Abstract
Since resistance to intravenous immunoglobulin (IVIG) is associated with coronary lesions (CALs) in Kawasaki disease (KD), it is crucial to identify patients at risk to protect them from coronary involvement. The available risk scores to predict IVIG resistance were developed in Asian populations in whom their effectiveness has been proven, but data on non-Asian children are limited. The aim of this study is to evaluate the ability of the Kobayashi, Egami, and Formosa risk scores to predict IVIG resistance and CALs in Italian patients with KD. A multicenter retrospective analysis involving children with KD diagnosed between 2000 and 2015 was carried out: 257 patients were enrolled (57.9% boys, 89.9% Caucasian); 43 patients were IVIG resistant (16.7%). The scores have low sensitivity and specificity in predicting IVIG resistance: respectively, KS 64% and 62.5%, ES 41.4% and 77.4%, and FS 70.8% and 44.9%. The predictive value of the 3 scores for predicting CALs was also poor.
Conclusion: Kobayashi, Egami, and Formosa Scores are ineffective in predicting IVIG resistance and coronary involvement in a predominantly Caucasian cohort. A specific score system for mostly Caucasian children with KD is needed enable the early identification of those at risk for CALs who could benefit from intensified treatment.
What is Known: • There are several risk scores developed in the Asian population to early identify patients with KD at risk for immunoglobulin-resistance and thus for coronary lesions. • Data are scarce on their effectiveness in non-Asian children. | |
What is New: • We present a comprehensive analysis of the ability of 3 Asian risk scores in a cohort of mostly Caucasian children to predict immunoglobulin resistance and coronary involvement. • Low sensitivity and specificity of the Asian scores for immunoglobulin-resistance and coronary lesions suggest the need for criteria specific for different ethnicities. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease (KD) is an acute self-limiting vasculitis mostly seen in children younger than 5 years of age. It predominantly affects medium-sized vessels with particular possible involvement of the coronary arteries. In high-income countries, KD is the leading cause of pediatric-acquired heart disease [1]. If untreated, coronary artery lesions (CALs) develop in about 15–25% of patients and may lead to severe complications such as ischemic heart disease and sudden death during either the acute or chronic phases of the disease [2]. The state-of-the-art treatment is high-dose intravenous immunoglobulin (IVIG) together with acetylsalicylic acid (ASA). Intravenous immunoglobulin should be instituted as early as possible within the first 10 days of illness onset, characterized by a high-grade fever. However, 10–15% of patients experience persistent or recurrent fever after completion of the initial IVIG administration and are thus classified as unresponsive to IVIG treatment [3]. Many studies have shown that this subgroup of patients is at increased risk of developing coronary artery abnormalities [4, 5].
Since the incidence of KD is 10 to 20 times higher in North-East Asian countries (especially Japan, Korea, and Taiwan) than in the USA and Europe [6], the largest cohort of patients and the longest surveillance reports come from Japan. Genetic susceptibility to KD is known to affect incidence, responsiveness to conventional treatment with IVIG, and coronary involvement. Indeed, the incidence among Japanese descendants living in Hawaii is similar to that reported for children from Japan, while the incidence among Caucasian Hawaiian children is comparable with that reported for white children in the continental USA [7]. However, findings regarding the associations between genetic background and distinct aspects of the disease found in Asian children have not been demonstrated in patients of other races [8,9,10].
The identification of patients at high risk for IVIG resistance at the time of presentation can allow us to identify those who may benefit from more intensive monitoring of their condition and who may require treatment modulation during the acute phase, with the potential addition of other anti-inflammatory agents to the conventional IVIG treatment. With this intention, risk-scoring algorithms have been developed by Asian authors, which take into account demographic (age at presentation), clinical (days of illness, presence of lymphadenopathy), and laboratoristic variables (% of neutrophils, platelet count (PLT), hemoglobin (Hb), aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, sodium (Na), C-reactive protein (CRP), lactate dehydrogenase (LDH), and total bilirubin as risk factors in their populations. The Kobayashi (KS) [11], Egami (ES) [12], and Sano [13] scores are, to date, the most widely known and used. More recently, another score has been developed for a population of Taiwanese children [14].
Interestingly, a number of studies aimed at evaluating the use of Japanese scoring systems in populations of mixed ethnicity failed to demonstrate real effectiveness in predicting IVIG resistance and coronary involvement in these non-Japanese populations. Tremoulet et al. evaluated the ES with 362 children in San Diego County diagnosed with KD in 2006. When applied to their population, the ES missed more than 60% of IVIG-resistant patients. The authors developed their own scoring system, based on days of illness ≤ 4, age-adjusted hemoglobin, % neutrophil bands, and gamma glutamyl-transferase, which appeared to have higher sensitivity (73% vs 38% using the ES) for detecting IVIG resistance and was more sensitive among Caucasian children, compared to other ethnicities [15].
Similar findings were reported by Sleeper et al. who evaluated the KS, ES, and Sano scores on North American children of mixed ethnicity using the dataset from the Pediatric Heart Network’s randomized, placebo-blind trial of pulsed corticosteroids for primary therapy for KD. The sensitivity of the abovementioned scores in predicting IVIG resistance was 33%, 42%, and 40%, respectively, with, at most, modest associations with CA z-scores as well [16]. Moreover, no differential treatment effect of steroids was found for subjects from this population classified as high versus low risk for IVIG resistance on the basis of these 3 scores, as opposed to the results of the RAISE study performed in a Japanese population which showed significant reduction in the development of CALs in patients with KD considered to be at risk for IVIG resistance according to the KS [17].
Previous studies aimed at applying different risk scores in non-Japanese populations failed to show a good effectiveness in predicting IVIG resistance and coronary involvement [18,19,20].
The purpose of this study was to evaluate the effectiveness of three different risk scoring systems from Japan and Formosa in order to identify subjects at risk for IVIG resistance and thus for the development of CALs in our cohort of Italian children with KD.
Materials and methods
The present multicenter retrospective study included all children diagnosed with KD between 2000 and 2015 in 13 Pediatric Units in Emilia-Romagna, a northern region of Italy. All KD diagnoses were made in accordance with the 2004 American Heart Association (AHA) Guidelines [21], distinguishing complete and incomplete/atypical forms of clinical presentation. The onset of illness was defined as the first day of fever. All patients were treated, in accordance with the 2004 AHA Guidelines, with IVIG at 2 g/kg in a single infusion before the tenth day of fever, together with aspirin at 80–100 mg/kg/day, subsequently switched to 3–5 mg/kg/day once the patient had been afebrile for at least 48 h. Intravenous immunoglobulin resistance was defined as persistent/recrudescent fever for at least 36 h but for no longer than 7 days after the completion of the first IVIG infusion. Treatment was defined as late when the first dose of IVIG was given after the 10th day of fever.
Echocardiography was performed in all children. Diagnosis of CALs was based on the clinical judgment of the reporting physician; the left anterior descending artery and right coronary artery were measured. Two criteria were applied depending on the definition used by each participating center. The first follows the definition of the Japanese Ministry of Health which classifies coronary arteries as abnormal if the internal lumen diameter is > 3 mm in children < 5 years old or > 4 mm in children ≥ 5 years old and if the internal diameter of a segment measures ≥ 1.5 times that of an adjacent segment. The second criteria defines CALs as a coronary z-score ≥ 2.5 [21]. Coronary artery lesions were defined if an artery exceeded the Japanese criteria or the z-scores ≥ 2.5.
A database was prospectively created and then retrospectively reviewed. It included demographic features and clinical characteristics, total days of fever, IVIG responsiveness, laboratory values (white blood cells (WBC), neutrophil and lymphocyte percentage, RBC, Hb, PLT, CRP, erythrocyte sedimentation rate (ESR), serum albumin, AST, ALT, Na) of the acute (from onset to the 10th day) stage of the disease. Patients who received IVIG after the 10th day of fever and those who were not treated with IVIG were excluded from the data analysis.
We applied the KS, ES, and Formosa (FS) risk score systems [11, 12, 14] (Table 1) to our cohort. The KS assesses the parameters days of fever, age ≤ 12 months, Na, AST, neutrophil percentage, CRP, and PLT; the ES assesses the parameters age < 6 months, days of fever, PLT, ALT, and CRP; and the FS assesses lymphadenopathy, neutrophil percentage, and albumin levels. A cut-off point of ≥ 4, ≥ 3, and ≥ 3, respectively, identifies patients at high risk of IVIG resistance in the abovementioned scoring systems. Table 1 shows published KS, ES, and FS data for IVIG resistance.
Statistical analysis
Data were expressed as the mean ± standard deviation (SD) for continuous variables, and median with range or number with percentage, as appropriate, for categorical variables. Student’s t test and Mann-Whitney U tests for continuous data and χ2 test for categorical data were used to compare variables between groups.
We divided KD patients into two groups (IVIG responders and non-responders) according to their response to IVIG. We subsequently compared demographic and clinical characteristics, presence of CALs, and laboratory findings from the acute and subacute phases between the two groups.
Sensitivity and specificity of the predictor cut-off for the positive score in KS, ES, and FS were calculated to predict IVIG unresponsiveness and the development of CALs. A ROC curve was developed to see the effectiveness of the overall score. The test was considered to be effective when the area under the ROC curve was higher than 0.5.
P < 0.05 was considered to be statistically significant.
The study analysis was performed using SPSS for Windows.
Results
Diagnosis and patient characteristics
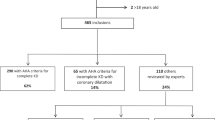
A total of 304 consecutive children diagnosed with KD were enrolled in this study. Ten children were excluded due to incomplete data, 26 due to late treatment, and 11 because they were not treated. Of the 257 patients included, 214 (83.3%) were IVIG responders and 43 (16.7%) were IVIG non-responders.
Baseline characteristics of IVIG responders and non-responders are shown and compared in Table 2. Race was not significantly different between the two groups: Caucasian was the most common ethnicity (91.1% of IVIG responders and 83.7% of non-responders), followed by Asian (4.2% and 9.3%, respectively). There was a higher incidence of CALs in IVIG non-responders than in responders (p = 0.01). Seasonality and total days of fever were significantly different between the two groups (p = 0.03 and p < 0.0001, respectively), while age at diagnosis, gender, and clinical presentation were not.
Comparison of laboratory values at the time of diagnosis showed that IVIG non-responders had higher neutrophil percentages (p = 0.008) and AST (p = 0.02), and lower lymphocyte percentages (p = 0.008). No other significant differences were found among the laboratory parameters (Table 3).
Complete data were available to calculate KS, ES, and FS risk scores for 145, 188, and 113 subjects, respectively.
Kobayashi, Egami, and Formosa scoring systems and IVIG resistance
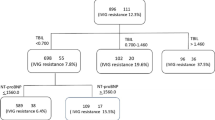
Sensitivity and specificity of the KS, ES, and FS are shown in Table 4. ROC curves are shown in Fig. 1.
Sixty-one children/145 (42%) had a positive KS (score ≥ 4), and 25/145 (41%) were IVIG non-responders. Sixteen children with a positive KS (26.2%) were IVIG non-responders. The sensitivity of the score was 64.0% and the specificity 62.5%. The negative predictive value was 89.3%, and the positive predictive value 26.2%. The area under the ROC curve was 0.4.
When applied to the subgroup of seven Asian patients, the KS had a sensitivity of 100% and a specificity of 75%.
Forty-eight patients out of 188 (25.5%) had a positive ES (score ≥ 3) and 29 out of 188 (15.4%) were IVIG non-responders. Twelve children with a positive ES were IVIG non-responders. Sensitivity was 41.4% and specificity was 77.4%. The area under the ROC curve was 0.32.
Sixty-six out of 113 patients (58.4%) had a positive FS (score ≥ 3) and 89 out of 113 patients (78.7%) were IVIG non-responders. Seventeen patients with a positive FS were IVIG non-responders. The sensitivity of the score was 70.8%, and the specificity was 44.9%. The area under the ROC curve was 0.32.
Kobayashi, Egami, and Formosa scoring systems and coronary anomalies
The predictive value of the KS, ES, and FS for CALs was poor. Results are shown in Table 4.
The KS and ES had a sensitivity of 41.9% and 38.5% and a specificity of 57.9% and 77.9%, respectively. Negative and positive predictive values were even lower than those calculated to identify IVIG non-responders. The FS showed a sensitivity of 72.0% and a specificity of 45.5%, a positive predictive value of 27.3%, and a negative predictive value of 85.1%.
Discussion
Our study evaluated the effectiveness of three different Asian scoring systems in predicting IVIG resistance and coronary lesions in the same Mediterranean population.
Since IVIG unresponsiveness is associated with increased risk for coronary involvement, it is mandatory to identify children at risk as soon after diagnosis as possible in order to adapt adjunctive anti-inflammatory treatment. Widely used risk scoring systems for predicting IVIG non-responsiveness come from studies in Asian populations, and they are based on demographic, clinical, and laboratoristic parameters. In these populations, these scores were effective for identifying KD patients who could benefit from additional anti-inflammatory therapy to reduce CALs.
The data presented show that the KS, ES, and FS systems were poor predictors of IVIG resistance in our cohort of Italian children with KD; thus, they represent unhelpful tools for identifying those patients who could benefit from adjunctive anti-inflammatory therapy during the acute phase. Moreover, our results also demonstrate that none of the considered scores were predictive for the development of CALs. As previously demonstrated, our findings show that IVIG non-responders have a higher incidence of CALs and longer fever duration. Gender, age at diagnosis, and clinical presentation were not significantly different between the two groups in our cohort, while the percentage of neutrophils and AST were significantly higher and the percentage of lymphocytes lower among the IVIG responders.
In Japan, the RAISE study demonstrated that in patients with a positive KS, adjunctive treatment with steroids is effective in reducing coronary lesions, and therefore cardio-vascular morbidity [17]. More recently, in patients at risk according to the ES, first-line treatment with intravenous steroids plus IVIG was shown to be effective in preventing coronary involvement [22].
Very recently, a study in Germany failed to prove a good prognostic value of the KS, ES, and Sano scores in a primarily Caucasian population because of poor sensitivity, and only the Sano score had a positive likelihood ratio for CALs 4 weeks after the onset of the disease [23]. In 2011, the KS, ES, and Sano scores were shown to have good specificity, but low sensitivity, for refractory KD and only the KS could significantly predict coronary artery involvement 5 weeks after the onset of KD in a Northern American Cohort [16]. Previous studies in non-Japanese populations from North America [15, 16], the US Midwest [19], Spain [18], and The UK [20] applied a single risk score and showed low sensitivity and specificity in predicting unresponsiveness to conventional treatment. Thus, so far, Asian scores have been demonstrated to be neither sufficiently sensitive nor specific in identifying high-risk patients in multi-ethnic non-Asian populations. Highlighting the crucial role played by ethnicity in terms of response to conventional and adjunctive treatments, a recent meta-analysis failed to demonstrate, in non-Asian patients, a beneficial effect of corticosteroids as rescue therapy in IVIG non-responders in reducing the incidence of coronary abnormalities [24], while it was shown to be effective in Asian children.
In our study, we were able to apply 3 score systems in the same population. Our findings show that in Italian children, the FS had the best sensitivity (slightly under 80%) and the lowest specificity, while the ES had the best specificity but the lowest sensitivity for IVIG resistance. However, ROC curves for the 3 scores were less than 0.5 demonstrating that all 3 scores were not useful for identifying IVIG resistance among the KD patients in our mostly Caucasian population. Furthermore, the considered scores were also ineffective for predicting coronary involvement.
The ethnicity of our cohort is similar to the German population described by Jakob et al. [23] and the Spanish cohort described by Sanchez-Manubens et al. [18], in which Caucasian children were the most highly represented (91.1% in our cohort, 95% in the German cohort, and 81.1% in the Spanish cohort). Both the German and Spanish authors also reported the failure of the different Asian scores in their cohorts.
The development of clinical and laboratory scores to predict IVIG resistance and coronary lesions in European populations is mandatory in order to permit early recognition and treatment with additional anti-inflammatory agents in children at increased risk. This would potentially prevent or, at least, limit coronary involvement and subsequent cardiovascular morbidity.
Limitations of this study include its retrospective nature and its sample size. In contrast, we were able to apply three different Asian Scores in the same Cohort of Italian children.
In conclusion, the KS, ES, and FS systems are not effective screening tools for predicting IVIG unresponsiveness or CALs among Italian patients with KD. This may be due the fact that our patients are mostly Caucasian, thus presenting a different genetic predisposition to the disease and, possibly, clinical and laboratoristic characteristics. Further multicenter studies are necessary in order to find a specific score for non-Asian populations which will enable the early identification of patients at increased risk for coronary involvement who could benefit from adjunctive anti-inflammatory treatment in addition to IVIG.
Abbreviations
- AHA:
-
American Heart Association
- ALT:
-
Alanine aminotransferase
- ASA:
-
Acetylsalicylic acid
- AST:
-
Aspartate aminotransferase
- CALs:
-
Coronary artery lesions
- CRP:
-
C-reactive protein
- ES:
-
Egami score
- ESR:
-
Erythrocyte sedimentation rate
- FS:
-
Formosa score
- Hb:
-
Hemoglobin
- IVIG:
-
Intravenous immunoglobulin
- KS:
-
Kobayashi score
- LDH:
-
Lactate dehydrogenase
- Na:
-
Sodium
- PLT:
-
Platelet count
- RBC:
-
Red blood cells
- SD:
-
Standard deviation
- WBC:
-
White blood cells
References
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, Kobayashi T, Wu MH, Saji TT, Pahl E, American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; and Council on Epidemiology and Prevention (2017) Diagnosis, treatment, and long-term Management of Kawasaki Disease: a scientific statement for health professionals from the American Heart Association. Circulation 135:e927–e999. https://doi.org/10.1161/CIR.0000000000000484
Eleftheriou D, Levin M, Shingadia D, Tulloh R, Klein NJ, Brogan PA (2014) Management of Kawasaki disease. Arch Dis Child 99:74–83. https://doi.org/10.1136/archdischild-2012-302841
Bar-Meir M, Kalisky I, Schwartz A, Somekh E, Tasher D, Israeli Kawasaki Group (2018) Prediction of resistance to intravenous immunoglobulin in children with Kawasaki disease. J Pediatric Infect Dis Soc 7:25–29. https://doi.org/10.1093/jpids/piw075
Hwang JY, Lee KY, Rhim JW, Youn YS, Oh JH, Han JW, Lee JS, Burgner D (2011) Assessment of intravenous immunoglobulin non-responders in Kawasaki disease. Arch Dis Child 96:1088–1090. https://doi.org/10.1136/adc.2010.184101
Wei M, Huang M, Chen S, Huang G, Huang M, Qiu D, Guo Z, Jiang J, Zhou X, Yu Q, Guo Y, Fu L, Gao W, Li F (2015) A multicenter study of intravenous immunoglobulin non-response in Kawasaki disease. Pediatr Cardiol 36:1166–1172. https://doi.org/10.1007/s00246-015-1138-0
Singh S, Vignesh P, Burgner D (2015) The epidemiology of Kawasaki disease: a global update. Arch Dis Child 100:1084–1088. https://doi.org/10.1136/archdischild-2014-307536
Holman RC, Belay ED, Christensen KY, Folkema AM, Steiner CA, Schonberger LB (2016) Hospitalizations for Kawasaki syndrome among children in the United States, 1997–2007. Pediatr Infect Dis J 29:483–488. https://doi.org/10.1097/INF.0b013e3181cf8705
Onouchi Y, Ozaki K, Burns JC, Shimizu C, Terai M, Hamada H, Honda T, Suzuki H, Suenaga T, Takeuchi T et al (2012) A genome-wide association study identifies three new risk loci for Kawasaki disease. Nat Genet 44:517–521. https://doi.org/10.1038/ng.2220
Lee YC, Kuo HC, Chang JS, Chang LY, Huang LM, Chen MR, Liang CD, Chi H, Huang FY, Lee ML, Huang YC, Hwang B, Chiu NC, Hwang KP, Lee PC, Chang LC, Liu YM, Chen YJ, Chen CH, Alliance TPID, Chen YT, Tsai FJ, Wu JY (2012) Two new susceptibility loci for Kawasaki disease identified through genome-wide association analysis. Nat Genet 44:522–525. https://doi.org/10.1038/ng.2227
Chang CJ, Kuo HC, Chang JS, Lee JK, Tsai FJ, Khor CC, Chang LC, Chen SP, Ko TM, Liu YM, Chen YJ, Hong YM, Jang GY, Hibberd ML, Kuijpers T, Burgner D, Levin M, Burns JC, Davila S, International Kawasaki Disease Genetics Consortium¶, Korean Kawasaki Disease Genetics Consortium¶, Taiwan Kawasaki Disease Genetics Consortium¶, Chen YT, Chen CH, Wu JY, Lee YC (2013) Replication and meta-analysis of GWAS identified susceptibility loci in Kawasaki disease confirm the importance of B lymphoid tyrosine kinase (BLK) in disease susceptibility. PLoS One 8:e72037. https://doi.org/10.1371/journal.pone.0072037
Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, Kobayashi T, Morikawa A (2006) Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation 113:2606–2612. https://doi.org/10.1161/CIRCULATIONAHA.105.592865
Egami K, Muta H, Ishii M, Suda K, Sugahara Y, Iemura M, Matuishi T (2006) Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr 149:237–240. https://doi.org/10.1016/j.jpeds.2006.03.050
Sano T, Kurotobi S, Matsuzaki K, Yamamoto T, Maki I, Miki K, Kogaki S, Hara J (2007) Prediction of non-responsiveness to standard high-dose gamma-globulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur J Pediatr 166:131–137. https://doi.org/10.1007/s00431-006-0223-z
Lin MT, Chang CH, Sun LC, Liu HM, Chang HW, Chen CA, Chiu SN, Lu CW, Chang LY, Wang JK, Wu MH (2016) Risk factors and derived formosa score for intravenous immunoglobulin unresponsiveness in Taiwanese children with Kawasaki disease. J Formos Med Assoc 115:350–355. https://doi.org/10.1016/j.jfma.2015.03.012
Tremoulet AH, Best BM, Song S, Wang S, Corinaldesi E, Eichenfield JR, Martin DD, Newburger JW, Burns JC (2008) Resistance to intravenous immunoglobulin in children with Kawasaki disease. J Pediatr 153:117–121. https://doi.org/10.1016/j.jpeds.2007.12.021
Sleeper LA, Minich LL, McCrindle BM, Li JS, Mason W, Colan SD, Atz AM, Printz BF, Baker A, Vetter VL, Newburger JW, Pediatric Heart Network Investigators (2011) Evaluation of Kawasaki disease risk-scoring systems for intravenous immunoglobulin resistance. J Pediatr 158:831–835. https://doi.org/10.1016/j.jpeds.2010.10.031
Kobayashi T, Saji T, Otani T, Takeuchi K, Nakamura T, Arakawa H, Kato T, Hara T, Hamaoka K, Ogawa S, Miura M, Nomura Y, Fuse S, Ichida F, Seki M, Fukazawa R, Ogawa C, Furuno K, Tokunaga H, Takatsuki S, Hara S, Morikawa A (2012) Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet 379:1613–1620. https://doi.org/10.1016/S0140-6736(11)61930-2
Sánchez-Manubens J, Antón J, Bou R, Iglesias E, Calzada-Hernandez J, Borlan S, Gimenez-Roca C, Rivera J, Kawasaki Disease in Catalonia Working Group (2016) Role of the Egami score to predict immunoglobulin resistance in Kawasaki disease among a Western Mediterranean population. Rheumatol Int 36:905–910. https://doi.org/10.1007/s00296-016-3499-y
Loomba RS, Raskin A, Gudausky TM, Kirkpatrick E (2016) Role of the Egami score in predicting intravenous immunoglobulin resistance in Kawasaki disease among different ethnicities. Am J Ther 23:e1293–e1299. https://doi.org/10.1097/MJT.0000000000000045
Davies S, Sutton N, Blackstock S, Gormley S, Hoggart CJ, Levin M, Herberg JA (2015) Predicting IVIG resistance in UK Kawasaki disease. Arch Dis Child 100:366–368. https://doi.org/10.1136/archdischild-2014-307397
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P, Baltimore RS, Wilson WR, Baddour LM, Levison ME, Pallasch TJ, Falace DA, Taubert KA, Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association, American Academy of Pediatrics (2004) Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the committee on rheumatic fever, endocarditis and Kawasaki disease, council on cardiovascular disease in the young, American Heart Association. Circulation 110:2747–2771. https://doi.org/10.1161/01.CIR.0000145143.19711.78
Ebato T, Ogata S, Ogihara Y, Fujimoto M, Kitagawa A, Takanashi M, Ishii M (2017) The clinical utility and safety of a new strategy for the treatment of refractory Kawasaki disease. J Pediatr 191:140–144. https://doi.org/10.1016/j.jpeds.2017.08.076
Jakob A, Horstmann J, Hufnagel M, Stiller B, Berner R, Schachinger E, Meyer K, Obermeier V (2018) Failure to predict high-risk Kawasaki disease patients in a population-based study cohort in Germany. Pediatr Infect Dis J:1. https://doi.org/10.1097/INF.0000000000001923
Chen S, Dong Y, Kiuchi MG, Wang J, Li R, Ling Z, Zhou T, Wang Z, Martinek M, Pürerfellner H, Liu S, Krucoff MW (2016) Coronary artery complication in Kawasaki disease and the importance of early intervention: a systematic review and meta-analysis. JAMA Pediatr 170:1156–1163. https://doi.org/10.1001/jamapediatrics.2016.2055
Author information
Authors and Affiliations
Contributions
Marianna Fabi conceptualized and designed the study and the data collection instruments, drafted the initial manuscript, and supervised the reviewed literature.
Laura Andreozzi carried out the statistical analysis and contributed to the collection of data, and to write the initial draft.
Elena Corinaldesi contributed to the collection of data and supervised the reviewed literature.
Tetyana Bodnar coordinated and supervised data collection, contributed to the critical revision of literature, and critically reviewed the manuscript.
Francesca Lami coordinated and supervised data collection, contributed to the critical revision of literature, and critically reviewed the manuscript.
Andrea Donti coordinated and supervised data collection, contributed to the critical revision of literature, and critically reviewed the manuscript.
Chiara Landini contributed to data acquisition and critically revised the manuscript.
Cristina Cicero contributed to data acquisition and critically revised the manuscript.
Monica Sprocati contributed to data acquisition and critically revised the manuscript.
Barbara Bigucci contributed to data acquisition and critically revised the manuscript.
Claudia Balsamo contributed to data acquisition and critically revised the manuscript.
Giorgia Di Fazzio contributed to data acquisition and critically revised the manuscript.
Federico Marchetti helped to draft the manuscript, contributed to the critical revision of literature, and reviewed the manuscript.
Bertrand Tchana helped to draft the manuscript, contributed to the critical revision of literature, and reviewed the manuscript.
Paola Sogno Valin helped to draft the manuscript, contributed to the critical revision of literature, and reviewed the manuscript.
Enrico Valletta helped to draft the manuscript, contributed to the critical revision of literature, and reviewed the manuscript.
Lorenzo Iughetti helped to draft the manuscript, contributed to the critical revision of literature, and reviewed the manuscript.
Marcello Lanari supervised the reviewed literature, contributed to the interpretation of data, and critically reviewed the manuscript for important content.
All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Central Review Board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Peter de Winter
Rights and permissions
About this article
Cite this article
Fabi, M., Andreozzi, L., Corinaldesi, E. et al. Inability of Asian risk scoring systems to predict intravenous immunoglobulin resistance and coronary lesions in Kawasaki disease in an Italian cohort. Eur J Pediatr 178, 315–322 (2019). https://doi.org/10.1007/s00431-018-3297-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3297-5