Abstract
Recently, the utilization of medical clowns to reduce anxiety, stress, and even pain associated with hospitalization has become popular. However, the scientific basis of this benefit and outcome is scant. Venipuncture and IV cannulation are very common sources of pain in ill children. To reduce pain, one common approach is to apply a local anesthetic prior to the procedure. In the current study, we sought to compare the utilization of medical clowning in this process with two control groups: (1) local anesthetic cream (EMLA®, Astrazeneca, London, UK) applied prior to the procedure (active control) and (2) the procedure performed with neither clown nor EMLA (control group). We hypothesized that a medical clown will reduce pain, crying, and anxiety in children undergoing this procedure.
Children aged 2–10 years who required either venous blood sampling or intravenous cannulation were recruited and randomly assigned to one of the three groups. Outcome measures consisted of the duration of the whole procedure (measured objectively by an independent observer), the duration of crying (measured objectively by an independent observer), subjective assessment of pain level (a commonly used validated scale), and anxiety level regarding future blood exams (by questionnaire). Analysis of variance (ANOVA) was used to compare between the groups. p < 0.05 was considered statistically significant.
One hundred children participated. Mean age was 5.3 ± 2.5 years (range 2–10 years). The duration of crying was significantly lower with clown than in the control group (1.3 ± 2.0 vs 3.8 ± 5.4 min, p = 0.01). With EMLA, this duration was 2.4 ± 2.9 min. The pain magnitude as assessed by the child was significantly lower with EMLA than in the control group (2.9 ± 3.3 vs 5.3 ± 3.8, p = 0.04), while with clown it was 4.1 ± 3.5, not significant when compared with the other two modalities. Hence, duration of crying was shortest with clown while pain assessment was lowest with EMLA. Furthermore, with clown duration of cry was significantly shorter than in controls, but pain perception did not significantly differ between these groups. As expected, the duration of the entire process was shortest in the control group (5.0 ± 3.8 min), moderate with clown (19.3 ± 5.8 min), and longest with EMLA (63.2 ± 11.4 min, p < 0.0001 between all). Parental reporting of a beneficial effect was greater with clown than with EMLA (3.6 ± 0.8 vs 3.0 ± 1.1, p = 0.02). Parental assessment of child’s anxiety related to future blood tests as evaluated by telephone the following day revealed that it was significantly lower with clown than in the control group or EMLA (2.6 ± 1.2 vs 3.7 ± 1.3 or 3.8 ± 1.6, p < 0.01 for both).
Conclusions: Distraction by a medical clown is helpful in children undergoing blood tests or line insertion. Although pain reduction was better with EMLA, both duration of cry and anxiety were lower with a medical clown. These results strongly encourage and support the utilization of medical clowns while drawing blood in children.
What is Known: |
• Venipuncture and IV cannulation are common sources of pain in children, which may be reduced utilizing a local anesthetic cream. • The utilization of medical clowns in these procedures has never been studied in a direct comparison with the use of anesthetic topical cream. |
What is New: |
• This novel study shows the ability of the medical clown to reduce anxiety and relive pain related to venipuncture and IV cannulation in children. • While topical anesthesia reduces pain, distraction by a clown reduces crying and anxiety in children undergoing blood exams. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venipuncture and IV cannulation are the two most common sources of pain in hospitalized children [13]. These procedures in children are often associated with stress, pain, crying, and can even fail due to a child’s irritability [23].
Understanding the ontogeny of the pediatric pain experience has increased significantly over the past 2 decades. Alleviating pediatric pain experience has become a major interest in the pediatric wards, and guidelines to deal with pediatric pain have been proposed [15]. Medical clowning is a relatively new approach and has expanded in recent years. Previous studies have shown that it can encourage oncology patients and even improve their immune function [1–3].
In pediatrics, medical clowns can distract the child during invasive procedures such as venipuncture, IV line insertion, and urinary bladder catheterization. [10, 11, 20, 21]. To deal with the pain related to venipuncture and IV cannulation, several methods have been suggested such as general sedation, local anesthesia [16], and recently, the distraction by a professional medical clown. However, currently, medical staff tend not to support the utilization of medical clowning predominantly due to lack of supporting evidence and the claim that it might delay the procedure [21]. Thus, in the current study, we planned to scientifically investigate the utility of medical clowning in such procedures and compare it to control condition and active control (local anesthesia). For this, we utilized a eutectic mixture of lidocaine 2.5 % and prilocaine 2.5 % which is indicated as a topical anesthetic cream (EMLA®, Astrazeneca, London, UK). We hypothesized that the utilization of medical clowning may in fact help when carrying out such minimally invasive procedures with reduced anxiety and pain and even improve the success and reduce duration of the procedure. Furthermore, reducing the pain associated with the procedure may result in diminished stress and fear from similar procedures in the future [13].
Methods
The study was approved by the Carmel IRB committee for human subject studies, and a parent had to give an informed consent prior to recruitment. Children were recruited from the emergency room and inpatient ward of Department of Pediatrics at the Carmel Medical Center. Inclusion criteria consisted of children aged 2–10 years, who required blood sampling/line insertion for clinical reasons. Children in this age group who were acutely ill and unstable or potentially so were excluded.
Following consent form signature and recruitment, children were randomly divided into three groups. There were specific time frames planned for the study (requiring clown and independent observer to be present), and within these time frames children and parents were invited to participate in the study, the arm of the study determined by order of arrival:
-
1.
Blood exam/venipuncture by standard clinical methods (without special aid, control group)
-
2.
Blood exam/venipuncture with a medical clown
-
3.
Blood exam/venipuncture under local anesthesia (EMLA).
The study clown underwent special training as a medical clown in which he studied both humor and distraction techniques and general children’s health and diseases, as well as safety and infection control measures. He had over 5 years of experience of hospital work in general and 3 years in the pediatric department in particular. In order to distract the children, the clown performed a series of funny actions such as inflating a comical balloon, humorous noises of animals, playing an accordion, and singing funny songs.
The primary outcome of the study was the duration of the crying phase, assessed by an independent observer, and additive in cases of intermittent crying episodes. The independent observer was a research assistant who measured the various duration of crying with a stopwatch. She did not have specific training nor was she part of the study team and was recruited specifically for this role. The duration of crying was defined as crying preceding the procedure (defined as the time of crying from the moment the child entered the examination room and until the child was lying on the examination bed), crying during the procedure of venipuncture, and crying following the procedure (from the time blood was drawn or IV line was inserted and until time of cessation of crying). Secondary outcome measures consisted of the duration of the whole procedure (determined by an independent research assistant), pain level assessed by the child, and quantitative evaluation of the child’s pain and anxiety by the parents (visual analogue scale, VAS). Pain level evaluated by the child was based on a scale of 10 faces (with numbered scale under the faces) running from a smiling face at one end (indicating no pain, =0) to a crying face at the other end (indicating terrible pain, =10) [18, 22]. Parents assessed their child’s pain and anxiety by a VAS. This VAS is a 10-cm line which runs from no pain (=0 cm) up to maximal pain (=10 cm) and parents indicated the line, and their response was measured in centimeters from the left. A similar VAS was used for anxiety. Overall positive effect of either the clown or EMLA was assessed by a simple question asking parents to rate on a scale of 0–5 whether the clown or the EMLA had a positive effect on the process (0 = no effect, 5 = maximal effect). Anxiety level regarding future blood exams was assessed by a research assistant’s telephone call 24 h after the procedure asking a simple question to score their estimate of the child’s anxiety in a non-validated 0–5 scale. Analysis of variance (ANOVA, for comparison of all groups) and unpaired two-tailed t tests (for comparisons between two groups) were used. p < 0.05 was considered statistically significant..
Detailed process
Description of the intervention by group:
-
1.
Blood exam/venipuncture standard routine way (control group):
The child lay on the bed while the parent was holding and talking to the child. A nurse held the hand of the child as the physician took the blood sample.
-
2.
Blood exam/venipuncture with medical clown assistance:
The clown utilized his expertise with music, magic, stories, etc., to entertain and distract the child while the blood exam was performed. The process (clown activity) started 10 min before the blood exam and was completed when the child left the room after venipuncture/IV placement.
-
3.
Active control group—children with local anesthesia by EMLA:
Local anesthesia consisted of a mixture of lidocaine and prilocaine was applied locally on skin surface at the site of planned venipuncture. After waiting for 50 min (time required for anesthesia), the blood sampling procedure was performed in the routine way.
Data analysis
Sample size calculation
Given an alpha error of 5 % and a power of 0.8, with predicted difference between the methods of 10 % on the pain/anxiety scales (estimation for clinical relevance), 90 children were required for the study (30 children in each group).
Statistical analyses
Analysis of variance (ANOVA, for comparisons of the three groups) and unpaired two-tailed t tests (for comparisons between two groups) were used. p < 0.05 was considered statistically significant.
Results
One hundred children participated in the trial. Mean age was 5.3 ± 2.5 years (range 2–10 years). Male to female ratio 1.12 (53:47, respectively). There were slightly but significantly more boys in the clown and control groups than in the EMLA group (Table 1). Of the 100 children participating, 41 underwent IV cannulation, and the rest underwent blood exam without IV cannulation (in the medical clown group the ratio was 3:1, in the EMLA group 2.3:1, and in the control group 2.4:1 IV cannulation vs blood exam). Average clock time of examination was 12:00 PM, which was similar for all subgroups. The medical reasons for requiring blood exam/ IV cannulation were variable. Common indications were fever, abdominal pain, limp, vomiting, and many others. This was similar, with no statistical differences, between the three subgroups. Most children required IV cannulation due to inability to drink, vomiting, or the need for IV therapy for various reasons (for example, IV fluids or medicines). These were also similar with no differences between the three groups. In the clown group (n = 33), none of the children reacted with coulrophobia (fear of clowns).
The mean number of blood examinations experienced by each participant prior to the current study was similar between the groups; in the clown group, there were 2.48 ± 1.80 (range 0–8) previous blood examinations, compared to 2.88 ± 2.63 (range 0–8) in the EMLA group and 1.90 ± 1.34 (range 0–8) in the control group (p = NS for all). While there were no differences between the groups, there was a general significant negative correlation between the number of previous blood exams and anxiety in the current exam (r = −0.25, p = 0.012).
Twenty-seven participants had elevated body temperature during the procedure (defined as above 38° C). Forty-three percent of these were in the clown group, 24 % in the EMLA group, and 33 % in the control group.
The average number of attempts required in order to perform the exam was 1.15 (range 1–4), with no differences between the groups: in the medical clown group 1.19 attempts (range 1–4), in the EMLA group 1.2 attempts (range 1–3), and 1.10 (range 1–3) in the control group (NS for all).
Of the 100 children who participated in the study, 30 children were admitted for further examination and therapy. There were no age or gender differences between the admitted and discharged children, although there was a minimal trend for younger children to be hospitalized. The within group distribution (percentage) between the medical clown/EMLA/control groups in the hospitalized vs discharged children was similar. In the hospitalized group, there was an understandably significantly higher percentage of IV line insertions than in the discharged group (73 % IV line insertion and 27 % blood exam in the hospitalized children, compared to 27 % IV line insertion and 73 % blood exam in the discharged group, p < 0.05).
The duration of the whole process was the shortest in the control group(5.0 ± 3.8 min, median 4.0), moderate in the clown group (19.3 ± 5.8 min, median 20.0), and longest with EMLA (63.2 ± 11.4 min, median 63.0, p < 0.0001 between all, given the significant waiting time until EMLA was effective). The time required for performing blood examination itself (defined as the time from the moment the child was lying in the bed and prepared for the procedure and up to the child returning to the parents’ care) was similar between the groups: in the medical clown group 2.46 ± 1.28 min (range 1–6 min, median 2 min), in the EMLA group 2.38 ± 0.9 min (range 1-6 min, median 2 min), and in the control group 2.68 ± 0.7 min (range 1-6 min, median 1.55 min, p = NS for all).
The duration of crying was significantly lower with clown than in the control group (1.3 ± 2.0 vs 3.8 ± 5.4 min, p = 0.01). With EMLA, this duration was intermediate: 2.4 ± 2.9 min, median 1.5 min (Table 2), not statistically different compared to clown or no aid groups.
Importantly, the duration of crying preceding the procedure (defined as the time of crying from the moment the child entered the examination room and up to the child was lying on bed) was significantly shortest with medical clown: 0.12 ± 0.21 min (range 0–3 min) vs 0.81 ± 0.90 min (range 0–3 min) with EMLA (p < 0.05) and 1 ± 0.60 min (range 0–3 min) in the control group (p < 0.01). There was no difference in duration of crying preceding the procedure between the EMLA and control group. Of note, the crying time following the procedure was relatively short in both the medical clown and the EMLA groups, but long in the control group (0.60 ± 0.83, range 1–6, median 0 min, 0.75 ± 0.84, range 1–6, median 0 min, and 2.1 ± 1.3, range 1–6, median 1 min, respectively, p < 0.05 between the clown and EMLA groups and the control group). There was no statistically significant difference in crying duration after the procedure between the clown and EMLA group. Interestingly, pain magnitude assessment by the child was significantly lower with EMLA than in controls (2.9 ± 3.3 (median 1.5 min) vs 5.3 ± 3.8 (median 5 min), p = 0.04), while with clown it was 4.1 ± 3.5 (median 5 min), not significant when compared with the other two modalities).
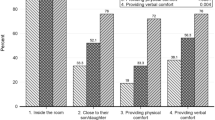
Parental assessment of child’s pain (VAS assessment of the parent on a scale of 0–10) was lowest in the medical clown group vs the other two modalities (2.35 ± 2.38 in the medical clown group, 3.24 ± 3.53 in the EMLA group, and 5.2 ± 3.2 in the control group, p < 0.05 between all groups). Similarly, parental assessment of child’s anxiety during the physical exam (VAS) was significantly lower in the medical clown group vs the EMLA group (2.98 ± 3.21 vs 5.60 ± 3.43, p = 0.05).
Parental reporting of the overall positive affect was significantly better with medical clown distraction than with EMLA (3.6 ± 0.8 vs 3.0 ± 1.1, p = 0.02). Parental reporting regarding their perception of the “traumatic” affect experienced by the child was also examined, and it was found that medical clown had a greater affect in trauma reduction (by parental report) as compared to EMLA (3.57 ± 0.57 vs 2.80 ± 0.87, p < 0.05).
Based on the pediatrician performing the blood exam/venipuncture perspective, pain level experienced by the child was similar in the EMLA and medical clown groups, and much higher in the control group (VAS scale 0–10): medical clown group 2.77 ± 2.07, EMLA 2.70 ± 1.80, and control group 4.4 ± 2.72). As for child’s anxiety estimated by the pediatrician, a major difference was noticed between the medical clown group and the other two modalities (medical clown group 2.91 ± 2.53, EMLA group 4.84 ± 3.56 and control group 5.8 ± 3.06, p < 0.05 between clown and the other two groups).
All parents were contacted by phone the following day. Their assessment of their child’s anxiety of future blood tests revealed that it was lower with clown than in controls or EMLA (2.6 ± 1.2 vs 3.7 ± 1.3 or 3.8 ± 1.6, p < 0.05 for both, Table 2).
Discussion
The current study shows that distraction by a medical clown is very helpful in children undergoing blood tests or intravenous catheter insertion. Although pain was lower with EMLA, both crying duration and anxiety were lower with the medical clown. Furthermore, the duration of the process was shorter with medical clown than with EMLA. These results strongly encourage and support the utilization of medical clowns while drawing blood in children. The effect of the presence of medical clown during blood exam\venipuncture in children has not been very systematically studied previously. Thus, our data are novel and enhance the existing literature.
Several factors are known to affect pain sensation associated with venipuncture or IV insertion. These include body temperature, age, past pain experience/blood exams, time of the day (circadian effect), personal and environmental factors, and the specific medical condition of the individual [13, 17, 23]. Since the current study was randomized, these factors were comparable between the groups. Age, past blood exams, clocktime, and reason for venipuncture were similar between the three groups.
In order to assess pain and anxiety levels in the current study, we chose several parameters, such as crying duration, anxiety level based on a VAS assessed by the child, by the parent, and by the staff. While crying duration is an easy numerical parameter, crying intensity is more subjective. Furthermore, assessment of anxiety and pain are substantially subjective. In order to reduce potential skewing of the results, we took several steps: 1. study conditions, timing, and population were similar between the groups. 2. objective measures (cry duration) was quantified by an independent objective observer. 3. study was randomized.
Greater reduction in crying duration associated with venipuncture in the clown group compared with the other two modalities was measured (Table 2). This probably represents decreased anxiety but not necessarily decreased pain. We believe that the reduction in crying duration results from the distraction, calming effect, and atmosphere created by the clown as described previously [8, 20]. Reduction in anxiety level in the medical clown group compared to the other two modalities was the main result of our study. Although the relationship between anxiety and pain is well-established [9, 13], in our study pain assessment (by the child) was greater with clown than with EMLA, yet the duration of crying was significantly lower with clown. This observation emphasizes the role of anxiety and fear of children in the setting of blood drawing, which is greater the actual pain level. Parental emotions, behavior, and health also play a role in children’s pain experiences. Overly protective parental behaviors increase distress and pain for the child [17]. Thus, while EMLA affects predominantly the child, clown activity affects both child and the parent, directly and indirectly (i.e., the parent is affected by both the clown and the positive response of the child). This further supports the mechanism of reduced crying duration with the clown despite lesser pain reduction. Parents in the medical clown group reported less pain for their children, probably secondary to the shorter duration of crying (Table 2). Hence, pain assessment was similar for children and their parents in the control group, but differed in the other two groups. While in the clown group, parents underestimated their children’s pain (probably due to shorter cry), in the EMLA group they overestimated it (probably due to longer cry, Table 2). Of note, none of our participants experienced coulrophobia (fear of clowns). The phenomenon of coulrophobia is clinically known and was previously reported in descriptive reports, but there are very sparse data in this regard and the exact prevalence of it still needs to be studied.
Pain is an inherently subjective experience and should be assessed and treated as such. Pain has sensory, emotional, cognitive, and behavioral components that are interrelated with environmental, developmental, sociocultural, and contextual factors. The concepts of pain and suffering extend well beyond that of a simple sensory experience.
Barriers to the treatment of pain in children include the following: (1) the myth that children do not feel pain the way adults do, or if they do, there is no untoward consequence, (2) positive aspects of pain such as “strengthening”, (3) misunderstanding of how to conceptualize and quantify a subjective experience, (4) the notion that addressing pain in children takes too much time and effort [6, 19]. Nowadays, assessment of pain and pain reduction is part of the standard of care given by any clinician [6, 19]. Several techniques to reduce negative effects have been studied [15, 18, 22]. One of the methods to reduce the pain of blood exam is the application of a local anesthetic cream. EMLA, which was utilized in the current study, is a mixture of lidocine 2.5 % and prolicain2.5 %. One disadvantage of this preparation is the long absorption time when applied on the dermis (3 mm in 60 min and 5 mm in 90 min.), therefore, it is important to apply the cream at least 50–60 min before blood exam. Additionally, applying EMLA on open or wounded skin may cause adverse effects such as methemoglobinemia and local allergic reaction [4, 5, 7, 24]. Furthermore, clinical experience has shown that blood exam with EMLA may require more venipuncture attempts as compared to no aid due to vasoconstriction [4], although this was not the case in the current study. On the other hand, EMLA was shown to reduce the painful experience of blood examination when compared to the control group [5], which consumes less time, has no adverse effects and incurs no medical expenses.
Of the 100 participants in this study, 30 children were hospitalized. These children tended to be younger than those who were discharged (although not statistically significant). The fact that hospitalized children had significantly higher rates of IV line insertion as opposed to blood tests indicates that hospitalization was anticipated by the treating pediatrician, but this should not affect the results of the study since the distribution to control/clown/EMLA was similar. Whether clown intervention can affect the decision to hospitalize or the duration of hospitalization was not in the scope of this study. Many previous factors have been shown to affect hospitalization and healthcare use such as body mass index, sleep disturbances, and lifestyle . [12, 14] which were not monitored in the current study.
While the strength of our study is the large sample size, randomization, and objective measures by independent observers, there are several limitations as well. First, the study was not blinded (i.e., the pediatrician, the parent, and the observer knew to which group the child belonged) which may have biased their judgment in questionnaires and subjective measures. This is of special importance when dealing with subjective measures. Secondly, there are no excellent quantitative measures for pain and anxiety. We used questionnaires and visual analog scales which are commonly used but not perfect [15, 18, 22]. Thirdly, we did not monitor children and families who declined participation and did not characterize the character of the parents. These may have affected the results. For example, families with potential coulrophobia may have declined participation. Finally, our study consisted of a wide range of both ages and medical conditions and indications for blood sampling. While including many diagnoses shortened study duration and allowed a large recruitment rate, it may have confounded our results. However, as the study was randomized, we do not think there was a bias toward any specific indication in any of the groups, and indeed, checking this statistically post factum, we found no differences between groups with regard to age, diagnosis, blood drawing vs venipuncture, and reason for admission (specific illness).
Conclusion
Despite these limitations, we believe our study is valid, indicating that utilization of medical clowns to reduce pain and anxiety during blood drawing is effective, safe, and has less negative effects on future blood examinations. Parents of children in the clown group felt that the child had less pain, less crying, and suffered less from the procedure. Future study of combining the use of EMLA with the use of medical clowns should be performed.
Abbreviations
- EMLA:
-
Eutectic mixture of local anesthetics
- IV:
-
Intravenous
- IVIG:
-
Intravenous immunoglobulin
- IRB:
-
Institutional review board
- NS:
-
No significant difference
- Min:
-
Minutes
- VAS:
-
Visual analogue scale
References
Anand KJ, Hickey PR (1987) Pain and its effects in the human neonate and fetus. NEJM 317:1321–1329
Bennett MP, Zeller JM, Rosenberg L, McCann J (2003) The effect of mirthful laughter on stress and natural killer cell activity. Altern Ther Health Med 9:38–45
Berry FA, Gregory GA (1987) Do premature infants require anesthesia for surgery? Anesthesiology 67:291–293
Bjerring P, Andersen PH, Arendt-Nielsen L (1989) Vascular response of human skin after analgesia with emla Cream. Br J Anaesth 63:655–660
Chen BK, Cunningham BB (2001) Topical anesthetics in children: agents and techniques that equally comfort patients, parents, and clinicians. Curr Opin Pediatr 13:324–330
Committee on Psychosocial Aspects of Child and Family Health and Task Force on Pain in Infants, Children, and Adolescents (2001) The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 108:793–797
Fradet C, McGrath PJ, Kay J, Adams S, Luke B (1990) A prospective survey of reactions to blood tests by children and adolescents. Pain 40:53–60
Glasper EA, Prudhoe G, Weaver K (2007) Does clowning benefit children in hospital? Views of Theodora Children’s. J Child Young People Nurs 1:24–28
Golan G, Tighe P, Dobija N, Perel Keidan A (2009) Clowns for the prevention of preoperative anxiety in children: a randomized controlled trial. Pediatr Anesth 19:262–266
Hansen LK, Kibaek M, Martinussen T, Kragh L, Hejl M (2011) Effect of a clown’s presence at botulinum toxin injections in children. a randomized, prospective study. J Pain Res 4:297–300
Hanuka P, Rotchild M, Gluzman A, Uziel Y (2011) Medical clowns: dream doctors as an important team member in the treatment of young children with juvenile idiopathic arthritis. 18th Pediatric Rheumatology European Society (PReS) Congress Bruges, Belgium. 14–18 September
Hering E, Pritzker I, Gonchar L, Pillar G (2009) Obesity in children is associated with increased health care use. Clin Ped 48:812–818
Kennedy RM, Luhmann J, Zempsky WT (2008) Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics 122:S130–S133
Kheirandish-Gozal L, Etzioni T, Bhattacharjee R, Tan HL, Samiei A, Molero Ramirez H, Abu Eta B, Pillar G (2013) OSA in children is associated with severity dependant deterioration in overnight endothelial function. Sleep Med 14:526–531
Lee GY, Yamada J, Kyololo O, Shorkey A, Stevens B (2014) Pediatric clinical practice guidelines for acute procedural pain: a systematic review. Pediatrics 133:500–515
Maunuksela E, Korpela MR (1986) Double-blind evaluation of a lignocine-prilocaine cream (EMLA) in children effect on the Pain Associated with Venous Cannulation. J Med BJA 58:1242–1245
Palermo TM, Valrie CR, Karlson CW (2014) Family and parent influences on pediatric chronic pain: a developmental perspective. Am Psychol 69:142–152
Ruskin D, Lalloo C, Amaria K, Stinson JN, Kewley E, Campbell F, Brown SC, Jeavons M, McGrath PA (2014) Assessing pain intensity in children with chronic pain: convergent and discriminant validity of the 0 to 10 numerical rating scale in clinical practice. Pain Res Manag 19:141–148
Schechter NL, Berde CB, Yaster M (1993) Pain in infants, children, and adolescents: an overview. In: Schechter NL, Berde CB, Yaster M (eds) Pain in Infants, Children, and Adolescents. Williams & Wilkins, Baltimore, pp 3–9
Tener D, Lev-Wiesel R, Franco NL, Ofir S (2010) Laughing through this pain: medical clowning during examination of sexually abused children: an innovative approach. J Child Sex Abuse 19:128–140
Vagnoli L, Caprilli S, Robiglio A, Messeri A (2005) Clown doctors as a treatment for preoperative anxiety in children: a randomized, prospective study. Pediatrics 116:e563–e567
von Baeyer CL, Stevens BJ, Chambers CT, Craig KD, Finley GA, Grunau RE, Johnston CC, Pillai Riddell R, Stinson JN, Dol J, Campbell-Yeo M, McGrath PJ (2014) Training highly qualified health research personnel: the pain in Child Health consortium. Pain Res Manag 19:267–274
Walco GA (2008) Needle pain in children: contextual factors. Pediatrics 122:S125–S129
William T, Zempsky WT, Cravero JP (2012) Relief of pain and anxiety in pediatric patient in emergency medical sysyem committee on pediatric emergency medicine, and section on anesthesiology and pain medicine. Pediatrics 130:e1391–e1405
Acknowledgments
The study was funded by a non-restrictive grant from MAGI foundation.
The authors have no financial relationship with the organization that sponsored the research any other conflict of interest regarding this research
Author's contributions
All authors participated in study design, data collection and manuscript drafting and approving.
Data analyses were performed by N. Meiri and G. Pillar.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Carmel IRB committee for human subject studies, and a parent had to give an informed consent prior to recruitment.
Additional information
Communicated by Jaan Toelen
Revisions received: 10 April 2015; 15 June 2015; 25 September 2015
Rights and permissions
About this article
Cite this article
Meiri, N., Ankri, A., Hamad-Saied, M. et al. The effect of medical clowning on reducing pain, crying, and anxiety in children aged 2–10 years old undergoing venous blood drawing—a randomized controlled study. Eur J Pediatr 175, 373–379 (2016). https://doi.org/10.1007/s00431-015-2652-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2652-z