Abstract
Purpose: This prospective study evaluates the diagnostic potential of Cytokeratin 20 (CK 20) RT-PCR for the detection of disseminated tumor cells in bone marrow and blood of a large cohort of patients with ductal adenocarcinoma of the pancreas and the prognostic value on overall survival prediction. Methods: Between 1994 and 2003, 172 patients (83 male, 89 female; 13–82 years) with pancreatic ductal adenocarcinoma underwent surgery. Bone marrow samples and venous blood were taken preoperatively and analyzed for disseminated tumor cells by nested CK 20 RT-PCR. Results: Disseminated tumor cells were detected in 81 (47.1%) of the 172 patients in the bone marrow and/or the venous blood. Overall, in 45 of the 135 (33.3%) bone marrow samples and in 52 of the 154 (33.8%) blood samples, CK 20 positive cells were detected. Detection rates increased with the UICC-tumor stage. According to Kaplan-Meier, univariate survival analysis of all 172 patients (n=78 R0-; n=18 R1- and n=5 R2-resected; n=71 palliative surgery) showed a statistically significant relationship of overall survival to radicality of the operation (P<0.0001), the UICC-stage of the tumors (P=0.0011) and the detection of disseminated tumor cells in bone marrow and/or venous blood (P=0.05). Patients with well- and moderately- differentiated tumors (G1 and G2) had a significantly longer survival (P=0.045) than patients suffering from poorly differentiated tumors (G3). A positive CK 20 status in the bone marrow and/or blood within the group of patients with G1 and G2 tumors had a significantly negative prognostic impact on their survival (P=0.046). Conclusions: Disseminated tumor cells can be detected in patients with pancreatic ductal adenocarcinoma by CK 20 RT-PCR. Detection rates are stage dependent, and survival analysis demonstrated statistically relevant data. From a clinical point of view, this finding is especially noteworthy for the group of well- and moderately-differentiated tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although operation techniques, multimodal treatment and lower postoperative mortality could improve overall 5-year survival rates of patients with pancreatic carcinoma, survival remains poor (Cameron et al. 1993; Yeo et al. 1995). Only 20% of the patients diagnosed with pancreatic head carcinoma can be resected with a curative intention (Bramhall et al. 1995). But even in these patients, tumor recurrence is frequent because of early lymphatic and hematogenous spread and consecutive development of distant metastases, local recurrence and peritoneal seeding.
Assessment of lymph node status as an indicator for tumor dissemination is routinely performed by histopathological examination. Tumor-associated antigens and/or tissue-specific markers have been used to detect disseminated tumor cells in immunohistochemical analyses and have also improved the results of detection by conventional cytology (Hosch et al. 1997). Molecular biological approaches have been developed in recent years and focused mainly on tumor-specific antigens and tissue-specific markers (Ando et al. 1997; Brown et al. 2001; Demeure et al. 1998; Tamagawa et al. 1997). Additionally, other compartments like bone marrow, blood and peritoneal lavage have been analyzed for minimal residual disease (Aihara et al. 1997; Heeckt et al. 1992; Vogel et al. 1999).
Owing to the variations in patient selection, methods and differences in detection rates in these studies, the prognostic impact of disseminated tumor cell detection in patients with ductal adenocarcinoma of the pancreas is still a matter of debate.
We have previously demonstrated that disseminated tumor cells in patients with pancreatic carcinoma can be detected by nested CK 20 RT-PCR (Soeth et al. 1997).
The aim of this study was to evaluate the detection of disseminated tumor cells in the bone marrow and the venous blood in the largest group of patients suffering from pancreatic ductal adenocarcinoma analyzed so far in this context and to determine the prognostic impact of these findings.
Methods
Patients
Between 1994 and 2003, 172 patients, with histologically proven ductal adenocarcinoma of the pancreas participated in this study. All patients underwent an explorative laparotomy and the decision, whether Whipple procedure, pylorus preserving resection or left resection (n=101), or palliative bypass surgery (n=71) was performed, was made by the surgeon during the operation. All patients were preoperatively informed about the study and gave their written consent.
In 78 patients (45.3%) a curative resection (R0) was performed. In 18 patients (10.5%) the definitive histological examination revealed a R1 resection. In 5 patients (2.9%) only a R2 resection could be reached and 71 patients (41.3%) obtained a palliative surgery. The UICC-stages (5th edition 1997) of the 172 resected patients were the following:
UICC-stage I: 10 (5.8%); II: 19 (11.1%); III: 51 (29.6%); IV: 92 (53.5%). Survival times on follow-up of these patients ranged between 4 months and 69 months (mean: 15.9 months, median 11 months).
Bone marrow and blood samples
After general anesthesia and prior to the operation, 10 ml of bone marrow were aspirated from the right iliac crest (anticoagulant: Lithium-Heparin).
Additionally, 20 ml of blood were taken from a central venous line directly before the operation (anticoagulant: Lithium-Heparin).
Isolation of total RNA
The mononuclear cell fraction was isolated by Ficoll-Isopaque (Amersham, Braunschweig, Germany) density-gradient centrifugation and then lysed in peq GOLD RNAPureTM (peqLab GmbH, Erlangen, Germany) and stored at −80°C. RNA isolation was performed according to the manufacturer’s directions. Finally, the total RNA was dissolved in 20 μl of RNAse-free water, and quality and yield were determined by agarose gel electrophoresis and absorption measurement at 260 and 280 nm (Biophotometer, Eppendorf, Germany), respectively.
CK 20 RT-PCR
The total RNA (2.0 μg) in a volume of 10 μl was denatured for 10 min at 70°C and quickly chilled on ice. The cDNA was synthesized in a total volume of 20 μl containing 5x first-strand buffer, 2 mM DTT, 200 U of SuperScript II (all from Invitrogen, Karlsruhe, Germany), 4 U of RNase inhibitor, 2.5 μM random hexamer primers, 0.5 mM of each deoxynucleotide triphosphate (all from Applied Biosystems, Weiterstadt, Germany). Incubation for 10 min at 24°C and 60 min at 42°C was followed by an inactivation step for 5 min at 95°C. PCR primers were synthesized by MWG-Biotech, Ebersberg, Germany:
-
CK 20-A sense, 5′-GCGTTTATGGGGGTGCTGGAG;
-
CK 20-B antisense, 5′- AAGGCTCTGGGAGGTGCGTCTC;
-
CK 20-C sense, 5′-CGGCGGGGACCTGTTTGT;
-
CK 20-D antisense, 5′-CAGTGTTGCCCAGATGCTTGTG;
-
GAPDH sense, 5′-CCAGCCGAGCCACATCGCTC;
-
and GAPDH antisense, 5′-ATGAGCCCCAGCCTTCTCCAT.
The PCR procedure was performed as previously described (Soeth et al. 1996, 1997).
Evaluation criteria
The samples were tested at least twice. If a CK 20 signal was detected in at least one test, the sample was judged as positive.
Controls
Bone marrow samples of 68 patients without malignancies were evaluated by CK 20 RT-PCR. In eight (11.8%) of these samples, a positive signal could be detected (two patients with colitis ulcerosa, two patients with pseudotumors of the lung, two patients with chronic pancreatitis, two patients with benign tumors of the liver).
In the venous blood samples in nine of 54 patients (16.7%), we also observed a positive signal (four patients with chronic pancreatitis, one patient with an adenoma of the papilla vateri, two patients with benign liver tumors, one patient with benign stenosis of the choledochus, one patient with a benign lung tumor).
In 20 blood samples of healthy controls, only one blood sample gave a positive signal.
Statistical analysis
The statistical analysis was performed using SPSS version 11.0 for windows PC.
Survival was analyzed using the method of Kaplan-Meier. Survival statistics in the cohort of patients were evaluated by the use of the log-rank test.
Results
Bone marrow samples and venous blood samples of 172 patients with ductal adenocarcinoma of the pancreas were analyzed by CK 20 RT-PCR. In 117 patients (68.0%), a PCR result in bone marrow and venous blood was obtained, while in 55 patients (32.0%) results from only one compartment could be introduced into the study. These included PCR results from 18 (10.5%) bone marrow samples and 37 (21.5%) blood samples. A CK 20 signal was detected in 81 (47.1%) of the 172 patients in bone marrow and/or venous blood samples. Analyzing either compartment alone, in 45 (33.3%) of the 135 bone marrow samples disseminated tumor cells were detected, while in 52 (33.8%) of the 154 blood samples tumor cells were found.
Table 1 shows the distribution of CK 20-positive results in bone marrow, blood and bone marrow and/or blood of all investigated patients in correlation to the patient’s age and gender and the clinical characteristics R (residual tumor) stage, TNM stage (UICC 1997) and tumor grade.
Focusing on the analyses of CK 20-positive bone marrow and/or blood findings, the detection rates were not significantly different regarding age and gender of the patients or the R stage and the grading of the primary tumor. However, detection rates were increased in patients with lymph node metastases compared to patients without positive lymph nodes, and patients with liver or peritoneal metastases did also show a higher rate of CK 20-positivity compared to patients without distant metastases.
In contrast to the aforementioned weak correlation, detection rates of disseminated tumor cells in bone marrow, blood and bone marrow and/or blood clearly increased with the increment of the UICC-stage. Figure 1 demonstrates the results of the statistical analysis (t test) of the different subgroups according to their CK 20 detection rate and the UICC-stage. In every subgroup the CK 20 detection rates increased significantly from the combined early stages I and II (UICC I/II) to stage III and stage IV, while the CK 20 detection rates between stage III and stage IV were only significant in the tested blood samples but not in the other both subgroups.
Detection rate of disseminated tumor cells in blood and bone marrow of patients with pancreatic carcinoma in dependence on the UICC-classification. Results of UICC-stages I and II are combined and presented by the white columns, while stage III and stage IV are shown in hatched and black, respectively. The first set of three columns refers to all analyzed bone marrow samples (n=135), the second set to all analyzed blood samples (n=154) and the third to all patients analyzed (n=172)
Concordance of bone marrow and blood results
Of 117/172 patients (68.0%) paired samples of bone marrow and blood could be analyzed (Table 2). In 47.9% (56/117) identical negative results and in 13.7% (16/117) identical positive results for both compartments were observed. Overall 61.5% (72/117) identical results for both compartments were found.
The prevalence of CK 20-positive findings in either bone marrow (23/117) or blood (22/117) samples of the paired samples was 38.5% (45/117). In this subgroup the detection rate for tumor cells in the bone marrow and/or blood was 52.1% (61/117), in bone marrow 33.3% (39/117) and in the blood 32.5% (38/117).
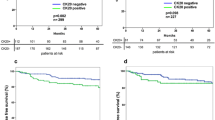
Prognostic value of the clinical characteristics
Survival analysis demonstrated that the age and the gender of the patients had no significant influence on their survival. On the other hand, R stage (P≤0.0001), the UICC-tumor stage (P=0.0011), the nodal stage (N0/N1, P=0.0005) and distant metastasis (M0/M1, P≤0.0001) significantly influenced the patients’ overall survival. The tumor differentiation did also significantly influence the patient survival as demonstrated in Fig. 2. In this analysis 159 patients were included with 117 patients in the grade 1/grade 2 group and 42 in the grade 3 group. Patients with well- or moderately-differentiated tumors (grade 1 or grade 2) had a significantly longer survival (P=0.045) compared to patients suffering from poorly differentiated grade 3 tumors. The mean survival time of patients suffering from grade 1 or grade 2 tumors was 25.2 months compared to 15.9 months for patients with grade 3 tumors.
Overall survival rate of patients (n=159) with pancreatic ductal carcinoma in dependence on the tumor differentiation. The patients with well- and moderately-differentiated tumors (grade 1 and grade 2; n=117; thin line) are compared with patients with poorly differentiated tumors (grade 3; n=42; bold line). The difference in survival with an advantage for patients with a grade 1 or grade 2 tumor compared to a grade 3 tumor was statistically significant (P=0.045)
Prognostic value of the detection of disseminated tumor cells by CK 20 RT-PCR
The Kaplan-Meier survival analysis of the subgroup of patients with CK 20-positive bone marrow and/or blood samples versus negative-tested patients demonstrated a statistically significant longer survival (P=0.05) of negative-tested patients (Fig. 3). The mean survival time of CK 20-positive-tested patients was 17.9 months compared to 26.1 months for the CK 20-negative-tested patient group.
Overall survival rate of patients (n=172) with pancreatic ductal carcinoma in dependence on the detection of disseminated tumor cells in the bone marrow and/or the blood. CK 20-negative patients (n=91; thin line) were compared to CK 20-positive individuals (n=81; bold line). The difference in survival showing an advantage for the negatively tested patients was statistically significant (P=0.05)
The analysis of the CK 20 status in the bone marrow and/or blood can also refine the survival prognosis for patients with grade 1 or grade 2 tumors. Figure 4 shows this survival analysis demonstrating that CK 20-positive-tested patients had a statistically significant shorter overall survival compared to CK 20-negative patients with grade 1 or grade 2 tumors (P=0.046). The mean survival time of CK 20-positive tested patients was 19.7 months compared to 29.9 months in the CK 20-negative-tested patients.
Overall survival rate of pancreatic ductal carcinoma patients (n=117) with well- or moderately-differentiated (grade 1 or grade 2) tumors in dependence on the detection of disseminated tumor cells in the bone marrow and/or the blood. CK 20-negative results (n=64; thin line) were compared with CK 20-positive results (n=53; bold line). The difference in survival with an advantage for the negatively tested patients was statistically significant (P=0.046)
Discussion
Ductal adenocarcinoma of the pancreas is associated with the worst prognosis even after curative resection. Patients die due to early metastasis or local recurrence. More sensitive staging methods need to be developed especially for this kind of tumor entity.
Several groups observed tumor cells in histopathologically negative lymph nodes of patients with pancreatic carcinoma, using immunocytological or PCR-based applications (Hosch et al. 1997; Kanemitsu et al. 2003; Niedergethmann et al. 2002; Ridwelski et al. 2001). It was shown that single aberrant cells can be detected with staining or molecular biological methods in patients’ compartments, like the bone marrow, blood and the peritoneal cavity (Burchill et al. 1995, 1999; Roder et al. 1999; Soeth et al. 1997; Van Heeck et al. 2001; Vogel et al. 1999; Z’graggen et al. 2001).
The detection of minimal residual disease raises the question whether patients are really sufficiently treated by the surgical procedure alone or whether an adjuvant chemotherapy should be suggested (Beger et al. 2003).
In previous studies we demonstrated that CK 20 can be used for the detection of disseminated tumor cells in colorectal carcinoma, and also for gastric and pancreatic carcinoma (Soeth et al. 1997). Our aim was supported by the finding that CK 20 is highly expressed in malignant ductal cancer cells of pancreatic carcinoma (Wildi et al. 1999). Therefore, we extended our investigations with this marker in a prospective study to pancreatic carcinoma patients.
To the best of our knowledge, this is the largest cohort of patients analyzed for disseminated tumor cells in pancreatic carcinoma using a molecular biological approach. The detection rates in the bone marrow (33.3%) and in the blood (33.8%) were almost equal and increased significantly with the advanced UICC-stages. This is in concordance with other studies mainly investigating peritoneal washes of patients suffering from pancreatic carcinoma (Fernandez-del Castillo et al. 1995; Konishi et al. 2002; Vogel et al. 1999; Yachida et al. 2002).
Investigating the bone marrow and the blood of the same patient increased the detection rate from 33% in each single compartment to 52% in the combined set. So far we did not examine whether the doubling of the volume of one specimen, bone marrow or blood, respectively, will end up with the same increment of overall detection and statistical significant data. If this turns out to be the case, then one might replace the bone marrow aspiration by investigating a larger amount of blood RNA which is the much more easily accessible clinical sample.
We could demonstrate a significant benefit in the survival of patients tested CK 20-negatively in bone marrow and/or blood samples (P=0.05). This is one out of an only limited number of univariate studies investigating the long-term survival of pancreatic carcinoma patients with significant outcome (Roder et al. 1999; Thorban et al. 1996, Vogel et al. 1999). To our knowledge, it is the only one yielding statistically significant data using a molecular biology-based approach.
Besides the objective parameters: tumor stage, UICC-tumor stage, nodal stage and distant metastases, also the more “subjective” grading system proposed in the classification of the WHO (Klöppel et al. 1996) significantly influenced and predicted the survival of the patients. Our present investigation on 159 patients concerning the tumor grading extends and supports a previous study with 70 patients from our university clinic (Lüttges et al. 2000). We could demonstrate a significant benefit in the survival of patients suffering from less aggressive grade 1 or grade 2 tumors compared to highly aggressive grade 3 tumors (P=0.045). The CK 20 RT-PCR analysis on patients with well- and moderately-differentiated tumors enabled us to divide this group in patients with a more promising (CK 20-negative) versus a poorer prognosis (CK 20-positive) with respect to survival (P=0.046). We therefore strongly suggest including such an analysis of the tumor cell dissemination in the decision process for further therapeutic strategies, e.g., adjuvant chemotherapy, at least of patients resected from grade 1 or grade 2 tumors.
In contrast to the subgroup identified with the CK 20 RT-PCR in well- and moderately-differentiated tumors, we were unable to identify a relevance of the detection of MRD in the early tumor stages I and II. So far no statistically significant results were obtained. However, the mean survival time in the CK 20-positively tested patient cohort (n=8) was 28.1 months in contrast to 47.7 months in the CK 20-negatively tested patient group (n=21). The lack of statistical significance might be explained by the small number of available patients with stage I and II (n=29) disease.
In conclusion, our data suggest that CK 20 positive tumor cells can be detected in patients with ductal pancreatic carcinoma in bone marrow and venous blood by using a molecular biological approach. In the group of patients, which is to our knowledge the largest group analyzed so far, our data reveal tumor cells as detectable in the circulation at a relatively early stage of the disease. The prevalence of isolated tumor cells in blood increases significantly with the UICC-tumor stage.
The survival analyses of resected patients demonstrated a prognostic impact of the detection of CK 20 positive cells in bone marrow and/or blood.
References
Aihara T, Noguchi S, Ishikawa O, Furukawa H, Hiratsuka M, Ohigashi H, Nakamori S, Monden M, Imaoka S (1997) Detection of pancreatic and gastric cancer cells in peripheral and portal blood by amplification of keratin 19 mRNA with reverse transcriptase-polymerase chain reaction. Int J Cancer 72:408–411
Ando N, Nakao A, Nomoto S, Takeda S, Kaneko T, Kurokawa, Nonami T, Takagi H (1997) Detection of mutant K-ras in dissected paraaortic lymph nodes of patients with pancreatic adenocarcinoma. Pancreas 15:374–378
Beger HG, Rau B, Gansauge F, Poch B, Link K-H (2003) Treatment of pancreatic cancer: challenge of the facts. World J Surg 27:1075–1084
Bramhall SR, Allum WH, Jones AG, Allwood A, Cummins C, Neoptolemos JP (1995) Treatment and survival in 13560 patients with pancreatic cancer, and incidence of the disease, in the West Midlands: an epidemiological study. Br J Surg 82:111–115
Brown HM, Ahrendt SA, Komorowski RA, Doffek KM, Wilson SD, Demeure MJ (2001) Immunhistochemistry and molecular detection of nodal micrometastases in pancreatic cancer. J Surg Res 95:141–146
Burchill SA, Bradbury MF, Pittman K, Southgate J, Smith B, Selby P (1995) Detection of epithelial cancer cells in peripheral blood by reverse transcriptase-polymerase chain reaction. Br J Cancer 71:278–281
Burchill SA, Lewis IJ, Selby P (1999) Improved methods using the reverse transcriptase polymerase chain reaction to detect tumor cells. Br J Cancer 79:971–977
Cameron JL, Pitt HA, Yeo CJ, Lillemore KD, Kaufmann HS, Coleman JA (1993) One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg 217:430–435
Demeure MJ, Doffek KM, Komorowski RA, Wilson SD (1998) Adenocarcinoma of the pancreas: detection of occult metastases in regional lymph nodes by a polymerase chain reaction-based assay. Cancer 83:1328–1334
Fernandez-del Castillo C, Rattner DW, Warshaw AL (1995) Further experience with laparoscopy and peritoneal cytology in the staging of pancreatic cancer. Br J Surg 82:1127–1129
Heeckt P, Safi F, Binder T, Bücheler M (1992) Freie intraperitoneale Tumorzellen beim Pankreascarzinom-Bedeutung für den klinischen Verlauf und die Therapie. Chirurg 63:563–567
Hosch SB, Knoefel WT, Metz S, Stoeklein N, Niendorf A, Broelsch CE, Itzbicki JR (1997) Early lymphhatic tumor cell dissemination in pancreatic cancer: Frequency and prognostic significance. Pancreas 15:154–159
Kanemitsu K, Hiraoka T, Tsuji T, Inoue K, Takamori H (2003) Implication of micrometastases of lymph nodes in patients with extended operation for pancreatic cancer. Pancreas 26:315–321
Klöppel G, Solcia E, Longnecker DS, Capella C, Sobin LH (1996) Histological typing of tumours of the exocrine pancreas. WHO International histological classification of tumours, 2nd edn. Springer, Berlin Heidelberg New York
Konishi M, Kinoshita T, Nakagohri T, Inoue K, Oda T, Takahashi S (2002) Prognostic value of cytologic examination of peritoneal washings in pancreatic cancer. Arch Surg 137:475–480
Lüttges J, Schemm S, Vogel I, Hedderich J, Kremer B, Klöppel G (2000) The grade of pancreatic ductal carcinoma is an independent prognostic factor and is superior to the immunohistolchemical assessment of proliferation. J Pathol 191:154–161
Niedergethmann M, Rexin M, Hildenbrand R, Knob S, Stum JW, Richter A, Post S (2002) Prognostic impact of routine, immunohistchemical, and molecular staging in respectable pancreatic adenocarcinoma. Am J Surg Pathol 26:1578–1587
Ridwelski K, Meyer F, Fahlke J, Kasper U, Roessner A, Lippert H (2001) Stellenwert von Cytokeratin- und CA19–9 Antigen im immunhistologischen Nachweis disseminierter Tumorzellen in Lymphknoten beim Pankreaskarzinom. Chirurg 72:920–926
Roder JD, Thorban S, Pantel K, Siewert JR (1999) Micrometastases in bone marrow: prognostic indicators for pancreatic cancer. World J Surg 23:888–891
Soeth E, Röder C, Juhl H, Krüger U, Kremer B, Kalthoff H (1996) The detection of disseminated tumor cells in bone marrow from colorectal-cancer patients by a cytokeratin-20-specific nested reverse-transcriptase-polymerase-chain reaction is related to the stage of disease. Int J Cancer 69:278–282
Soeth E, Vogel I, Röder C, Juhl H, Marxsen J, Krüger U, Henne-Bruns D, Kremer B, Kalthoff H (1997) Comparative analysis of bone marrow and venous blood isolates from gastrointestinal cancer patients for the detection of disseminated tumor cells using reverse transcription PCR. Cancer Res 57:3106–3110
Tamagawa E, Ueda M, Takahashi S, Sugano K, Uematsu S, Mukai M, Ogata Y, Kitajima M (1997) Pancreatic lymph nodal and plexus micrometastases detected by enriched polymerase chain reaction and nonradioisotopic single strand conformation polymorphism analysis: a new predictive factor for recurrent pancreatic carcinoma. Clin Cancer Res 3:2143–2149
Thorban S, Roder JD, Pantel K, Siewert JR (1996) Epithelial tumor cells in bone marrow of patients with pancreatic carcinoma detected by immunocytochemical staining. Eur J Cancer 32:363–365
Van Heeck NT, Tascilar M, Beekveld JL, Drilenburg P, Offerhaus GJA, Gouma DJ (2001) Micrometastases in bone marrow of patients with suspected pancreatic and ampullary cancer. EJS0 27:740–745
Vogel I, Krüger U, Marxsen J, Soeth E, Kalthoff H, Henne-Bruns D, Kremer B, Juhl H (1999) Disseminated tumor cells in pancreatic cancer patients detected by immunocytology: a new prognostic factor. Clin Cancer Res 5:593–599
Wildi S, Kleeff J, Maruyama H, Maurer CA, Friess H, Buchler MW, Lander AD, Korc M (1999) Characterization of cytokeratin 20 expression in pancreatic and colorectal cancer. Clin Cancer Res 5:2840–2847
Yachida S, Fukushima M, Sakamoto M, Matsuno Y, Kosuge T, Hirohashi S (2002) Implications of peritoneal washing cytology in patients with potentially resectable pancreatic cancer. Br J Surg 89:573–578
Yeo CJ, Cameron JL, Lillemoe KD, Sitzmann JV, Hruban RH, Goodman SN, Dooley WC, Coleman J, Pitt HA (1995) Pancreaticoduodenectomy for cancer of the head of the pancreas: 201 patients. Ann Surg 221:721–731
Z’graggen K, Centeno BA, Fernandez-del Castillo C, Jimenez RE, Werner J, Warshaw AL (2001) Biological implications of tumor cells in blood and bone marrow of pancreatic cancer patients. Surgery 129:537–546
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soeth, E., Grigoleit, U., Moellmann, B. et al. Detection of tumor cell dissemination in pancreatic ductal carcinoma patients by CK 20 RT-PCR indicates poor survival. J Cancer Res Clin Oncol 131, 669–676 (2005). https://doi.org/10.1007/s00432-005-0008-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-005-0008-1