Abstract
Dense deposit disease (DDD, formerly known as membranoproliferative glomerulonephritis (MPGN) type II) is a subtype of C3 glomerulopathy (C3G). Electron-dense deposits in the glomerular basement membrane characterize this glomerulonephritis. DDD typically presents with a nephritic syndrome that progresses to end-stage renal failure in 50 % of patients despite treatment. The pathogenic basis of DDD is uncontrolled activation of the alternative complement cascade although the potential triggering events that precipitate the development of complement dysregulation are typically unknown. There are isolated reports of an apparent association between streptococcal infection and DDD, as well as with MPGN types I and III. However, this association has not been deemed compelling, perhaps because so few cases have been reported or because of a current lack of evidence for a plausible hypothesis to connect a streptococcal infection with subsequent disease. In this report, we describe two patients with DDD who definitely had an antecedent streptococcal infection with the phenotype of acute post-streptococcal glomerulonephritis and whose initial kidney biopsy findings on light microscopy were indistinguishable from acute post-streptococcal glomerulonephritis. These patients had additional points of interest: recurrence of gross hematuria with recurrent streptococcal infections, slowly progressive course, persistently low serum C3 concentration, positive C3 nephritic factor, and positive risk alleles in the complement factor H (CFH) gene. Conclusion: We suggest that streptococcal infection may trigger DDD in individuals genetically predisposed by virtue of a disorder in complement regulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dense deposit disease (DDD) is a subtype of C3 glomerulopathy characterized by linear, electron-dense deposits in the glomerular basement membrane [2, 5, 6]. The pathogenic basis of DDD is uncontrolled activation of the alternative complement cascade secondary to dysregulation of the C3 convertase [2, 5, 6, 11]. C3 convertase dysregulation can develop as a result of genetic mutations in genes in the alternative complement pathway or secondary to autoantibodies known as C3 nephritic factors (C3Nefs) that stabilize C3 convertase and prevent its breakdown. Most commonly, however, patients with DDD segregate specific alleles of complement genes that increase disease susceptibility [1].
How specific alleles of complement genes contribute to the development of DDD is unknown as they are insufficient themselves to cause disease [11, 18]. Environmental triggers of DDD are poorly documented, although there are reported cases possibly triggered by streptococcal pharyngitis or cellulitis [2, 5, 12]. Even fewer still are cases in which patients present with both a clinical and pathological diagnosis of acute post-streptococcal glomerulonephritis (APSGN) that later evolves into DDD [13, 17]. In this report, we describe two patients who presented with the clinical phenotype of APSGN and whose initial biopsies were consistent with APSGN. However, their atypical course prompted repeat renal biopsies that were diagnostic of DDD. Both patients appear to have nonprogressive disease at least in the short term.
Case reports
Patient 1
A 7-year-old female with a history of recurrent streptococcal throat infections and tonsillectomy at age 4 years was referred for macroscopic hematuria 1 month after being treated for culture-positive group A β-hemolytic streptococcal pharyngitis. At initial presentation and after 9 days of macroscopic hematuria, she had a normal blood pressure of 102/48 mmHg, normal urine output, and no edema. Urinalysis revealed numerous red blood cells and RBC casts by microscopy, 4+ protein, and negative leukocytes and nitrites by dipstick. The serum creatinine concentration was elevated at 1.0 mg/dL (normal range 0.2–0.6 mg/dL) with normal serum electrolyte and albumin concentrations. The antistreptolypsin O (ASO) titer was elevated at 1,240 IU/mL (normal <150 IU/mL), and the serum C3 concentration was low at 39 mg/dL (normal range 87–181 mg/dL); ANA was negative. The patient had no family history of renal disease. She was diagnosed with APSGN and was monitored as an outpatient.
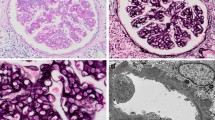
The patient continued to have macroscopic hematuria 3 weeks after initial presentation, although her serum creatinine concentration had improved to 0.7 mg/dL. Her hemoglobin was 10.2 g/dL (normal range 11.5–15.5 g/dL) with a urine protein-to-creatinine ratio of 1.67 (normal <0.2) and serum albumin concentration of 3.9 mg/dL. She had normal blood pressures throughout this time. Due to persistent macroscopic hematuria and proteinuria, a diagnostic renal biopsy was performed. The biopsy revealed subepithelial deposits with diffuse mesangial matrix expansion with segmental solidification. Two of 11 glomeruli also showed crescentic changes (Fig. 1a). Immunofluorescence (IF) was positive for C3 along the peripheral capillary loops and Bowman's capsule (Fig. 1b). Electron microscopy samples contained only medulla. The acute diffuse proliferative glomerulonephritis with few cellular crescents seen on light microscopy was consistent with a post-infectious glomerulonephritis [9].
After her renal biopsy, the patient had improvement in hematuria for 1 week until she developed another streptococcal pharyngitis associated with sore throat, fever, and positive strep culture that again resulted in macroscopic hematuria. Urinalysis revealed numerous RBCs and 2+ protein with RBC and granular casts. The C3 concentration remained low at 50 mg/dL and the C4 was slightly low at 15.8 mg/dL (normal range 16–45 mg/dL); the serum creatinine concentration had improved to 0.6 mg/dL. Although the macroscopic hematuria resolved within a week of initiation of amoxicillin for recurrent strep pharyngitis, the low C3 (22 mg/dL) and 2+ proteinuria persisted for 6 months. Therefore, a repeat renal biopsy was done and she was started on an angiotensin II receptor blocker. The repeat renal biopsy revealed minimally increased mesangial cellularity with no crescents on light microscopy (Fig. 2a). There was positive C3 immunofluorescence staining in the tubular basement membranes with weak staining in the glomerular capillary loops and negative IF staining for IgM and IgG (Fig. 2b). Ultrastructural studies revealed ribbon-like discontinuous electron-dense material in the basement membrane lamina densa consistent with DDD and C3 glomerulopathy (Fig. 2c). A complete complement profile revealed low serum C3 concentration at 21 mg/dL (normal 71–150 mg/dL) but normal C4 at 19.6 mg/dL, normal factor H at 51.7 mg/dL (normal 37–68 mg/dL), and normal factor I at 4.2 mg/dL (normal 2.4–4.9 mg/dL). C3 nephritic factor was positive at 704 U/mL (normal <5 U/mL).
Patient 1's follow-up kidney needle core biopsy. a A representative glomerulus is normal in size and shows only minimally increased cellularity (×400). b C3 immunofluorescent staining of tubular basement membranes with weak glomerular staining (×400). c Electron microscopy shows discontinuous, ribbon-like, electron-dense material (asterisk) in the lamina densa of capillary basement membranes
An oral course of prednisone at 2 mg/kg/day was given for 4 weeks, after which urinalysis revealed no blood or protein, and she was switched to every-other-day prednisone with a prolonged prednisone taper. She remained in remission with persistently low serum C3 concentrations ranging from 22 to 50 mg/dL. There were no macular drusen or features of partial lipodystrophy. Prednisone was discontinued after 16 months with normal renal function, normal blood pressure, and no proteinuria. She continues to be monitored as an outpatient with a diagnosis of DDD without progression 5 years after presentation. Her last visit revealed normal creatinine and blood pressure, with 2+ proteinuria and improving protein-to-Cr ratio but persistently low serum C3 concentration of 37 mg/dL, and she continues on losartan and amoxicillin prophylaxis for renal protection.
Genetic evaluation was performed to evaluate for possible etiology of the DDD. She had no disease-causing variants in CFH, CFI, MCP, and C3, and no deletion or duplication of the following genes was detected: CFH, CFHR3, CFHR1, CFHR4, CFHR2, and CFHR5. However, she had four copies of CFH DDD/C3 glomerulonephritis (C3GN)-associated risk alleles, including two copies of the single nucleotide polymorphism Val62 and two copies of the single nucleotide polymorphism His402, both in the CFH gene. Studies show that having two or more risk variants in the CFH gene increases the odds ratio of developing disease [1].
Patient 2
A 6-year-old female with an uneventful past medical history presented with upper respiratory tract (URT) symptoms and tea-colored urine. Rapid strep antigen was positive and urinalysis revealed proteinuria and RBC casts. She had a normal ASO of 106 IU/mL but an elevated DNase B antibody titer of 290 U/mL (normal range 0–70 U/mL). Urine protein-to-creatinine ratio was elevated at 4.0. Serum C3 concentration was low at 8 mg/dL and serum C4 concentration was normal at 22.7 mg/dL. She was diagnosed with APSGN and was treated with amoxicillin for 10 days. A week after completing the antibiotics, the patient had a recurrence of URT symptoms and tea-colored urine. A rapid streptococcal test was again positive, and she was started on amoxicillin clavulanate. Two days later, she developed emesis and diarrhea and was admitted for dehydration. On admission, the patient had 3+ proteinuria and large blood on urinalysis, but her creatinine (0.4 mg/dL) and blood pressures remained normal and she had no edema or hypertension.
Macroscopic hematuria resolved one and a half months after her initial presentation, but she was found to have +RBCs and 2+ proteinuria on follow-up urinalysis and a persistently low serum C3 concentration of 7 mg/dL. A diagnostic renal biopsy revealed light microscopic features suggestive of a proliferative post-infectious glomerulonephritis, with minimal mesangial hypercellularity and no thickening of the glomerular basement membranes (Fig. 3a). The mesangium and glomerular capillary loops were positive for C3 in a ribbon-like and coarsely granular pattern (Fig. 3b). Immunofluorescence was negative for IgA and IgG but was positive for IgM especially in the mesangium and capillary loops. Ultrastructural studies revealed numerous ribbon-like dense deposits within the mesangium and glomerular capillary loops consistent with DDD and C3 glomerulopathy (Fig. 3c). Occasional subepithelial deposits were also noted. The patient was started on lisinopril for renal protection. Factor H was low normal at 188 μg/mL (normal range 160–412 μg/mL), and C3 nephritic factor was presumptively positive at 3.61 (normal <0.5). A year after initial presentation, the patient had an episode of macroscopic hematuria and proteinuria with a recurrent streptococcal infection. Renal function remained normal with normal blood pressure and normal serum creatinine. Repeat complement evaluation 8 months after presentation showed persistently low C3 at 0.6 mg/dL and low C4 at 9 mg/dL, which is atypical for DDD but has been seen in isolated cases [10, 14]. The patient was monitored closely as an outpatient and continued to have 1+ proteinuria and trace blood on urinalysis although serum creatinine concentration and blood pressure remain normal. She was continued on a regimen of lisinopril 5 mg daily and amoxicillin prophylaxis. Two and a half years after presentation, the patient has now developed nephrotic syndrome with protein-to-Cr ratio of 10,621 mg/g Cr (normal 21–161 mg/g Cr), hypoalbuminemia 1.7 g/dL (normal 3.7–5.6 g/dL), edema, and hypercholesterolemia 258 mg/dL (high >200 mg/dL). She has been started on prednisolone 30 mg twice daily, has continued lisinopril 5 mg daily and amoxicillin 250 mg daily, and was started on iron supplementation. At this time, her creatinine remains normal at 0.5 mg/dL and C3 remains low at <15 mg/dL.
Patient 2's kidney needle core biopsy. a A representative glomerulus shows minimal mesangial widening and hypercellularity. Note the presence of polymorphonuclear leukocytes within the glomerular capillaries (×600). b C3 immunofluorescence labels mesangium and capillary loop in a coarse granular (asterisk) and ribbon-like (square) pattern (×400). c Electron microscopy reveals the presence of electron-dense deposits within the mesangium (asterisk) and glomerular peripheral capillary loops (square) in a ribbon-like, discontinuous fashion
Genetic evaluation revealed risk variants in the CFH gene. She was found to have two copies of the single nucleotide polymorphism Val62 in the CFH gene. The rest of her genetic workup was normal.
Discussion
Both patients presented with clinical and histopathological features of APSGN including macroscopic hematuria with RBC casts, a positive ASO titer or anti-DNase B titers, low serum C3 concentrations, and light microscopic findings consistent with APSGN [9]. Due to persistently low C3 concentrations as well as persistent proteinuria and hematuria, they underwent renal biopsies that revealed findings consistent with DDD including ribbon-like dense deposits within the mesangium and glomerular capillary loops and positive C3 staining in the mesangium and capillary loops [6, 8, 14, 16]. Both patients were also positive for C3Nefs, which are strongly associated with DDD [2, 3, 5]. Further genetic workup to evaluate their atypical course revealed positive risk variants in the complement CFH gene. Having two or more of these risk variants increases the odds ratio of developing DDD [1, 14]. Mutations and polymorphisms in the CFH gene are associated with dysregulation of the complement alternative pathway and have been found to be associated with both DDD and atypical hemolytic uremic syndrome. In a study that examined complement dysregulation and DDD, 50 % of patients with mutations in the CFH gene also had C3Nefs that likely placed them at increased risk for DDD similar to our patients [14]. However, having C3Nefs and/or genetic mutations is not sufficient to cause DDD, and reports have shown that family members of patients with DDD who carry the same genetic mutations and/or C3Nefs do not develop renal disease [20]. It is possible that the DDD or C3G may develop in patients with genetic predisposition who then have an environmental trigger such as a streptococcal infection to initiate the uncontrolled activation of the alternative complement pathway.
There are several possible explanations for the clinical course in these patients. It is possible that the two disease processes were independent, and they had presymptomatic DDD until they presented with APSGN. Neither patient had previous urinalyses nor complement measurements to infer that there was no evidence of renal disease or hypocomplementemia prior to their initial presentation. It is also possible that both patients were incorrectly diagnosed with APSGN and were presenting with an early disease that had not yet developed the complete histological features of established DDD [2]. Unfortunately, in the first patient, there were no glomeruli in the electron microscopy portion of the original biopsy, so it is possible that she had evidence of DDD at that time. However, it seems more plausible that the APSGN triggered DDD in two previously healthy but genetically predisposed children. As precedence, streptococci infections are known to trigger C3 glomerulonephritis (C3GN), another subtype of C3 glomerulopathy [15].
There have been multiple case studies assessing a possible etiology for how streptococcal infection can trigger the development of DDD or C3 glomerulopathy. One plausible explanation for the development of DDD after streptococcal infection is the persistent deposition in the renal glomeruli of a nephritis-associated plasmin receptor (NAPlr), a nephritogenic antigen found in Streptococcus [12, 18, 19]. This antigen activates the alternative complement pathway with in vivo activation of C3 [18]. In one patient who presented with DDD after streptococcal infection, late biopsies were positive for NAPlr months after initial presentation [18]. Similarly, a 12-year-old boy who presented with persistent hypocomplementemia, proteinuria, and macroscopic hematuria after a streptococcal infection was found to have renal biopsy findings consistent with DDD [13]. His kidney biopsy was positive for NAPlr more than 8 weeks later. Another proposed streptococcal antigen that may trigger immune activation is streptococcal pyrogenic exotoxin B (SpeB), a cationic cysteine proteinase secreted by streptococci. One study found deposition of SpeB in 12/17 biopsies of patients with acute post-streptococcal glomerulonephritis and co-localized with NaPlr in one patient [4]. Less data exists for prolonged deposition of SpeB in patients with DDD or C3G, but more research is needed. The prolonged deposition of streptococcal antigens such as NAPlr or SpeB may have triggered DDD in our genetically susceptible patients.
Our two patients and the previously reported patients offer evidence of a streptococcal etiology of DDD/C3G as they presented initially with APSGN, which persisted with a prolonged course of low serum C3 concentrations and repeated episodes of glomerulonephritis. Both of our patients were found on later biopsies to have changes consistent with DDD possibly due to continued glomeruli deposition of antigen-activating C3. In these genetically susceptible individuals, the infection may have triggered uncontrolled activation of the alternative complement pathway resulting in DDD. Alternatively, the streptococcal infection may have triggered development of autoantibodies that stabilize the C3 convertase, as has been reported in three patients with acute post-streptococcal glomerulonephritis associated with the presence of C3Nefs [7]. However, these patients differ from ours in that the C3Nef activity was transient and undetectable 1–4 months after presentation, by which time C3 levels had normalized. The relationship between the C3Nefs and the DDD-associated haplotypes remains unknown. It is possible that without this exposure to group A Streptococcus, the patients we report would not have developed renal disease or would have developed it at a much later date.
Vernon and colleagues describe an informative patient similar to ours who developed C3 glomerulopathy after streptococcal infection [20]. In aggregate, these three patients suggest that this sequence may occur in genetically susceptible patients. Vernon's patient presented with persistent hypocomplementemia with low serum C3, persistent hematuria, and proteinuria after streptococcal infection. A renal biopsy 20 months after presentation showed intramembranous electron-dense deposits and some mesangial deposits consistent with C3G with a membranoproliferative pattern of glomerulonephritis. Further investigation found a heterozygous mutation in the gene encoding complement factor H-related protein 5 (CFHR5). In contrast to our patients, she was negative for C3Nefs and all other genetic evaluations were normal. She was asymptomatic prior to this streptococcal infection but developed recurrence of her gross hematuria and proteinuria after a recurrent infection. Her sister and mother had the same heterozygous mutation but no evidence of low serum C3 concentration or renal disease; this enhances the likelihood, as in our patients, that the streptococcal infection was the trigger for the patient's DDD.
It is important to note that both of our patients and the patients in similar case reports appear to have slowly progressive DDD. There is no disease-specific treatment for DDD, and about 50 % of patients develop end-stage renal disease within 10 years of diagnosis, and most patient who receive transplants develop recurrent disease in their allografts [2, 3, 5]. The early course in our patients was not progressive. Patient 1 appeared to respond to corticosteroid treatment and shows no progression of renal disease 3 years from initial presentation with no hypertension, nephrotic syndrome, or renal insufficiency despite persistently low serum C3 concentrations. Patient 1 remains on amoxicillin prophylaxis and losartan to prevent repeated injury to her kidney. Patient 2 initially had improvement in proteinuria after initiation of an ACE inhibitor but did develop recurrence of gross hematuria with subsequent streptococci infections. Patient 2 has now progressed to nephrotic syndrome although has normal serum creatinine at this time. We will continue to follow her closely; however, her initial course was still slowly progressive compared to most dense deposit disease which is associated with nephrotic range proteinuria and progressive renal disease unresponsive to treatment early in diagnosis.
Interestingly, in all cited case reports of patients developing DDD after streptococcal infection, symptoms have resolved with minimal treatment [13, 18, 20]. None of these patients progressed to ESRD or developed further kidney damage despite persistently low serum C3 concentrations. The implications of the persistently low C3 are difficult to interpret. It is possible that these patients may have minimal clinical disease (“silent phase” of nephritis/nephrotic syndrome) and that their kidney function may slowly deteriorate over the long term. Alternatively, these patients may offer insight into the subset of patients with DDD who do not progress to end-stage renal failure, easily achieve clinical remission, or have a more slowly progressive course. Our patients remain on ACE inhibitor/angiotensin II receptor antagonist to prevent possible progression of disease and amoxicillin prophylaxis to prevent recurrent damage. Patient 1 remains minimally symptomatic with only microscopic hematuria and hypocomplementemia as evidence of her disease. Unfortunately, patient 2 has now progressed to nephrotic syndrome despite amoxicillin prophylaxis and lisinopril but has been restarted on prednisone 30 mg twice daily to try and treat her current symptoms.
Identifying underlying triggers driving the development of complement dysregulation in patients with DDD may be important in developing disease-specific therapies [11]. Our cases illustrate a potential trigger, but further research is required to validate the importance and significance of our observations.
References
Abrera-Abeleda MA, Nishimura C, Smith J, Sethi S, McRae J, Murphy B, Silvestri G, Skerka C, Jozsi M, Zipfel P, Hageman G, Smith R (2006) Variations in the complement regulatory genes factor H (CFH) and factor H related 5 (CFHR5) are associated with membranoproliferative glomerulonephritis type II (dense deposit disease). J Med Genet 43(7):582–589
Alchi B, Jayne D (2010) Membranoproliferative glomerulonephritis. Pediatr Nephrol 25:1409–1418
Appel G, Cook H, Hagerman G, Jennette J, Kashgarian M, Kirschfink M, Lambris J, Lanning L, Lutz H, Meri S, Rose N, Salant D, Sethi S, Smith R, Smoyer W, Tully H, Tully S, Walker P, Welsh M, Wurzner R, Zipfel P (2005) Membranoproliferative glomerulonephritis type II (dense deposit disease): an update. Am Soc Nephrol 16:1392–1403
Batsford S, Mezzano S, Mihatsch M, Schiltz E, Rodriguez-Iturbe B (2005) Is the nephritogenic antigen in post-streptococcal glomerulonephritis pyrogenic exotoxin B (SPE B) or GAPDH? Kidney Int 68:1120–1129
Cansick J, Lennon R, Cummins C, Howie A, McGraw M, Saleem M, Tizard E, Hulton S, Milford D, Taylor C (2004) Prognosis, treatment and outcome of childhood mesangiocapillary (membranoproliferative) glomerulonephritis. Nephrol Dial Transplant 19:2769–2777
D'Agati V, Bomback A (2012) C3 glomerulopathy: what’s in a name? Kidney Int 82:379–381
Fremeaux-Bacchi V, Weiss L, Demouchy C, May A, Palomera S, Kazatchkine M (1994) Hypocomplementaemia of poststreptococcal acute glomerulonephritis is associated with C3 nephritic factor (C3NeF) IgG autoantibody activity. Nephrol Dial Transplant 9(12):1747–1750
Kambham N (2012) Postinfectious glomerulonephritis. Adv Anat Pathol 19(5):338–347
Kasahara T, Hayakawa H, Okubo S, Okugawa T, Kabuki N, Tomizawa S, Uchiyama M (2001) Prognosis of acute poststreptococcal glomerulonephritis (APSGN) is excellent in children, when adequately diagnosed. Pediatr Int 43:364–367
Kerns E, Rozansky D, Troxell ML (2013) Evolution of immunoglobulin deposition in C3-dominant membranoproliferative glomerulopathy. Pediatr Nephrol 28(11):2227–2231
Licht C, Fremeaux-Bacchi V (2009) Hereditary and acquired complement dysregulation in membranoproliferative glomerulonephritis. Thromb Haemost 2:271–278
Rodriguez-Iturbe B, Batsford S (2007) Pathogenesis of poststreptococcal glomerulonephritis a century after Clemens von Pirquet. Kidney Int 71:1094–1104
Sawanobori E, Umino A, Kanai H, Matsushita K, Iwasa S, Kitamura H, Oda T, Yoshizawa N, Sugita K, Higashida K (2009) A prolonged course of Group A streptococcus-associated nephritis: a mild case of dense deposit disease (DDD)? Clin Nephrol 6:703–707
Servais A, Noël LH, Roumenina LT, Le Quintrec M, Ngo S, Dragon-Durey M, Macher M, Zuber J, Karras A, Provot F, Moulin B, Grunfeld J, Niaudet P, Lesavre P, Fremeaux-Bacchi V (2012) Acquired and genetic complement abnormalities play a critical role in dense deposit disease and other C3 glomerulopathies. Kidney Int 82(4):454–464
Sethi S, Fervenza FC, Zhang Y, Zand L, Meyer NC, Borsa N, Nasr SH, Smith RJH (2013) Atypical post-infectious glomerulonephritis is associated with abnormalities in the alternative pathway of complement. Kidney Int 83(2):293–299
Sethi S, Nester CM, Smith RJ (2012) Membranoproliferative glomerulonephritis and C3 glomerulopathy: resolving the confusion. Kidney Int 81:434–441
Shahidi-Asl M, Ananth M, Boineau F, Meleg-Smith S (2000) Apparent progression of acute glomerulonephritis to dense deposit disease. Ultrastruct Pathol 24:273–277
Suga K, Kondo S, Matsuura S, Kinoshita Y, Kitano E, Hatanaka M, Kitamura H, Hidaka Y, Oda T, Kagami S (2010) A case of dense deposit disease associated with a group A streptococcal infection without the involvement of C3NeF or complement factor H deficiency. Pediatr Nephrol 25:1547–1550
Uchida T, Oda T, Watanabe A, Izumi T, Higashi K, Kushiyama T, Miura S, Kumagai H (2011) Clinical and histologic resolution of poststreptococcal glomerulonephritis with large subendothelial deposits and kidney failure. Am J Kidney Dis 58:113–117
Vernon K, Goicoechea de Jorge E, Hall A, Fremeaux-Bacchi V, Aitman T, Cook H, Hangartner R, Koziell A, Pickering M (2012) Acute presentation and persistent glomerulonephritis following streptococcal infection in a patient with heterozygous complement factor H-related protein 5 deficiency. Am J Kidney Dis 60(1):121–125
Conflict of interest
We certify that we have nothing to disclose. There is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prasto, J., Kaplan, B.S., Russo, P. et al. Streptococcal infection as possible trigger for dense deposit disease (C3 glomerulopathy). Eur J Pediatr 173, 767–772 (2014). https://doi.org/10.1007/s00431-013-2245-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-013-2245-7