
Bone turnover markers
PINP levels (the Netherlands/Belgium and German sub-studies only) decreased from baseline in the tamoxifen group and increased in the exemestane group (Table 3 and Fig. 4a). Differences between treatment groups in changes from baseline to month 6 (P < 0.0001) and month 12 (P < 0.0001) were statistically significant (other time points were not tested). Differences between treatment groups in changes from baseline to month 12 were also significantly different between the German and Netherlands/Belgium sub-studies for PINP levels (P = 0.0237).
The trends over the study period for the differences between treatment groups in CTx (the Netherlands/Belgium sub-study only) and ICTP (German sub-study only) followed a similar pattern as observed with PINP levels (Table 3; Fig. 4b, c).
Additional analysis
Shift in BMD status
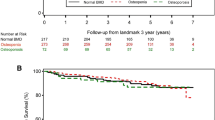
Among patients with a normal BMD value at baseline, a higher proportion of those in the exemestane group developed osteopenia at months 12 and 24 (Fig. 5). Only one patient in the exemestane group with a normal BMD value at baseline developed osteoporosis at 12 months.
Discussion
Our results show that tamoxifen and exemestane were significantly different with regard to change from baseline to months 12 and 24 in lumbar spine BMD. The observed changes in lumbar spine BMD corresponded to an average bone gain of 1.2% after 12 months and 0.2% after 24 months in the tamoxifen group, compared with an average bone loss of 2.6% after 12 months and 3.5% after 24 months in the exemestane group. Although the differences between the treatment groups remained statistically significant, the BMD changes appeared to stabilize over time. Observed changes in the other BMD variables followed a similar pattern. Markers of bone turnover were increased with exemestane and decreased with tamoxifen, and there was a statistically significant difference between the treatment groups at months 6 and 12. These changes, which are indicative of bone loss with exemestane, also appeared to stabilize after initial treatment.
In the first analysis of the overall TEAM trial at 2.75 years, exemestane was associated with a significant increase compared with tamoxifen in the incidence of osteoporosis (4.7% vs. 2.1%, respectively; P ≤ 0.001), but no significant increase in the incidence of fractures (2.7% vs. 2.3%, respectively) (Jones et al. 2008b). At a median of 5.1 years of follow-up, compared with the sequence of tamoxifen followed by exemestane, upfront exemestane was associated with a significant increase in osteoporosis (5.4% vs. 9.9%, respectively; P < 0.001), arthralgia (20.0% vs. 23.5%, respectively; P < 0.001), and fractures (3.5% vs. 5.1%, respectively; P < 0.001) (Rea et al. 2009).
Results from other studies evaluating the effects of exemestane on bone health are generally consistent with our findings. A randomized, double-blind study comparing exemestane and placebo showed that exemestane modestly enhanced BMD loss from the femoral neck, but had no significant influence on lumbar bone loss after 2 years of treatment. There was a significant increase in the markers of both bone resorption and formation in the exemestane group (Lönning et al. 2005). The fracture rate was similar in the exemestane and placebo groups (Lönning et al. 2005).
In the IES, patients who were disease-free after 2–3 years of tamoxifen were randomized to switch to exemestane or continue treatment with tamoxifen, for a total of 5 years’ endocrine therapy. In this study, patients who switched to exemestane had significantly longer OS when patients with ER-negative disease were excluded from the analysis. The effects of tamoxifen and exemestane on bone health were assessed in a sub-group of 206 patients (Coleman et al. 2007). Within 6 months, patients who switched to exemestane experienced a significant decrease in BMD from baseline at both the total hip and lumbar spine. In year 2, the rate of bone loss had slowed (Coleman et al. 2007). There was also an increase in bone resorption and bone formation markers in patients receiving exemestane (Coleman et al. 2007).
Other AIs have been shown to decrease BMD when used as adjuvant treatment. In the Anastrozole, Tamoxifen Alone or in Combination (ATAC) bone sub-study, BMD at the lumbar spine and total hip was significantly decreased by 6–7% in the anastrozole group and increased in the tamoxifen group after 5 years’ treatment (Eastell et al. 2008). In the overall ATAC study, there was a significantly increased rate of fractures (P < 0.0001) in patients treated with anastrozole compared with those receiving tamoxifen (Howell et al. 2005). Similarly, in the Breast International Group (BIG) 1-98 trial of adjuvant therapy with letrozole or tamoxifen in postmenopausal patients with endocrine-responsive early breast cancer, after 5 years of treatment, the incidence of fractures was higher among patients treated with letrozole (9.3%) than among patients treated with tamoxifen (6.5%) (Rabaglio et al. 2009).
Long-term data suggest the effect of AIs on bone health may be reversed after treatment completion. At a median follow-up of 100 months in the overall ATAC study, patients treated with anastrozole had experienced a significantly higher incidence of fractures during active treatment compared with patients receiving tamoxifen; however, there was no difference in the incidence of fractures after completion of treatment (Forbes et al. 2008). It remains unclear whether these results were due to selection bias, since women with a high risk of fracture or who sustained a fracture during the trial were excluded or dropped out. Additionally, it is unknown to what extent anti-fracture medications (such as bisphosphonates) were used. Data from the IES (at a median follow-up of 91 months) suggested that the differences between tamoxifen- and exemestane-treated patients with regard to incidence of osteoporosis or fracture decreased after treatment completion (Coleman et al. 2008a; Coombes et al. 2009).
It has been proposed that the steroidal AI exemestane may have different effects on bone metabolism compared with the non-steroidal AIs letrozole and anastrozole. A recent study in postmenopausal patients with breast cancer showed that although there were no significant differences in bone turnover marker levels between exemestane and anastrozole, there was a significant difference in BMD levels in favor of exemestane, after 3 years of treatment (Hozumi et al. 2010). However, results to date have been conflicting, and further studies are required to fully determine any differential effects of AIs on bone health (Goss et al. 2004, 2007; Hadji 2008a; Hadji and Bundred 2007; McCloskey et al. 2007; Miller et al. 2008).
The effects of AIs on bone health should be considered in the context of their superior efficacy and other tolerability benefits relative to tamoxifen. Furthermore, AI-associated bone loss is not life threatening and can be managed (Coleman et al. 2008b; Hadji et al. 2008).
In conclusion, exemestane treatment resulted in decreases in BMD and increases in the markers of bone formation and resorption. In contrast, BMD was increased and markers of bone turnover were decreased with tamoxifen. However, BMD and bone turnover changes appeared to stabilize after initial treatment.
References
Coates AS, Keshaviah A, Thurlimann B et al (2007) Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1–98. J Clin Oncol 25:486–492
Coleman RE, Banks LM, Girgis SI et al (2007) Skeletal effects of exemestane on bone-mineral density, bone biomarkers, and fracture incidence in postmenopausal women with early breast cancer participating in the intergroup exemestane study (IES): a randomised controlled study. Lancet Oncol 8:119–127
Coleman RE, Banks LM, Girgis SI et al (2008a) Reversal of skeletal effects of endocrine treatments in the intergroup exemestane study. Poster presentation at San Antonio Breast Cancer Symposium (SABCS), San Antonio, Texas, USA, 10–14 December
Coleman RE, Bolten WW, Lansdown M et al (2008b) Aromatase inhibitor-induced arthralgia: clinical experience and treatment recommendations. Cancer Treat Rev 34:275–282
Coombes RC, Hall E, Gibson LJ et al (2004) A randomized trial of exemestane after 2–3 years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 350:1081–1092
Coombes RC, Kilburn LS, Snowdon CF et al (2007) Survival and safety of exemestane versus tamoxifen after 2–3 years’ tamoxifen treatment (Intergroup Exemestane Study): a randomised controlled trial. Lancet 369:559–570
Coombes RC, Kilburn LS, Beare S et al (2009) Survival and safety post study treatment completion: an updated analysis of the intergroup exemestane study (IES)—submitted on behalf of the IES investigators. Oral presentation at the joint ECCO 15-ESMO 34 meeting, Berlin, Germany, 20–24 Sept 2009
Eastell R, Adams JE, Coleman RE et al (2008) Effect of anastrozole on bone mineral density: 5 year results from the anastrozole, tamoxifen, alone or in combination trial 18233230. J Clin Oncol 26:1051–1057
Forbes JF, Cuzick J, Buzdar A et al (2008) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100 month analysis of the ATAC trial. Lancet Oncol 9:45–53
Frenkel B, Hong A, Baniwal SK et al (2010) Regulation of adult bone turnover by sex steroids. J Cell Physiol 224:305–310
Goldhirsch A, Ingle JN, Gelber RD et al (2009) Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol 20:1319–1329
Goss PE, Qi S, Cheung AM et al (2004) Effects of the steroidal aromatase inhibitor exemestane and the nonsteroidal aromatase inhibitor letrozole on bone and lipid metabolism in ovariectomized rats. Clin Cancer Res 10:5717–5723
Goss PE, Hadji P, Subar M et al (2007) Effects of steroidal and nonsteroidal aromatase inhibitors on markers of bone turnover in healthy postmenopausal women. Breast Cancer Res 9:R52
Hadji P (2007) Aromatase inhibitor-associated bone loss in breast cancer. US Oncolo Dis 1:18–21
Hadji P (2008a) Aromatase inhibitor-associated bone loss in breast cancer patients is distinct from postmenopausal osteoporosis. Crit Rev Oncol Hematol 69:73–82
Hadji P (2008b) Menopausal symptoms and adjuvant therapy-associated adverse events. Endocr Relat Cancer 15:73–90
Hadji P, Bundred N (2007) Reducing the risk of cancer treatment-associated bone loss in patients with breast cancer. Semin Oncol 34:S4–S10
Hadji P, Body JJ, Aapro MS et al (2008) Practical guidance for the management of aromatase inhibitor-associated bone loss. Ann Oncol 19:1407–1416
Hadji P, Ziller M, Kieback DG et al (2009a) Effects of exemestane and tamoxifen on bone health within the tamoxifen exemestane adjuvant multicentre (TEAM) trial: results of a German, 12 month, prospective, randomised sub-study. Ann Oncol 20:203–207
Hadji P, Ziller M, Kieback DG et al (2009b) The effect of exemestane or tamoxifen on markers of bone turnover: results of a German sub-study of the tamoxifen exemestane adjuvant multicentre (TEAM) trial. Breast 18:159–164
Howell A, Cuzick J, Baum M et al (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62
Hozumi Y, Aihara T, Suemasu K et al (2010) The effect of exemestane and anastrozole on bone mineral density and bone turnover markers in postmenopausal early breast cancer patients: final results of 3 years after randomization of N-SAS (national surgical adjuvant study) BC04, the TEAM Japan sub-study. Poster presentation at the European Breast Cancer Conference, Barcelona, Spain, 24–27 March
Jones S, Stokoes C, Sborov M (2008a) The effect of tamoxifen or exemestane on bone mineral density during the first 2 years of adjuvant treatment of postmenopausal women with early breast cancer. Clin Breast Cancer 8:527–532
Jones SE, Seynaeve C, Hasenburg A et al (2008b) Results of the first planned analysis of the TEAM (tamoxifen exemestane adjuvant multinational) prospective randomized phase III trial in hormone sensitive postmenopausal early breast cancer. Oral presentation at San Antonio breast cancer symposium (SABCS), San Antonio, Texas, USA, 10–14 December
Lönning PE, Geisler J, Krag LE et al (2005) Effects of exemestane administered for 2 years versus placebo on bone mineral density, bone biomarkers, and plasma lipids in patients with surgically resected early breast cancer. J Clin Oncol 23:5126–5137
Love RR, Mazess RB, Barden HS et al (1992) Effects of tamoxifen on bone mineral density in postmenopausal women with breast cancer. N Engl J Med 326:852–856
McCloskey EV, Hannon RA, Lakner G et al (2007) Effects of third generation aromatase inhibitors on bone health and other safety parameters: results of an open, randomised, multi-centre study of letrozole, exemestane and anastrozole in healthy postmenopausal women. Eur J Cancer 43:2523–2531
Miller WR, Bartlett J, Brodie AM et al (2008) Aromatase inhibitors: are there differences between steroidal and nonsteroidal aromatase inhibitors and do they matter? Oncologist 13:829–837
National Comprehensive Cancer Network (2009) NCCN clinical practice guidelines in oncology: breast cancer V.1.2009. http://www.nccn.org/professionals/physician_gls/PDF/breast.pdf
Rabaglio M, Sun Z, Price KN et al (2009) Bone fractures among postmenopausal patients with endocrine-responsive early breast cancer treated with 5 years of letrozole or tamoxifen in the BIG 1–98 trial. Ann Oncol 20:1489–1498
Rea DW, Hasenburg A, Seynaeve C et al (2009) Five years of exemestane as initial therapy compared to 5 years of tamoxifen followed by exemestane: The TEAM trial, a prospective, randomized, phase III trial in postmenopausal women with hormone-sensitive early breast cancer. Oral presentation at San Antonio Breast Cancer Symposium (SABCS), San Antonio, Texas, USA, 10–13 December
van Nes JGH, Papapoulos SE, Braun JJ et al (2008) Effect of exemestane on bone turnover markers and bone mineral density (BMD): 2 year results of the Dutch/Belgian Tamoxifen Exemestane Adjuvant Multicentre (TEAM) trial. Poster presentation at San Antonio breast cancer symposium (SABCS), San Antonio, Texas, USA, 10–14 December
van Nes JGH, Seynaeve C, Jones S et al (2010) Variations in loco regional therapy in postmenopausal patients with early breast cancer treated in different countries. Br J Surg 97:671–679
Acknowledgments
The authors would like to acknowledge Dr Luc Dirix for his help with the Belgian data. Editorial assistance for this paper was provided by Caroline Masterman at ACUMED (Tytherington, UK) and was funded by Pfizer, Inc. This work was supported by a scientific research grant from Pfizer, Inc [grant number EXEAPO-0028-119].
Conflict of interest
Dr Hadji has received unrestricted educational grants, scientific research grants, and lecture fees from Pfizer, Inc. Dr Hasenburg has received honoraria for lectures from Pfizer, Inc. Dr Jones has received honoraria as a member of the speakers bureau for Pfizer, Inc. Dr Ziller has received support for travel to meetings for the study. Dr Menschik is a Pfizer employee and holds Pfizer stock. Dr Asmar, Dr van de Velde, Dr van Nes, Dr Nortier, and Mr Kuck have no conflicts of interest beyond elements of the Pfizer funding of the study noted in the Acknowledgements. The corresponding author had full access to all data and final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hadji, P., Asmar, L., van Nes, J.G.H. et al. The effect of exemestane and tamoxifen on bone health within the Tamoxifen Exemestane Adjuvant Multinational (TEAM) trial: a meta-analysis of the US, German, Netherlands, and Belgium sub-studies. J Cancer Res Clin Oncol 137, 1015–1025 (2011). https://doi.org/10.1007/s00432-010-0964-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-010-0964-y