Abstract
Purpose
Primary androgen deprivation therapy (PADT) is an important treatment modality for men with localized or locally advanced prostate cancer and without bone metastasis. There is, however, a lack of data on the biochemical relapse (BR) outcomes in these patients. Here, we studied the outcome of a contemporary series of men treated by PADT and investigated predictive risk factors for BR.
Methods
One hundred and fifty-five patients treated by PADT formed the initial study cohort, and BR outcomes in this group were reviewed. The outcomes of men with bone scan negative disease were specifically analysed. The predictive value of a panel of clinical risk factors for BR was evaluated using univariate and multivariate analysis. The results were further validated in a separate cohort of patients without bone metastasis from a second institution (n = 84).
Results
Median follow-up was 70 months. In the first study cohort, 109/155 men (70%) had bone scan negative disease. In these patients, only 45% developed BR during the follow-up period with only 28% relapsing within 5 years of initiating PADT. Key-independent factors predicting BR were a high PSA nadir (p = 0.001) and a shorter time to nadir (p < 0.001). A nadir of ≤0.1 ng/ml and time to nadir of >24 months specifically identified men with a very good outcome from PADT. In a second-independent cohort, very similar overall and 5-year BR rates were observed in men without bone metastasis (39 and 35%, respectively). PSA nadir thresholds identified in the first cohort were again able to define a good prognostic group in this re-test cohort (p = 0.005 and p = 0.01, respectively).
Conclusion
Men treated by PADT and without bone metastasis can have very durable responses to PADT with the majority remaining BR free at 5 years. PSA nadir and time to nadir are key predictors of a good outcome in this group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Androgen deprivation therapy is an important treatment modality for men with prostate cancer (Huggins and Hodges 1941; Schally 2007; Sharifi et al. 2005). Primary ADT (PADT) is the treatment of choice in metastatic disease and is recommended in older men with locally advanced tumours and who are unsuitable for radical therapy (Heidenreich et al. 2008). In recent years, however, the numbers of men presenting with metastatic disease has been declining with the widespread use of PSA testing and the majority now present with more local disease (Cooperberg et al. 2003a, b; Evans and Moller 2003). In the United Kingdom, many of these men will be treated by PADT as the sole modality of treatment (http://www.nycris.nhs.uk). Despite its widespread use, however, the biochemical relapse–free survivals for these men in contemporary clinical practice have not been well reported. Such information would be a valuable resource in providing accurate information to patients as to their likely risk of disease response and relapse.
PADT will eventually fail for many men, and they will progress to castration resistant disease which remains a difficult condition to treat. There are currently no predictive models used in routine practice to define men at high risk of biochemical relapse from PADT. It is not also clear if the same risk factors or risk factor cut-offs are equally predictive of biochemical relapse in men with and without bone metastasis at presentation (Wilson et al. 1985; Ishikawa et al. 1989; Soloway et al. 1989). The identification of risk factors that can predict good or poor responses to PADT would clearly be a valuable tool in clinical management. Risk factors predicting biochemical relapse can help in early identification of those men who are likely to relapse quickly. Equally, some men who may have prolonged and very durable responses to PADT may need less intensive follow-up.
In this study, we undertook an outcome analysis of the therapeutic response following PADT in a contemporary cohort of men from two different institutions. Our goal was to determine the rates of biochemical relapse in men with bone scan negative disease and to test for clinical predictive factors of relapse in this group.
Patients and methods
One hundred and fifty-five patients (median age 76 years) diagnosed with prostate cancer during 1999–2001 and treated with PADT in a single centre were included in this study. Men in this cohort were diagnosed by PSA testing and biopsy and clinically staged by examination. All men had data evaluable from isotope bone scans before commencing PADT. Staging CT scans were not performed in any patient as it is not a routine staging investigation in our centres. Patients underwent PADT with either luteinizing hormone releasing hormone agonists (LHRHa) (with anti-androgen cover) or bilateral subcapsular orchidectomy (BSO). All patients were followed up in a single clinic with all PSA biochemistry processed using an identical assay (Total PSA, Siemens Healthcare Diagnostics). PSA was measured at 3 monthly intervals for the first year and thereafter 6 monthly if the PSA response was stable. The PSA was considered to be stable at all other time points if it remained at the nadir level or if higher, failed to meet the criteria for BR. Any rise in PSA prompted a return to 3 monthly or sooner repeat assessments. The following clinical parameters were investigated: Continuous variables were age, presenting PSA, percentage biopsy involvement, lowest PSA value achieved (PSA nadir) and time to nadir. Categorical variables were Gleason sum score, clinical stage (TNM criteria) and metastasis (presence or absence). These variables were tested against the primary clinical outcome of Biochemical Relapse (BR) as defined by the EAU (date of the first of three consecutive rising PSA at least 2 weeks apart resulting in two 50% increases over the nadir value) (Heidenreich et al. 2008). Patients were further stratified into two sub-groups based on objective radio-isotope evidence of the presence or absence of bone metastasis. To validate the findings from the first cohort, the outcomes from a separate cohort of 84 patients with non-bone metastatic prostate cancer were reviewed from a second urology unit. All men were diagnosed and followed up over a similar time frame as the initial study group and were treated with PADT only. Outcomes were assessed using identical criteria as described above. Statistical analysis for the study was performed using univariate Cox regression analysis, and significant factors were further tested in multivariate analysis using a forward selection procedure. The Log rank test and Kaplan–Meier survival curves were used to assess the relationship between different threshold values and BR. A level of p < 0.05 was taken as being statistically significant.
Results
BR outcomes and predictive factors in men without bone metastasis at presentation
The clinical characteristics of the initial study cohort of 155 men are shown in Table 1. The mean follow-up was 58 months with a median of 70 months. The overall frequency of BR was 57% (n = 88) in this cohort. 109 (70%) had no bone metastasis following an isotope bone scan while 46 (30%) men had positive bone scans. For patients without bone metastasis 45% (n = 49) developed BR within the median follow time of 70 months. In these men only 30/109 (28%) relapsed within 5 years of starting PADT. By way of comparison, men with bone metastasis had a predictably much worse outcome with 85% (n = 39) developing BR within 5 years. In this group the median time to BR was only 16 months (range 5–72) with 31/46 (67%) relapsing within 2 years of initiating treatment. Clinical variables were analysed for their value in predicting BR within the study period. The non-metastatic and metastatic groups were investigated separately to determine potential predictive factors for the event of BR (Table 2). In non-metastatic patients the risk factors for BR on univariate analysis included a high PSA nadir, shorter time to nadir, younger age, high clinical stage and high percentage core positivity. In multivariate analysis a high PSA nadir (p < 0.001), shorter time to nadir (p < 0.001) and advanced clinical stage (p = 0.01) were independent predictors of BR. In the bone metastasis group, adverse factors for BR on univariate analysis were a high PSA nadir, shorter time to nadir, younger age and a high presenting PSA. In multivariate analysis a high PSA nadir (p = 0.002), shorter time to nadir (p < 0.001) and younger age (p = 0.03) were strong independent predictors of BR. These results suggest that while there is a difference in risk factors associated with outcome in non-metastatic and bone metastatic cohorts, the PSA nadir and time to nadir are common factors predictive of BR.
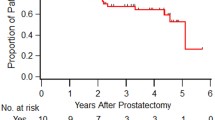
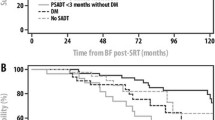
Optimal PSA nadir and time to nadir thresholds in men without bone metastasis at presentation
In this study, as expected BR rates differed significantly in men with and without bone metastasis. We therefore hypothesized that different PSA nadir and time to nadirs would be needed to discriminate good or poor responders in these groups. To identify the optimal thresholds, different PSA nadirs were tested using Kaplan–Meier survival analysis. In men without bone metastasis, the median PSA nadir for the group was 0.45 (range 0.01–15.9). We therefore tested different PSA nadir thresholds around this median to identify a level which would best identify a good outcome group. Threshold values of ≤0.1, >0.1–0.4, >0.4–1 and >1 ng/ml were tested and allowed a proportional division of the cohort. In this analysis, lower PSA nadir thresholds identified men with reduced risks of BR (p = 0.01 for trend) (Fig. 1a). In particular, men who achieved a PSA threshold of ≤0.1 ng/ml had the lowest risk of BR with only one individual relapsing in the follow-up period of 5 years. Further analysis of lower thresholds was not performed as there were too few numbers for accurate analysis in this study. In men with bone metastasis, the median nadir PSA was 3.2; therefore, higher threshold values of <1, >1–5 and >5 ng/ml were tested. Again, we observed that lower PSA nadir thresholds identified men with reduced risks of BR (p < 0.0001 for trend) (Fig. 1b). In this cohort, men with a PSA threshold of ≤1 ng/ml had the best outcome. A similar analysis was done for the time to PSA nadir. In men without bone metastasis, longer nadir times were associated with improved BR with an overall median time to nadir of 17 months. We therefore tested different time to nadir thresholds around this median (<12, 12–24 and >24 months) to identify an optimal cut-off. Longer times to nadir identified men with a reduced risk of BR in this analysis (p = 0.001 for trend) (Fig. 2a). Men with a time to nadir of >24 months in particular had a low incidence of BR with only three relapsing in the study period. In men with bone metastasis, however, the median time to PSA nadir was only 8 months, and the majority of men had relapsed within 24 months of PADT. In this group therefore we tested time to nadir thresholds of <6, 6–12 and >12 months and identified a reduced risk of BR in men with longer times to nadir (p < 0.0001 for trend) (Fig. 2b). In this cohort, men with a PSA threshold of >12 months had the best outcome. These results suggest that the PSA nadir has different relevant clinical cut-off values depending on the presence or absence of concurrent bone metastasis. In men without metastasis, in this study, achieving a nadir of ≤0.1 or time to nadir of >24 months appeared to identify a group of men with a particularly low risk of BR.
Validation of study results in a re-test cohort
To further investigate the robustness of our findings in non-bone metastatic men, we analysed the outcomes of PADT-treated men from a second geographically distinct centre. Eight-four men with bone scan negative disease were included in this re-test cohort (Table 3). There was no significant difference in the median age, presenting PSA, clinical stage or Gleason sum score between the first and second groups (Table 3). Strikingly, we observed very similar overall and 5 year BR rates when the two cohorts were compared (39% versus 45%, p = 0.43 and 35% versus 28%, p = 0.29, respectively). We next tested if PSA nadir thresholds previously identified would be able to predict outcome in this second cohort. In this re-test, we used the threshold of ≤0.1 ng/ml as this had defined a group with the lowest events of BR in our initial cohort. In this analysis, men who achieved a PSA nadir value of ≤0.1 had a significantly better response to PADT in comparison with men with a PSA nadir of >0.1 (p = 0.005) (Fig. 3a). Similarly, for time to nadir, we used the threshold of >24 months as this had defined a group with the lowest events of BR in our initial cohort. In this re-test, men who achieved nadir at >24 months had significantly better outcomes from PADT compared to men who achieved PSA nadirs at <24 months (p = 0.01) (Fig. 3b). These results in a re-test cohort support the findings from our initial study cohort and confirm that the proposed PSA nadir thresholds are able to identify good outcome groups in men without evidence of bone metastasis treated by PADT.
Discussion
This study did not seek to compare the BR outcome between men with and without bone metastasis. Rather, our aim was to investigate the specific outcomes in men without metastasis treated by PADT. In this study, 70% of informative cases had no evidence of bone metastasis at presentation. Results from the CaPSURE and SEER databases suggest that this trend is also evident in the United States with PADT being widely used as a primary treatment modality for many men without bone metastatic disease (Cooperberg et al. 2003a; Shahinian et al. 2005). Published data from the UK Northern and Yorkshire Cancer Registry has shown that up to 60% of men aged over 70 and 20% of men aged 55–69 with non-metastatic disease are treated by PADT as the sole treatment modality (http://www.nycris.nhs.uk). Despite this widespread uptake, however, we could not find any published data on the expected BR outcomes following PADT among men presenting with non-metastatic disease in the United Kingdom. In the present study, only a third of patients without bone metastasis had relapsed by 5 years post initiation of PADT and less than half had relapsed at a median of 70-month follow-up. These findings were very consistent across two independent cohorts of men from separate hospitals in this study. These results are very similar to studies reported in the United States. In one study, men treated by PADT had an overall BR rate of only 25% over a 5-year follow-up period (Janoff et al. 2005). Kawakami et al. (2006) further reported that 67.3% of men in their study were relapse free at 5 years after PADT. Both our results and the data from these studies suggest very durable responses to PADT in men without bone metastasis with many patients achieving prolonged periods of sustained disease control.
Risk stratification tools are not in common use to identify good and poor responders to ADT. In this report, we were particularly interested in defining risk factors for BR in men without bone metastasis treated by PADT. We also compared risk factors with a cohort of men with evidence of bone metastasis. In our initial study of the whole group, multivariate analysis identified bone metastasis, high PSA nadir and a shorter time to nadir as the most significant risk factors for BR. These findings are supported by other studies of PADT in mixed populations of men (Kwak et al. 2002; Morote et al. 2004). In a sub-analysis of men without bone metastasis, PSA nadir and time to nadir retained a strong independent predictive value for BR. The positive association between a high PSA nadir and BR has been consistently reported by many studies (Benaim et al. 2002; Oefelein et al. 2002; Morote et al., 2005). The relationship between time to nadir and BR however is more controversial with different groups reporting contradictory findings. Oefelein et al. (2002) and Cooper (1992) for instance have reported that a shorter time to nadir predicts a better biochemical-free survival. Other studies, however, in keeping with our findings have found a better biochemical relapse free and indeed overall survival with a more prolonged time to PSA nadir (Morote et al. 2005; Choueiri et al. 2009). In men presenting with bone scan positive disease, PSA nadir and time to nadir again emerged as strong predictive risk factors for BR. These findings lead us to conclude that a high PSA nadir and shorter time to nadir are key common predictive factors of PADT failure irrespective of metastatic status.
There is currently no consensus on the optimal PSA nadir and time to nadir predictive of ADT response with different thresholds reported by individual studies. Individual studies in the literature have reported very different optimal thresholds for metastatic disease. Kwak et al. (2002) reported that a PSA nadir of <1.1 ng/ml was most sensitive in identifying men with a lower risk of BR. Morote et al. (2005), in contrast, found that a PSA nadir of <2 ng/ml was associated with a lower risk of BR. Differences in PSA thresholds have also been found in studies with survival as an end point. In the SWOG 9346 study, a PSA nadir of <4 ng/ml after 7 months of treatment was a strong predictor of improved overall survival (Hussain et al. 2006). In contrast, Choueiri et al. (2009) have recently reported that a time to nadir of >6 months and PSA nadir <0.2 ng/ml were optimal in predicting a shorter overall survival in men with metastatic disease. These studies highlight the lack of consensus on the optimal PSA nadir and time to nadir which can discriminate good and poor responders. In keeping with our findings, however, they confirm the strong prognostic importance of the PSA response after PADT. To our knowledge, clinically useful thresholds have not been previously investigated or defined for PADT in men with non-metastatic disease. In this study, we observed that lower PSA nadir thresholds were associated with reduced risks of BR. A PSA nadir of ≤0.1 ng/ml optimally identified non-metastatic men with the lowest incidence of BR. As our sample size was relatively small, we did not test lower thresholds as the number of cases was low. It is therefore possible that lower thresholds for the PSA nadir may be better discriminators but this requires further studies with larger cohort sizes. Crucially, however, the relevant nadir thresholds levels are very different compared to men with metastasis in which much higher nadirs were observed. Similarly, we observed that a time to nadir of >24 months optimally identified non-metastatic men with a very low incidence of BR after PADT.
Our study has some inherent limitations. We only used radioisotope evidence of bone involvement as the criteria for metastasis and this is the standard of care in the United Kingdom (http://guidance.nice.org.uk/CG58/Guidance/pdf/English). We therefore cannot comment if bone scan negative men in our series might have had soft tissue or lymph node metastasis at presentation. Indeed, as far as we are aware no study has tested how often CT scans may show soft tissue metastasis when a bone scan is normal in prostate cancer. It is possible that those who had poorer outcomes in the bone scan negative group did have evidence occult metastasis and this merits further investigation. At the current time, however, CT scans are not currently recommended as investigations for suspected metastatic disease in either the EAU or UK NICE guidelines (Heidenreich et al. 2008; http://guidance.nice.org.uk/CG58/Guidance/pdf/English). The pre-defined study end point was BR, and the study follow-up was relatively short. We are currently evaluating if the same risk factors are associated with disease-specific mortality though we will need further follow-up to robustly evaluate this. Data from the United States, for example, has shown that PADT has a 5-year disease-specific and overall survival rate of up to 95 and 85%, respectively (Kawakami et al. 2006; DiBlasio et al. 2009). In the Prostate Cancer Group study from Japan, the 10-year cause-specific survival for men treated solely by PADT was 78% (Akaza et al. 2006). We are continuing to monitor both cohort of patients and intend to report on the validity of our identified risk factors over a longer term in terms of BR and survival in future work.
In summary, in this study, most men who receive PADT for bone scan negative disease can have very durable responses with the majority remaining hormone responsive at 5-year post-treatment. The post-treatment PSA nadir and time to nadir may be useful predictive factors of treatment response for PADT. Our findings provide a rationale basis for a multicentre prospective study to further validate the findings and which is currently being planned. Such studies may afford the opportunity to identify and test predictive models of BR which can then be used to refine follow-up regimes for patients. The current results may also help in the counselling of men without bone metastasis treated by PADT as to their expected response to treatment.
References
Akaza H, Homma Y, Usami M, Hirao Y, Tsushima T, Okada K, Yokoyama M, Ohashi Y, Aso Y, Prostate Cancer Study Group (2006) Efficacy of primary hormone therapy for localized or locally advanced prostate cancer: results of a 10-year follow-up. BJU Int. 98:573–579
Benaim EA, Pace CM, Lam PM, Roehrborn CG (2002) Nadir prostate-specific antigen as a predictor of progression to androgen-independent prostate cancer. Urology: 59:73–78
Choueiri TK, Xie W, D’Amico AV et al (2009) Time to prostate-specific antigen nadir independently predicts overall survival in patients who have metastatic hormone-sensitive prostate cancer treated with androgen-deprivation therapy. Cancer 115:981–987
Cooper EH (1992) Prostate specific antigen in diagnosis, staging, and follow-up of prostate cancer. Prostate 4:125–129
Cooperberg MR, Grossfeld GD, Lubeck DP (2003a) National practice patterns and time trends in androgen ablation for localized prostate cancer. J Natl Cancer Inst 95:981–989
Cooperberg MR, Lubeck DP, Mehta SS et al (2003b) Time trends in clinical risk stratification for prostate cancer: implications for outcomes (data from CaPSURE). J Urol 170:S21–S25 (discussion S6–S7)
DiBlasio CJ, Malcolm JB, Hammett J, Wan JY, Aleman MA, Patterson AL, Wake RW, Derweesh IH (2009) Survival outcomes in men receiving androgen-deprivation therapy as primary or salvage treatment for localized or advanced prostate cancer: 20-year single-centre experience. BJU Int 104:1208–1214
Evans HS, Moller H (2003) Recent trends in prostate cancer incidence and mortality in southeast England. Eur Urol 43:337–341
Heidenreich A, Aus G, Bolla M et al (2008) EAU guidelines on prostate cancer. Eur Urol 53:68–80
Huggins C, Hodges C (1941) Studies in prostate cancer: the effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Cancer Res 1:293–297
Hussain M, Tangen CM, Higano C (2006) Absolute prostate-specific antigen value after androgen deprivation is a strong independent predictor of survival in new metastatic prostate cancer: data from Southwest Oncology Group Trial 9346 (INT-0162). J Clin Oncol 24:3984–3990
Ishikawa S, Soloway MS, Van der Zwaag R, Todd B (1989) Prognostic factors in survival free of progression after androgen deprivation therapy for treatment of prostate cancer. J Urol 141:1139–1142
Janoff DM, Peterson C, Mongoue-Tchokote S et al (2005) Clinical outcomes of androgen deprivation as the sole therapy for localized and locally advanced prostate cancer. BJU Int 96:503–507
Kawakami J, Cowan JE, Elkin EP, Latini DM, DuChane J, Carroll PR, CaPSURE Investigators (2006) Androgen-deprivation therapy as primary treatment for localized prostate cancer: data from Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE). Cancer 106:1708–1714
Kwak C, Jeong SJ, Park MS, Lee E, Lee SE (2002) Prognostic significance of the nadir prostate specific antigen level after hormone therapy for prostate cancer. J Urol 168:995–1000
Morote J, Trilla E, Esquena S et al (2004) Nadir prostate-specific antigen best predicts the progression to androgen-independent prostate cancer. Int J Cancer 108:877–881
Morote J, Esquena S, Abascal JM et al (2005) Usefulness of prostate-specific antigen nadir as predictor of androgen-independent progression of metastatic prostate cancer. Int J Biol Markers 20:209–216
North and Yorkshire Cancer Registry and Information Service. http://www.nycris.nhs.uk
Oefelein MG, Ricchiuti VS, Conrad PW et al (2002) Clinical predictors of androgen-independent prostate cancer and survival in the prostate-specific antigen era. Urology 60:120–124
Schally AV (2007) Luteinizing hormone-releasing hormone analogues and hormone ablation for prostate cancer: state of the art. BJU Int 100(Suppl 2):2–4
Shahinian VB, Kuo YF, Freeman JL, Orihuela E, Goodwin JS (2005) Increasing use of gonadotropin-releasing hormone agonists for the treatment of localized prostate carcinoma. Cancer 103:1615–1624
Sharifi N, Gulley JL, Dahut WL (2005) Androgen deprivation therapy for prostate cancer. JAMA 294:238–244
Soloway MS, Ishikawa S, van der Zwaag R, Todd B (1989) Prognostic factors in patients with advanced prostate cancer. Urology 33:53–56
Wilson DW, Harper ME, Jensen HM et al (1985) A prognostic index for the clinical management of patients with advanced prostatic cancer: a British Prostate Study Group investigation. Prostate 7:131–141
Acknowledgments
Work supported by Cancer Research UK.
Conflict of interest statement
The authors declare that they have no conflict of interest in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
S. Hori and T. Jabbar are the joint first authors.
Rights and permissions
About this article
Cite this article
Hori, S., Jabbar, T., Kachroo, N. et al. Outcomes and predictive factors for biochemical relapse following primary androgen deprivation therapy in men with bone scan negative prostate cancer. J Cancer Res Clin Oncol 137, 235–241 (2011). https://doi.org/10.1007/s00432-010-0877-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-010-0877-9