Abstract
Relapses of steroid-sensitive nephrotic syndrome are traditionally treated with prednisone 2 mg/kg/day or 60 mg/m2/day. Retrospective data support the use of lower doses. We designed a prospective randomized pilot study to investigate the efficacy of different doses in achieving remission of steroid sensitive nephrotic syndrome relapse. The cohort included 30 children with relapsed steroid sensitive nephrotic syndrome, mean age 6.3 ± 3 years and mean disease duration 2.2 ± 1.8 years. The children were randomized to receive 2, 1.5, or 1 mg/kg/day prednisone. The corresponding times to response, defined as the first of 3 consecutive days without proteinuria, were 7.2 ± 1.4, 10.2 ± 5.1, and 9 ± 3.3 days; the difference between the 1.5 and 2 mg/kg/day groups was statistically significant. One patient each in the 1 mg/kg/day and the 1.5 mg/kg/day groups failed to respond and were switched to 2 mg/kg/day, leading to a response after 3 and 10 days, respectively. Mean cumulative prednisone doses in the 3 groups were 45.5 ± 3.4, 42.7 ± 25.9, and 24.9 ± 7.4 mg/kg, respectively (P < 0.05).
Conclusion: In the present study, treatment of childhood steroid sensitive nephrotic syndrome relapse with prednisone 1–1.5 mg/kg/day led to a significantly lower cumulative dose than the standard dose. Treatment with a lower dose may be equally safe and effective to the standard dose.
What is Known: | |
• Relapses of steroid-sensitive nephrotic syndrome are traditionally treated with standard-dose steroids. | |
• Treatment with corticosteroids may have significant adverse effects mainly with long-term use. | |
What is New: | |
• Treatment of steroid sensitive nephrotic syndrome relapse with 1–1.5 mg/kg/day prednisone may lead to a significantly lower cumulative dose. | |
• Treatment with a lower steroid dose may be as effective as the standard dose in achieving remission of steroid sensitive nephrotic syndrome relapse. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic steroid-sensitive nephrotic syndrome (SSNS) is the most common chronic glomerular disease of childhood [3, 4, 12]. Prednisone has been the first-line therapeutic option for SSNS for the last 50 years. About 90% of patients respond to prednisone treatment, but 60% have recurrent episodes [3].
The early International Study of Kidney Disease in Children clearly showed that a prednisone dose of 60 mg/m2 or 2 mg/kg/day was effective in achieving remission of relapsed SSNS [5, 12]. However, it caused significant adverse effects in frequent relapsing and steroid-dependent patients who needed repeated steroid courses, and about 20–30% of patients required steroid-sparing medications [3, 5, 12]. High daily doses of prednisone are associated with more side effects [1], and higher cumulative doses have been found to strongly correlate with behavioral side effects [7].
In young children, there is a significant difference between prednisone dose based on body weight (2 mg/kg/day) and dose based on body surface area (60 mg/m2/day), sometimes reaching 20%. Nevertheless, studies have reported no significant difference in outcomes [6, 10]. Several observational and retrospective studies suggested that doses lower than the accepted 60 mg/m2 of prednisone may be equally beneficial for relapses of SSNS [2, 8, 9, 11]. Surveys among pediatric nephrologists in Canada [11] and across Europe [2] reported wide variability in prednisone dosing. A retrospective multi-center analysis showed up to threefold variation in prednisone dose [8]. Another retrospective study investigated the effect of 1 mg/kg/day of prednisone in 50 patients treated for 87 relapses of SSNS and found that 70% of patients responded within 7 days and 77%, within10 days [9].
However, there are no randomized controlled studies of the effect of different prednisone doses on relapses of idiopathic childhood SSNS in terms of the rate of remission, time to remission, total prednisone dose, and other factors. The present pilot study was designed to fill this gap. The aim of the study was to compare the efficacy of three different prednisone doses in achieving short-term remission in relapsing childhood SSNS.
Methods
A prospective randomized controlled design was used. The cohort included patients aged 1–18 years with a relapse of SSNS who were being followed at the nephrology clinic of a tertiary pediatric medical center from August 2014 to December 2016. Only those who were not receiving prednisone at the time of relapse and had never before received other immunosuppressive drugs were enrolled. In previous exacerbations, all patients were advised to receive the standard prednisone dose of 2 mg/kg/day. Relapse was defined as proteinuria on dipstick test (> 3+) accompanied by protein/creatinine ratio > 2 mg/mg and/or serum albumin < 3 g/dl and/or edema.
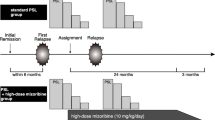
Patients were divided into three prednisone treatment groups in running order of enrollment, as follows: first patient, 2 mg/kg/day; second, 1.5 mg/kg/day; third, 1 mg/kg; and so forth (Fig. 1). Patients and clinicians were informed about prednisone dose only after randomization. Remission was defined as negative/trace protein on urine dipstick test for 3 consecutive days. Patients who failed to achieve remission on the lower doses after 14 days were switched to 2 mg/kg/day.
After remission was achieved, the prednisone dose was tapered down as follows:
2-mg/kg group, dose was reduced to 1.5 mg/kg every other day for 2 weeks; then in 10 mg decrements every 2 weeks until a dose of 10–15 mg every other day was achieved; and then to 5 mg every other day for 2 weeks. Overall, patients received an average of 10–12 weeks’ treatment.
1.5-mg/kg group, dose was reduced to 1 mg/kg every other day for 2 weeks; then in 10 mg decrements every 2 weeks until a dose of 10–15 mg every other day was achieved; then to 5 mg every other day for 2 weeks. Overall, patients received an average of 8–10 weeks’ treatment.
1-mg/kg group, dose was reduced to 1 mg/kg every other day for 2 weeks; then in 10 mg decrements every 2 weeks until a dose of 10–15 mg/every other day was reached; and then to 5 mg every other day for 2 weeks. Overall, patients received an average of 8–10 weeks’ treatment.
We calculated the cumulative prednisone dose during the study period based on data from the patient’s clinical charts.
All patients were followed for 6 months from the day of recruitment, including the duration of prednisone treatment and 3-month post-treatment. Decisions regarding further treatment after completion of the regimen (start steroid sparing/continue low-dose steroids/observation alone) were made by the treating nephrologist.
The primary outcome measure was the total prednisone cumulative dose in the three dose groups. The secondary outcome measure was the time to achieve short-term remission and number of patients achieving remission.
Intention-to-treat statistical analysis was performed. The groups were compared for background factors, time to response, and rate of failure during the treatment regimens using one-way analysis of variance (ANOVA). Differences among the three groups were analyzed with Kruskal-Wallis test, and between any two groups, with Mann-Whitney test. A P value of < 0.05 was considered significant.
For power calculations, we used G* power 3.0.10 software. For a sample of 30 divided into 3 groups, the power in one-way ANOVA was 0.97. We performed the test with an effect size of 0.8 while our effect size was higher than 1.
The study was approved by the local Helsinki committee and the Israel Ministry of Health. Written informed consent was obtained from the parents of all participants.
Results
Thirty children met the inclusion criteria. The randomization is shown in Fig. 1. Background characteristics of the cohort are shown in Table 1. There were no significant differences among the groups in any of the background characteristics.
One patient in the 1 mg/kg/day group and one in the 1.5 mg/kg/day group failed to respond after 14 days. Both were switched to 2 mg/kg/day and achieved a response after an additional 3 and 10 days, respectively.
The mean cumulative doses of prednisone per body weight during treatment were 45.5 ± 3.4 mg/kg in the 2 mg/kg/day group, 42.7 ± 25.9 mg/kg in the 1.5 mg/kg/day group, and 24.9 ± 7.4 mg/kg in the 1 mg/kg/day group. The difference was statistically significant between the 1 mg/kg/day and 1.5 mg/kg/day groups (P = 0.007), the 1 mg/kg/day and 2 mg/kg/day groups (P < 0.001), and the 1.5 mg/kg/day and 2 mg/kg/day groups (P = 0.024).
Analysis of previous disease exacerbations yielded a mean time of 6.8 ± 0.9 days to response for the whole cohort, with no significant differences between groups (P = 0.5).
The mean and median times to remission are shown in Table 2. The difference in means was statistically significant between the 2 and 1.5 mg/kg/day groups (P = 0.04) but not between the 2 mg/kg/day and 1 mg/kg/day groups. The median times (Table 2) were almost uniform among the groups. None of the patients had treatment-related complications.
Table 3 summarizes the findings during 3 months after completion of the prednisone regimen. The rate of sustained remission was similar in the three groups. However, given that 27% of the cohort received continued treatment with either a low prednisone dose or a steroid-sparing drug, the effect of the regimen on future relapses could not be reliably analyzed.
Discussion
The present study of children with a relapse of SSNS showed that those treated with a low prednisone dose of 1 mg/kg/day or 1.5 mg/kg/day achieved a similar clinical response to those treated with the standard dose. The cumulative dose was significantly lower (by 25–50%) in the lower-dose groups than the highest-dose group. There was only a small difference in the cumulative dose between the 1.5 mg/kg/day and the 2 mg/kg/day groups, but the standard deviation in the 1.5 mg/kg/day group was wide, probably owing to the particularly prolonged time to response of one patient who received a 3.3-fold higher dose than rest of the group. This point is noteworthy because most of the children benefited from the low prednisone dose, and the difference was statistically significant.
To our knowledge, this is the first prospective randomized controlled study comparing three prednisone doses for the treatment of relapsed SSNS. Our results are in line with a recent retrospective uncontrolled analysis which documented a 77% response rate to a prednisone dose of 1 mg/kg/day [9].
Time to achievement of remission is an important factor in the treatment of childhood SSNS. A longer response time may be associated with complications of the disease itself and with longer exposure to high daily prednisone dose. We found that time to response did not change during the relapse events evaluated in this study or in previous disease exacerbations in the same patients despite the fact that two-thirds of the cohort had received higher prednisone doses in previous exacerbations. Comparison of the time to achieve remission among the groups yielded a significant difference between the 1.5 and the 2 mg/kg/day groups in mean values but not in median values or range. This may be explained by the intent-to-treat statistical analysis: one nonresponding patient from the 1.5 mg/kg/day group remained in that group even after he was switched to 2 mg/kg/day.
These findings, together with the significantly lower cumulative dose in the low-dose groups, suggest that the standard prednisone dose, and consequently, the total patient exposure to prednisone, can be decreased in children with relapsed SNSS without adverse clinical consequences.
Our study was not designed to measure differences in the subsequent relapse rate because the inclusion criteria did not consider the patients’ long-term therapy plan. Nevertheless, we found that the number of patients who remained in remission 3 months after completion of treatment was similar in all three groups.
Our study was limited by the single-center setting and small number of patients. Although the difference in the mean cumulative prednisone dose between the study groups reached statistical significance, a larger multicenter study is needed to confirm these results. Another limitation concerns the randomization process since right after randomization both patients and physicians were aware of the prednisone dose.
In addition, larger and, importantly, longer and well-designed studies are needed to analyze differences by prednisone dose in subsequent relapse rates and the occurrence of side effects.
Conclusion
The present prospective randomized controlled pilot study showed that treatment of a relapse of childhood SSNS with a lower-than-standard prednisone dose led to a significantly lower cumulative dose. Treatment with a lower dose may be as safe and effective as the standard dose. We need to proceed with similar studies to determine the optimal and individually adjusted prednisone dose in this patient group.
Abbreviations
- SNSS:
-
steroid-sensitive nephrotic syndrome
References
Buchman AL (2001) Side effects of corticosteroid therapy. J Clin Gastroenterol 33:289–294
Deschênes G, Vivarelli M, Peruzzi L, ESPN Working Group on Idiopathic Nephrotic Syndrome (2017) Variability of diagnostic criteria and treatment of idiopathic nephrotic syndrome across European countries. Eur J Pediatr 176:647–654. https://doi.org/10.1007/s00431-017-2891-2892
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, Wigfall D, Miles P, Powell L, Lin JJ, Trachtman H, Greenbaum LA (2009) Management of childhood onset nephrotic syndrome. Pediatrics 124:747–757. https://doi.org/10.1542/peds.2008-1559
Lombel RM, Gipson DS, Hodson EM, Kidney Disease: Improving Global Outcomes (2013) Treatment of steroid-sensitive nephrotic syndrome: new guidelines from KDIGO. Pediatr Nephrol 28:415–426. https://doi.org/10.1007/s00467-012-2310-x
Mehls O, Hoyer PF (2011) Dosing of glucocorticosteroids in nephrotic syndrome. Pediatr Nephrol 26:2095–2098. https://doi.org/10.1007/s00467-011-1993-8
Mishra OP, Basu B, Upadhyay SK, Prasad R, Schaefer F (2010) Behavioural abnormalities in children with nephrotic syndrome. Nephrol Dial Transplant 25:2537–2541. https://doi.org/10.1093/ndt/gfq097
Pasini A, Aceto G, Ammenti A, NefroKid Study Group et al (2015) Best practice guidelines for idiopathic nephrotic syndrome: recommendations versus reality. Pediatr Nephrol 30:91–101. https://doi.org/10.1007/s00467-014-2903-7
Raja K, Parikh A, Webb H, Hothi D (2017) Use of a low-dose prednisolone regimen to treat a relapse of steroid-sensitive nephrotic syndrome in children. Pediatr Nephrol 32:99–105
Raman V, Krishnamurthy S, Harichandrakumar KT (2016) Body weight-based prednisolone versus body surface area-based prednisolone regimen for induction of remission in children with nephrotic syndrome: a randomized, open-label, equivalence clinical trial. Pediatr Nephrol 31:595–604. https://doi.org/10.1007/s00467-015-3285-1
Samuel S, Morgan CJ, Bitzan M, Mammen C, Dart AB, Manns BJ, Alexander RT, Erickson RL, Grisaru S, Wade AW, Blydt-Hansen T, Feber J, Arora S, Licht C, Zappitelli M (2013) Substantial practice variation exists in the management of childhood nephrotic syndrome. Pediatr Nephrol 28:2289–2298. https://doi.org/10.1007/s00467-013-2546-0
Tarshis P, Tobin JN, Bernstein J, Edelman CM Jr (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the international study of kidney disease in children. J Am Soc Nephrol 8:769–776
Author information
Authors and Affiliations
Contributions
Yael Borovitz—designed the research, patient, and data collection and planned the statistical analysis; participated in enrollment, investigation, data collection, and analysis; and drafted and revised the manuscript.
Hadas Alfandary—participated in patient enrollment and investigation, data collection, and revised the manuscript.
Orly Haskin—participated in patient enrollment and investigation, data collection, and revised the manuscrip
Shelly Levi—participated in patient enrollment and investigation, data collection, revised the manuscript.
Shulamit Kaz—participated in patient enrollment and investigation, data collection, and revised the manuscript.
Miriam Davidovits—designed the research, monitored data collection, participated in the investigation and data collection, and revised the manuscript.
Amit Dagan—designed the research, patient, and data collection; planned the statistical analysis; participated in enrollment, investigation, data collection, and analysis; drafted and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all parents or guardians of the study participants.
Additional information
Communicated by Mario Bianchetti
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borovitz, Y., Alfandary, H., Haskin, O. et al. Lower prednisone dosing for steroid-sensitive nephrotic syndrome relapse: a prospective randomized pilot study. Eur J Pediatr 179, 279–283 (2020). https://doi.org/10.1007/s00431-019-03506-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03506-5