Abstract
In children with ileocolic intussusception sonography is increasingly being used for diagnosis, whereas fluoroscopy is frequently used for guiding non-invasive reduction. This study assessed the success rate of radiation-free sonography-guided hydrostatic reduction in children with ileocolic intussusception, using novel well-defined success rate indices. All children were evaluated who presented from 2005 to 2013 to the local university hospital with ileocolic intussusception. The patients were treated with sonography-guided hydrostatic reduction unless primary surgery was clinically indicated. The according success rate was determined by indices of Bekdash et al. They represent the ratio of persistently successful non-surgical reductions versus four different denominators, depending on including/excluding cases with primary surgery and including/excluding cases requiring bowel resection/intervention. Fifty-six consecutive patients were included (age, 3 months to 7.8 years). About 80 % of the patients presented until 24 h and 20 % until 48 h after the onset of symptoms. Seven patients underwent primary surgery, with bowel resection required in three cases. Hydrostatic reduction was attempted in 49 patients, being permanently successful in 41 cases (selective reduction rate 41/49 = 83.7 %; crude reduction rate 41/56 = 73.2 %). The remaining eight patients underwent secondary surgery, with just two patients not requiring surgical bowel resection/intervention (corrected selective reduction rate 41/43 = 95.3 %). The composite reduction rate was 87.2 % (successful/feasible reductions, 41/47). Conclusion: Radiation-free sonography-guided hydrostatic reduction has a good success rate in children with ileocolic intussusception. It may be particularly valuable in centers that are already experienced with using sonography for the diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ileocolic intussusception with telescoping of the terminal ileum into the colon may be fatal if persistent, since the intussuscepted bowel subsequently becomes ischemic, necrotic, and perforates with associated peritonitis [1, 9, 19, 20]. However, with early diagnosis and treatment, the disease has a good prognosis. In young children, ileocolic intussusception is often idiopathic without obvious lead point [1]. Classical clinical symptoms are colicky pain, vomiting, and bloody stool, and the intussusception may present as a palpable mass [1, 20]. However, these signs and symptoms may not all be present or may have causes other than intussusception. For differential diagnosis, an abdominal ultrasonography is well suitable, having a high accuracy for detecting and excluding ileocolic intussusception in children [1, 15, 17, 19, 29]. Many cases can be non-surgically reduced by air or contrast enema under fluoroscopic guidance [4, 19, 29]. An evolving alternative is sonography-guided hydrostatic reduction that requires no radiation and no change of imaging methods in case of sonography-based diagnosis [17, 21, 22, 25].
The purpose of this study was to analyze the failure and success of sonography-guided hydrostatic reduction in a consecutive cohort of children with ileocolic intussusception.
Patients and methods
Patients
From January 2005 to December 2013 (9 years), all children were recorded who presented to the University Hospital of Goettingen with ileocolic intussusception. In that city and its surroundings, this is generally the site where the children with suspected intussusception are admitted to by their physicians or parents. Additional data were retrospectively retrieved from patient charts, digital information systems, and archived sonography images. The local ethics committee waived ethical approval of this type of study.
Sonography-based diagnosis
After obtaining the history, such as clinical examination, placing an IV line, and taking blood samples for laboratory studies, patients with suspected intussusception generally received an abdominal sonography shortly after admission. The abdomen was studied by a 5 MHz curved-array transducer and the bowel by an 8 MHz linear transducer. Until July 2011, a HDI ATL 5000 ultrasound system (Philips, Hamburg, Germany) and since then a Logiq E9 instrument (GE Healthcare, Solingen, Germany) was used.
Sonography-guided hydrostatic reduction with saline enema
In clinically stable patients with confirmed intussusception, a sonography-guided hydrostatic reduction [22, 25, 30] was attempted with informed parental consent in agreement with the pediatric surgeons. During regular hours, the procedure was jointly performed by the author and his pediatric assistants learning sonography, and during off-hours by one or more of eight experienced pediatricians and pediatric surgeons. The patient was placed on the sonography table in supine position without sedation. A Foley catheter was inserted into the rectum, and the balloon was inflated with about 5 mL of air to seal the anus and prevent outflow of the saline [5]. The catheter was connected to a bag with warmed saline, hanging 50–100 cm above the child (37–74 mmHg pressure gradient). The reduction of the intussusception was monitored using the linear sonography transducer. The saline enema usually pushed back the intussuscepted bowel into the ascending colon with little effort, but the remainder in front of the ileocecal valve was frequently more resistant. For reduction of this remainder, up to three attempts lasting up to 3 min were made with the saline bag elevated to 100–150 cm above the child (74–110 mmHg) [14, 30]. Between such phases of elevated hydrostatic pressure, the saline bag was lowered to relieve the pressure and allow for bowel perfusion [30]. The pressure was limited to such levels to avoid bowel perforation. The hydrostatic reduction was considered successful if saline was flowing through the ileocecal valve into the terminal ileum [25] and if the completely reduced (and generally wall-thickened) terminal ileum was visualized without residuals of the intussusception. Unsuccessful cases were referred to surgical reduction according to individual clinical decisions. Patients with successful hydrostatic reduction were routinely reevaluated by sonography the next day. This was done earlier, if a recurrent intussusception was clinically suspected. In recurrent intussusceptions up to two further hydrostatic reductions were performed. If technically successful but succeeded by a further recurrence then surgery was performed [16], since a pathologic lead point might be causative to avoid bowel lesions and to provide a definite solution.
Primary surgical treatment
Patients with sonography-confirmed ileocolic intussusception and markedly reduced general condition (as assessed on clinical grounds, including lethargy) were treated by primary surgical reduction without attempting hydrostatic reduction. Additional bowel resection was performed as required.
Patient groups
For analysis, the patients were grouped by their outcome into four major groups:
-
(A)
Primary hydrostatic reduction successful without recurrence;
-
(B)
Primary hydrostatic reduction technically successful, but recurrence leading to surgery;
-
(C)
Primary hydrostatic reduction not possible, leading to surgery;
-
(D)
Primary surgery because of markedly reduced general condition.
In this study, all patients of group (B) showed repeated recurrence of the intussusception despite of technically successful hydrostatic reductions; otherwise, an according patient group “repeated reduction in recurrent intussusception, leading to permanent success” would have been defined. The surgical groups (B−D) were furthermore subdivided into two subgroups: (1) pure surgical reduction and (2) with bowel resection or other intervention that was required in addition to surgical reduction.
Indices of success in hydrostatic reduction
The success rate of sonography-guided hydrostatic reduction was determined by four indices defined by Bekdash et al. [3]. They represent the ratio of persistently successful non-surgical reductions versus four different denominators, depending on whether all patients or just the attempted non-invasive reductions are included and depending on whether patients requiring bowel resection/intervention are included or excluded (Tables 1 and 2). Additionally, the “technical success rate” of hydrostatic reduction was calculated, with technical success defined as complete reduction, also if the intussusception recurred within 48 h (Table 2).
Statistical analysis
The patient data were summarized by standard descriptive statistics. Differences between the patient groups (A−D) were studied by analysis of variance for ranked and continuous covariates, and by a generalized linear model for binomial count data. SAS 9.3 (SAS Institute, Cary, N.C., USA) was used for statistical analysis with the significance level set to P < 0.05.
Results
All patients
During the 9-year study period, 56 consecutive children were diagnosed with ileocolic intussusception. One further patient with failed hydrostatic reduction showed ileoileocolic intussusception at surgery and was excluded from this study. Among the patients with ileocolic intussusception, the age ranged from 3 months to 7.8 years (mean 2.4 years) with a small peak at ages of 6–12 months (21 % of patients). About 59 % of patients were male (33 of 56). About 60 % of patients presented until 12 h, 20 % until 24 h, and 20 % until 48 h after the onset of symptoms. Colicky pain was the most common clinical symptom (79 % of patients), followed by vomiting (38 %) and bloody stool (9 %), and 96 % of the patients showed at least one symptom of this classical triad. An abdominal mass was palpable in 29 % of cases. The general condition was reduced mildly in 23 patients, moderately in 27 patients, and markedly in 6 patients. All patients were treated by sonography-guided hydrostatic reduction and/or by surgery and survived without disabilities. Among the patients with hydrostatic reductions, one patient vomited during the procedure but did not aspirate and none encountered bowel perforation. In all surgical cases, the intussusception did not recur. Regarding the patient groups and the success of hydrostatic reduction, there were no significant differences between the 41 patients who presented during regular hours and the 15 patients who presented during off-hours. Further results of the patient groups A−D are provided in Tables 3 and 4 and in the following.
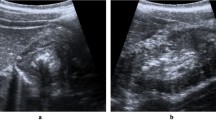
Group A. Hydrostatic reduction without recurrence
Forty-one patients (73.2 % of all) were successfully treated with hydrostatic reduction without recurrence. Their age ranged from 6 months to 7.8 years. In most cases (28 of 41), the intussusception reached to right colic flexure. On average, hydrostatic reduction was finished after 7 min (range, 3–14 min). The hydrostatic reduction was significantly more successful in patients presenting within 12 h after onset of symptoms (90.6 %, 29 of 32) than in patients presenting later (70.6 %, 12 of 17) (P = 0.016). One case is presented with sonography images elsewhere [25].
Group B. Hydrostatic reduction with recurrence, leading to surgery
In five patients, the hydrostatic reduction was technically possible, but the intussusception recurred within 24 h. Up to two further hydrostatic reductions were performed in these patients, always with technical success but further recurrence. At surgery in one patient, a Meckel’s diverticulum was resected, one patient received an ileocecal resection with lymphofollicular hyperplasia of the terminal ileum diagnosed at histopathology, and in three other patients the cecum was fixed to the terminal ileum to prevent further intussusceptions.
Group C. Hydrostatic reduction attempted but not possible, leading to surgery
In three patients, sonography-guided hydrostatic reduction failed and the parents decided not for delayed repeat enema but for surgery. Two patients had a lengthy intussusception extending into the transverse colon. In both patients, the intussusceptum was pushed back into the cecum but the remainder could not be reduced. Subsequent surgical reduction was performed without bowel resection. In the third patient, the appendix was involved into the intussusception, requiring resection. All three patients additionally had gastroenteritis with diarrhea and vomiting.
Group D. Primary surgery without attempting hydrostatic reduction
Seven patients with markedly reduced general condition were primarily treated by surgery. Their age ranged from 3 to 13 months, which was significantly younger than in the other patient groups (P = 0.002). Clinically, these young children did not show colicky pain but vomiting as the dominant clinical symptom, in addition to their markedly reduced generally condition. Also, five of them showed bloody stool, whereas the patients of the other groups did not (P = 0.018). Four of the seven patients additionally had gastroenteritis with diarrhea, two of them with viruses detected in the stool (Adenovirus and Norovirus). Five of seven patients had a relatively long intussusception, extending into the transverse colon or to the left colon flexure (P < 0.001). In three patients, sonography showed prominent free peritoneal fluid (P < 0.001). Before surgery, it was unclear who might need bowel resection in this patient group. Based on intraoperative findings such resection was required in three of the seven patients (Table 3).
Indices of success in sonography-guided hydrostatic reduction
Regarding all 56 patients, sonography-guided hydrostatic reduction was successfully applied without need for surgery in 41 patients, resulting in a “crude reduction rate” of 73.2 % (41/56; Table 2). Among the other 15 patients, 6 received pure surgical reduction and 9 additionally required bowel resection or other surgical interventions. Excluding the latter resulted in a “composite reduction rate” of 87.2 % (41/47).
Overall, hydrostatic reduction was attempted in 49 patients. In 41 patients, it was successful without surgery, leading to a “selective reduction rate” of 83.7 % (41/49). The remaining eight patients were surgically reduced because of repeated recurrences despite of technically successful hydrostatic reductions (five patients, Group B) or failed hydrostatic reductions (three patients, Group C), and six of them required bowel resection or other surgical intervention. Excluding the latter resulted in “corrected selective reduction rate” of 95.3 % (41/43).
Discussion
Ileocolic intussusception in young children is mostly idiopathic and can frequently be reduced non-surgically, if diagnosis and therapy are timely before bowel necrosis and perforation occurs [17]. Globally, sonography is used for diagnosis in about half of cases, and in Europe and North America it is becoming the favored method [19]. However, globally fluoroscopy is used for guiding non-invasive reduction in most cases [19]. With fluoroscopic guidance, air enema is considered the method of choice and more successful than liquid enema [4]. Sonography-guided hydrostatic reduction with saline enema is a radiation-free alternative [21, 22] and showed good results in this study, where most patients were diagnosed and treated relatively timely (80 % within 24 h after onset of symptoms). The technique of saline enema is simple, but sonographic imaging experience with intussusceptions is required for guiding the reduction. Therefore, this radiation-free reduction method is feasible in the large number of centers that apply sonography for diagnosing intussusceptions [1, 15, 17, 19].
Main study findings
Among 43 patients who were clinically eligible for non-surgical reduction and who did not require bowel resection or other surgical intervention, sonography-guided hydrostatic reduction showed permanent success in 95.3 % of cases (corrected selective reduction rate = 41/43, group A). Two other patients had a lengthy intussusception extending into the transverse colon that was surgically resolved (group C1).
In three other patients, a non-surgical reduction was technically successful but followed by recurrences until the cecum was surgically fixed and three further patients required bowel resection in addition to surgical reduction. Therefore, the selective reduction rate among attempted reduction was 83.7 % (41/49 patients, groups A + B + C).
Seven patients were clinically not considered eligible for hydrostatic reduction because of their markedly reduced general condition (group D). Compared to the 49 patients with attempted hydrostatic reductions, these seven patients were generally younger (3–13 months), presented not with colicky pain but with vomiting as the major symptom and some had bloody stool. Effectively, three of these seven patients (43 %, group D2) required bowel resection. The other four patients (group D1) all had bloody stool, and these cases bowel necrosis could not be ruled out before surgical inspection.
In total, 41 of 56 patients were treated without surgery, indicating the overall applicability of sonography-guided hydrostatic reduction (crude reduction rate, 73.2 %). The other 15 patients (26.8 % of 56) required primary or secondary surgery, with bowel resection in six cases and fixation of the cecum in three cases. Among the six surgical patients with no bowel resection, there were four patients in whom primary surgery had been clinically indicated (group D1). Therefore, only in 2 of 56 patients (group C1) a different non-invasive reduction method might (or might not) have been more successful than sonography-guided hydrostatic reduction.
All five patients with bloody stool had a markedly reduced general condition and underwent primary surgery. Therefore, the present study provides no data about the success rate of hydrostatic reduction in children with intussusception who are presenting with bloody stools and a sufficiently good general condition.
Success rate indices
In this study, the success rate indices of non-surgical reduction ranged from 73.2 to 95.3 %, depending on the inclusion/exclusion of cases with surgical bowel resection/intervention or inclusion/exclusion of cases who directly underwent surgical reduction without hydrostatic reduction attempts (Table 2). The index definitions of Bekdash et al. [3] are valuable for this purpose. The corrected selective reduction rate (here 95.3 %) is suitable for describing the maximum achievable success in cases that are in principle feasible for non-surgical reduction. The crude reduction rate (here 73.2 %) shows how much can be achieved at minimum without surgery. It also shows that surgery is still required in a relevant fraction [29].
Further study findings
The patients’ age distribution and the observed male predominance were typical for idiopathic ileocolic intussusception in childhood [6, 20, 29]. Most patients (96 %) showed at least one symptom of the classical triad (colicky pain, vomiting, and bloody stool) [1]. However, none showed all three symptoms, probably due to the timely diagnosis in most cases, where the disease had not advanced to bowel necrosis and acute abdomen.
About 80 % of patients presented within 24 h after the onset of symptoms to the hospital. This timely presentation may have several reasons, such as the dense medical infrastructure. In these patients, the success rate of hydrostatic reduction was significantly higher than in the remaining 20 % of patients, who presented 24–48 h after the onset of symptoms (P = 0.016).
About 29 % of patients presented with concomitant gastroenteritis that may have triggered the intussusception. Most patients had enlarged mesenteric lymph nodes >10 mm nearby the ileocecal region, which may have facilitated the intussusception as a hypomochlion. Small amounts of free peritoneal fluid were no contraindication for hydrostatic reduction that was successful in six of eight such cases. Marked amounts of free fluid were found only in patients presenting with markedly reduced general condition, but this fluid did not represent bowel perforation according to surgical findings in this study. All patients showed a thickened terminal ileum after reduction. This may indicate wall edema of the previously intussuscepted bowel and/or preexisting hypertrophic lymphoid tissue in the bowel wall. Technically, successful hydrostatic reductions were finished within 15 min, which may serve for orientation about how long an attempt should be made at least.
Comparison to other studies and reduction methods
Previously, a randomized-controlled trial of Hadidi et al. [14] has reported that fluoroscopy-guided pneumatic reduction (success in 45/50 children, 90 %) is superior to sonography-guided hydrostatic reduction (success in 32/47 children, 68.1 %). In that study, three of the 15 patients with failed hydrostatic reductions required bowel resection [14], resulting in a corrected selective reduction rate of 72.7 % for sonography-guided hydrostatic reduction. Similar to the present study, they applied hydrostatic pressures up to 150 cm H2O (≤110 mmHg), nearly equal to their pneumatic reduction pressures (≤120 mmHg). However, their time needed for hydrostatic reduction was much longer than for pneumatic reduction (only seven reductions were successful within 15 min according to their Fig. 2) and also much longer than in the present study. Interestingly, their success rates at first attempt were similar for pneumatic (30/50 patients) and hydrostatic reduction (28/47 patients), indicating no difference in the easy-to-treat cases. However, final success after the second and third attempt of pneumatic reduction (45/50 patients) was much higher than with hydrostatic reduction (31/47 patients). This may indicate that pneumatic reduction is more successful in the difficult-to-treat cases or that Hadidi et al. [14] were just more experienced with pneumatic reduction [14, 21]. In comparison, in the present study, the success rate of hydrostatic reduction was higher (41/49, 83.7 %), just two of the eight unsuccessful cases had simple surgical reduction, and the corrected selective reduction rate was also higher (95.3 %).
A prospective German multicenter surveillance in 2006–2007 reported the selective reduction rate of sonography-guided hydrostatic reduction as 80.5 % (439/546 patients) while that of radiography-guided pneumatic reduction was 89 % (97/109 patients) [18]. However, the applied reduction pressures were not reported, although higher pressure at pneumatic reduction may be a cause for higher success rates. Also, that study was not randomized. Several studies have shown good success of sonography-guided hydrostatic reduction with selective reduction rates of 75.0−96.0 % and corrected selective reduction rates of 76.0−98.6 % [2, 7, 8, 10, 12, 18, 22, 23, 26–28, 31, 33, 34]. The current study adds to this evidence with detailed consideration of different indices of success [3].
Sonography-guided pneumatic reduction is a further alternative with high reported selective reduction rates of 90.6−95.3 % and corrected selective reduction rates of 92.7−97.6 % [13, 17, 24, 32, 35]. This method could be particularly useful for those who want to replace fluoroscopy-guided pneumatic reduction by radiation-free imaging guidance while keeping the pneumatic technique, potentially also under general anesthesia in apparently non reducible intussusception [11]. It bears a small risk of bowel perforation [13, 35] that also exists in liquid enema reduction [1].
Regarding fluoroscopy-guided pneumatic and hydrostatic reduction, Bekdash et al. [3] have summarized 28 studies and presented corresponding success rate indices. Compared to all 28 studies, the success rate indices of the present study ranged between the median and the upper quartile. Compared to studies using exclusively pneumatic reduction, the success rate indices of the present study were at the median or above. This indicates the potential of sonography-guided hydrostatic reduction as alterative to fluoroscopy-guided pneumatic reduction, at least in patients who present timely within 24 h after onset of symptoms to the hospital.
Non-invasive reduction attempts versus primary surgical reduction
In 73 % of the children (41 patients of group A), surgery was avoided by the hydrostatic reduction. In the other patients, the delay of surgery did not alter the outcome. Therefore, this study adds to the evidence that an attempt of non-invasive reduction is useful in patients who are clinically feasible.
Conclusions
In children with ileocolic intussusception sonography-guided hydrostatic reduction has a good success rate. Particularly in centers that use sonography for diagnosing intussusceptions, this method is a valuable radiation-free alternative to fluoroscopy-guided pneumatic reduction.
References
Applegate KE (2009) Intussusception in children: Evidence-based diagnosis and treatment. Pediatr Radiol 39(Suppl 2):S140–S143
Bai YZ, Qu RB, Wang GD, Zhang KR, Li Y, Huang Y, Zhang ZB, Zhang SC, Zhang HL, Zhou X, Wang WL (2006) Ultrasound-guided hydrostatic reduction of intussusceptions by saline enema: a review of 5218 cases in 17 years. Am J Surg 192(3):273–275
Bekdash B, Marven SS, Sprigg A (2013) Reduction of intussusception: Defining a better index of successful non-operative treatment. Pediatr Radiol 43(6):649–656
Beres AL, Baird R (2013) An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery 154(2):328–334
Betz BW, Hagedorn JE, Guikema JS, Barnes CL (2013) Therapeutic enema for pediatric ileocolic intussusception: using a balloon catheter improves efficacy. Emerg Radiol 20(5):385–391
Chen SC, Wang JD, Hsu HY, Leong MM, Tok TS, Chin YY (2010) Epidemiology of childhood intussusception and determinants of recurrence and operation: Analysis of national health insurance data between 1998 and 2007 in Taiwan. Pediatr Neonatol 51(5):285–291
Choi SO, Park WH, Woo SK (1994) Ultrasound-guided water enema: an alternative method of nonoperative treatment for childhood intussusception. J Pediatr Surg 29(4):498–500
Crystal P, Hertzanu Y, Farber B, Shabshin N, Barki Y (2002) Sonographically guided hydrostatic reduction of intussusception in children. J Clin Ultrasound 30(6):343–348
Desai R, Curns AT, Patel MM, Parashar UD (2012) Trends in intussusception-associated deaths among US infants from 1979–2007. J Pediatr 160(3):456–460
Di Renzo D, Colangelo M, Lauriti G, De Girolamo F, Persico A, Lelli Chiesa P (2012) Ultrasound-guided Hartmann’s solution enema: First-choice procedure for reducing idiopathic intussusception. Radiol Med 117(4):679–689
Diaz-Aldagalan Gonzalez R, Perez-Martinez A, Pison-Chacon J, Ayuso-Gonzalez L, Salcedo-Munoz B, Goni-Orayen C (2012) Rescue by pneumoenema under general anaesthesia of apparently non-reducible intestinal intussusception. Eur J Pediatr 171(1):189–191
Gonzalez-Spinola J, Del Pozo G, Tejedor D, Blanco A (1999) Intussusception: the accuracy of ultrasound-guided saline enema and the usefulness of a delayed attempt at reduction. J Pediatr Surg 34(6):1016–1020
Gu L, Zhu H, Wang S, Han Y, Wu X, Miao H (2000) Sonographic guidance of air enema for intussusception reduction in children. Pediatr Radiol 30(5):339–342
Hadidi AT, El Shal N (1999) Childhood intussusception: a comparative study of nonsurgical management. J Pediatr Surg 34(2):304–307
Hryhorczuk AL, Strouse PJ (2009) Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol 39(10):1075–1079
Hsu WL, Lee HC, Yeung CY, Chan WT, Jiang CB, Sheu JC, Wang NL, Shih SL (2012) Recurrent intussusception: when should surgical intervention be performed? Pediatr Neonatol 53(5):300–303
Ito Y, Kusakawa I, Murata Y, Ukiyama E, Kawase H, Kamagata S, Ueno S, Osamura T, Kubo M, Yoshida M (2012) Japanese guidelines for the management of intussusception in children, 2011. Pediatr Int 54(6):948–958
Jenke AC, Klaassen-Mielke R, Zilbauer M, Heininger U, Trampisch H, Wirth S (2011) Intussusception: Incidence and treatment-insights from the nationwide German surveillance. J Pediatr Gastroenterol Nutr 52(4):446–451
Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM (2013) Childhood intussusception: a literature review. PLoS One 8:e68482
Kaiser AD, Applegate KE, Ladd AP (2007) Current success in the treatment of intussusception in children. Surgery 142(4):469–475
Khanna G, Applegate K (2008) Ultrasound guided intussusception reduction: are we there yet? Abdom Imaging 33(1):38–40
Khong PL, Peh WC, Lam CH, Chan KL, Cheng W, Lam WW, Ai VH, Saing H, Tam PK, Leong LL, Low LC (2000) Ultrasound-guided hydrostatic reduction of childhood intussusception: Technique and demonstration. Radiographics 20(5):E1
Krishnakumar HS, Maheshwari U (2006) Ultrasound guided hydrostatic reduction in the management of intussusception. Indian J Pediatr 73(3):217–220
Lee JH, Choi SH, Jeong YK, Kwon WJ, Jeong AK, Kang BS, Shin SH (2006) Intermittent sonographic guidance in air enemas for reduction of childhood intussusception. J Ultrasound Med 25(9):1125–1130
Menke J (2012) Ileocolic intussusception and hydrostatic reduction in a 2-year-old girl. BMJ Case Rep 2012
Nayak D, Jagdish S (2008) Ultrasound guided hydrostatic reduction of intussusception in children by saline enema: our experience. Indian J Surg 70(1):8–13
Peh WC, Khong PL, Chan KL, Lam C, Cheng W, Lam WW, Mya GH, Saing H, Leong LL, Low LC (1996) Sonographically guided hydrostatic reduction of childhood intussusception using Hartmann’s solution. Am J Roentgenol 167(5):1237–1241
Riebel TW, Nasir R, Weber K (1993) US-guided hydrostatic reduction of intussusception in children. Radiology 188(2):513–516
Samad L, Marven S, El Bashir H, Sutcliffe AG, Cameron JC, Lynn R, Taylor B (2012) Prospective surveillance study of the management of intussusception in UK and Irish infants. Br J Surg 99(3):411–415
Sanchez TR, Potnick A, Graf JL, Abramson LP, Patel CV (2012) Sonographically guided enema for intussusception reduction: a safer alternative to fluoroscopy. J Ultrasound Med 31(10):1505–1508
Shehata S, El Kholi N, Sultan A, El Sahwi E (2000) Hydrostatic reduction of intussusception: Barium, air, or saline? Pediatr Surg Int 16(5–6):380–382
Todani T, Sato Y, Watanabe Y, Toki A, Uemura S, Urushihara N (1990) Air reduction for intussusception in infancy and childhood: Ultrasonographic diagnosis and management without X-ray exposure. Z Kinderchir 45(4):222–226
Wang GD, Liu SJ (1988) Enema reduction of intussusception by hydrostatic pressure under ultrasound guidance: a report of 377 cases. J Pediatr Surg 23(9):814–818
Wood SK, Kim JS, Suh SJ, Paik TW, Choi SO (1992) Childhood intussusception: US-guided hydrostatic reduction. Radiology 182(1):77–80
Yoon CH, Kim HJ, Goo HW (2001) Intussusception in children: US-guided pneumatic reduction–initial experience. Radiology 218(1):85–88
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Jaan Toelen
Rights and permissions
About this article
Cite this article
Menke, J., Kahl, F. Sonography-guided hydrostatic reduction of ileocolic intussusception in children: Analysis of failure and success in consecutive patients presenting timely to the hospital. Eur J Pediatr 174, 307–316 (2015). https://doi.org/10.1007/s00431-014-2394-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-014-2394-3