Abstract
Introduction: Radical prostatectomy and radiotherapy are currently accepted treatment modalities for localized prostate cancer. Regarding radiotherapy, current evidence suggests that favorable treatment outcome critically depends on adequate radiation doses. However, the exact role of dose in relation to the individual risk profile is complex. In order to evaluate available data on radiation dose response relationships, in prostate cancer, a thorough and critical literature analysis was performed. Material and methods: Studies on dose response relationships from randomized trials, dose escalation trials, retrospective subgroup analyses and pooled data were identified by Pubmed and ISI web of sciences searches and were critically reviewed. Results and conclusion: All available data suggest a clear dose response relationship for radiotherapy for localized prostate cancer. In low risk cases, most studies suggest that doses of 70–72 Gy are adequate. Dose escalations up to 78–80 Gy seem to be beneficial for intermediate risk patients. Due to confounding variables, the dose response curves for high-risk patients are less steep. The integration of dose escalation into a more comprehensive treatment protocol is difficult, since trials on the relative impact of either hormonal ablation or inclusion of adjuvant nodal regions on dose escalation are missing
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Population based trials and experience from larger centers show that adequately administered radiotherapy can achieve cure rates comparable to surgical treatment for localized prostate cancer within available follow-up periods (Chuba et al. 2001; Kupelian et al. 2002; Potosky et al. 2000). A recent retrospective analysis of 1,054 patients from a single center could demonstrate that, after correction of stage uncertainties, patients treated with an adequate dose have a long-term outcome, which is not distinct from those treated with surgery (Kupelian et al. 2002). Similar data were obtained after pooling data from two centers, although the mean follow-up time was somewhat shorter (Kupelian et al. 2004).
In addition, studies on quality of life and side effects prove that, despite a different spectrum of side effects, the overall impact of either treatment modality on the patients’ sense of well being is comparable (Kupelian et al. 2002; Madalinska et al. 2001; Wei et al. 2002). In this regard, surgically treated patients are reported to have a higher incidence of erectile dysfunction and urinary incontinence, whereas, radiation series report more rectal complications. Interestingly, the costs of radiotherapy seem to be substantially lower than those of surgical treatment (Burkhardt et al. 2002).
The issue of missing a pathological stage in patients undergoing primary radiation therapy remains problematic in developing a risk adapted treatment. However, nomograms or risk tables derived from surgical series allow an approximation of the risk of local extension and distant manifestations. Although some nomograms and equations derived from those data sets failed to prove the precise predication in prospective series, others were adequately predictive (Kattan et al. 2000). In merely all series, the predication of extraprostatic extension, seminal vesicle involvement, pelvic lymph node involvement and distant manifestations are derived from the clinical T stage, PSA level and Gleason grade of the biopsy [for review see (Ross et al. 2001)]. Based on these items, Roach et al. (2000) propagated a stratification of patients with prostate cancer into four different risk groups. Using the same parameters, other groups have suggested the separation into three different risk groups (Hanks et al. 2002; Kuban et al. 2003; Zelefsky et al. 2001).
Based on the individual risk profile, treatment strategies for localized prostate cancer have to cover issues of local control, prevention of distant spread and treatment of microscopic locoregional spread. Local control is critically important for the prevention of distant spread, since a second wave of “late” metastasis has occurred in patients with local failure (Coen et al. 2002).
Radiation based treatment options for localized prostate cancer generally include conformal three-dimensional (3D), CT planned percutaneous radiotherapy (Dearnaley et al. 1999; Pollack et al. 2000b; Zelefsky et al. 1998), intensity modulated conformal percutaneous radiotherapy (IMRT) (Kupelian et al. 2001b; Zelefsky et al. 2002) and various brachytherapy approaches either alone (Zelefsky et al. 1999) or in combination with external radiotherapy (Galalae et al. 2002; Singh et al. 2000).
In order to increase the efficacy of radiotherapy, two distinct approaches were tested: besides strategies, which basically rely on dose escalation, the combination with hormones has been proven to be suitable to increase local control and biochemical relapse-free interval rates. The issues of dose escalation will be covered in more detail in the following paragraphs.
Since the inclusion of androgen deprivation therapy increases local control, the results of four major trials on the combination of radiotherapy with androgen ablation should be shortly mentioned.
The EORTC randomized patients with locally advanced prostate cancer (cT1/2 G3 or cT3/4 all G and all cN1) to receive either 50 Gy to the pelvis and a 20-Gy boost to the prostate alone or in combination with 3.6 mg goserelin (Zoladex) subcutaneously every 4 weeks starting on the first day of irradiation and continuing for 3 years. A substantial benefit in terms of local control, disease specific survival and overall survival was noted for the combination arm (Bolla et al. 1997, 2002).
Less pronounced effects were seen in a similar RTOG trial (85–31), which randomized cT3 or pT3 or pN1 patients to receive goserelin 3.6 mg for 2 years starting in the last week of radiotherapy. Whereas, local control, and biochemical evidence of disease was significantly influenced by goserelin, an overall survival benefit was only seen in a subgroup analysis of patients with Gleason scores 8–10 (Lawton et al. 2001).
Another RTOG trial (86–10) randomized patients with bulky tumors (T2–T4) with or without pelvic lymph node involvement and without evidence of distant metastases to receive 3.6 mg goserelin every 4 weeks and flutamide for 2 months before and during radiation therapy (Pilepich et al. 2001). Subgroup analysis revealed that the beneficial effect of short-term androgen ablation occurs preferentially in patients with Gleason score 2–6, resulting in a highly significant improvement of all endpoints, including survival. In contrast, patients with Gleason 7–10 tumors had no improvement of locoregional control or survival (Pilepich et al. 2001). A combined analysis of both RTOG trials omitting the postoperative cases from 85–31 showed an advantage for longer hormone suppression when compared with the short term treatment in the 86–10 trial (Horwitz et al. 2001).
Recently published results from RTOG 94–13 (Roach et al. 2003) and 92–02 (Hanks et al. 2003) also underline that the addition of a neoadjuvant and long-term suppression of testosterone is advantageous in intermediate and high-risk patients.
Radiation dose may be an important factor in both local control of localized prostate cancer and treatment complications. First results from the pre PSA era showed significant dose effects depending on tumor stage and allowed a better understanding of factors, which influence outcome of prostate cancer patients (Hanks et al. 1988). Favored by improvements in radiation treatment technologies, numerous clinical trials on dose escalation strategies have been performed in order to optimize radiation therapy results.
The following review is based on two randomized trials, six dose escalation trials, five population-based, large single center analyses and five single center analyses partly considering special subgroups. Literature search was done using Pubmed and ISI Web of Science between 1985 and 2003 (search terms ‘prostate cancer’, ‘radiation‘ or ‘radiotherapy’, ‘dose response’, ‘dose escalation’) including abstracts performed at meetings of the ASTRO, ESTRO and ECCO.
Dose escalation
Basic considerations
It is a known fact that there is a dose response relationship for clinical control of localized prostate cancer. First reports from the mid eighties have revealed that higher radiation doses seemed to be necessary for local control of more advanced cancers (Chuba et al. 2001; Hanks et al. 1985).
The importance of this early observations was clearly underlined by findings from postirradiation biopsies performed much later in patients enrolled in a prospective phase I dose escalation trial at Memorial Sloan-Kettering Cancer Center (Levegrun et al. 2002; Zelefsky et al. 1998).
Between 1988 and 1998, 1,080 patients with stage T1c–T3 clinically localized adenocarcinoma of the prostate were treated with conformal photon beam 3D radiotherapy to doses between 64.8 and 81.0 Gy (four different dose levels). The outcome of 103 patients, who underwent postirradiation biopsies ≥2.5 years (median 3.3 years) after the end of treatment was analyzed. Patients who received androgen deprivation therapy at any time were excluded. The histological diagnosis of the prostate biopsy was classified as positive (without typical radiation-induced changes), negative (no evidence of carcinoma), or indeterminate (severe treatment effects). Only positive biopsies were considered as a failure, because studies of serial biopsies have reported that 52–85% of patients with an initial indeterminate biopsy after treatment resolved to negative upon subsequent biopsy (Crook et al. 1995; Prestidge et al. 1997).
In a bivariate analysis, Dmean and the risk group category were independent predictors of biopsy outcome for all evaluated risk group definitions. Values of TCD50 showed a clear separation of 9–10.6 Gy between low and high-risk patients, corresponding dose response curves were steeper (γ50=3.4–5.2) than those for all patients analyzed together (γ50=2.9). These data strongly support the assumption that eradication of prostate tumor cells is dose-dependent and may provide evidence that dose response varies by prognostic subgroup (Levegrun et al. 2002; Zelefsky et al. 1998).
A few years after the first paper on dose response correlations, it became evident that the achievement of local control is of critical importance not only for the local treatment of the disease, but also for overall survival, since local control is a critical denominator for the occurrence of distant metastasis (Coen et al. 2002; Fuks et al. 1991; Kuban et al. 1987; Zagars et al. 1991). In this regard, Zagars et al. (1991) showed that the actuarial incidence of metastases was significantly higher in patients, who could not be controlled locally. Local control was found to be a significant covariate in addition to stage and grade after multivariate Cox proportional hazard regression analysis of 679 patient data sets treated with I125 implants (Fuks et al. 1991).
Another approach was used by Kuban and coworkers. The failure pattern data of 647 patients were used to calculate the local survival advantage (LSA), which was calculated by multiplying the total local failure rates by the proportion of patients with local control, who did not have an isolated distant recurrence. It could be demonstrated that LSA was low (5%) for more localized tumors (A2 Jewett) and 16% for more advanced stages (C Jewett). The authors also concluded that local control significantly contributes to total disease control (Kuban et al. 1987). A recent paper confirmed this assumption by showing that locally uncontrolled cancer is related to increased distant metastasis in strong association with a “second wave” of metastatic seeding (Coen et al. 2002).
Randomized trials
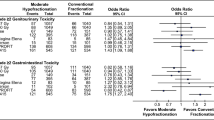
A randomized prospective trial remains the best study to answer clinical questions. However, only two randomized trials were performed addressing questions of radiation doses for prostate cancer (Pollack et al. 2000b, 2002; Shipley et al. 1995; Gardner et al. 2002) (Table 1). Importantly, patients receiving antihormonal treatment other than that for salvage treatment were excluded in both trials. The first trial included patients with T3–T4, Nx, N0–2, M0 patients. The patients were randomized to receive 50.4 Gy by four-field photons (including pelvic nodes) and either an additional 25.2 CGE by conformal protons (103 patients with a total dose of 75.6 CGE) or an additional 16.8 Gy Boost by conventional photons (99 patients, total dose 67.2 Gy). No significant differences in terms of overall survival (OS), disease free survival (DSS), and total recurrence free survival (TRFS) were detectable. However, a significant benefit of a higher radiation dose was detected when local control in patients with poorly differentiated tumors was analyzed. Local control at 8 years was achieved in 84% of the patients in the high dose group and only 19% in the conventional dose group (P=0.0014). The percentage of grade 1 and 2 rectal bleeding (32 vs 12%, P=0.002) and amount of urethral strictures (19 vs 8%, P=0.07) was higher in the dose escalated arm.
The results of the second randomized trial were published in 2000 (Pollack et al. 2000b) and updated in 2002 (Pollack et al. 2002). A total of 305 patients with T1–T3 stage tumors were randomized to receive 70 Gy or 78 Gy of external-beam radiotherapy. All patients were treated with a conventional photon four-field box up to 46 Gy. For those in the 70 Gy group, radiation was continued with reduced field size, whereas, those in the 78 Gy group received a six-field conformal boost using 3D treatment planning. Compared to the randomized trial reported by Shipley, more favorable to intermediate risk patients were enrolled. Stratification was based on pretreatment prostate-specific antigen level (PSA). Gleason scores were available for most patients. As stated above, no neoadjuvant or adjuvant antihormonal treatment was allowed. The most impressive result was that no differences in terms of freedom from biochemical/or disease failure (FFF) were detectable in the group of patients with a PSA ≤ 10 ng/ml.
Multivariate survival analysis using categorical variables revealed that pretreatment PSA (<10 vs >10 ng/ml), Gleason score (2–6 vs 7–10), randomization (70 vs 78 Gy) and T stage (T1/2 vs T3) were independent variables for outcome (FFF). The greatest effect of dose escalation was noted for those with a pretreatment PSA > 10 ng/ml, the FFF rate was 62% for the 78 Gy arm versus 43% for those who received 70 Gy (P=0.01). A similar relationship was not observed for Gleason score. In addition, grade 2 or higher rectal toxicity rates were significantly more common in the 78 Gy group (12 vs 26%, P=0.001). Grade 2 or higher bladder complications occurred in similar rates in both arms. The authors concluded that an increase of 8 Gy resulted in a significant improvement in FFF for patients at intermediate to high risk.
Dose escalation trials
After the initial observation of dose response relationships, several dose escalation trials were initiated (Bey et al. 2000; Hanks et al. 1998, 1999, 2002; Ryu et al. 2002; Zelefsky et al. 1998, 2001, 2002) (Table 2).
The data set provided by the Sloan–Kettering group is currently by far the largest. 1,100 patients were irradiated from 64.8 Gy in 5.4 Gy increments up to a dose of 86.4 Gy. A clear dose response was detectable for either PSA control and pathohistological clearance. It is important to notice that the benefit of dose escalation was not restricted to a certain risk profile.
In terms of histological clearance, which was analyzed in a proportion of the patients, 4 of 41 patients (10%), who received 81 Gy had a positive biopsy 2,5 years or greater after treatment. In comparison, 27 of 119 (23%) after 75.6 Gy, 23 of 68 (34%) after 70.2 Gy and 13 of 24 (54%) after 64.8 Gy were positive. Since dose escalation is potentially associated with an increased toxicity, the spectrum and severity of side effects was analyzed. As expected, the incidence of toxicity after 3D conformal radiation therapy was clearly related to the irradiation dose.
Subsequently, 772 patients were treated with IMRT only on the 81 and 86.4 Gy dose level. Basic aim of the trial was to validate the feasibility of IMRT in a larger set of patients. Thus, basically toxicity related endpoints were evaluated. The use of IMRT allowed dose escalation without a significant increase in toxicity (Table 2). In terms of efficacy, the authors reported 3-year actuarial bNED rates of 92, 86, and 81%, for favorable, intermediate, and unfavorable risk group patients, respectively.
Another important escalation trial was performed by Hanks et al. (1998, 1999, 2002) at the Fox Chase Center. The initial trial included 229 patients, who were treated with doses from 63 Gy to 79 Gy. The authors noticed that in patients with a PSA below 10 ng/ml no dose response was detectable for the estimated bNED or PSA nadir. However, in the PSA 10–19.9 ng/ml group, a bNED dose response was demonstrated. A logit response model revealed 5-year bNED estimates of 35% at 70 Gy and 75% at 76 Gy. Similar to the Sloan–Kettering trials, the overall rates of side effects were low (RTOG grade 3 or 4 gastrointestinal side effects for the whole collective at 5 years was <1%).
Another single-arm dose escalation study published in 2000 (Bey et al. 2000) was conducted at five French institutions. Among 120 patients, without neoadjuvant anti-hormonal therapy, results were compared among two groups, one group receiving 66–70 Gy (n=37) and the other group receiving 74–80 Gy (n=83). A clear dose response relationship (achieving a PSA nadir of ≤1 ng/ml) was demonstrated. No difference was observed regarding the incidence of late gastrointestinal and urinary toxicities.
The results of a further dose escalation trial performed at the University of Michigan were published in 2003 by Symon et al. (2003). After treatment with 3D conformal radiotherapy, 1,473 patients were analyzed regarding biochemical failure. A highly significant dose response relationship was seen for the intermediate risk patients, and the calculated hazard ratio from Cox regression model for this risk group demonstrated that each 1 Gy increment was associated with an 8% reduction in the probability of failure. Similar to the studies introduced above, no dose effect was seen for the low (T1–2, Gleason score ≤ 6, PSA ≤ 10 ng/ml) and high-risk (T3–4, Gleason score ≥ 8, PSA > 20 ng/ml) patients.
The RTOG trial (94–06) was conducted to determine the maximally tolerated dose using 3D conformal radiotherapy (Ryu et al. 2002). One hundred and seventy-three patients with T1/2 stage prostate cancer received 79.2 Gy. The minimum planning target volume (PTV) dose was limited to 73.8 Gy to reduce the rectal dose. With a median follow-up of 3.3 years the authors noted toxicity rates comparable to that reported for previous lower (68.4 and 73.8 Gy) dose levels. No patient experienced ≥ grade 3 acute toxicity, no grade 4 or 5 late toxicity occurred. A total of 4 (2.4%) patients developed grade 3 toxicity (three urinary, one rectal). Data on biochemical outcomes are not yet available.
Population-based, retrospective or pooled data analyses
Most of the data on dose responses in relation to disease stage are derived from retrospective analyses from various centers. Despite all known disadvantages of retrospective approaches, these published data are an extremely useful tool for clinical decision making (Tables 3 and 4).
One key study used the RTOG patient data base to answer the question to what extent radiation dose influences the outcome of prostate cancer patients (Valicenti et al. 2000). A total of 1,465 patients, who were treated in RTOG phase III trials with radiation therapy alone (77–06, 75–06, 86–10 and 85–31) was included. The patients received radiation doses between 60 Gy and 78 Gy. The dose variations resulted from the allowable prescribed doses within the study protocols and the final prescriptions for the individual patients (65–72 Gy). A median dose of 68.4 Gy was applied. The Cox multivariate analysis of factors associated with local progression, DSS and OS showed age, T stage, nodal status and Gleason score to be independently significant. The key finding of this study was that patients with Gleason scores from 8 to 10 had a significant benefit in terms of disease-specific and overall survival when receiving radiation doses above 66 Gy. Therefore, this finding is in good accordance with the observation from the randomized trial comparing the outcome with and without an addition proton boost, showing also that tumor grade influences outcome depending on radiation dose (Shipley et al. 1995). Unfortunately, PSA was not routinely determined at the time so that the influence of PSA cannot be determined in this regard.
Another retrospective analysis assessed dose response in high grade prostate cancers (Fiveash et al. 2000). The study population comprised 180 patients with all PSA levels (0.3–257 ng/ml), all T stages and Gleason scores 8–10. After stratification by dose level (<70 Gy vs 70–75 Gy vs >75 Gy), the following results were obtained: bNED rates (5 year) of the entire cohort were 55% versus 75% versus 58%. A significant benefit of a higher radiation dose was detected only for patients with T1–2 stages with bNED (2 years) rates of 94% versus 88% versus 68%, respectively. On multivariate analysis, in T1–2 stage patients, radiation dose and pretreatment PSA were found to be predictive for PSA failure.
Pollack et al. (2000a) summarized the results of 1,127 stage T1–4 prostate cancer patients treated with external beam radiotherapy at the M.D. Anderson Cancer Center. A total of 982 patients received a conventional four-field approach to 60–70 Gy. In 145 patients, conformal 3D treatment planning was employed to apply a boost dose to the prostate (74–78 Gy). Dose stratifications were ≤67, >67–77 and >77 Gy. A multivariate analysis revealed that dose (P= 0.0001) was an independent predictor of bNED. The actuarial bNED rates for all patients by dose group ≤67 Gy versus >67–77 Gy versus >77 Gy (50 months) were ~55%, ~70% (P<0.0001) and ~77% (P=0.10), respectively. A dose escalation from ≤67 Gy versus >67–77 G was associated with a benefit for all subgroups. In contrast, only favorable patients with a PSA > 10 ng/ml were shown to have a benefit of an additional dose escalation beyond 77 Gy. No such effect was seen in high-risk patients.
Kupelian et al. (2002) analyzed biochemical relapse-free survival rates after either external beam radiation or radical prostatectomy. The radiation group was additionally analyzed by comparing bNED outcomes in those treated with 68–71.9 Gy to those treated with 72–78 Gy. Regardless of any risk stratifications (Gleason ≥7 or/and PSA ≥ 10 or/and stage T2b–c) a clear dose response relationship with an improved biochemical outcome for the patients treated with a radiation dose ≥72 Gy could be demonstrated. Actuarial bNED rates (72 months) for unfavorable patients were ~46% versus ~83%.
Importantly, no differences of the bNED rates were detectable between patients after radical prostatectomy or curative radiotherapy, provided that doses above 72 Gy were applied. It has to be noticed that the radiotherapy group included significantly (P<0.001) fewer patients with favorable tumors.
Another study from the Fox Chase Cancer Center (Hanks et al. 2000), pooled data of 618 patients including the 229 patients enrolled in the first dose escalation trial. The favorable PSA<10 ng/ml subgroup was analyzed regarding effects of doses below and above 72.5 Gy, whereas, the cut-off for all other subgroups was set to 76 Gy.
Dose comparisons using Kaplan–Meier estimates showed significant differences in 5 year bNED for three subgroups (Table 3). However, no effects of increased radiation does were seen in patients with: PSA <10 ng/ml and no additional risk factor (< or >72.5 Gy), PSA 10–19.9 ng/ml and no additional risk factor (< or >76 Gy) and all patients with PSA ≥ 20 ng/ml and additional risk factors (< or >76 Gy). Similar results were obtained when the treatment efficacy of 73 Gy and 78 Gy was analyzed using calculation of dose response curves. When calculating a theoretical therapeutic benefit, the authors showed that a dose escalation of 5 Gy is associated with a 15–45% increase in 5 year bNED rate for various prognostic subgroups.
Since most of the studies available only documented dose response relationships for patients with a PSA above 10 ng/ml, a high Gleason score or existence of perineural invasion (PNI), Pinover et al. (2000) analyzed the Fox Chase Cancer Center cohort with pretreatment PSA levels ≤ 10 ng/ml (n=488). No significant dose response (stratification <72.5 vs 72.5–75.9 vs ≥76 Gy, median doses 70.7 vs 72.8 vs 77.3 Gy, respectively) was detectable for the entire group (5 year bNED 73% vs 86% vs 89%) and for good prognosis patients (T1–2a, Gleason score 2–6, no PVI, n=310) with bNED rates of 80, 86 and 91%, respectively. For the subgroup of poor prognosis patients (≥ one unfavorable risk factor), dose response was seen for those receiving ≥76 Gy compared to the lower dose groups (70% vs 75% vs 94%), and multivariate analysis for the poor prognosis subset demonstrated dose to be the only independent predictor for improved bNED.
Similar findings were presented by Hurwitz et al. (2002) comparing dose groups of <66 Gy versus 66.6 Gy versus >66.6 Gy in 264 low risk prostate cancer patients. Neither significant differences in (5 years) bNED rates between the three dose groups (79.2% vs 78.4% vs 84.5%) nor between two separately defined dose groups (≤65 Gy vs ≥68 Gy) were found. However, the issue of optimal radiation dose in patients with very favorable prostate cancers remains unsolved. In this regard Kupelian et al. (2001a) analyzed dose response relationships in 292 favorable patients with pretreatment PSA ≤ 10 ng/ml and Gleason score ≤ 6 and stage T1–2c. Patients were stratified by PSA (≤4 vs >4 ng/ml), Gleason score (≤5 vs 6), T stage (T1–2a vs T2b–c) and radiation dose (<72 vs ≥72 Gy), and the median radiation doses for the two stratification groups were 68 Gy and 78 Gy, respectively. In contrast to the Fox Chase good prognosis subgroup analysis and to the randomized M. D. Anderson dose escalation trial, but in accordance with the results from the Sloan–Kettering group, a significant dose response could be demonstrated with projected (5 and 8 years) bNED rates of 77% vs 95%. Also, PSA level was an independent predictor of outcome. A separate comparison between patients treated with 74 Gy (n=30) and those treated with 78 Gy (n=63) failed to demonstrate a dose response, thus the authors recommend 74 Gy for patients with a favorable risk constellation.
As mentioned above, the subgroup analysis in 103 patients on biopsy outcome as main endpoint (Levegrun et al. 2000, 2002) documented a clear evidence for dose response relationships depending on PSA (≤10 ng/ml vs >10 ng/ml), Gleason score (≤6 vs >6) and T stage (<T2c vs ≥T2c). The TCD50 values differed from low risk to intermediate risk and high-risk constellation with 64.7 versus 69.4 versus 74.1 Gy, respectively. The strongest effect on the TCD50value was documented for the T stage followed by the Gleason score. Despite having a lower impact on the TCD50 value when compared to T stage and Gleason score, the PSA level also was found to be important.
The results of the largest analysis on pooled data (including Cleveland, Fox Chase, Sloan–Kettering, M.D. Anderson and others) including 4,839 patients were published in 2003 by Kuban et al. (2003) and Thames et al. (2003). The median follow-up was 6.3 years and thus longer than follow-up periods in previous studies. Dose responses were analyzed after splitting the population into <70 Gy versus ≥70 Gy and <72 Gy versus ≥72 Gy dose groups. The bNED rate for the entire group was found to be 59% at 5 years and 53% at 8 years. When the analysis was restricted to patients who received doses ≥70 Gy, the actuarial bNED rates were 61% and 55%. Multivariate analysis using categorical variables revealed that pretreatment PSA, Gleason score, radiation dose, T stage and treatment year were independent variables for biochemical outcome. For low risk patients, no clear dose response effect was seen (cutpoint 70 Gy and 72 Gy). Similarly, no dose response was detectable in patients with a high-risk profile using a 70 Gy cut-off. Pronounced dose effects were documented for the intermediate risk group (both cut points) and to a lesser degree in the high-risk group using the 72 Gy cut-off. The bNED (8 years) rates for the intermediate risk patients were ~52% versus ~60% (70 Gy cut-off) ~50% versus ~64% (72 Gy cut-off).
Discussion
All available data provide a clear evidence for a dose response relationship in radiotherapy of prostate cancer. This conclusion is supported by results from clinical trials using bNED and disease free survival as endpoint and also pathohistological data on prostate cancer eradication. Therefore, strategies of dose escalation, which were suggested at least 25 years ago, can now be considered to be effective.
Nevertheless, multiple problems still remain unsolved. The most important problem relates to the long natural history of prostate cancer making it difficult to determine which type of local therapy is best in men with life expectancies longer than 8–10 years at diagnosis. Although bNED is frequently used as surrogate endpoint, biochemical failure is still not an the optimal predictor of mortality at 10 years after definitive therapy. Thus a long-term follow-up with overall survival endpoints is still needed.
In regard to radiotherapy strategies, one of the key issues is the question which patients benefit from dose escalation. Although the most evident effects of dose escalation could be observed in intermediate risk patients, the situation is definitively more complex. In this regard, the given heterogeneity within a certain risk group mandates a more detailed analysis. Using the initial PSA, Gleason score and T stage, the group of low risk patients generally is defined as: cT1c–T2a, PSA ≤ 10 ng/ml and Gleason ≤ 6. Most data available suggest that increases of the radiation dose beyond 70–72 Gy do not significantly increase the control probability. This interpretation is supported by data from the randomized M.D. Anderson Trial, most dose escalation trials and the analysis of defined subgroups from pooled patient groups or single centers (Hurwitz et al. 2002; Pinover et al. 2000; Pollack et al. 2000a, b). In addition, the calculated TCD50 value of 64.7 Gy with an associated γ50 of 37 fits well into the required dose range of clinical results (Levegrun et al. 2002).
However, a least two studies support the assumption that higher doses may also be required for low risk patients. The analysis of the pathohistological results from the MSKCC dose escalation trial undoubtly revealed an increased pathological clearance in relation to increased radiation doses, also in low risk patients (Zelefsky et al. 2001). In addition, in his retrospective analysis Kupelian et al. (2001a) revealed a significant improvement of bNED even in low risk patients. Hence, it is reasonable to assume that a dose of 70 Gy represents the lower threshold of the dose range for low risk patients and 74 Gy probably is a more aggressive upper limit. The presence of other risk factors, e.g., perineural invasion or number of positive biopsies may be of assistance in creating subgroups within the low risk group, which might require different doses. Regarding target volumes for patients with a low risk profile, an adequate coverage of the prostate without seminal vesicles seems to be reasonable (Kestin et al. 2002).
A different picture emerges when the dose response for patients with a more advanced risk constellation is analyzed. All data including results from retrospective, pooled and also randomized studies show that at least a PSA level above 10 ng/ml or higher Gleason scores require higher doses for adequate control. Depending on the prognostic predictors T stage, PSA level and Gleason score with three consecutive risk group definitions, the strongest dose response relationships were seen in patients at intermediate risk. Although the definition of risk groups are not consistent in many trials, most commonly patients with PSA levels from >0 ng/ml to <20 ng/ml or presence of one risk factor including a higher T stage (>T2a <T4) or Gleason score (>6) are considered to represent the intermediate risk population. In fact, all available data demonstrate that increasing radiation doses beyond 70–72 Gy significantly increased the control probability.
Although all data unequivocally show a dose response for intermediate risk patients, the optimal upper dose level is not known yet. Data from the dose escalation trials support the interpretation that even doses above ~77 Gy may increase the treatment efficacy. In accordance with these clinical observations, the pathohistological results from the MSKCC dose escalation trial demonstrate the lowest rate of positive biopsies in patients who received the highest radiation dose with 81 Gy (Zelefsky et al. 2001). The derived TCD50 value of 69.4 Gy is well compatible with the clinically observed dose responses. (Levegrun et al. 2002). However, the question in how far doses of 86 Gy as used by Zelefsky really increase the bNED rate remains to be clarified.
Besides all issues on dose responses other important variables have to be taken into account in order to define an optimal treatment approach for intermediate risk patients. In this regard, it has been shown that the probability of locoregional spread increases with T stage, PSA level and Gleason score. The randomized RTOG 94–13 trial could show that for a calculated risk of nodal involvement exceeding 15%, the pelvic nodes should be included into the target volume.
Many patients treated as intermediate risk patients have a calculated risk of ≥15% of locoregional spread. Two competing approaches are therefore available. Up to now, no study has been done in order to test the open question whether dose escalation alone, in combination with irradiation of pelvic or in combination with hormonal ablation is optimal. In order to circumvent the evident problem, several institutions implement node-sampling strategies prior to a radiotherapy of the prostate alone (Fossa et al. 2003). However, this practice has not been evaluated in a larger setting.
In addition to the open question on target volume, patients with an intermediate risk constellation were shown to benefit from an additional concomitant and adjuvant hormonal blockade. In most trials on dose escalation, hormonal manipulations were strictly excluded. It remains therefore unclear up to what extent a dose escalation is effective when additional hormonal measures are integrated into the therapeutic concept. Again, no prospective trial on this special issue is available. In a retrospective analysis, Nguyen and co-workers showed that, at least for high-risk patients, the addition of short-term hormone ablation during radiotherapy did not complement for a lacking dose (Nguyen et al. 2003). It seems therefore possible that both approaches in combination will turn out to be more active. It has to be taken into account that the combination of radiotherapy with long-term hormonal ablation is associated with small but reproducible increase in rectal toxicity (Hanks et al. 2003). Therefore, dose escalation in combination with hormonal ablation should be performed with caution.
The problem of competing risks is even higher in patients with more advanced prostate cancer, since locoregional and systemic spread are major limiting factors. Thus, the dose response curves for patients in advance stages were shown to be less steep. The most widely accepted approaches for these patients are to combine radiotherapy with adjuvant coverage of the pelvic nodes and a long-term hormonal suppression. It has not been evaluated prospectively if an additional dose escalation increases the efficacy in this setting.
Taken together, it seems reasonable to assume that radiation doses between 70 Gy and 74 Gy are sufficient for low risk prostate cancer. Patients with an intermediate risk profile benefit from a dose escalation. Based on available data, no clear cut recommendation regarding target volume (prostate only vs inclusion of pelvic nodes), additional hormonal treatments (no vs short-term vs long-term) or staging lymphadenectomy (no vs yes) can be derived. However, all data suggest that doses above 74 Gy seem to be advisable. For high-risk patients, a currently accepted treatment option is radiotherapy with 70 Gy to the prostate, 45–50.4 Gy to the pelvic nodes and long-term hormonal ablation.
For future research, several key issues have to be distinguished. Although few studies already reported on late toxicity (36 month), it is mandatory to further closely follow the development of late toxicities in patients after dose escalation. In this regard, late toxicity to the urethra may turn out to be dose limiting. In this regard, long-term follow-up data of the initial proton dose escalation trial suggest that even after long-time periods, the incidence of hematuria raises steadily (Gardner et al. 2002; Shipley et al. 1995). It is therefore important to develop strategies, which will reduce the probability of urinary side effects. In this regard, IMRT based dose escalation restricted to partial volumes of the prostate shown to contain the highest tumor burden would be a potentially interesting strategy. Pickett et al. (Pickett et al. 1999) employed MRT spectroscopy data in order to define a 90-Gy boost volume within the prostate. It can also be speculated that other parameters, including choline PET CT data or hypoxia derived PET markers may guide dose escalation strategies. In addition to technological improvements, further clinical studies determining the relative value of either hormonal blockade or dose escalation alone or in combination are required.
References
Bey P, Carrie C, Beckendorf V, Ginestet C, Aletti P, Madelis G, Luporsi E, Pommier P, Cowen D, Gonzague-Casabianca L, Simonian-Sauve M, Maingon P, Naudy S, Lagrange J, Marcie S (2000) Dose escalation with 3D-CRT in prostate cancer: French study of dose escalation with conformal 3D radiotherapy in prostate cancer-preliminary results. Int J Radiat Oncol Biol Phys 48:513–517
Bolla M, Gonzalez D, Warde P, Dubois JB, Mirimanoff RO, Storme G, Bernier J, Kuten A, Sternberg C, Gil T, Collette L, Pierart M (1997) Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N Engl J Med 337:295–300
Bolla M, Collette L, Blank L, Warde P, Dubois JB, Mirimanoff RO, Storme G, Bernier J, Kuten A, Sternberg C, Mattelaer J, Lopez Torecilla J, Pfeffer JR, Lino Cutajar C, Zurlo A, Pierart M (2002) Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet 360:103–106
Burkhardt JH, Litwin MS, Rose CM, Correa RJ, Sunshine JH, Hogan C, Hayman JA (2002) Comparing the costs of radiation therapy and radical prostatectomy for the initial treatment of early-stage prostate cancer. J Clin Oncol 20:2869–2875
Chuba PJ, Moughan J, Forman JD, Owen J, Hanks G (2001) The 1989 patterns of care study for prostate cancer: five-year outcomes. Int J Radiat Oncol Biol Phys 50:325–334
Coen JJ, Zietman AL, Thakral H, Shipley WU (2002) Radical radiation for localized prostate cancer: local persistence of disease results in a late wave of metastases. J Clin Oncol 20:3199–3205
Crook JM, Perry GA, Robertson S, Esche BA (1995) Routine prostate biopsies following radiotherapy for prostate cancer: results for 226 patients. Urology 45:624–31; discussion 631–632
Dearnaley DP, Khoo VS, Norman AR, Meyer L, Nahum A, Tait D, Yarnold J, Horwich A (1999) Comparison of radiation side-effects of conformal and conventional radiotherapy in prostate cancer: a randomised trial. Lancet 353:267–272
Fiveash JB, Hanks G, Roach M, Wang S, Vigneault E, McLaughlin PW, Sandler HM (2000) 3D conformal radiation therapy (3DCRT) for high grade prostate cancer: a multi-institutional review. Int J Radiat Oncol Biol Phys 47:335–342
Fossa SD, Lilleby W, Waehre H, Berner A, Torlakovic G, Paus E, Olsen DR (2003) Definitive radiotherapy of prostate cancer: the possible role of staging lymphadenectomy. Int J Radiat Oncol Biol Phys 57:33–41
Fuks Z, Leibel SA, Wallner KE, Begg CB, Fair WR, Anderson LL, Hilaris BS, Whitmore WF (1991) The effect of local control on metastatic dissemination in carcinoma of the prostate: long-term results in patients treated with 125I implantation. Int J Radiat Oncol Biol Phys 21:537–547
Galalae RM, Kovacs G, Schultze J, Loch T, Rzehak P, Wilhelm R, Bertermann H, Buschbeck B, Kohr P, Kimmig B (2002) Long-term outcome after elective irradiation of the pelvic lymphatics and local dose escalation using high-dose-rate brachytherapy for locally advanced prostate cancer. Int J Radiat Oncol Biol Phys 52:81–90
Gardner BG, Zietman AL, Shipley WU, Skowronski UE, McManus P (2002) Late normal tissue sequelae in the second decade after high dose radiation therapy with combined photons and conformal protons for locally advanced prostate cancer. J Urol 167:123–126
Hanks GE, Leibel SA, Krall JM, Kramer S (1985) Patterns of care studies: dose-response observations for local control of adenocarcinoma of the prostate. Int J Radiat Oncol Biol Phys 11:153–157
Hanks GE, Martz KL, Diamond JJ (1988) The effect of dose on local control of prostate cancer. Int J Radiat Oncol Biol Phys 15:1299–1305
Hanks GE, Hanlon AL, Schultheiss TE, Pinover WH, Movsas B, Epstein BE, Hunt MA (1998) Dose escalation with 3D conformal treatment: five year outcomes, treatment optimization, and future directions. Int J Radiat Oncol Biol Phys 41:501–510
Hanks GE, Hanlon AL, Pinover WH, Horwitz EM, Schultheiss TE (1999) Survival advantage for prostate cancer patients treated with high-dose three-dimensional conformal radiotherapy. Cancer J Sci Am 5:152–158
Hanks GE, Hanlon AL, Pinover WH, Horwitz EM, Price RA, Schultheiss T (2000) Dose selection for prostate cancer patients based on dose comparison and dose response studies. Int J Radiat Oncol Biol Phys 46:823–832
Hanks GE, Hanlon AL, Epstein B, Horwitz EM (2002) Dose response in prostate cancer with 8–12 years’ follow-up. Int J Radiat Oncol Biol Phys 54:427–435
Hanks GE, Pajak TF, Porter A, Grignon D, Brereton H, Venkatesan V, Horwitz EM, Lawton C, Rosenthal SA, Sandler HM, Shipley WU (2003) Phase III trial of long-term adjuvant androgen deprivation after neoadjuvant hormonal cytoreduction and radiotherapy in locally advanced carcinoma of the prostate: the Radiation Therapy Oncology Group Protocol 92–02. J Clin Oncol 21:3972–3978
Horwitz EM, Winter K, Hanks GE, Lawton CA, Russell AH, Machtay M (2001) Subset analysis of RTOG 85–31 and 86–10 indicates an advantage for long-term vs. short-term adjuvant hormones for patients with locally advanced nonmetastatic prostate cancer treated with radiation therapy. Int J Radiat Oncol Biol Phys 49:947–956
Hurwitz MD, Schnieder L, Manola J, Beard CJ, Kaplan ID, D’Amico AV (2002) Lack of radiation dose response for patients with low-risk clinically localized prostate cancer: a retrospective analysis. Int J Radiat Oncol Biol Phys 53:1106–1110
Kattan MW, Zelefsky MJ, Kupelian PA, Scardino PT, Fuks Z, Leibel SA (2000) Pretreatment nomogram for predicting the outcome of three-dimensional conformal radiotherapy in prostate cancer. J Clin Oncol 18:3352–3359
Kestin L, Goldstein N, Vicini F, Yan D, Korman H, Martinez A (2002) Treatment of prostate cancer with radiotherapy: should the entire seminal vesicles be included in the clinical target volume? Int J Radiat Oncol Biol Phys 54:686–697
Kuban DA, el-Mahdi AM, Schellhammer PF (1987) Effect of local tumor control on distant metastasis and survival in prostatic adenocarcinoma. Urology 30:420–426
Kuban DA, Thames HD, Levy LB, Horwitz EM, Kupelian PA, Martinez AA, Michalski JM, Pisansky TM, Sandler HM, Shipley WU, Zelefsky MJ, Zietman AL (2003) Long-term multi-institutional analysis of stage T1–T2 prostate cancer treated with radiotherapy in the PSA era. Int J Radiat Oncol Biol Phys 57:915–928
Kupelian PA, Buchsbaum JC, Reddy CA, Klein EA (2001a) Radiation dose response in patients with favorable localized prostate cancer (Stage T1–T2, biopsy Gleason < or =6, and pretreatment prostate-specific antigen < or =10). Int J Radiat Oncol Biol Phys 50:621–625
Kupelian PA, Reddy CA, Klein EA, Willoughby TR (2001b) Short-course intensity-modulated radiotherapy (70 GY at 2.5 GY per fraction) for localized prostate cancer: preliminary results on late toxicity and quality of life. Int J Radiat Oncol Biol Phys 51:988–993
Kupelian PA, Elshaikh M, Reddy CA, Zippe C, Klein EA (2002) Comparison of the efficacy of local therapies for localized prostate cancer in the prostate-specific antigen era: a large single-institution experience with radical prostatectomy and external-beam radiotherapy. J Clin Oncol 20:3376–3385
Kupelian PA, Potters L, Khuntia D, Ciezki JP, Reddy CA, Reuther AM, Carlson TP, Klein EA (2004) Radical prostatectomy, external beam radiotherapy <72 Gy, external beam radiotherapy > or =72 Gy, permanent seed implantation, or combined seeds/external beam radiotherapy for stage T1–T2 prostate cancer. Int J Radiat Oncol Biol Phys 58:25–33
Lawton CA, Winter K, Murray K, Machtay M, Mesic JB, Hanks GE, Coughlin CT, Pilepich MV (2001) Updated results of the phase III Radiation Therapy Oncology Group (RTOG) trial 85–31 evaluating the potential benefit of androgen suppression following standard radiation therapy for unfavorable prognosis carcinoma of the prostate. Int J Radiat Oncol Biol Phys 49:937–946
Levegrun S, Jackson A, Zelefsky MJ, Venkatraman ES, Skwarchuk MW, Schlegel W, Fuks Z, Leibel SA, Ling CC (2000) Analysis of biopsy outcome after three-dimensional conformal radiation therapy of prostate cancer using dose-distribution variables and tumor control probability models. Int J Radiat Oncol Biol Phys 47:1245–1260
Levegrun S, Jackson A, Zelefsky MJ, Venkatraman ES, Skwarchuk MW, Schlegel W, Fuks Z, Leibel SA, Ling CC (2002) Risk group dependence of dose-response for biopsy outcome after three-dimensional conformal radiation therapy of prostate cancer. Radiother Oncol 63:11–26
Madalinska JB, Essink-Bot ML, de Koning HJ, Kirkels WJ, van der Maas PJ, Schroder FH (2001) Health-related quality-of-life effects of radical prostatectomy and primary radiotherapy for screen-detected or clinically diagnosed localized prostate cancer. J Clin Oncol 19:1619–1628
Nguyen KH, Horwitz EM, Hanlon AL, Uzzo RG, Pollack A (2003) Does short-term androgen deprivation substitute for radiation dose in the treatment of high-risk prostate cancer? Int J Radiat Oncol Biol Phys 57:377–383
Pickett B, Vigneault E, Kurhanewicz J, Verhey L, Roach M (1999) Static field intensity modulation to treat a dominant intra-prostatic lesion to 90 Gy compared to seven field 3-dimensional radiotherapy. Int J Radiat Oncol Biol Phys 44:921–929
Pilepich MV, Winter K, John MJ, Mesic JB, Sause W, Rubin P, Lawton C, Machtay M, Grignon D (2001) Phase III radiation therapy oncology group (RTOG) trial 86–10 of androgen deprivation adjuvant to definitive radiotherapy in locally advanced carcinoma of the prostate. Int J Radiat Oncol Biol Phys 50:1243–1252
Pinover WH, Hanlon AL, Horwitz EM, Hanks GE (2000) Defining the appropriate radiation dose for pretreatment PSA < or = 10 ng/ml prostate cancer. Int J Radiat Oncol Biol Phys 47:649–654
Pollack A, Smith LG, von Eschenbach AC (2000a) External beam radiotherapy dose response characteristics of 1127 men with prostate cancer treated in the PSA era. Int J Radiat Oncol Biol Phys 48:507–512
Pollack A, Zagars GK, Smith LG, Lee JJ, von Eschenbach AC, Antolak JA, Starkschall G, Rosen I (2000b) Preliminary results of a randomized radiotherapy dose-escalation study comparing 70 Gy with 78 Gy for prostate cancer. J Clin Oncol 18:3904–3911
Pollack A, Zagars GK, Starkschall G, Antolak JA, Lee JJ, Huang E, von Eschenbach AC, Kuban DA, Rosen I (2002) Prostate cancer radiation dose response: results of the M. D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys 53:1097–1105
Potosky AL, Legler J, Albertsen PC, Stanford JL, Gilliland FD, Hamilton AS, Eley JW, Stephenson RA, Harlan LC (2000) Health outcomes after prostatectomy or radiotherapy for prostate cancer: results from the prostate cancer outcomes study. J Natl Cancer Inst 92:1582–1592
Prestidge BR, Hoak DC, Grimm PD, Ragde H, Cavanagh W, Blasko JC (1997) Posttreatment biopsy results following interstitial brachytherapy in early-stage prostate cancer. Int J Radiat Oncol Biol Phys 37:31–39
Roach M, Lu J, Pilepich MV, Asbell SO, Mohiuddin M, Terry R, Grignon D, Mohuidden M (2000) Four prognostic groups predict long-term survival from prostate cancer following radiotherapy alone on Radiation Therapy Oncology Group clinical trials. Int J Radiat Oncol Biol Phys 47:609–615
Roach M III, DeSilvio M, Lawton C, Uhl V, Machtay M, Seider MJ, Rotman M, Jones C, Asbell SO, Valicenti RK, Han S, Thomas CR Jr, Shipley WS (2003) Phase III trial comparing whole-pelvic versus prostate-only radiotherapy and neoadjuvant versus adjuvant combined androgen suppression: Radiation Therapy Oncology Group 9413. J Clin Oncol 21:1904–1911
Ross PL, Scardino PT, Kattan MW (2001) A catalog of prostate cancer nomograms. J Urol 165:1562–1568
Ryu JK, Winter K, Michalski JM, Purdy JA, Markoe AM, Earle JD, Perez CA, Roach M, Sandler HM, Pollack A, Cox JD (2002) Interim report of toxicity from 3D conformal radiation therapy (3D-CRT) for prostate cancer on 3DOG/RTOG 9406, level III (79.2 Gy). Int J Radiat Oncol Biol Phys 54:1036–1046
Shipley WU, Verhey LJ, Munzenrider JE, Suit HD, Urie MM, McManus PL, Young RH, Shipley JW, Zietman AL, Biggs PJ et al (1995) Advanced prostate cancer: the results of a randomized comparative trial of high dose irradiation boosting with conformal protons compared with conventional dose irradiation using photons alone. Int J Radiat Oncol Biol Phys 32:3–12
Singh A, Zelefsky MJ, Raben A, Lombardi D, Leibel SA (2000) Combined 3-dimensional conformal radiotherapy and transperineal Pd-103 permanent implantation for patients with intermediate and unfavorable risk prostate cancer. Int J Cancer 90:275–280
Symon Z, Griffith KA, McLaughlin PW, Sullivan M, Sandler HM (2003) Dose escalation for localized prostate cancer: substantial benefit observed with 3D conformal therapy. Int J Radiat Oncol Biol Phys 57:384–390
Thames H, Kuban D, Levy L, Horwitz EM, Kupelian P, Martinez A, Michalski J, Pisansky T, Sandler H, Shipley W, Zelefsky M, Zietman A (2003) Comparison of alternative biochemical failure definitions based on clinical outcome in 4839 prostate cancer patients treated by external beam radiotherapy between 1986 and 1995. Int J Radiat Oncol Biol Phys 57:929–943
Valicenti R, Lu J, Pilepich M, Asbell S, Grignon D (2000) Survival advantage from higher-dose radiation therapy for clinically localized prostate cancer treated on the Radiation Therapy Oncology Group trials. J Clin Oncol 18:2740–2746
Wei JT, Dunn RL, Sandler HM, McLaughlin PW, Montie JE, Litwin MS, Nyquist L, Sanda MG (2002) Comprehensive comparison of health-related quality of life after contemporary therapies for localized prostate cancer. J Clin Oncol 20:557–566
Zagars GK, von Eschenbach AC, Ayala AG, Schultheiss TE, Sherman NE (1991) The influence of local control on metastatic dissemination of prostate cancer treated by external beam megavoltage radiation therapy. Cancer 68:2370–2377
Zelefsky MJ, Leibel SA, Gaudin PB, Kutcher GJ, Fleshner NE, Venkatramen ES, Reuter VE, Fair WR, Ling CC, Fuks Z (1998) Dose escalation with three-dimensional conformal radiation therapy affects the outcome in prostate cancer. Int J Radiat Oncol Biol Phys 41:491–500
Zelefsky MJ, Wallner KE, Ling CC, Raben A, Hollister T, Wolfe T, Grann A, Gaudin P, Fuks Z, Leibel SA (1999) Comparison of the 5-year outcome and morbidity of three-dimensional conformal radiotherapy versus transperineal permanent iodine-125 implantation for early-stage prostatic cancer. J Clin Oncol 17:517–522
Zelefsky MJ, Fuks Z, Hunt M, Lee HJ, Lombardi D, Ling CC, Reuter VE, Venkatraman ES, Leibel SA (2001) High dose radiation delivered by intensity modulated conformal radiotherapy improves the outcome of localized prostate cancer. J Urol 166:876–881
Zelefsky MJ, Fuks Z, Hunt M, Yamada Y, Marion C, Ling CC, Amols H, Venkatraman ES, Leibel SA (2002) High-dose intensity modulated radiation therapy for prostate cancer: early toxicity and biochemical outcome in 772 patients. Int J Radiat Oncol Biol Phys 53:1111–1116
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganswindt, U., Paulsen, F., Anastasiadis, A.G. et al. 70 Gy or more: which dose for which prostate cancer?. J Cancer Res Clin Oncol 131, 407–419 (2005). https://doi.org/10.1007/s00432-005-0681-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-005-0681-0