Abstract
Measles outbreaks were recently reported in Europe due to low immunization rates. In this scenario, identifying the reasons of no vaccination is crucial to set up strategies to improve immunization rate. A cross-sectional study was conducted to investigate the determinants of missed vaccination in children living in Southern Italy, during the 2016 outbreak. A standardized face-to-face questionnaire was used to record demographic data, immunization status, and reasons for missed vaccination. A total of 1141 children (median age 86 months, male 47.2%) was enrolled, 77.8% of the children were adequately vaccinated for age, 6.3% were incompletely vaccinated for age, and 15.9% did not receive any vaccine dose. Vaccination rate and reasons for not vaccinating significantly varied according to age, with children ≤ 24 months showing the lowest rate (67.8%). Reasons for not vaccinating included fear for side effects (51%), presence of underlying chronic conditions (12.2%), skip scheduled appointment (12.2%), refusal of vaccination (10.3%), acute illnesses (7.2%), and allergy to eggs (4.6%). The presence of underlying condition was a risk factor for inadequate immunization (p < 0.0001). Only 4.7% of conditions were true contraindications to vaccine administration.
Conclusion: We reported inadequate measles immunization rate in Southern Italy, with lowest rates in children ≤ 2 years or with underlying conditions. Only a minority had true contraindications to vaccine uptake. Implementation strategies addressed to health-care professionals and families should focus on the reported determinants to increase measles vaccination coverage.
What is Known: • Measles is a viral, highly communicable disease, preventable by vaccine. • Measles elimination in Europe failed as demonstrated by outbreaks in several countries, due to low immunization rates. | |
What is New: • Inadequate measles immunization rate due to false contraindications in Southern Italy, with lowest rates in children ≤ 2 years. • The presence of underlying disease is a risk factor for inadequate immunization. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Measles is an acute viral and communicable disease preventable by vaccine and responsible for potentially severe complications [28]. Despite the availability of a safe vaccine, measles accounts for about 150,000 deaths annually worldwide [30, 33]. According to the World Health Organization (WHO), a vaccination coverage of at least 95% of local population is needed to prevent dissemination and reach measles elimination [31]. However, despite remarkable progress in reducing measles incidence, vaccine hesitancy is becoming a major barrier to reach this goal [24, 26].
Measles elimination in Europe, defined as the interruption of indigenous transmission of infection for a 12-month period from all member states [25], was one of the WHO goals by 2015 [31]. This goal failed, as demonstrated by the report of 4484 cases of measles in 30 European countries between February 2016 and January 2017 [19, 32]. Romania, the UK, and Italy reported the highest number of cases, with children below 5 years of age accounting for more than 40% of patients [11].
In keeping with these data, a high incidence rate (2.9/100,000 inhabitants) was recorded in 2016 in Campania Region, the most crowded region in Southern Italy [12], and a relevant increase in the hospital admissions due to measles infection was observed at Regional Referral Centre for Pediatric Infectious Diseases.
Local surveillance data in a cohort of children living in Campania region reported that 92% of children below 24 months of age received a first dose of combined measles-mumps-rubella (MMR) vaccine [13]; however, we hypothesized that the increasing incidence of measles in our region might be the expression of a further reduction in the immunization rate.
Identifying the reasons that induce parents and caregivers to refuse or to skip measles vaccination is of paramount importance to set up effective strategies of implementation of vaccination coverage.
Primary aims of our study were to evaluate measles immunization rate in children living in Campania Region during the 2016 outbreak and to specifically investigate the determinants of missed vaccination in this setting.
Materials and methods
Study design and population
This cross-sectional study was carried out between November 1, 2016, and March 3, 2017, in two tertiary care University Hospitals in Naples, the largest city in Southern Italy with about 3 million inhabitants. In order to estimate the measles vaccination coverage, we enrolled a convenience sample of children aged > 15 months accessing the Department of Pediatrics of the University of Naples Federico II and of the University of Campania Luigi Vanvitelli. All families in ambulatory care, day hospital, or regular hospitalization were invited to participate to the study.
A standardized questionnaire was administered face-to-face by four residents in pediatrics, after receiving parents’ consent, asking information on child demographic data, presence of underlying chronic conditions, ongoing chronic treatments, and immunization records. All families of children who were not vaccinated or delayed the second scheduled dose of MMR vaccine were asked to report the reasons for missed vaccination. It was reported anonymously.
In addition, we compared the coverage for measles with that for diphtheria/tetanus/pertussis/hepatitis B/polio/haemophilus influenzae type b (DTaP-HB-IPV-Hib) vaccine to understand the specific determinants of missed MMR vaccine administration.
In order to increase data reliability and to reduce reporting bias, only children whose families exhibited the regional immunization record were included in the study.
All data were loaded in a Microsoft Excel® database. This observational study was approved by the Committee for the evaluation of clinical studies and by the Ethical Committee of the University of Campania Luigi Vanvitelli (protocol number 19181/17).
Vaccination coverage and determinants of missed vaccination
According to the indications provided by Italian Ministry of Health, a first dose of MMR vaccination is currently recommended for children at 12–15 months of age and a second dose should be administered in pre-school children between 5 and 6 years [14]. Based on these indications, we distinguished children in three categories:
-
1)
“Not vaccinated”: children who did not receive any dose of MMR vaccine;
-
2)
“Adequately vaccinated for age”: children who received one dose between 15 and 72 months of age and two doses if aged > 72 months;
-
3)
“Incompletely vaccinated for age”: children aged > 72 months who received only one dose of MMR vaccine.
We analyzed the barriers to vaccination and compared the reported reasons for not vaccinating with the contraindications and precautions for MMR vaccination reported by the American Committee of Immunization Practice and the Centre for Diseases Control and Prevention [29].
In addition, we analyzed the data by dividing the population into four age groups (15–24 months, 25–72 months, 73–120 months, and > 120 months) to explore possible variations according to child age.
Immunization rate: best- and worst-case scenario
Although the two terms “vaccination coverage” and “immunization rate” are often used as synonymous, we defined the first as the rate of children receiving a vaccine dose according to schedule, and the second as the immunological response that confers protection against infection after vaccine uptake.
From an immunological point of view, a durable protection against measles infection is conferred by a single vaccine dose in most people. The second dose is intended to provide protection to those who fail to respond to the first one. Children receiving the first dose at 12 months develop measles antibodies in 93–95% of cases, and children getting vaccination at 15 months reach 97–98%. Administration of two doses of vaccine provides serologic evidence of immunity in 97–99% of people [1, 27]. About ¼ of children undergoing immunosuppressive treatment or chemotherapy become susceptible to measles with a reduction of circulating antibody titers below protective levels [4].
Taking into account the above premises, we defined a “best-case” and “worst-case scenario” by calculating the number children who may acquire a complete immunization against measles after receiving one or two doses of MMR vaccine.
The “best-case scenario” was calculated considering that 99% of children were immunized after two doses of MMR vaccine and that children receiving a single dose were potentially vaccinated at 15 months of age and only 2% of them did not reach immunization against measles.
The “worst-case scenario” was calculated starting from children who did not receive any vaccination dose and applying the lowest vaccine effectiveness reported in literature (93% after one dose at 12 months; 97% after two doses). In the worst-case scenario, we also considered that about 1% of children < 17 years may lose protection against measles [2].
Statistical analysis
Vaccination coverage was calculated as the proportion of vaccinated subjects to the total number of individuals in the categories studied. Face-to-face interview avoided missing data.
Data are expressed as number and percentage or means ± standard deviations (SD), as appropriate. Comparison of categorical and continuous variables was performed using the chi-square test and the t test, respectively. When the study groups were more than two, the ANOVA test was used to compare continuous variables. Chi-square with Fisher’s correction was used to address any differences for categorical variables, as needed. Data were further analyzed according to different age ranges. Univariate and multivariate analysis of variables influencing the risk of inadequate vaccination was performed using the logistic regression analysis and Cox’s regression model. Risk was reported as odds ratio (OR) with 95% confidence intervals (95%CI). Statistical analysis was performed using the SPSS Statistics software (version 20.0 for Windows; SPSS Inc., Chicago, IL, USA). A p value < 0.05 was considered statistically significant. This study has been conducted according to the STROBE checklist for cross-sectional studies (Supplementary table S1).
Results
A total of 1276 families were invited to participate, 5 refused to answer the questionnaire and 130 could not exhibit the vaccination records. Finally, 1141 children (median age 86 months, male 47.2%) were enrolled (Fig. 1). The overall characteristics of study population are reported in Table 1.
Vaccination coverage
Five hundred sixty-six children (49.6%) showed a complete MMR immunization schedule and 181 children (15.9%) did not receive any MMR dose (Table 1).
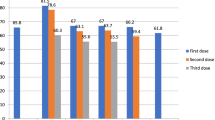
The overall measles vaccination coverage of 84.1% (children receiving at least one dose) was significantly lower than the coverage reported for DTaP-HB-IPV-Hib vaccine in children aged > 15 months (84.1% vs 97.7%, p < 0.0001). The difference was even larger if only children with adequate MMR immunization for age were considered (77.8% vs 97.7%, p < 0.0001). Vaccination coverage significantly varied according to age group (p = 0.0001), with children aged below 24 months showing the lowest rate (67.8%) (Fig. 2).
Measles vaccination coverage in Italian children according to age range. Children were considered adequately vaccinated for age if received two doses of MMR or one dose < 6 years, incompletely vaccinated if received only one dose after 6 years of age and not vaccinated if did not receive any MMR dose.
The overall estimate of measles immunization rate ranged between 82.9 and 78.9% according to the “best-case” and “worst-case scenario,” respectively (Table 2).
Among children with inadequate MMR vaccination schedule, only 14.4% of families expressed the intention to vaccinate their children in the next future.
Determinants of missed vaccination
Two hundred sixty-three children (22.2%) were not appropriately vaccinated according to age. Different reasons for not vaccinating were reported by families, including fear for MMR vaccine side effects (128, 48.7%), presence of underlying chronic conditions (25, 9.5%), skip/forget a scheduled appointment (29, 11.0%), overall refuse of vaccination policies (25, 9.9%), presence of concomitant acute illnesses (18, 6.8%), and allergy to eggs (12, 4.6%). Only one patient was undergoing chemotherapy during the study period (Fig. 3). For 13 children, parents refused to report the reasons for omitting vaccination (Fig. 1).
The MMR vaccination coverage in children with underlying chronic conditions was significantly lower if compared to otherwise healthy children (31.8% vs 79.1%, p < 0.001). The presence of any underlying chronic condition was a major risk factor for inadequate measles immunization either in univariate (OR 9.5, 95%CI 4.0 to 22.5, p < 0.0001), and multivariate analysis (OR 10.8, 95%CI 4.3 to 27.0, p < 0.0001).
Male children had a slightly higher risk of inadequate coverage (OR 1.44, 95%CI 0.88 to 2.3).
The determinants of missed vaccination significantly varied according to age (p < 0.0001), with the presence of acute illness being prevalent in children aged < 24 months (35.7%), and an overall refuse of immunization more common in families of pre-school children (Fig. 3). The presence of underlying chronic conditions ranged from 6.1% in children 2–6 years to 13.2% in those aged > 10 years (Fig. 3). Egg allergy was the reason for not vaccinating in 10.7% of children < 24 months and in 4.6% of the entire population. However, none of the children had had severe immune reaction to eggs (Table 3).
Comparing the reasons reported by families with the indications of health authorities, only 4.7% of the reasons for not vaccinating children actually were true contraindications to MMR vaccination and a further 3% were in the list of conditions requiring special precautions (Supplemental figure S2).
Discussion
Despite the availability of an effective and safe vaccine, measles is currently spreading throughout Europe due to inadequate immunization rate of local population. To ensure population-based measles herd immunity, at least 92–95% of subjects need to be vaccinated [20]. We demonstrated that in the most populous region of Southern Italy, where a measles outbreak recently occurred, less than 85% of children are adequately vaccinated with an estimated immunization rate ranging between 79 and 82% according to the worst and best-case scenario, respectively. The lowest vaccination coverage was found in young children (67.8% below 2 years and 83.6% below 6 years of age) and in those with underlying chronic conditions. These are actually the categories at higher risk of severe measles-related complications and death.
The Italian Health Surveillance System (EpiCentro) reported an overall immunization rate of 92% (range 72–95%) similar to those recorded in other countries where recent outbreaks occurred, such as in the USA where MMR vaccination rates ranged between 84 and 92% according to child age [13, 22]. However, the immunization rate in our sample population living in Southern Italy appeared even lower than that reported at national level. As a further demonstration of this low immunization rate, Campania recorded the first cases of measles infection during the outbreak started in November 2016 (when the survey began), similarly to what happened in 2002 measles outbreak when measles incidence increased sharply after a registration of 65% MMR coverage [8].
In keeping with these data, the US Centre for Diseases Control and Prevention recently released a warning for American children traveling to Italy [7]. In this scenario, identifying the reasons that lead families to skip vaccination is crucial to set up effective strategies to improve measles immunization rate.
About 10% of enrolled families expressed an overall lack of trust in vaccination policies. As demonstrated by comparing the coverage for MMR to that of DTaP-HB-IPV-Hib vaccine, we observed that children belonging to families “against vaccination” did not complete any vaccine schedule. The rate of people “against vaccination” recorded in our population appeared significantly higher than that reported in a recent large survey at national level performed by the Italian National Institute of Health (about 1% of responders declared against vaccination) [16]. This large difference between vaccine acceptance in Southern Italy and overall national data might be related to the setting, local socio-educational level and population income, as previously supported by evidence in other European countries [5].
The effects of parental beliefs against vaccination were more evident in pre-school children, accounting for about a quarter of not vaccinated cases. Although many different factors may affect this result, the young age of parents and their source of information likely impact on this decision.
However, the implementation of MMR vaccine appears to be loaded by further barriers. The fear of MMR-related side effects was the major reason for not vaccinating children in our population, accounting for more than half of missed vaccination. The adverse effects of the MMR vaccine are usually mild and self-limited, and serious adverse effects occur in about 1/million cases. However, the hypothesis of a link between MMR vaccine and autism spectrum disorders, postulated by Wakefield and colleagues about 20 years ago, progressively gained public attention. The effects of that weak, biased and controversial evidence, and, even more, of the fraudulent dissemination promoted by mass media, directly led to a decline in MMR vaccination rates in many countries [18].
A substantial body of evidence found no link between the MMR vaccine and autism spectrum disorders and the decrease in MMR vaccination (or even withdrawal) did not influence the rate of autism [15, 21]. Taking into account the strength of current evidence and the benefit of the vaccine, the hypothesis to conduce a randomized clinical trial to determine whether the MMR vaccine causes autism has been defined “unethical” [3]. A rigorous study conducted in about 95,000 children, including siblings of autistic children, provided conclusive evidence on the “lack of harmful association” between MMR vaccine and autism spectrum disorders [22]. However, to have a relevant impact on public health, true results should receive the same resonance as the “bad news” on vaccines. As a demonstration of the rooted beliefs, in our population, two families ascribed their child diagnosis of autism to previous MMR uptake.
Egg allergy was reported as a further reason for not vaccinating against measles in about 1/20 families, even though none of the children had ever experienced severe reactions. Although current measles vaccines are derived from chicken embryo-fibroblast tissue cultures, there is evidence that children with egg allergy are at low risk of anaphylactic reactions to MMR and may receive measles vaccines without special precautions [1].
In keeping with our results, other authors identified the fears regarding vaccine safety as one of the major determinants of low MMR vaccine uptake [6, 16]. In addition, they reported that the dissatisfaction with the quality of information surrounding vaccination are linked with parental hesitancy to have their children vaccinated. The quality of information disseminated either to health-care workers or to general population is the starting point to reach an adequate coverage.
Several evidences demonstrated the increasing use of social media to broadcast health information. However, recent studies reported a considerable and negative impact of mass media and social networks on immunization practice and decision-making in Italian population, whereas frequently, the position of authoritative medical organization has little impact [9, 10].
In contrast, there is evidence that a trusting relationship between families and a health-care professional, who take time to discuss vaccine procedures and concerns, may positively influence parents’ views on vaccination [23]; in a recent Italian survey, the vast majority of parents considered the family pediatrician as a reliable source of information about vaccination [16].
It is relevant that, in our population, less than 5% of conditions reported by families as reasons for not vaccinating were true contraindications to MMR vaccine. This is the direct effect of the lack of knowledge among stakeholders of vaccination policies and of spreading inaccurate information to families. Children with underlying chronic conditions, who are exposed to a 9-fold increased risk of not receiving adequate MMR vaccination, provide a clear example of the weakness of the role of physicians in implementing immunization. In two third of those children, the reasons reported by families—and likely validated by health-care professionals—were not real contraindications to MMR vaccine uptake.
According to our results, the strategies to improve MMR immunization rate should address two different audiences: health-care practitioners and families. Supplemental Figure S2 reported potential strategies to implement MMR vaccination in accordance with the barriers identified. An appropriate and updated education should be provided to physicians and other health-care practitioners involved in vaccination policies and, in parallel, simple, unambiguous, and straightforward information should be disseminated to general population in order to improve vaccination uptake.
Despite medical advice and family acceptance of vaccination, a further 11% of families skip or forget scheduled appointments in our population, meaning that some children are unvaccinated due to missed opportunities.
During outbreaks, all health-care practitioners have to offer vaccination at indicated times, check vaccination schedule of all patients, and offer “catch-up vaccination” to those who were not vaccinated at the appropriate time.
This study has some limitations. First, the study population included children who refer to clinical departments of Pediatrics rather than involving the overall healthy pediatric population. In that setting, the proportion of children with severe conditions (i.e., inflammatory bowel diseases, rheumatologic diseases) might be over-represented in comparison to other settings and may potentially impact on the overall vaccination coverage. However, in order to limit the selection bias, we enrolled a large pediatric population including children in outpatient and inpatient settings. As a demonstration of the representativeness of the study population, the rate of children affected by chronic conditions is similar to the overall pediatric population in Italy, with about 10% of children with atopy/asthma and less than 5% with other underlying conditions. Although children accessing a tertiary care hospital might have conditions more severe than those reported in the overall population (i.e., severe asthma rather than mild-to-moderate features).
To avoid potential reporting bias, only children exhibiting the immunization records were included in the study.
In addition, we did not investigate the role of different health-care workers in suggesting or providing vaccination to the study population. However, based on previous data collected in the same setting, we are aware that immunization is mainly recommended by primary care pediatricians and physicians working in referral centres (for those with chronic illnesses), with vaccination centers seeming to have little or no effect [17]. However, this redundancy of role by physicians managing children, mainly those with at-risk conditions, has been identified as a further barrier to vaccine uptake [17].
In conclusion, we reported inadequate measles immunization rate in children living in Southern Italy in concomitance with measles outbreak. The vaccination coverage was lower in children below 2 years of age and in those with underlying chronic conditions, who are those potentially exposed to severe complications and death. Only a minority of not vaccinated children presented conditions that really contraindicate vaccination. The fear of MMR-related adverse events, the inappropriate interpretation of chronic diseases and suspected allergies as potential contraindications were the main barriers to MMR vaccine uptake. Strategies to implement MMR vaccination should focus on these determinants of missed vaccination to increase measles immunization rate.
Abbreviations
- DTaP-HB-IPV-Hib:
-
Diphtheria/tetanus/pertussis/hepatitis B/polio/haemophilus influenzae type b
- MMR:
-
Measles-mumps-rubella
- WHO:
-
World Health Organization
References
American Academy of Pediatrics – RedBook Edition 2015
Bednarczyk RA, Orenstein WA, Omer SB (2016) Estimating the number of measles-susceptible children and adolescents in the United States using data from the National Immunization Survey-Teen (NIS-Teen). Am J Epidemiol 184(2):148–156
Bester JC (2016) Measles and measles vaccination: a review. JAMA Pediatr 170(12):1209–1215
Bochennek K, Allwinn R, Langer R, Becker M, Keppler OT, Klingebiel T, Lehrnbecher T (2014) Differential loss of humoral immunity against measles, mumps, rubella and varicella-zoster virus in children treated for cancer. Vaccine 3227:3357–3361
Bocquier A, Ward J, Raude J, Peretti-Watel P, Verger P (2017) Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Expert Rev Vaccines 16:1107–1118
Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, Vincent CA, Fraser G, Sevdalis N (2010) Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine 28(26):4235–4248
Center for Diseases control and prevention n.d. Traveler’s health: Measles in Italy. Available from: https://wwwnc.cdc.gov/travel/notices/watch/measles-italy
Centers for Disease Control and Prevention (CDC) (2003) Measles epidemic attributed to inadequate vaccination coverage--Campania, Italy, 2002. MMWR Morb Mortal Wkly Rep 52:1044–1047
Covolo L, Ceretti E, Passeri C, Boletti M, Gelatti U (2017) What arguments on vaccinations run through YouTube videos in Italy? A content analysis. Hum Vaccin Immunother 31:1–7
De Marco G, Ummarino D, Giannetti E, Magurno T, Guarino A (2005) Impact of mass media communication in the implementation of influenza vaccination for infants. Arch Pediatr Adolesc Med 159:596
ECDC Surveillance and disease data. Monthly measles epidemiological updates. Available from: http://ecdc.europa.eu/en/healthtopics/measles/epidemiological_data/Pages/measles_surveillance_reports.aspx
Epicentro. Morbillo & Rosolia News: il bollettino della sorveglianza integrata morbillo-rosolia, Available from: http://www.epicentro.iss.it/problemi/morbillo/bollettino/RM_News_2016_34.pdf. (accessed 30 Oct 2018)
Epicentro. Available from: http://www.epicentro.iss.it/temi/vaccinazioni/dati_Ita.asp#morbillo (accessed 30 Oct 2018)
Filia A, Bella A, Rota M, Tavilla A, Magurano F, Baggieri M, Nicoletti L, Iannazzo S, Pompa M, Declich S (2013) Analysis of national measles surveillance data in Italy from October 2010 to December 2011 and priorities for reaching the 2015 measles elimination goal. Euro Surveill 18(20)
Fombonne E, Zakarian R, Bennett A, Meng L, McLean-Heywood D (2006) Pervasive developmental disorders in Montreal, Quebec, Canada: prevalence and links with immunizations. Pediatrics 118(1):e139–e150
Giambi C, Fabiani M, D'Ancona F, Ferrara L, Fiacchini D, Gallo T, Martinelli D, Pascucci MG, Prato R, Filia A, Bella A, Del Manso M, Rizzo C, Rota MC (2018) Parental vaccine hesitancy in Italy - results from a national survey. Vaccine 36(6):779–787
Giannattasio A, Lo Vecchio A, Franzese A, Prisco F, Femiano P, Guarino A (2010) Redundancy of roles by physicians in charge of paediatric diabetes is a barrier to flu immunisation. Arch Dis Child 95:399–400
Godlee F, Smith J, Marcovitch H (2011) Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ 342:c7452
Grammens T, Maes V, Hutse V, Laisnez V, Schirvel C, Trémérie JM, Sabbe M (2016) Different measles outbreaks in Belgium, January to June 2016 - a challenge for public health. Euro Surveill 21(32)
Hethcote HW (1983) Measles and rubella in the United States. Am J Epidemiol 1171:2–13
Honda H, Shimizu Y, Rutter M (2005) No effect of MMR withdrawal on the incidence of autism: a total population study. J Child Psychol Psychiatry 46(6):572–579
Jain A, Marshall J, Buikema A, Bancroft T, Kelly JP, Newschaffer CJ (2015) Autism occurrence by MMR vaccine status among US children with older siblings with and without autism. JAMA 313(15):1534–1540
Leask J, Chapman S, Hawe P, Burgess M (2006) What maintains parental support for vaccination when challenged by anti-vaccination messages? A qualitative study. Vaccine 24(49–50):7
Lo NC, Hotez PJ (2017) Public health and economic consequences of vaccine hesitancy for measles in the United States. JAMA Pediatr 171(9):887–892
Mankertz A, Mulders MN, Shulga S, Kremer JR, Brown KE, Santibanez S, Muller CP, Tikhonova N, Lipskaya G, Jankovic D, Khetsuriani N, Martin R, Gavrilin E (2011) Molecular genotyping and epidemiology of measles virus transmission in the World Health Organization European region, 2007-2009. J Infect Dis 204(Suppl 1):S335–S342
McIntosh ED, Janda J, Ehrich JH, Pettoello-Mantovani M, Somekh E (2016) Vaccine hesitancy and refusal. J Pediatr 175:248–249
McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS (2013) Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 62(RR-04):1–34
Rota PA, Moss WJ, Takeda M, de Swart RL, Thompson KM, Goodson JL (2016) Measles. Nature Rev Dis Primers 2:16049
Vaccine Recommendations and Guidelines of the ACIP n.d. Contraindications and precautions updates. Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html
World Health Organization (WHO). Renewed commitment to measles and rubella elimination and prevention of congenital rubella syndrome in the WHO European Region by 2015. Regional Committee for Europe. Sixtieth session. Moscow, 13–16 September 2010
World Health Organization (WHO). Surveillance guidelines for measles, rubella and congenital rubella syndrome in the WHO European region. Update December 2012. Available at: http://www.euro.who.int/__data/assets/pdf_file/0018/79020/e93035-2013.pdf
World Health Organization (WHO) (2012) Global measles and rubella strategic plan: 2012–2020. WHO, Geneva Available from: http://apps.who.int/iris/bitstream/10665/70254/1/WHO_IVB_10.02_eng.pdf. (accessed 30 Oct 2018)
World Health Organization (WHO). Measles. Fact sheet no 286. 2013. MRI report 2012. Available at: http://www.measlesrubellainitiative.org/wp-content/uploads/2013/07/MRI-2012-Annual-Report.pdf
Author information
Authors and Affiliations
Contributions
ALV and AG conceived the study.
ALV and MDC designed the study protocol and prepared the first draft of the survey.
AG revised and approved the survey before dissemination.
MDC, MCF, FC, and FWB administered the survey to families and caregivers.
MDC and MCF developed the database. ALV performed the statistical analysis and wrote the first draft of the manuscript. ALV and MDC produced tables and figures.
AG and MMDG provided substantial contribution to draft the paper and reviewed the final manuscript.
All authors gave their final approval of the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Nicole Ritz
Electronic supplementary material
Supplemental table S1
STROBE checklist (PDF 96 kb)
Supplemental figure S2
The frequency of real contraindications (black) and false contraindications and other barriers (shaded in black) are reported according to each category. On the right column, different strategies to be addressed to health-care workers and general population are proposed to improve vaccination coverage
Rights and permissions
About this article
Cite this article
Lo Vecchio, A., Cambriglia, M.D., Fedele, M.C. et al. Determinants of low measles vaccination coverage in children living in an endemic area. Eur J Pediatr 178, 243–251 (2019). https://doi.org/10.1007/s00431-018-3289-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3289-5