Abstract
The effectiveness of using a face mask with a small diffuser for oxygen delivery (OxyMask) was compared to use of a high-flow nasal cannula (HFNC) in patients with moderate or severe bronchiolitis.
The study population in this open, phase 4, randomized controlled trial consisted of 60 patients aged 1–24 months diagnosed with moderate or severe bronchiolitis and admitted to an intensive care unit (ICU) for oxygen therapy. The patients were randomized into two groups according to the method of oxygen delivery: a diffuser mask group and an HFNC group.
There were seven failures in the mask group and none in the HFNC group. The survival probability differed significantly between the two treatment methods (p = 0.009).
Time to weaning off oxygen therapy was 56 h in the HFNC group and 96 h in the mask group (p < 0.001).
Conclusion: HFNC use decreased the treatment failure rate and the duration of both oxygen therapy and ICU treatment compared to the diffuser mask, which implies that an HFNC should be the first choice for treating patients admitted to the ICU with severe bronchiolitis.
What is known: • A high-flow nasal cannula (HFNC) does not significantly reduce the time on oxygen compared to standard therapy in children with moderate to severe bronchiolitis. Observational studies show that, since the introduction of HFNC, fewer children with bronchiolitis need intubation. For children with moderate to severe bronchiolitis there is no proof of its benefit. | |
What Is New: • In children with moderate to severe bronchiolitis, HFNC provides faster and more effective improvement than can be achieved with a diffuser mask. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute bronchiolitis results from inflammation of the bronchioles and is usually caused by viral infection. It is most common in children younger than 2 years of age and is a frequent reason for a child being admitted to the hospital. There is no established, specific therapy for acute bronchiolitis, and it is commonly treated using supplemental oxygen and by ensuring that the patient remains hydrated [1].
The OxyMask (Southmedic Inc., Barrie, ON, Canada) is a new face mask for oxygen delivery that uses a small diffuser to concentrate and direct oxygen toward the mouth and nose. It is capable of delivering up to 90% of the fraction of inspired oxygen (FiO2) with minimal CO2 retention. In this system, the FiO2 can be adjusted by modifying the flow velocity to deliver the quantity of oxygen that the patient requires. Oxygen is supplied to the patient in a jet that flows from a device mounted on the oxygen mask. This ensures that a high concentration of oxygen is provided at a low flow rate. In addition, carbon dioxide retention is minimal because the mask has a fenestrated structure. Therefore, a diffuser mask is a more effective oxygen delivery method than many other low-flow delivery systems including the nasal cannula and simple oxygen mask [2,3,4].
Oxygen therapy using a high-flow nasal cannula (HFNC) is a high-flow oxygen delivery system that enhances the efficiency of respiration with high flow rates to clear dead space and provide fresh oxygen. This system supplies oxygen at a high flow rate through a loose nasal cannula. HFNC therapy provides heated and humidified oxygen to fill the dead space in the nasopharynx and generally produces low but not measurable positive airway pressure. It enhances the passage of air through the airway by reducing inspiratory pressure [5]. Previous studies have demonstrated that using an HFNC can decrease respiratory effort and improve gas exchange [6, 7]. In recent years, many studies have indicated that high-flow nasal oxygen therapy is more effective than low-flow systems. This is substantiated by significant decreases in the use of mechanical ventilation since HFNC therapy was introduced [8, 9].
Previous reports on the effectiveness of HFNC therapy in treating acute bronchiolitis have come primarily from observational work and there are few relevant, randomized controlled studies [10,11,12]. In addition, previous studies have compared HFNC therapy with less effective, low-flow systems (e.g., the simple mask or nasal cannula) [10,11,12]. Our experience suggests that oxygen therapy using an HFNC is more effective than with an OxyMask in patients with moderate to severe bronchiolitis, and that the former allows faster recovery. To the best of our knowledge, no randomized controlled trial has compared the effectiveness of the HFNC and diffuser mask in treating bronchiolitis.
In this study, we compared oxygen therapy using an HFNC and a diffuser mask (an effective low-flow oxygen delivery system) to treat patients with moderate to severe acute bronchiolitis admitted to an intensive care unit (ICU).
Materials and methods
Objective and design
This study was a single-center, open, phase 4, randomized controlled trial comparing oxygen therapy delivered using a diffuser mask with using an HFNC in children younger than 24 months who were diagnosed with moderate or severe bronchiolitis. The severity of bronchiolitis in all children admitted to the ICU was assessed using a clinical scoring system that included general health status, respiration rate, heart rate, and the presence of chest retractions [13] (Table 1). The Wang clinical severity scores ranged from 9 to 12, 4 to 8, and 1 to 3 in patients with severe, moderate, and mild bronchiolitis, respectively.
The primary objective of the study was to determine whether there is any difference between the two methods’ treatment failure rates. The secondary objectives were to determine whether the two treatment methods produce differences in time to weaning off oxygen therapy or lengths of hospital and ICU stays, or in clinical or laboratory parameters.
We hypothesized that compared to using a diffuser mask, oxygen therapy using an HFNC would decrease the treatment failure rate and ICU stay because the patients would improve more rapidly.
Ethical consent and clinical trial registration
The study was approved by the Erciyes University Medical School Ethical Committee on Clinical Trials (#2016/115). This trial was registered with Clinicaltrials.gov (number NCT03342781). Informed consent was obtained from the parents of all patients included in the study.
Patient selection
The study population consisted of patients admitted to the pediatric ICU with a diagnosis of moderate or severe bronchiolitis from the Emergency Department of Kayseri Emel Mehmet Tarman Children’s Hospital, Kayseri Teaching Hospital and University of Medical Sciences, between March and December of 2016.
Definitions
The diagnoses of acute bronchiolitis were made according to definitions provided by the National Institute for Health and Care Excellence (NICE) [14]. Patients with symptoms of viral respiratory tract infection (cough, rhinorrhea, nasal obstruction, tachypnea, retraction, prolonged expiration, and cyanosis) and requiring supplemental oxygen were diagnosed with acute bronchiolitis [15]. The requirement for supplemental oxygen was defined as SpO2 < 92% while breathing room air [14].
Inclusion and exclusion criteria
Included patients were aged between 1 and 24 months and had been diagnosed with moderate or severe acute bronchiolitis. Any patients requiring immediate respiratory support (non-invasive or invasive mechanical ventilation, altered mental status, or apnea at presentation), those already admitted to the ICU due to respiratory failure, those with underlying chronic lung disease or cardiovascular disorders, those with obstructions of the upper respiratory tract, and those with cranial malformations were excluded.
Randomization
After obtaining patient consent in the ICU, patients were randomly allocated to receive either therapy (1:1) using a block size of four, with stratification for sex.
Study groups and measurements
In total, 60 patients were included in the study, with 30 patients in each group. The patients were randomly assigned to either the diffuser mask group or the HFNC group. For each group, demographic data (age, sex, weight, and severity of bronchiolitis), additional therapies provided (e.g., salbutamol or ipratropium nebulizer solution, salbutamol inhaler, corticosteroids, antibiotics), and baseline laboratory parameters (C-reactive protein, procalcitonin, white blood cell and neutrophil counts) were recorded.
Diffuser mask group
Patients received oxygen therapy (10–15 L/min) from an OxyMask (Southmedic, Inc.) to maintain SpO2 > 94%. Weaning from supplemental oxygen was permitted at any time for delivery of the lowest possible amount of oxygen to maintain an oxygen saturation level of at least > 94%. Oxygen therapy was halted if SpO2 was maintained at a level > 94% for more than 4 h. In such cases, the oxygen flow rate was decreased to 2 L/min and the patient was monitored while breathing room air. He or she was then transferred to a ward.
HFNC group
Patients received oxygen therapy at a high flow rate from a Precision Flow nasal cannula (Vapotherm, Inc., Stevensonville, MD, USA). A 1.9-mm pediatric cannula, which can dispense 1–20 L/min of oxygen, was used in this study. The initial oxygen flow rate was 1 L/kg/min, up to a maximum of 20 L/min. Oxygen was delivered at an air:oxygen ratio of 1:1, resulting in a maximum FiO2 of 60%. The FiO2 was then decreased to 20%. HFNC therapy was halted if SpO2 was maintained at a level > 94% for more than 4 h at an FiO2 value of 20%. The patient was then transferred to a ward.
Primary outcome
In both groups, the primary endpoint was treatment failure, defined as an escalation of care at any time point during the hospital stay. At the point of care, the treating clinicians determined treatment failure as fulfillment of at least two of three clinical criteria and the requirement for escalation of care [16].
-
1.
No change or an increase in respiration rate compared to baseline.
-
2.
No change or an increase in heart rate compared to baseline.
-
3.
Persistence of low SpO2 (< 92%) measurements despite an adequate oxygen flow rate and FiO2 in the HFNC group/oxygen flow rate of 15 L/min in the mask group.
In the diffuser mask patient group, when oxygen therapy failed, the HFNC treatment protocol was applied. We also planned to implement non-invasive mechanical ventilation if treatment failed in the HFNC-group patients.
Secondary outcomes
In both groups, we determined whether there were any differences in time to weaning off oxygen therapy, length of ICU stay, or length of hospital stay, and recorded any changes in respiration and heart rates, pH, partial pressure of carbon dioxide (pCO2), and oxygen saturation (SpO2) between baseline (0 h) and 1, 6, 12, 24, and 48 h. In addition, we recorded any differences in adjunct therapies used (e.g., antibiotic therapy, bronchodilator therapy) between groups. We also examined whether there were any differences in the rates of recovery in each group by measuring improvements in respiration and heart rates recorded at 1, 6, 12, 24, and 48 h compared to baseline values. In recording the time to weaning off oxygen therapy, we included oxygen supplied after crossover to another therapy if the first treatment had failed.
Measurements
All parameters were measured at baseline and at 1, 6, 12, 24, and 48 h; thereafter, daily measurements were recorded throughout each patient’s stay in the ICU.
Heart rate
Heart rates were measured using a PVM-2701 monitor (Nihon Kohden, Corp., Tokyo, Japan).
Respiration rate
Respiration rates were measured over a period of 1 min by a nursing team.
pH, lactate, and CO2 measurements
For all patients, pH, lactate, and CO2 measurements were recorded from capillary blood samples using an ABL800 FLEX blood gas analyzer (Radiometer Medical A/S, Bronshoj, Denmark). The blood samples were drawn from the heel or big toe at baseline and at 1, 6, 12, 24, and 48 h.
SpO2 measurement
SpO2 was measured non-invasively using a PVM-2701 monitor (Nihon Kohden, Corp.). The saturation probe was applied to the patient’s right palm. SpO2 was measured at baseline and at 1, 6, 12, and 24 h; thereafter, daily measurements were recorded throughout each patient’s stay in the ICU.
Statistical analysis
All statistical analyses were performed using IBM SPSS for Windows software (ver. 21.0; IBM, Corp., Armonk, NY, USA). The primary analysis of all outcomes was followed by an intent to treat (ITT) analysis.
The Shapiro-Wilk test was used and data normality was assessed using histograms and q-q plots. The Levene test was applied to assess variance homogeneity. Survival probabilities were predicted using the Kaplan-Meier method, and group comparisons were performed with the log-rank test. In those analyses, the event status was defined as treatment failure (0: no failure, 1: failure) and survival time was given in hours. Repeated measures ANOVA was used to assess repeated variables. Independent samples t test, Mann-Whitney U test, and one-way repeated measures ANOVA were applied for between-group and within-group comparisons. A Bonferroni correction was applied to adjust p values to control for multiple testing. In all analyses, p < 0.05 (and an adjusted p < 0.05) was considered to indicate statistical significance.
Results
Characteristics of the patients
A total of 82 children less than 24 months of age were admitted to the Pediatric Intensive Care Unit with a primary diagnosis of bronchiolitis between March 1, 2016, and December 1, 2016. Of these, five patients were misdiagnosed and the remaining 77 patients were correctly diagnosed as having bronchiolitis. Of those admitted, five patients with mild bronchiolitis were excluded from the study. Of the remaining 72 patients with moderate to severe bronchiolitis, 12 were excluded based on the exclusion criteria. None of the 60 remaining patients refused study participation. These children were randomly assigned to receive HFNC or diffuser mask therapy (n = 30 in each group), and all were included in the primary analysis (Fig. 1). There were no significant differences in age, sex, weight, severity of bronchiolitis, baseline heart or respiration rate, SpO2, pCO2, pH, lactate level, white blood cell count, C-reactive protein, or procalcitonin level between the diffuser mask and HFNC groups (p > 0.05; Tables 2 and 3). There were also no significant differences in the use of salbutamol or ipratropium nebulizer solution, intravenous steroids, or antibiotics between the diffuser mask and HFNC groups (p > 0.05).
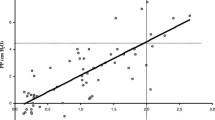
Primary outcome
The Kaplan-Meier plot is shown in Fig. 2. There were seven failures in the mask group and none in the HFNC group. The survival probability differed significantly between the two treatments (p = 0.009). The most common cause of treatment failure was increased use of oxygen (n = 4), followed by persistent tachycardia (n = 2) and persistent tachycardia (n = 1).
Secondary outcomes
The treatment failure rate, time to weaning off oxygen, length of ICU stay, and length of hospital stay were all significantly lower in the HFNC group (p = 0.011, p < 0.001, p < 0.001, and p < 0.001, respectively) (Table 4). The treatment failure rate was 23.3% (n = 7) in the mask group whereas there were no failures in the HFNC group. None of the patients in any group required mechanical ventilation.
The decrease (%) in respiration rate compared to baseline at 6 h was significantly greater in the HFNC group (Table 5). The decreases (%) in heart rate compared to the baseline values were significantly greater in the HFNC group at 1, 6, 12, 24, and 48 h (Table 5).
There were no significant differences between baseline respiration rates, whereas the rates at 1, 6, 12, 24, and 48 h were significantly lower in the HFNC group (Table 6). There were no significant differences between baseline heart rates and those at 1 h, whereas the rates in the HFNC group were significantly lower at 6, 12, 24, and 48 h than in the diffuser mask group (Table 6). There were no significant differences in baseline, 24, and 48 h SpO2, whereas the values at 1, 6, and 12 h were significantly higher in the HFNC group than in the other groups (Table 6). No significant differences were observed in pCO2 or lactate values obtained at baseline, 1, 6, 12, 24, or 48 h (Table 5).
Discussion
In our study, the success rate in patients administered oxygen therapy for acute bronchiolitis was twofold higher in those treated with an HFNC than in those treating using a diffuser mask. We also found that HFNC use decreased the time to weaning off oxygen and length of ICU stay compared to use of a diffuser mask. Although respiration and heart rates were markedly decreased in both groups, patients in the HFNC group recovered more rapidly than those in the diffuser mask group. No significant difference in CO2 decrease was observed between the two groups.
Oxygen therapy via HFNC creates positive pressure in the nasopharyngeal area and decreases respiratory workload and respiratory stress due to the high velocity of oxygen delivery. When therapy is provided using an HFNC, oxygen consumption decreases because the activity of the diaphragm increases. The workload of the accessory respiratory muscles is also reduced; therefore, HNFC slows progression to respiratory failure and decreases the intubation rate [11, 17]. The oxygen supplied is heated and humidified, preventing mucosal injury by reducing inflammatory reactions. Furthermore, because pulmonary vasoconstriction is inhibited, the overall duration of ICU treatment is also likely to be reduced [18, 19].
Although there have been many studies on HFNC therapy, there have been few randomized controlled studies [10,11,12]. To the best of our knowledge, no study has compared the use of a diffuser mask and HFNC to treat acute bronchiolitis. In a randomized, controlled study in patients presenting to the emergency department with moderate bronchiolitis, Kepreotes et al. [10] compared nasal cannula (a low-flow oxygen delivery system) and HFNC therapy; there were no significant differences between groups in either the time to weaning off oxygen therapy or the length of hospital stay. However, the authors found that treatment failure was significantly lower in the standard therapy group than in the HVNC group. In a multicenter randomized, controlled study in patients presenting to the emergency department with bronchiolitis and a need for oxygen, Franklin et al. [12] compared nasal cannula (a low-flow oxygen delivery system) and HFNC therapy; the treatment failure rate was lower in the HFNC group than in the standard therapy group. However, these two groups did not significantly differ with respect to the length of hospital stay or duration of oxygen supplementation. In the small semi-randomized pilot study by Milani et al. [11] involving patients with moderate to severe bronchiolitis who were younger than 12 months old, the duration of oxygen therapy and length of hospital stay were lower in patients receiving HFNC therapy than in those receiving standard oxygen therapy. Similar to studies by Kepreotes et al. and Franklin et al., our results demonstrated a significantly lower rate of treatment failure in the HFNC group than in the diffuser mask group, and no cases of treatment failures in the HFNC group. In contrast to the results of Franklin et al. [12] and Kepreotes et al. [10], however, our HFNC patients had a more rapid recovery, a shorter time to weaning off oxygen, and a shorter length of hospital stay. However, this may have been due to the fact that our study was conducted almost entirely on patients with severe bronchiolitis who required admission to the ICU. Only one patient had moderate bronchiolitis. HFNC can be more effective for patients with severe bronchiolitis requiring ICU admission as it may provide more rapid recovery in such patients. We found that time to weaning off oxygen therapy and length of ICU stay were lower in patients receiving HFNC therapy.
Decreases in respiration and heart rates are important factors when assessing treatment effectiveness in patients with respiratory failure. Improvements in respiration and heart rates are better indicators of treatment success than many other parameters [20,21,22]. HFNC therapy would probably be most effective during the first few hours of respiratory failure, when the inspiratory flow is insufficient [19, 20]. In the randomized controlled study of Milani et al. [11], both the respiration rate and the heart rate decreased more markedly, particularly within the first 8 h, in patients receiving HFNC therapy than in those treated using a mask. In our study, marked decreases in respiration and heart rates were observed in both groups. Therefore, oxygen therapy using a diffuser mask is also effective for treating acute bronchiolitis. However, the decreases in heart and respiration rates compared to baseline values were significantly greater in the HFNC group. In other words, there was a more rapid clinical recovery in patients receiving HFNC therapy. The shorter ICU treatment durations observed in the HFNC group support this conclusion.
Diffuser masks deliver a jet of concentrated oxygen to the patient’s mouth and nose through a small diffuser. However, diffuser masks differ from other low-flow oxygen-delivery systems because the mask is open, which allows carbon dioxide to disperse. Therefore, carbon dioxide inhalation is unlikely even if the flow rate is low [2,3,4]. In a prospective comparative study involving adult patients with acute respiratory failure, Lam et al. [23] found that the end-tidal CO2 volume was significantly lower in patients wearing a diffuser mask compared to those wearing a non-rebreather oxygen mask. In a study involving adult patients with chronic oxygen dependency, which compared the Venturi mask (a high-flow oxygen-delivery system) with the diffuser mask. In another prospective comparative study, Beecroft et al. [3] found no significant differences in the end-tidal CO2 volumes or capillary pCO2 between the groups. In our study, the respiration and heart rates were lower, whereas SpO2 levels were higher, in the HFNC group compared to the diffuser mask group. However, no significant differences in pCO2 were observed between the groups. This could mean that an HFNC is more effective for restoring oxygen; however, a diffuser mask is just as effective as an HFNC in preventing carbon dioxide retention.
This study had some limitations. It was performed in a single center, had a limited sample size, and was not performed in a blinded manner In addition, repeated sampling for capillary blood gases was conducted. All of these factors may have influenced the results. Minimal patient handling to reduce the risk of exhaustion, together with careful noninvasive monitoring for complications such as apnea and respiratory failure, are the mainstays of management [24]. For assessment of carbon dioxide, end-tidal CO2 measurement rather than invasive capillary sampling is recommended.
However, our clinical and laboratory parameter data demonstrate that HFNC use promotes more rapid recovery in patients with severe bronchiolitis compared to those given oxygen therapy using a diffuser mask. Use of an HFNC also decreased the treatment failure rate and the duration of ICU treatment. Therefore, it should be the first choice for providing oxygen therapy to patients with severe bronchiolitis. However, a diffuser mask is just as effective as an HFNC in retaining carbon dioxide.
In conclusion, HFNC provides more rapid improvement of clinical and laboratory findings in patients with severe bronchiolitis. Therefore, HFNC should be considered the first choice for oxygen therapy in patients admitted to the ICU with severe bronchiolitis.
Abbreviations
- FiO2 :
-
Fraction of inspired oxygen
- HFNC:
-
High-flow nasal cannula
- ICU:
-
Intensive care unit
- pCO2 :
-
Partial pressure of carbon dioxide
- SpO2 :
-
Oxygen saturation
References
Tapiainen T, Aittoniemi J, Immonen J, Jylkkä H, Meinander T, Nuolivirta K, Peltola V, Salo E, Seuri R, Walle SM, Korppi M (2016) Finnish guidelines for the treatment of community-acquired pneumonia and pertussis in children. Acta Paediatr 105(1):39–43. https://doi.org/10.1111/apa.13177
Paul JE, Hangan H, Hajgato J (2009) The OxyMask(™) development and performance in healthy volunteers. Med Devices (Auckl) 2:9–17
Beecroft JM, Hanly PJ (2006) Comparison of the OxyMask and Venturi mask in the delivery of supplemental oxygen: pilot study in oxygen-dependent patients. Can Respir J 13(5):247–252
Ling E, McDonald L, Dinesen TR, DuVall D (2002) The OxyArm—a new minimal contact oxygen delivery system for mouth or nose breathing. Can J Anaesth 49(2):297–301
Bressan S, Balzani M, Krauss B, Pettenazzo A, Zanconato S, Baraldin E (2013) High-flow nasal cannula oxygen for bronchiolitis in a pediatric ward: a pilot study. Eur J Pediatr 172(12):1649–1656. https://doi.org/10.1007/s00431-013-2094-4
Pham TM, O'Malley L, Mayfield S, Martin S, Schibler A (2015) The effect of high flow nasal cannula therapy on the work of breathing in infants with bronchiolitis. Pediatr Pulmonol 50(7):713–720. https://doi.org/10.1002/ppul.23060
Hough JL, Pham TM, Schibler A (2014) Physiologic effect of high-flow nasal cannula in infants with bronchiolitis. Pediatr Crit Care Med 15(5):e214–e219. https://doi.org/10.1097/PCC.0000000000000112
Keenan SP, Sinuff T, Cook DJ, Hill NS (2004) Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med 32(2):2516–2523
Ten Brink F, Duke T, Evans J (2013) High-flow nasal prong oxygen therapy or nasopharyngeal continuous positive airway pressure for children with moderate-to-severe respiratory distress? Pediatr Crit Care Med 14(7):e326–e331. https://doi.org/10.1097/PCC.0b013e31828a894d
Kepreotes E, Whitehead B, Attia J, Oldmeadow C, Collison A, Searles A, Goddard B, Hilton J, Lee M, Mattes J (2017) (HFWHO RCT): an open, phase 4, randomised controlled trial. Lancet 389(10072):930–939. https://doi.org/10.1016/S0140-6736(17)30061-2
Milani GP, Plebani AM, Arturi E, Brusa D, Esposito S, Dell'Era L, Laicini EA, Consonni D, Agostoni C, Fossali EF (2016) Using a high-flow nasal cannula provided superior results to low-flow oxygen delivery in moderate to severe bronchiolitis. Acta Paediatr 105(8):e368–e372. https://doi.org/10.1111/apa.13444
Franklin D, Babl FE, Schlapbach LJ, Oakley E, Craig S, Neutze J, Furyk J, Fraser JF, Jones M, Whitty JA et al (2018) A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 378(12):1121–1131. https://doi.org/10.1056/NEJMoa1714855
Wang EE, Milner RA, Navas L, Maj H (1992) Observer agreement for respiratory signs and oximetry in infants hospitalized with lower respiratory infections. Am Rev Respir Dis 145(1):106–109
National Institute for Health and Care Excellence (2015) Bronchiolitis: diagnosis and management of bronchiolitis in children. Clinical Guideline NG 9
Zorc JJ, Hall CB (2010) Bronchiolitis: recent evidence on diagnosis and management. Pediatrics 125(2):342–349. https://doi.org/10.1542/peds.2009-2092
Franklin D, Dalziel S, Schlapbach LJ, Babl FE, Oakley E, Craig SS, Furyk JS, Neutze J, Sinn K, Whitty JA et al (2015) PARIS and PREDICT. Early high flow nasal cannula therapy in bronchiolitis, a prospective randomised control trial (protocol): a Paediatric Acute Respiratory Intervention Study (PARIS). BMC Pediatr 14(15):183. https://doi.org/10.1186/s12887-015-0501-x
Mayfield S, Bogossian F, O'Malley L, Schibler A (2014) High-flow nasal cannula oxygen therapy for infants with bronchiolitis: pilot study. J Paediatr Child Health 50(5):373–378. https://doi.org/10.1111/jpc.12509
Subhi R, Smith K, Duke T (2009) When should oxygen be given to children at high altitude? A systematic review to define altitude-specific hypoxaemia. Arch Dis Child 94(1):6–10. https://doi.org/10.1136/adc.2008.138362
Sinha IP, McBride AKS, Smith R, Fernandes RM (2015) CPAP and high-flow nasal cannula oxygen in bronchiolitis. Chest 148(3):810–823. https://doi.org/10.1378/chest.14-1589
Schibler A, Pham TM, Dunster KR, Foster K, Barlow A, Gibbons K, Hough JL (2011) Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery. Intensive Care Med 37(5):847–852. https://doi.org/10.1007/s00134-011-2177-5
Abboud PA, Roth PJ, Skiles CL, Stolfi A, Rowin ME (2012) Predictors of failure in infants with viral bronchiolitis treated with high-flow, high-humidity nasal cannula therapy. Pediatr Crit Care Med 13(6):e343–e349. https://doi.org/10.1097/PCC.0b013e31825b546f
McKiernan C, Chua LC, Visintainer PF, Allen H (2010) High flow nasal cannulae therapy in infants with bronchiolitis. Pediatr 156(4):634–638. https://doi.org/10.1016/j.jpeds.2009.10.039
Lamb K, Piper D (2016) Southmedic OxyMask(TM) compared with the Hudson RCI(®) non-rebreather mask(TM): safety and performance comparison. Can J Respir Ther Winter 52(1):13–15
Everard ML (1995) Bronchiolitis. Origins and optimal management Drugs 49(6):885–896
Acknowledgements
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/HMz1WF
Author information
Authors and Affiliations
Contributions
Conception: ABE; Design: ABE, EC; Supervision: ABE; Materials: ABE, IG, HS, YAT, AK; Data collection and processing: ABE, EC; Analysis and/or interpretation: ABE, GZ, EC; Literature review: ABE, EC; Writer: ABE; Critical review: ABE.
Corresponding author
Ethics declarations
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all participants included in the study.
Conflict of interest
The authors declare that they have no conflicts of interest.
Informed consent
Consent was obtained from all individual parents and participants included in the study
Additional information
Communicated by Peter de Winter
Electronic supplementary material
ESM 1
(DOCX 21.3 kb)
Rights and permissions
About this article
Cite this article
Ergul, A.B., Calıskan, E., Samsa, H. et al. Using a high-flow nasal cannula provides superior results to OxyMask delivery in moderate to severe bronchiolitis: a randomized controlled study. Eur J Pediatr 177, 1299–1307 (2018). https://doi.org/10.1007/s00431-018-3191-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3191-1