Abstract
Purpose
Most breast cancer patients with estrogen receptor-negative/progesterone receptor-positive (ER−/PgR+) tumors are premenopausal cases, with few alternatives of adjuvant endocrine therapy but tamoxifen (TAM). The efficacy of adjuvant TAM on ER−/PgR+ patients is still controversial. In this study, we evaluated the efficacy of adjuvant TAM on patients with ER−/PgR+ tumors.
Methods
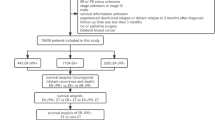
Among all 1,836 consecutive patients with operable primary breast cancer, 798 cases were with ER+/PgR+ tumors and 205 with ER−/PgR+ tumors. By sub-grouping the patients according to ER/PR phenotypes and whether the patients had been treated with adjuvant TAM therapy or not, we investigated the differences of survivals between groups.
Results
Patients with ER−/PgR+ tumors were younger than those with ER+/PgR+ tumors (P = 0.021), and were mainly premenopausal (P = 0.013). ER−/PgR+ patients were related to more involved lymph nodes and later stage. In the absence of TAM treatment, ER+/PgR+ group had a similar survival to ER−/PgR+ group in terms of 5-year disease-free survival (DFS), as well as overall survival (OS). After TAM treatment, both groups had increased survival rates comparing with the baseline of non-TAM-treated groups. Moreover, significant survival differences were then observed between TAM-treated ER+/PgR+ group and TAM-treated ER−/PgR+ group either in DFS (P = 0.016) or OS (P = 0.007). Of the TAM-treated patients, by sub-dividing the chemotherapy-treated population into CMF (cyclophosphamide, methotrexate and 5-fluorouracil) group and CA(E)F (cyclophosphamide, doxorubicin/epirubicin and 5-fluorouracil) group, we found that ER−/PgR+ group got more benefits from CMF regimen than from CA(E)F. Subpopulation treatment effect pattern plot (STEPP) analysis showed that the ER−/PgR+ group had an obvious worse survival than ER+/PgR+ group in younger patients (<55 years). Axillary lymph nodes involvement was the only independent prognostic factor for ER−/PgR+ group.
Conclusions
Our results indicate that patients with ER−/PgR+ tumors are mainly premenopausal and young. Although patients with ER−/PgR+ tumors are generally considered as candidates for endocrine therapy clinically, the ER−/PgR+ group gains less benefits from adjuvant TAM treatment than ER+/PgR+ group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The effectiveness of tamoxifen (TAM) has been confirmed in all-stage breast cancer patients with estrogen receptor positive (ER+) tumors (Osborne 1998a). Recently, results from multiple large randomized trials indicate that aromatase inhibitors (AIs) are preferable to postmenopausal patients (Winer et al. 2005), but are contraindicated to premenopausal women. Therefore, at present, 5-year treatment of TAM is still the golden standard of endocrine therapy for premeonopausal patients with primary breast cancer (Goldhirsch et al. 2005; Jonat et al. 2006).
As the synthesis of progesterone receptor (PgR) is stimulated by estrogen through an interaction with ER (Fanelli et al. 1996), PgR is considered to be a putative marker of functional ER (Cui et al. 2005). It was once believed that the presence of ER was a prerequisite for PgR expression. However, recent studies, by immunologic methods using antibodies that can measure both occupied and unoccupied receptors, have proved the existence of tumors expressing PgR with relatively insufficient ER (Keshgegian 1994; Kiani et al. 2006). In addition, ER−/PgR+ breast carcinoma cell lines, such as Evsa-T cell (Borras et al. 1997) have been established.
It is not surprising that ER+/PgR+ phenotype is more common than the other three phenotypes, and the profiles of ER+/PgR+ and ER−/PgR− tumors can unambiguously predict the response to endocrine therapy. ER+/PgR− and ER−/PgR+ phenotypes might show an intermediate response rate to endocrine therapy. In a locally advanced or metastatic setting, the response rate of ER−/PgR+ tumors to hormonal therapy was lower than that of ER+/PgR+ tumors (Bezwoda et al. 1991; Osborne 1998b). In the adjuvant setting, however, there were few published evidences regarding ER−/PgR+ tumors. Although the natural history of ER−/PgR+ tumor and its responsiveness to endocrine therapy are still controversial (Nikolic-Vukosavljevic et al. 2002), patients of such phenotype generally are treated with hormonal therapy clinically. Then a question emerges, whether the expression of PgR could predict the effectiveness of adjuvant TAM treatment even when ER is truly absent or insufficient. In this study, we sought to evaluate the efficacy of adjuvant TAM on patients with ER−/PgR+ tumors.
Patients and methods
Patients
There were totally 1,863 consecutive operable breast cancer patients, who were admitted into Shanghai Cancer Hospital from Jan 1991 to Dec 2001 with available ER and PgR profiles (1,175 ER+ cases (63.1%); 1,003 PgR+ cases (53.8%)). Seven hundred and ninety eight patients were ER+/PgR+ and 205 were ER−/PgR+. The clinicopathologic data and follow-up information of each patient came from the database established by Surgery Department of Shanghai Cancer Hospital.
The median age of patients was 50 years (26–86 years) and median tumor size was 3.0 cm (0.5–10 cm). Stage was classified according to TNM staging of UICC/AJCC. Each patient received appropriate surgery according to individual situation. About 86% of patients received chemotherapy, and the majority received CMF (cyclophosphamide, methotrexate and 5-fluorouracil) or CA(E)F (cyclophosphamide, doxorubicin/epirubicin and 5-fluorouracil) regimens. No one used trastuzumab in an adjuvant setting. Post-relapse therapies, including chemotherapy, endocrine therapy, and radiotherapy, were performed individually. The median follow-up time was 48 months (6–141 months). The follow-up rates of 1-year, 2-year, and 5-year were 93% (931/1,003), 69.3% (695/1,003), and 49.7% (498/1,003), respectively.
In order to improve comparability, we excluded the patients receiving AIs and other endocrine therapies such as ovarian ablation or function suppression. “TAM-treated patients” were defined as those who received TAM in an adjuvant setting for 3–5 years and started within 8 months after operation, or those who were supposed to receive adjuvant TAM therapy, but did not finish it due to recurrence, metastasis or death; “non-TAM-treated patients” are those who did not take adjuvant TAM treatment or stopped it within 1 year due to any other causes except for recurrence, metastasis, and death.
Steroid receptor assay
In present study, ER and PgR statuses were carried out by established immunohistochemical (IHC) method of avidin-biotin-peroxidase complex (ABC) assay described by previous reference (Shimada et al. 1985; Yu et al. 2007b). Immunoreactivity scoring was performed by evaluating the percentage of cancer cell nuclear staining, while cytoplasmic staining was ignored. Percentage of staining cells equal to or more than 10% was considered positive. The histopathologic and IHC outcomes were approved and checked by two pathologists independently in Pathology Department of Shanghai Cancer Hospital. In present study, we obtained the ER and PgR profiles from database directly as described before (Yu et al. 2007a). Among all 1,836 cases, 42.8% patients were with ER+/PgR+ tumors, 20.2% with ER+/PgR−, 25.9% with ER−/PgR−, and 11.0% with ER−/PgR+ tumors.
Statistical analysis
Statistical analysis consisted of student t test for continuous variables, chi-square (χ 2) analysis for categorical variables (performing Fisher’s exact test when χ 2 test unavailable), and log-rank test for prognostic differences between subgroups of patients whose survival curves were derived by Kaplan-Meier. Five-year survival rate was evaluated by life table method. Multivariate analysis was carried out by Cox risk proportion model, and adjusted by following variables: age, menopausal status, tumor size, stage, pathologic pattern, nodal status, adjuvant chemotherapy, adjuvant TAM treatment, and HER-2 status.
Overall survival (OS) was defined as the interval between diagnostic biopsy or surgery and death for any causes. Disease-free survival (DFS) was calculated as the date from the diagnostic biopsy or surgery to the earliest occurrence (local, regional, distant) or the second primary cancer or death without any evidence of recurrence. We also used the subpopulation treatment effect pattern plot (STEPP) methodology to analyze the age effect on survival both in ER+/PgR+ and ER−/PgR+ groups. STEPP involves defining several overlapping subgroups of patients on the basis of a covariate of interest and studying the resulting pattern of the treatment effects estimated within each subgroup (Bonetti and Gelber 2000). Two sided P value lower than or equal to 0.05 was considered statistically significant. The SPSS 12.0 for windows software package was used for analysis.
Results
Differences between ER+/PgR+ group and ER−/PgR+ group
The mean age of patients with ER−/PgR+ tumors was younger than those with ER+/PgR+ tumors (50 vs. 52 years, P value of t test = 0.021). Correspondingly, ER−/PgR+ patients were more likely to be premenopausal than ER+/PgR+ patients (64 vs. 54%; P value of χ 2 test = 0.013 Table 1). The mean size of ER−/PgR+ tumors was 34 mm, a little larger than that of ER+/PgR+ tumors of 31 mm. The lymph nodes involvements were also distributed differently. Finally, we found that more patients with ER−/PgR+ tumors received adjuvant chemotherapy (P = 0.249) and less ER−/PgR+ patients received adjuvant TAM treatment (P < 0.001). However, there were no significant differences between the two groups in terms of stage, pathologic pattern and HER-2 status.
Different therapeutic efficacy of adjuvant TAM on patients with ER+/PgR+ tumors and ER−/PgR+ tumors
As most ER−/PgR+ patients were premenopausal cases, TAM was usually the first option as adjuvant endocrine therapy at present. In order to determine the effectiveness of adjuvant TAM on different phenotypes, we compared the ER+/PgR+ patients with ER−/PgR+ patients in both non-TAM-treated group and TAM-treated group. In non-TAM-treated patients, better outcomes were observed in ER+/PgR+ group than those in ER−/PgR+ group in terms of 5-year DFS, as well as OS (DFS in Fig. 1 and OS in Fig. 2, both in light color; see detailed in Table 2), but without a statistical significance. However, in TAM-treated patients, survival rates of each group increased respectively, compared with the baselines of non-TAM-treated groups (DFS in Fig. 1 and OS in Fig. 2, both in dark color; see detailed in Table 2) with a statistical significance between the two TAM-treated groups in terms of DFS (P = 0.016) and OS (P = 0.007), indicating that an obvious gap between survival curves emerged. Notably, this study was a retrospective research and biases were unavoidable. We thus investigated the comparability between groups. It was shown that clinical and pathological features between ER+/PgR+ group and ER−/PgR+ group in both non-TAM-treated and TAM-treated groups seemed to be comparable, except for tumor size, lymph nodes involvement, and HER-2 status (data shown in supplemental table 1).
Various chemotherapeutic modalities had different mechanisms with different therapeutic efficacies. In order to investigate the potential difference of chemotherapeutic efficacy on different hormonal receptor phenotypes, we divided patients into subgroups according to chemotherapy regimens used. Of the TAM-treated patients, 83.7% received chemotherapy, including 52.9% receiving CMF, 29.0% receiving CA(E)F, and the remaining 1.8% receiving other regimens containing taxanes and vincristine. As Fig. 3 showed, chemotherapy improved survival of ER−/PgR+ patients significantly, while the ER+/PgR+ patients seemed to get limited benefits compared with the baseline. By sub-dividing the chemotherapy-treated population into CMF and CA(E)F group, we found that ER−/PgR+ group got more benefits from CMF regimen than from CA(E)F.
DFS curves of TAM-treated ER+/PgR+ group and ER−/PgR+ group by different chemotherapeutic regimens. a Without chemotherapy. P value of difference between ER+/PgR+ group and ER−/PgR+ group is <0.0001. b With chemotherapy. P value of difference between ER+/PgR+ group and ER−/PgR+ group is 0.2405. c With CMF regimen. P value of difference between ER+/PgR+ group and ER−/PgR+ group is 0.7589. d With CA(E)F regimen. P value of difference between ER+/PgR+ group and ER−/PgR+ group is 0.1221
Survival tendency by age and prognostic factors of patients with ER−/PgR+ tumors
STEPP analysis was used to explore the patterns of differential survival tendency by varying age in ER+/PgR+ and ER−/PgR+ group. Figure 4 showed that ER+/PgR+ group had a slight survival advantage over ER+/PgR− group in patients older than 55 years; moreover, the superiority was extremely obvious in younger population (40–55 years). This interesting finding revealed that younger ER−/PgR+ patients had a worse survival. While in the <40 years population, ER+/PgR+ group and ER−/PgR+ group seemed to have similar survival rates, which might be due to the relatively fewer cases in this strata.
Subpopulation treatment effect pattern plots (STEPP) analysis of the age effect on DFS in both ER+/PgR+ group and ER−/PgR+ group. STEPP analyses plot shows 5-year disease-free survival (DFS) on the y-axis for subpopulations of patients with mean age shown on the x-axis. For this sliding-window STEPP analysis, subpopulation contained 100 patients in ER+/PgR+ group (total 798 cases) and 50 patients in ER−/PgR+ group (total 205 cases). Each subsequent subpopulation was formed moving from left to right by dropping 20 patients with the lowest age and adding 20 patients with the next higher age in ER+/PgR+ group, and dropping five and adding five, in ER−/PgR+ group
Some clinicopathologic and molecular markers had been identified as prognostic factors for breast cancer, such as age, tumor size, numbers of involved lymph nodes, and HER-2 status, etc. In our study, the independent prognostic factors of DFS for all patients were stage, numbers of involved lymph nodes, use of adjuvant endocrine therapy, and HER-2 status (data not shown). However, it was questionable whether these putative factors had similar prognostic value for ER−/PgR+ patients. We thus investigated the prognostic factors for ER−/PgR+ phenotype (Table 3). Only the numbers of involved lymph nodes was an independent factor of DFS/OS for ER−/PgR+ patients. Another important item, use of TAM treatment, had an insufficient prognostic value with a tendency of prognostic significance in OS (P = 0.078). Other items such as age, stage, and HER-2, did not provide enough prognostic value for ER−/PgR+ phenotype.
Discussion
The frequency of ER−/PgR+ tumors is about 2–7% in western breast cancer patients (Bernoux et al. 1998; Grann et al. 2005), 8% in Middle-East counterparts as reported (Kiani et al. 2006). In present study of China, the proportion was up to 11%. Since previous studies suggested that such hormonal receptor phenotype occurred more commonly in tumors of younger women and most Chinese breast cancer patients were premenopausal cases(Yu et al. 2007a), it might partly account for the higher frequency of ER−/PgR+ breast tumors in Chinese population. Besides, the patients with ER−/PgR+tumors were significantly different from those with ER+/PgR+ tumors regarding tumor size, stage, and lymph nodes involvement.
As most patients with ER−/PgR+ tumors are premenopausal cases and not candidates for AIs, it is thus quite important to evaluate the efficacy of adjuvant TAM treatment on such hormonal receptor subgroup. Grann et al. (2005) reported that the patients with ER−/PgR+ tumors had worse survival in terms of breast-cancer-specific mortality compared with those with ER+/PgR+ tumors. Bernoux et al. (1998) revealed that ER−/PgR+ group tended to have worse DFS than ER−/PgR− group. Dramatically, another study showed that the patients with ER−/PgR+ tumors had significantly worse survival than the other three hormonal receptor phenotypes (Keshgegian and Cnaan 1996). Regretfully, most studies just compared the survival outcomes directly without considering the heterogeneity of systemic therapies, especially endocrine therapies, among such groups. Heterogeneity, however, would surely compromise the reliability of conclusions. Thereafter, we compared the ER+/PgR+ group with ER−/PgR+ group in both non-TAM treated and TAM-treated patients on the basis of comparability between groups in most clinicopathologic features. Among non-TAM-treated patients, ER+/PgR+ group and ER−/PgR+ group had similar survival. Among TAM-treated patients, we observed that ER+/PgR+ and ER−/PgR+ group had improved 5-year survival, respectively. Moreover, we also found ER+/PgR+ group got more survival benefits than ER−/PgR+ group from adjuvant TAM.
Theoretically, the level of ER in tumor is determinative to its response to TAM. The phenomenon that patients with ER−/PgR+ tumors got more benefits from TAM, a selective estrogen receptor modulator, is mainly related to the absence or insufficiency of ER expression in tumor. Since, most ER negative tumors are ER insufficient, rather than absolutely ER absent ones, ER−/PgR+ tumors would still get benefit from TAM, although it was modest. Otherwise, the underlying mechanisms of anti-cancer effects of TAM via non-ER pathway still remain ambiguous (Levine 2003). In addition, we found that in those TAM-treated patients with ER−/PgR+ tumors, CMF seemed to be more effective than CA(E)F. It derived another question that whether different hormonal receptor phenotypes had their own optimal chemotherapeutic strategy. However, it is difficult to illuminate such an issue in a retrospective study. There is a need of rigorous prospective studies to evaluate the effectiveness of various chemotherapy regimens on different hormonal receptor phenotypes.
STEPP analysis was used to explore the patterns of differential survival tendency by varying age in ER+/PgR+ group and ER−/PgR+ group. These findings indicated that ER−/PgR+ patients with poorer survival tended to be younger and premenopausal. Moreover, differing from ER+/PgR+ phenotype, ER−/PgR+ patients had only a unique independent prognostic factor of axilla lymph nodes involvement for both DFS and OS. Using adjuvant TAM therapy or not, had a limited prognostic value, which is consistent with our findings that ER−/PgR+ group got less benefits from adjuvant TAM.
In conclusion, patients with ER−/PgR+ tumors were mainly premenopausal and younger, accounting for about 10% in Chinese breast cancer patients. Although patients with ER−/PgR+ tumors were generally considered as candidates for endocrine therapy clinically, ER−/PgR+ group gained less benefit from adjuvant TAM treatment compared with ER+/PgR+ group actually.
References
Bernoux A, de Cremoux P, Laine-Bidron C, Martin EC, Asselain B, Magdelenat H (1998) Estrogen receptor negative and progesterone receptor positive primary breast cancer: pathological characteristics and clinical outcome. Institut Curie Breast Cancer Study Group. Breast Cancer Res Treat 49:219–225
Bezwoda WR, Esser JD, Dansey R, Kessel I, Lange M (1991) The value of estrogen and progesterone receptor determinations in advanced breast cancer. Estrogen receptor level but not progesterone receptor level correlates with response to tamoxifen. Cancer 68:867–872
Bonetti M, Gelber RD (2000) A graphical method to assess treatment-covariate interactions using the Cox model on subsets of the data. Stat Med 19:2595–2609
Borras M, Lacroix M, Legros N, Leclercq G (1997) Estrogen receptor-negative/progesterone receptor-positive Evsa-T mammary tumor cells: a model for assessing the biological property of this peculiar phenotype of breast cancers. Cancer Lett 120:23–30
Cui X, Schiff R, Arpino G, Osborne CK, Lee AV (2005) Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol 23:7721–7735
Fanelli MA, Vargas-Roig LM, Gago FE, Tello O, Lucero De Angelis R, Ciocca DR (1996) Estrogen receptors, progesterone receptors, and cell proliferation in human breast cancer. Breast Cancer Res Treat 37:217–228
Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thurlimann B, Senn HJ (2005) Meeting highlights: international expert consensus on the primary therapy of early breast cancer 2005. Ann Oncol 16:1569–1583
Grann VR, Troxel AB, Zojwalla NJ, Jacobson JS, Hershman D, Neugut AI (2005) Hormone receptor status and survival in a population-based cohort of patients with breast carcinoma. Cancer 103:2241–2251
Jonat W, Pritchard KI, Sainsbury R, Klijn JG (2006) Trends in endocrine therapy and chemotherapy for early breast cancer: a focus on the premenopausal patient. J Cancer Res Clin Oncol 132:275–286
Keshgegian AA (1994) Biochemically estrogen receptor-negative, progesterone receptor-positive breast carcinoma. Immunocytochemical hormone receptors and prognostic factors. Arch Pathol Lab Med 118:240–244
Keshgegian AA, Cnaan A (1996) Estrogen receptor-negative, progesterone receptor-positive breast carcinoma: poor clinical outcome. Arch Pathol Lab Med 120:970–973
Kiani J, Khan A, Khawar H, Shuaib F, Pervez S (2006) Estrogen receptor alpha-negative and progesterone receptor-positive breast cancer: lab error or real entity? Pathol Oncol Res 12:223–227
Levine L (2003) Tamoxifen stimulates arachidonic acid release from rat liver cells by an estrogen receptor-independent, non-genomic mechanism. BMC Cancer 3:24
Nikolic-Vukosavljevic D, Kanjer K, Neskovic-Konstantinovic Z, Vukotic D (2002) Natural history of estrogen receptor-negative, progesterone receptor-positive breast cancer. Int J Biol Markers 17:196–200
Osborne CK (1998a) Tamoxifen in the treatment of breast cancer. N Engl J Med 339:1609–1618
Osborne CK (1998b) Steroid hormone receptors in breast cancer management. Breast Cancer Res Treat 51:227–238
Shimada A, Kimura S, Abe K, Nagasaki K, Adachi I, Yamaguchi K, Suzuki M, Nakajima T, Miller LS (1985) Immunocytochemical staining of estrogen receptor in paraffin sections of human breast cancer by use of monoclonal antibody: comparison with that in frozen sections. Proc Natl Acad Sci USA 82:4803–4807
Winer EP, Hudis C, Burstein HJ, Wolff AC, Pritchard KI, Ingle JN, Chlebowski RT, Gelber R, Edge SB, Gralow J, Cobleigh MA, Mamounas EP, Goldstein LJ, Whelan TJ, Powles TJ, Bryant J, Perkins C, Perotti J, Braun S, Langer AS, Browman GP, Somerfield MR (2005) American Society of Clinical Oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. J Clin Oncol 23:619–629
Yu KD, Di GH, Wu J, Lu JS, Shen KW, Shen ZZ, Shao ZM (2007a) Development and trends of Surgical Modalities for Breast Cancer in China: a review of 16-year data. Ann Surg Oncol 14:2502–2509
Yu KD, Liu GY, Di GH, Wu J, Lu JS, Shen KW, Shen ZZ, Shao ZM (2007b) Progesterone receptor status provides predictive value for adjuvant endocrine therapy in older estrogen receptor-positive breast cancer patients. Breast 16:307–315
Acknowledgment
This research was supported in part by the National Key Project of China (2001BA703BO5), and the grant from Shanghai Science and Technology Committee (06dj14004, 06DZ19504).
Author information
Authors and Affiliations
Corresponding author
Additional information
Yu Ke-da and Di Gen-hong have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yu, Kd., Di, Gh., Wu, J. et al. Breast cancer patients with estrogen receptor-negative/progesterone receptor-positive tumors: being younger and getting less benefit from adjuvant tamoxifen treatment. J Cancer Res Clin Oncol 134, 1347–1354 (2008). https://doi.org/10.1007/s00432-008-0414-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-008-0414-2