Abstract
Paracetamol (acetaminophen) is one of the most popular and widely used drugs for the treatment of pain and fever in children. This drug has multiple mechanisms of action, but its pharmacodynamic is still not well known. The central nervous system is the main site of action and it mirrors the paracetamol effect compartment. The recommended dosages and routes of administration should be different whether paracetamol is used for the treatment of pain or fever. For example, the rectal route, while being efficacious for the treatment of fever, should be avoided in pain management. Paracetamol is a safe drug, but some clinical conditions and concomitant drugs, which are frequent in clinical practice, may increase the risk of paracetamol toxicity. Therefore, it is important to optimize its administration to avoid overdoses and maximize its effect. The principal mediator of the paracetamol toxicity is the N-acetyl-p-benzo-quinone imine (NAPQI), a toxic product of the paracetamol metabolism, which could bind cysteine groups on proteins forming paracetamol–protein adduct in the liver. Conclusion: Although frequently prescribed, the concept of “effect compartment concentration” and the possible co-factors that could cause toxicity at recommended doses are not familiar to all pediatricians and general practitioners. We reviewed the literature concerning paracetamol mechanisms of action, we highlighted some relevant pharmacodynamic concepts for clinical practice, and we summarized the possible risk factors for toxicity at therapeutic dosages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paracetamol (acetaminophen) is the most popular analgesic and antipyretic drug for the treatment of pain and fever in children. It represents the drug of choice for the management of mild to moderate pain and, according to NICE guidelines, for the management of the children with fever who appear distressed [112].
Increased paracetamol prescription followed an association noted between Reye’s syndrome and aspirin [29].
The mechanisms by which paracetamol achieves its effects on pain are still debated. Paracetamol is generally considered to be safe and effective in recommended doses, even if concerns have arisen over the past decade as paracetamol has been increasingly recognized as a major cause of acute liver failure in adults in the United States [62].
While paracetamol is an important cause of acute liver failure in children, it plays a relatively small role in the etiology of acute liver failure from a global standpoint [107]. A recent report showed that a significant number of adults develop elevations in hepatic transaminase levels while receiving recommended doses of paracetamol in a controlled research setting [117].
Elements of pharmacokinetics: how is paracetamol absorbed and metabolized?
Absorption
Paracetamol has a pK a of 9.5, and, in the alkaline medium of duodenum, is largely non-ionised and consequently absorbed primarily by passive non-ionic diffusion [13]. Absorption within the stomach is minimal, and the limiting step for absorption is gastric empting into the duodenum [40]. Absorption may be altered by formulation. Bioavailability for the oral route is estimated at 63–89 % [16, 105]. Tablets and capsules must disintegrate and then dissolute, introducing a lag time before duodenal uptake. Paracetamol effervescent tablets [100] and liquid paracetamol (elixir, drops, syrup) [16] are absorbed significantly faster. The time to peak concentration is approximately 45 to 60 min after oral administration of regular release tablets and there may be large variation in individual plasma paracetamol concentrations measured 60 min after oral administration [16]. Liquid paracetamol has a time to peak of about 30 min [16].
The absorption from the rectal route is considered the most erratic and unpredictable, with reported values of bioavailability ranging from 24 % to 98 % [32, 105]. For the rectal route, the time to peak plasma concentration ranges from 107 to 288 min after rectal administration [32].
Age also has an impact on paracetamol absorption. Because of slower gastric empting, oral absorption in neonates is delayed [5]. Normal adult rates may not be reached until 6–8 months of age [41].
The IV route of administration shows consistently earlier and higher peak plasma or cerebrospinal fluid (CSF) concentration than oral or rectal routes [105].
Distribution
The binding of paracetamol to plasma proteins is low (10–25 %) [28], while it is widely distributed, with a volume of distribution of 0.8–1 l/kg [95].
Because of differences in body composition (e.g., higher body water content) and because of the fact that paracetamol is a water-soluble compound, the distribution volume is higher in the newborn: the peripheral volume of distribution decreases from 27 weeks postmenstrual age (45.0 l × 70 kg−1) to reach 110 % of its mature value by 6 months of age [10]. Paracetamol has been shown to be able to penetrate into the CSF. It is also able to penetrate in the placenta and is excreted in breast milk at low levels [14, 15, 61]. The estimated maximum dose to the neonate through breast milk was 1.85 % of the weight-adjusted maternal oral dose of paracetamol (1.0 g) [80].
The concept of effect compartment concentration
Time delays between paracetamol concentrations and analgesic effect have been reported in adult volunteers [12, 79] and children [11]. Moreover, several studies have documented a time delay of 1–2 h between maximum plasma concentration and maximum temperature reduction (Fig. 1) [40, 54, 119].
Time–concentration profile for a child given paracetamol elixir. A concentration of 10 mg/l is reached both before (during the absorption phase) and after (elimination phase) maximum concentration. There is a delay between maximum concentration and peak effect of about 1 h. (Data from Gibb and Anderson [40])
These time delays mean that there is not a direct relationship between concentration and effect. Paracetamol must move from the plasma to an effect compartment where exerts its pharmacological action [40] and the CSF compartment mirrors the paracetamol effect compartment.
There is an important difference in the required effect compartment concentrations for analgesia and fever reduction. A minimum target effect compartment concentration of 10 mg/l is required for pain relief in children (Fig. 2) [11] and recently confirmed also in neonates [4]. The minimum target effect compartment concentration for antipyresis is 5 mg/l (Fig. 3) [40]. The effect compartment concentration of 10 mg/l is obtainable both with i.v. [10] and oral routes [40]; at standard doses, the rectal route can provide an effect compartment concentration of 5 mg/l [40]. To obtain a higher effect, compartment concentration with rectal route should require much higher and not safe doses.
Effect compartment concentration–analgesic response relationship for paracetamol in children after tonsillectomy. Small concentration increases have maximal effect up to effect compartment concentration of 10 mg/l. Further increasing concentration has minimal effect on pain score. A VAS pain score (0–10) measured effectiveness. (Data from Anderson et al. [11])
Effect compartment concentration–response relationship for paracetamol antipyresis. The temperature reduction is expressed in Fahrenheit (F). (From Anderson [8])
The clinical relevance of these concepts is that the needed outcome (analgesia or antipyresis) must drive the route of administration (e.g., rectal route is not appropriate for pain management). The choice of the interval of the drug administration could be also driven by the evidence of the time delay between maximum plasma concentration and maximum effect [40]. Therefore, if needed, the anticipation of the dose administration can allow an efficacious and steady concentration in the effect compartment, with a minimum interval of administration of 4 h.
Metabolism and elimination
In adults, paracetamol is metabolized mainly in the liver by glucuronidation (50–60 %), sulfation (25–30 %), and oxidation (<10 %) [84, 93]. Additionally, hydroxylation to form 3-hydroxyparacetamol and methoxylation to form 3-methoxyparacetamol, along with excretion of free or unconjugated paracetamol in the urine, represent minor clearance pathways [73]. Paracetamol is subject to a first pass hepatic metabolism, which justifies the variability of absorption between patients [16] and between different ages [5].
None of the metabolites of paracetamol has analgesic or antipyretic effects. All of the metabolites are excreted in the urine in a dose-dependent manner, with more than 90 % of an administered dose excreted within 24 h. Enterohepatic circulation is negligible [53]. The renal elimination capacity is reflected by diuresis, glomerular filtration rate and renal tubular activity. The extensive variability in early infancy relates to maturation (e.g., age, birthweight) and disease characteristics (e.g., peripartal asphyxia, renal congenital malformations) [5].
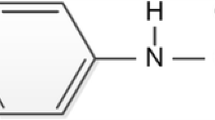
Oxidation of paracetamol occurs via a CYP450-dependent, mixed-function oxidase enzyme pathway, primarily by CYP2E1 and CYP3A4, to form N-acetyl-p-benzo-quinone imine (NAPQI) [66]. NAPQI is near-instantaneously conjugated with intracellular glutathione to 3-glutathione-S-yl-paracetamol by reacting with either intracellular glutathione directly or through a glutathione-transferase-catalyzed reaction [33]. NAPQI may cause hepatotoxicity after a massive acute overdose if glutathione stores are exhausted. With therapeutic doses of paracetamol, sufficient glutathione stores are present to conjugate the small amount of NAPQI produced. Additionally, there is an active repletion process for glutathione [63].
In children, paracetamol metabolism pathways are the same as in adults, but the relative contribution of each pathway or enzyme to the overall paracetamol metabolism changes with age.
The sulfation pathway is mature at birth; however, the glucuronidation pathway takes about 2 years to mature [114]. As the glucuronidation activity in younger children is less than that seen in older children and adults, the sulfation pathway is a more important route of metabolism for paracetamol in younger children [72]. Even if the rate of excretion of various paracetamol metabolites changes with age, the plasma half-life of paracetamol is similar across different age groups [72].
CYP2E1 levels are low in neonates, and gradually increase during the first year to reach the adult value in children aged 1–10 years [115].
However, in neonates, metabolic clearance of paracetamol through sulfation matures more rapidly than glucuronidation which is still poor. This results in lower clearance and slower decrease after the peak paracetamol concentration has been reached. Because of this lower clearance, accumulation is more likely [5].
The development of hepatotoxicity caused by paracetamol is dependent on the balance of the formation rate of NAPQI, the elimination rate from sulfation and glucuronidation conjugation pathways, and the initial content and repletion rate of hepatic glutathione [83].
Young children appear to be most resistant to paracetamol-induced hepatotoxicity because of both reduced rates of oxidation by CYP2E1 and the neonate’s increased ability to replete glutathione compared with adults [91].
Elements of pharmacodynamics: how does paracetamol act?
It has been assumed that paracetamol mainly acts through the cyclooxygenase (COX) pathway. Its action appears to be mostly central; it readily passes the blood–brain barrier [30, 61] and inhibits prostaglandin synthesis in the brain [9, 39]. The inhibition of the prostaglandin synthesis in the brain leads to temperature reduction probably modifying hypothalamic temperature set-point [39].
Paracetamol does not have significant anti-inflammatory activity nor does inhibit production of the pro-clotting trombaxane 2 (TXA2). Paracetamol does not appear to have a major effect peripherally, which explains both its favorable lack of several adverse effects associated with NSAIDs, such as stomach ulcers, impaired hemostasis, reduced renal flow and the absence of anti-inflammatory (positive) effects in the settings of inflammation (e.g., arthritis).
The mechanism of action of paracetamol analgesia is multifactorial. Inhibition of prostaglandin synthesis in the brain plays a major role, but alternative mechanisms of action are proposed:
-
Central serotonergic mechanism: paracetamol could activate the serotonergic inhibitory descending pain pathways with analgesic effect [90].
-
Effect on cannabinoid (CB) receptors: two research groups [48, 82] have demonstrated an active metabolite of paracetamol (the fatty acid amide N-arachidonoylphenolamine) that shares the ability of CBs to display analgesic activity and to lower body temperature [19, 42].
-
Inhibitory action on spinal l-arginine–nitric oxide (NO) pathway: depolarization of afferent neurons by peripheral harmful stimuli leads to activation of spinal N-methyl-d-aspartate (NMDA) receptors. Rodent studies suggest that these, in turn, promote the synthesis of NO (a neurotransmitter at a spinal level conveying nociceptive information) [49, 70]. Nonsteroidal anti-inflammatory drugs (NSAIDs) and paracetamol interfere with nociception associated with spinal NMDA receptor activation. This effect may involve an inhibitory action on spinal NO mechanisms [20].
Elements of pharmacodynamics: side effects
Paracetamol is usually well tolerated at recommended therapeutic doses. Rash and other allergic reactions occur occasionally. The rash usually is erythematous or urticarial, but sometimes it is more serious and may be accompanied by drug fever and mucosal lesions [58]. The use of paracetamol has been associated anecdotally with neutropenia, thrombocytopenia, and pancytopenia [37, 121]. Hypotension, flushing, and tachycardia are also reported on infusion [21].
Several observational studies have reported associations between paracetamol use in children and asthma, some epidemiological evidence links paracetamol exposure in pregnancy and childhood with asthma [45]. The underlying biological mechanisms are not clear. The paracetamol use might influence asthma pathogenesis through depletion of glutathione, a major antioxidant in the airways [104]. This might influence asthma in two ways. The toxic metabolite NAPQI may increase oxidative stress causing epithelial damage and increased airway inflammation [45]. In vitro, the equivalent of therapeutic doses of paracetamol can reduce intracellular concentrations of GSH in human alveolar macrophages which, in antigen presenting cells, leads to preferential Th2 cytokine responses [89]. Another possibility is that acetaminophen causes airways epithelial damage through its actions as a selective cyclooxygenase-2 (COX-2) inhibitor, since it has been proposed that COX-2 plays an important role in repair of damaged airway epithelium [116]. Recently, a novel mechanism has been proposed. A study in mice showed that the equivalent of therapeutic doses of acetaminophen produced detectable concentrations of NAPQI in the lung. NAPQI in turn, stimulated the transient receptor potential ankyrin-1 (TPRA1) which caused neurogenic airway inflammation [78]. Finally, about the mechanisms operating prenatally, Henderson and Shaheen [45] speculated that acetaminophen crosses the placenta and the foetus is capable of generating NAPQI in late gestation. Future research should be directed towards establishing robust experimental evidence of the association between paracetamol and asthma, including the size of the effect and the estimated population-attributable benefit arising from interventions to modify paracetamol use in different groups [45].
Elements of pharmacodynamics: toxicity
The toxicity of paracetamol is closely linked to its metabolism. With therapeutic dosing, paracetamol is predominantly metabolized by glucuronidation and sulfation. Approximately 5 % to 10 % of the drug is oxidized by CYP450-dependent pathways to NAPQI. NAPQI is detoxified by glutathione and eliminated in the urine or bile. The NAPQI that is not detoxified may bind cysteine groups on proteins forming paracetamol–protein adducts in the liver [51]. High levels of adducts correspond to liver toxicity in patients with paracetamol-related acute liver failure [51]. Probably the NAPQI causes damage through binding mitochondrial proteins. This binding leads to decreased mitochondrial respiration, increased oxidative stress, and then to hepatic cellular necrosis [68]. Reports of liver toxicity in pediatric patients have suggested that a minimal, single paracetamol dose of 120–150 mg/kg (the normal dosage is 20 mg/kg) of body weight may be associated with hepatotoxicity [2, 46].
Hepatotoxicity after therapeutic dosing of paracetamol in children is rarely reported in defined-population studies. Case reports suggest that this phenomenon may occur, but few reports contain sufficient data to support a probable causal relationship [64]. Other reported cases of severe hepatotoxicity in children have been attributed to cumulative toxicity from repeated doses rather than acute intoxication from a single massive overdose [98]. Reports of hepatotoxicity in association with dosages reported to be in therapeutic range [47, 65] may represent inaccurate memory of administered doses or a narrower paracetamol therapeutic window because of associated conditions (Tables 1 and 2). Theoretically, not only an inherited but also an acquired higher activity of CYP2E1 could increase conversion of paracetamol to NAPQI [111] (Table 1). In fact, children with a family history of hepatic toxicity to paracetamol have an increased risk to develop a toxic reaction [7].
The kidney is the second target organ of paracetamol toxicity: renal dysfunction occurs in about 25 % of cases with significant hepatotoxicity and in more than 50 % of those with hepatic failure [94]. However, renal impairment after acute paracetamol overdose may also occur in the absence of hepatotoxicity [23].
Renal dysfunction after acute paracetamol overdose is the result of the local formation of NAPQI, that causes tubular necrosis [94]. However, several other nephrotoxic mechanisms have been proposed [35], because acute renal failure has been reported despite adequate treatment with N-acetylcysteine (NAC) [35]. Renal damage is also produced by chronic use of paracetamol, it has been showed a dose-dependent relationship between heavier paracetamol use and an increased risk of end-stage renal disease [87].
Conditions, situations and concomitant drugs that may increase the risk of paracetamol toxicity with therapeutic dosing
Since the NAPQI formation rate is related to acetaminophen toxicity, some situations, conditions (Table 1) or drugs (Table 2) could lead to increased risk of paracetamol toxicity by increasing formation of NAPQI or reducing glutathione stores.
Fasting is associated with increased paracetamol hepatotoxicity in humans [118] and animals [71] apparently because of increased metabolism to NAPQI [22, 97]. Protein-caloric malnutrition [123], obesity [81] and poorly controlled diabetes [106] are associated with increased activity of CYP2E1 that may increase formation of NAPQI (Table 1).
Detoxification may be reduced in patients with chronic protein-caloric malnutrition, who also have low glutathione levels [101].
Numerous drugs (Table 2) may affect paracetamol elimination or NAPQI detoxification and some of their effects on CYP2E1 activity are variable. Isoniazid first inhibits then enhances NAPQI formation as it is cleared [26, 75, 99]. Ethanol ingested chronically increases CYP2E1 activity and depletes glutathione, which enhances susceptibility to paracetamol toxicity [7, 75], whereas acute ethanol ingestion reduces paracetamol toxicity through competitive inhibition of CYP2E1 [6, 99].
Concurrent treatment with one or more of the drugs listed in Table 2 may be quite common among children with chronic illnesses. Adequate dosage and length of treatment should be considered in these cases [6, 71, 98, 118]. Whether hepatic injury from underlying conditions, such as viral infections or metabolic diseases, is exacerbated by paracetamol remains uncertain [7]. However, some studies show that an underlying condition can increase the risk of hepatic injury. For example, Ceelie et al. [25] showed that some children with myopathies receiving recommended doses of paracetamol might be at increased risk for development of toxicity resulting in acute liver failure.
Clinical presentation of paracetamol intoxication
Paracetamol intoxication typically includes four phases [7].
The first consists of anorexia, nausea, vomiting, malaise, and diaphoresis, which may provoke administration of additional doses of paracetamol. In the second phase, the first-phase signs resolve and are replaced by right upper quadrant pain or tenderness, liver enlargement, and oliguria in some patients. Bilirubin, hepatic enzyme levels and the prothrombin time increase. In the third phase, usually 3 to 5 days into the course, anorexia, nausea, vomiting, and malaise reappear, along with signs of hepatic failure, including jaundice, hypoglycemia, coagulopathy, and encephalopathy. Renal failure and cardiomyopathy may also develop. The fourth phase is associated with recovery or progression to death from complete liver failure. Paracetamol poisoning may also present with central nervous system depression, shock, hypothermia, and metabolic acidosis [38].
Paracetamol toxicity treatment
With acute ingestion of paracetamol, the Rumack–Mathews nomogram is a valuable tool to assess the risk of hepatotoxicity [88, 96]. Overdose with intravenous paracetamol poses a specific management problem, as standard nomograms cannot be directly applied. In intravenous paracetamol overdose plasma levels peak immediately after intravenous injection, and will normally be lower than predicted from the same oral dose at the same time after ingestion. Guidance on management of IV paracetamol overdose is available from the UK National Poisons Information Service (NPIS), and is update regularly on Toxbase, the database of the NPIS (http://www.toxbase.org). IV paracetamol is potentially very toxic in overdose and managing clinicians are encouraged to discuss all patients with overdose with the local poisons information service.
Treatment is based on the use of NAC. A dose of activated charcoal is recommended within 6 to 8 h after an acute ingestion [88].
Intravenous administration of NAC over a 10-h period (rapidly) is associated with a higher frequency of allergic and anaphylactoid reactions (angioedema, hypotension, bronchospasm) [96] than is oral administration. Longer infusion periods (48 h or longer) of NAC result in improved tolerance and reduced adverse effects [88].
The treatment of hepatotoxicity caused by subacute overdosing is difficult and consultation of an expert should be considered.
Paracetamol and fever
Fever is one of the most common clinical symptoms managed by pediatricians and other health care providers and accounts, by some estimates, for one-third of all presenting conditions in children [31]. Fever is not an illness but a physiologic homeostatic mechanism that has beneficial effects in fighting infections [50]. Fever retards the growth and reproduction of bacteria and viruses, enhances neutrophil production and T-lymphocyte proliferation, and aids in the body’s acute-phase reaction [1]. The degree of fever does not generally correlate with severity of illness [1]. Moreover, the majority of evidence indicates that clinicians cannot rely on response to antipyretics to predict serious illness in febrile children [55]. Recent data on outcomes of meningitis, showed no improvement in patients treated with paracetamol in addition to antimicrobials compared with placebo in addition to antimicrobials [86, 113]. Other studies showed also poorer outcomes in patients with sepsis and bacteremia treated with other NSAIDS compared with patients treated with paracetamol [59, 60]. In patients with sepsis, the paracetamol may inhibit the immunological response [52]. Therefore, clinicians should be aware of the potential side effect to treat fever in infectious diseases in terms of poorer outcome of the patients treated with antipyretics.
The most consistently identified serious concern of caregivers and health care providers is that high fevers, if left untreated are associated with seizures, brain damage and death [17, 92].
It is argued that by creating undue concern over these presumed risks of fever, for which there is no clearly established relationship, physicians are promoting an exaggerated desire in parents to achieve normothermia by aggressively treating fever in their children. Moreover, there is no evidence that antipyretic therapy decreases the recurrence of febrile seizures [108].
In view of this, it is recommended to treat only children with fever who appear distressed [112]. It could be also useful to treat febrile children with concomitant drowsiness to discern if this condition is related simply to the fever or a potentially severe illness. Paracetamol doses of 5–15 mg/kg per dose given every 4 to 6 h orally or 15 to 20 mg/kg rectally are generally regarded as safe and effective (maximum dose 75 mg/kg/day) [103]. A dose of 90 mg/kg/day is considered by many authorities to be the definition of “supra-therapeutic dosing” [64, 103]. Typically, the onset of an antipyretic effect is within 30 to 60 min; approximately 80 % of children will experience a decreased temperature within that time [103, 109]. Although alternative dosing regimens have been suggested [77, 102, 110], no consistent evidence has indicated that the use of an initial loading dose by either the oral (30 mg/kg per dose) or rectal (40 mg/kg per dose) route improves antipyretic efficacy. The use of higher loading doses in clinical practice would add potential risks for dosing confusion leading to hepatotoxicity; therefore, such doses are not recommended [109].
Nabulsi et al. [77] showed that standard (15 mg/kg) oral, standard (15 mg/kg) rectal and high-rectal (35 mg/kg) paracetamol have similar antipyretic effectiveness. The effect compartment concentration of paracetamol that is sufficient for antipyretic effect is 5 mg/l (Fig. 3) [40] and this level is obtainable with rectal administration at standard dose. Much higher and not safe doses would be required for higher effect compartment concentrations and therefore, high-rectal dose should not be administered.
Moreover, there is no evidence to support the belief that rectal suppositories, whether prescribed in the standard dose of 15 mg/kg, or in the high dose of 30–40 mg/kg, are superior to oral paracetamol in terms of rapidity of action, or in the extent of temperature reduction [77]. The oral route should be preferred because of its predictable rapid absorption while the rectal route is effective in fever treatment in case of vomiting, or conditions preventing oral administration [77, 102]. Use of IV paracetamol is safe [124] and should be restricted to cases in which the oral or rectal route is not suitable.
A practice frequently used to control fever is the alternating or combined used of paracetamol and ibuprofen. Although 4 h was the most frequent interval, parents reported alternating therapy every 2, 3, 4, and 6 h, which suggests that there is no consensus on dosing instructions [120].
Some studies provide some evidence that combination therapy may be more effective at lowering temperature, questions remain regarding the safety of this practice as well as the effectiveness in improving discomfort [44, 57, 76, 85, 120]. There is no evidence that combination therapy results in overall improvement in other clinical outcomes. Therefore, the evidence to support or refuse the routine use of combination treatment with both paracetamol and ibuprofen are insufficient [109].
The NICE, in the updated guidance to help assess children with fever of May 2013, advises against giving both agents simultaneously and only considers alternating these agents if the distress, related to febrile condition, persists or recurs before the next dose is due [112].
Paracetamol and pain
Pain is a common condition in children and occurs predominantly during infectious illnesses, musculoskeletal injuries and after painful procedures or surgery.
Timely administration of analgesia affects the entire medical experience and can have a lasting effect on a child’s and the family’s reaction to current and future medical care [36].
Recommended paracetamol doses for pain management are given in Table 3 [122].
Paracetamol is the drug of choice for the management of mild to moderate pain and the management of moderate to severe pain with adjunctive opioid analgesics.
A large number of studies have been performed comparing paracetamol with NSAIDs for either analgesia or antipyresis in children. Most studies show either a similar effect or a slight superior effect of NSAIDs but one major criticism of such studies is that paracetamol dosing may not be equipotent with that of NSAID used [8]. Paracetamol has a better safety record for treatment of fever and pain related to upper airways infection since NSAIDS carry a higher risk of gastritis and renal impairment [18, 74]. NSAIDS showed to be superior for the treatment of muscle-skeletal traumatic pain [3, 27], and for the treatment of headache [67].
The rectal administration should be avoided in pain management because the effect compartment concentration of paracetamol required for analgesic effect is 10 mg/l (Fig. 2) [40]. This value is obtainable with oral administration at recommended doses of 15–20 mg/kg [122], but to obtain these levels with rectal route, it has been shown that the dose of rectal paracetamol should be greater than 40 mg/kg [40]. This dose exposes to a major risk of toxicity [103].
The US Food and Drug Administration approved IV paracetamol in January 2011 for short-term use in relieving moderate to severe pain. An intravenous paracetamol use is approved in children 2 years of age and older for the treatment of pain at a dose of 15 mg/kg every 6 h, not to exceed 75 mg/kg/day [34].
In the management of severe pain, the IV route could be preferred since it has a faster onset and results in more predictable pharmacokinetics than oral or rectal paracetamol formulations [16].
In the absence of iatrogenic medication error events, the IV use for the pain treatment is safe and effective [124].
Moreover, this formulation represents an attractive alternative or support with a dose sparing effect to IV opioids and non-steroidal anti-inflammatory drugs. Korpela et al. [56] showed that a single dose of 40 or 60 mg/kg of rectal paracetamol has a clear morphine-sparing effect in day-case surgery in children if administered at the induction of anesthesia. A meta-analysis of Remy et al. confirmed the morphine-sparing effect showing that paracetamol combined with patient-controlled analgesia morphine induced a significant morphine-sparing effect but did not change the incidence of morphine-related adverse effects. Ceelie et al. [24] in a recent randomized controlled trial showed that among infants undergoing major surgery, the addition of postoperative intermittent intravenous paracetamol to continuous morphine infusion compared with continuous morphine only resulted in a lower cumulative morphine dose over 48 h and a lower incidence of apnea and use of naloxone.
Finally, combination therapy with modest doses of paracetamol and ibuprofen has been shown to achieve as effective analgesia as single drug therapy with higher doses [69], while combination therapy with higher doses may increase propensity to adverse effects without analgesic gain [43].
Conclusions
Paracetamol is widely used but its analgesic mechanisms of action are still not well known. Paracetamol doses are different when treating fever or pain. Rectal administration of paracetamol should be avoided in pain management. While being a safe and effective drug it is important to optimize its administration to avoid overdoses and maximize effect. Fever phobia should be avoided and rationalized. Possible factors for increased risk of toxicity should be well known to the general pediatrician.
References
Adam HM (1996) Fever and host responses. Pediatr Rev 17:330–331
Alander SW, Dowd MD, Bratton SL, Kearns GL (2000) Pediatric acetaminophen overdose: risk factors associated with hepatocellular injury. Arch Pediatr Adolesc Med 154:346–350
Ali S, Drendel AL, Kircher J, Beno S (2010) Pain management of musculoskeletal injuries in children: current state and future directions. Pediatr Emerg Care 26:518–524
Allegaert K, Naulaers G, Vanhaesebrouck S, Anderson BJ (2013) The paracetamol concentration–effect relation in neonates. Paediatr Anaesth 23:45–50
Allegaert K, van de Velde M, van den Anker J (2013) Neonatal clinical pharmacology. Paediatr Anaesth
Altomare E, Leo MA, Lieber CS (1984) Interaction of acute ethanol administration with acetaminophen metabolism and toxicity in rats fed alcohol chronically. Alcohol Clin Exp Res 8:405–408
American Academy of Pediatrics. Committee on Drugs (2001) Acetaminophen toxicity in children. Pediatrics 108:1020–1024
Anderson BJ (2004) Comparing the efficacy of NSAIDs and paracetamol in children. Paediatr Anaesth 14:201–217
Anderson BJ (2008) Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth 18:915–921
Anderson BJ, Pons G, Autret-Leca E, Allegaert K, Boccard E (2005) Pediatric intravenous paracetamol (propacetamol) pharmacokinetics: a population analysis. Paediatr Anaesth 15:282–292
Anderson BJ, Woollard GA, Holford NH (2001) Acetaminophen analgesia in children: placebo effect and pain resolution after tonsillectomy. Eur J Clin Pharmacol 57:559–569
Arendt Nielsen L, Nielsen JC, Bjerring P (1991) Double-blind, placebo controlled comparison of paracetamol and paracetamol plus codeine: a quantitative evaluation by laser induced pain. Eur J Clin Pharmacol 40:241–247
Bagnall WE, Kelleher J, Walker BE, Losowsky MS (1979) The gastrointestinal absorption of paracetamol in the rat. J Pharm Pharmacol 31:157–160
Bannwarth B, Netter P, Lapicque F, Gillet P, Péré P, Boccard E, Royer RJ, Gaucher A (1992) Plasma and cerebrospinal fluid concentrations of paracetamol after a single intravenous dose of propacetamol. Br J Clin Pharmacol 34:79–81
Berlin CM Jr, Yaffe SJ, Ragni M (1980) Disposition of acetaminophen in milk, saliva, and plasma of lactating women. Pediatr Pharmacol (New York) 1:135–141
Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R, Leone S (2006) Paracetamol: new vistas of an old drug. CNS Drug Rev 12:250–275
Betz MG, Grunfeld AF (2006) ‘Fever phobia’ in the emergency department: a survey of children’s caregivers. Eur J Emerg Med 13:129–133
Bianciotto M, Chiappini E, Raffaldi I, Gabiano C, Tovo PA, Sollai S, de Martino M, Mannelli F, Tipo V, Da Cas R, Traversa G, Menniti-Ippolito F, Italian Multicenter Study Group for Drug and Vaccine Safety in Children (2013) Drug use and upper gastrointestinal complications in children: a case–control study. Arch Dis Child 98:218–221
Bisogno T (2008) Endogenous cannabinoids: structure and metabolism. J Neuroendocrinol 20(Suppl 1):1–9
Björkman R (1995) Central antinociceptive effects of non-steroidal anti-inflammatory drugs and paracetamol. Experimental studies in the rat. Acta Anaesthesiol Scand Suppl 103:1–44
Boyle M, Nicholson L, O’Brien M, Flynn GM, Collins DW, Walsh WR, Bihari D (2010) Paracetamol induced skin blood flow and blood pressure changes in febrile intensive care patients: an observational study. Aust Crit Care 23:208–214
Brown BL, Allis JW, Simmons JE, House DE (1995) Fasting for less than 24 h induces cytochrome P450 2E1 and 2B1/2 activities in rats. Toxicol Lett 81:39–44
Campbell NR, Baylis B (1992) Renal impairment associated with an acute paracetamol overdose in the absence of hepatotoxicity. Postgrad Med J 68:116–118
Ceelie I, de Wildt SN, van Dijk M, van den Berg MM, van den Bosch GE, Duivenvoorden HJ, de Leeuw TG, Mathôt R, Knibbe CA, Tibboel D (2013) Effect of intravenous paracetamol on postoperative morphine requirements in neonates and infants undergoing major noncardiac surgery: a randomized controlled trial. JAMA 309:149–154
Ceelie I, James LP, Gijsen V, Mathot RA, Ito S, Tesselaar CD, Tibboel D, Koren G, de Wildt SN (2011) Acute liver failure after recommended doses of acetaminophen in patients with myopathies. Crit Care Med 39:678–682
Chien JY, Peter RM, Nolan CM, Wartell C, Slattery JT, Nelson SD, Carithers RL Jr, Thummel KE (1997) Influence of polymorphic N-acetyltransferase phenotype on the inhibition and induction of acetaminophen bioactivation with long-term isoniazid. Clin Pharmacol Ther 61:24–34
Clark E, Plint AC, Correll R, Gaboury I, Passi B (2007) A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics 119:460–467
Clissold SP (1986) Aspirin and related derivatives of salicylic acid. Drugs 32:8–26
Committee on Infectious Disease AAoP (1982) Aspirin and Reye’s syndrome. Pediatrics 69:810
Courade JP, Martin K, Besse D, Delchambre C, Hanoun N, Hamon M, Eschalier A, Caussade F, Cloarec A (2001) Acetaminophen distribution in the rat central nervous system. Life Sci 69:1455–1464
Crocetti M, Moghbeli N, Serwint J (2001) Fever phobia revisited: have parental misconceptions about fever changed in 20 years? Pediatrics 107:1241–1246
Cullen S, Kenny D, Ward OC, Sabra K (1989) Paracetamol suppositories: a comparative study. Arch Dis Child 64:1504–1505
Dahlin DC, Miwa GT, Lu AY, Nelson SD (1984) N-Acetyl-p-benzoquinone imine: a cytochrome P-450-mediated oxidation product of acetaminophen. Proc Natl Acad Sci U S A 81:1327–1331
Dart RC, Rumack BH (2012) Intravenous acetaminophen in the United States: iatrogenic dosing errors. Pediatrics 129:349–353
Davenport A, Finn R (1988) Paracetamol (acetaminophen) poisoning resulting in acute renal failure without hepatic coma. Nephron 50:55–56
Fein JA, Zempsky WT, Cravero JP, Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine, American Academy of Pediatrics (2012) Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics 130:e1391–405
Fischereder M, Jaffe JP (1994) Thrombocytopenia following acute acetaminophen overdose. Am J Hematol 45:258–259
Flanagan RJ, Mant TG (1986) Coma and metabolic acidosis early in severe acute paracetamol poisoning. Hum Toxicol 5:179–182
Flower RJ, Vane JR (1972) Inhibition of prostaglandin synthetase in brain explains the anti-pyretic activity of paracetamol (4-acetamidophenol). Nature 240:410–411
Gibb IA, Anderson BJ (2008) Paracetamol (acetaminophen) pharmacodynamics: interpreting the plasma concentration. Arch Dis Child 93:241–247
Grand RJ, Watkins JB, Torti FM (1976) Development of the human gastrointestinal tract: a review. Gastroenterology 70:790–810
Gühring H, Hamza M, Sergejeva M, Ates M, Kotalla CE, Ledent C, Brune K (2002) A role for endocannabinoids in indomethacin-induced spinal antinociception. Eur J Pharmacol 454:153–163
Hannam J, Anderson BJ (2011) Explaining the acetaminophen–ibuprofen analgesic interaction using a response surface model. Paediatr Anaesth 21:1234–1240
Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, Peters TJ (2009) Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial. Health Technol Assess 13:iii–iv, ix–x, 1–163.
Henderson AJ, Shaheen SO (2013) Acetaminophen and asthma. Paediatr Respir Rev 14:9–15
Henretig FM, Selbst SM, Forrest C, Kearney TK, Orel H, Werner S, Williams TA (1989) Repeated acetaminophen overdosing. Causing hepatotoxicity in children. Clinical reports and literature review. Clin Pediatr (Phila) 28:525–528
Heubi JE, Barbacci MB, Zimmerman HJ (1998) Therapeutic misadventures with acetaminophen: hepatoxicity after multiple doses in children. J Pediatr 132:22–27
Högestätt ED, Jönsson BA, Ermund A, Andersson DA, Björk H, Alexander JP, Cravatt BF, Basbaum AI, Zygmunt PM (2005) Conversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous system. J Biol Chem 280:31405–31412
Inoue T, Mashimo T, Shibata M, Shibuta S, Yoshiya I (1998) Rapid development of nitric oxide-induced hyperalgesia depends on an alternate to the cGMP-mediated pathway in the rat neuropathic pain model. Brain Res 792:263–270
Jaffe DM (2002) Assessment of the child with fever. In: Rudolph CD, Rudolph AM, Hostetter MK, Lister GE, Siegel NJ (eds) Rudolph’s pediatrics, 21st edn. McGraw-Hill, New York, pp 302–309
James LP, Chiew A, Abdel-Rahman SM, Letzig L, Graudins A, Day P, Roberts D (2013) Acetaminophen protein adduct formation following low-dose acetaminophen exposure: comparison of immediate-release vs extended-release formulations. Eur J Clin Pharmacol 69:851–857
Jefferies S, Saxena M, Young P (2012) Paracetamol in critical illness: a review. Crit Care Resusc 14:74–80
Ji P, Wang Y, Li Z, Doddapaneni S, Hertz S, Furness S, Sahajwalla CG (2012) Regulatory review of acetaminophen clinical pharmacology in young pediatric patients. J Pharm Sci 101:4383–4389
Kelley MT, Walson PD, Edge JH, Cox S, Mortensen ME (1992) Pharmacokinetics and pharmacodynamics of ibuprofen isomers and acetaminophen in febrile children. Clin Pharmacol Ther 52:181–189
King D (2013) Question 2: does a failure to respond to antipyretics predict serious illness in children with a fever? Arch Dis Child 98:644–646
Korpela R, Korvenoja P, Meretoja OA (1999) Morphine-sparing effect of acetaminophen in pediatric day-case surgery. Anesthesiology 91:442–447
Kramer LC, Richards PA, Thompson AM, Harper DP, Fairchok MP (2008) Alternating antipyretics: antipyretic efficacy of acetaminophen versus acetaminophen alternated with ibuprofen in children. Clin Pediatr (Phila) 47:907–911
Kuehn B (2013) FDA: Acetaminophen may trigger serious skin problems. JAMA 310:785
Kuikka A, Sivonen A, Emelianova A, Valtonen VV (1997) Prognostic factors associated with improved outcome of Escherichia coli bacteremia in a Finnish university hospital. Eur J Clin Microbiol Infect Dis 16:125–134
Kuikka A, Valtonen VV (1998) Factors associated with improved outcome of Pseudomonas aeruginosa bacteremia in a Finnish university hospital. Eur J Clin Microbiol Infect Dis 17:701–708
Kumpulainen E, Kokki H, Halonen T, Heikkinen M, Savolainen J, Laisalmi M (2007) Paracetamol (acetaminophen) penetrates readily into the cerebrospinal fluid of children after intravenous administration. Pediatrics 119:766–771
Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, Reisch JS, Schiødt FV, Ostapowicz G, Shakil AO, Lee WM, Acute Liver Failure Study Group (2005) Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology 42:1364–1372
Lauterburg BH, Mitchell JR (1987) Therapeutic doses of acetaminophen stimulate the turnover of cysteine and glutathione in man. J Hepatol 4:206–211
Lavonas EJ, Reynolds KM, Dart RC (2010) Therapeutic acetaminophen is not associated with liver injury in children: a systematic review. Pediatrics 126:e1430–1444
Makin AJ, Wendon J, Williams R (1995) A 7-year experience of severe acetaminophen-induced hepatotoxicity (1987–1993). Gastroenterology 109:1907–1916
Manyike PT, Kharasch ED, Kalhorn TF, Slattery JT (2000) Contribution of CYP2E1 and CYP3A to acetaminophen reactive metabolite formation. Clin Pharmacol Ther 67:275–282
Manzano S, Doyon-Trottier E, Bailey B (2010) Myth: ibuprofen is superior to acetaminophen for the treatment of benign headaches in children and adults. CJEM 12:220–222
McGill MR, Jaeschke H (2013) Metabolism and disposition of acetaminophen: recent advances in relation to hepatotoxicity and diagnosis. Pharm Res 30:2174–2187
Mehlisch DR, Aspley S, Daniels SE, Bandy DP (2010) Comparison of the analgesic efficacy of concurrent ibuprofen and paracetamol with ibuprofen or paracetamol alone in the management of moderate to severe acute postoperative dental pain in adolescents and adults: a randomized, double-blind, placebo-controlled, parallel-group, single-dose, two-center, modified factorial study. Clin Ther 32:882–895
Meller ST, Dykstra C, Gebhart GF (1992) Production of endogenous nitric oxide and activation of soluble guanylate cyclise are required for N-methyl-d-aspartate-produced facilitation of the nociceptive tail-flick reflex. Eur J Pharmacol 214:93–96
Miller MG, Price VF, Jollow DJ (1986) Anomalous susceptibility of the fasted hamster to acetaminophen hepatotoxicity. Biochem Pharmacol 35:817–825
Miller RP, Roberts RJ, Fischer LJ (1976) Acetaminophen elimination kinetics in neonates, children, and adults. Clin Pharmacol Ther 19:284–294
Miners JO, Osborne NJ, Tonkin AL, Birkett DJ (1992) Perturbation of paracetamol urinary metabolic ratios by urine flow rate. Br J Clin Pharmacol 34:359–362
Misurac JM, Knoderer CA, Leiser JD, Nailescu C, Wilson AC, Andreoli SP (2013) Nonsteroidal anti-inflammatory drugs are an important cause of acute kidney injury in children. J Pediatr 162:1153–1159
Murphy R, Swartz R, Watkins PB (1990) Severe acetaminophen toxicity in a patient receiving isoniazid. Ann Intern Med 113:799–800
Nabulsi M, Tamim H, Mahfoud Z, Itani M, Sabra R, Chamseddine F, Mikati M (2006) Alternating ibuprofen and acetaminophen in the treatment of febrile children: a pilot study. BMC Med 4:4
Nabulsi M, Tamim H, Sabra R, Mahfoud Z, Malaeb S, Fakih H, Mikati M (2005) Equal antipyretic effectiveness of oral and rectal acetaminophen: a randomized controlled trial. BMC Pediatr 5:35–42
Nassini R, Materazzi S, Andrè E, Sartiani L, Aldini G, Trevisani M, Carnini C, Massi D, Pedretti P, Carini M, Cerbai E, Preti D, Villetti G, Civelli M, Trevisan G, Azzari C, Stokesberry S, Sadofsky L, McGarvey L, Patacchini R, Geppetti P (2010) Acetaminophen, via its reactive metabolite N-acetyl-p-benzo-quinone imine and transient receptor potential ankyrin-1 stimulation, causes neurogenic inflammation in the airways and other tissues in rodents. FASEB J 24:4904–16
Nielsen JC, Bjerring P, Arendt Nielsen L, Petterson KJ (1992) Analgesic efficacy of immediate and sustained release paracetamol and plasma concentration of paracetamol. Double blind, placebo-controlled evaluation using painful laser stimulation. Eur J Clin Pharmacol 42:261–264
Notarianni LJ, Oldham HG, Bennett PN (1987) Passage of paracetamol into breast milk and its subsequent metabolism by the neonate. Br J Clin Pharmacol 24:63–67
O’Shea D, Davis SN, Kim RB, Wilkinson GR (1994) Effect of fasting and obesity in humans on the 6-hydroxylation of chlorzoxazone: a putative probe of CYP2E1 activity. Clin Pharmacol Ther 56:359–367
Ottani A, Leone S, Sandrini M, Ferrari A, Bertolini A (2006) The analgesic activity of paracetamol is prevented by the blockade of cannabinoid CB1 receptors. Eur J Pharmacol 531:280–281
Palmer GM, Atkins M, Anderson BJ, Smith KR, Culnane TJ, McNally CM, Perkins EJ, Chalkiadis GA, Hunt RW (2008) I.V. acetaminophen pharmacokinetics in neonates after multiple doses. Br J Anaesth 101:523–530
Patel M, Tang BK, Kalow W (1992) Variability of acetaminophen metabolism in Caucasians and Orientals. Pharmacogenetics 2:38–45
Paul IM, Sturgis SA, Yang C, Engle L, Watts H, Berlin CM Jr (2010) Efficacy of standard doses of Ibuprofen alone, alternating, and combined with acetaminophen for the treatment of febrile children. Clin Ther 32:2433–2440
Pelkonen T, Roine I, Cruzeiro ML, Pitkäranta A, Kataja M, Peltola H (2011) Slow initial β-lactam infusion and oral paracetamol to treat childhood bacterial meningitis: a randomised, controlled trial. Lancet Infect Dis 11:613–621
Perneger TV, Whelton PK, Klag MJ (1994) Risk of kidney failure associated with the use of acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs. N Engl J Med 331:1675–1679
Perry HE, Shannon MW (1998) Efficacy of oral versus intravenous N-acetylcysteine in acetaminophen overdose: results of an open-label, clinical trial. J Pediatr 132:149–152
Peterson JD, Herzenberg LA, Vasquez K, Waltenbaugh C (1998) Glutathione levels in antigen-presenting cells modulate Th1 versus Th2 response patterns. Proc Natl Acad Sci U S A 95:3071–3076
Pickering G, Estève V, Loriot MA, Eschalier A, Dubray C (2008) Acetaminophen reinforces descending inhibitory pain pathways. Clin Pharmacol Ther 84:47–51
Piñeiro-Carrero VM, Piñeiro EO (2004) Liver. Pediatrics 113:1097–1106
Poirier MP, Davis PH, Gonzalez-del Rey JA, Monroe KW (2000) Pediatric emergency department nurses’ perspectives on fever in children. Pediatr Emerg Care 16:9–12
Prescott LF (1980) Kinetics and metabolism of paracetamol and phenacetin. Br J Clin Pharmacol 10:291S–298S
Prescott LF (1982) Analgesic nephropathy. Drugs 23:75–149
Prescott LF (2001) Paracetamol (acetaminophen): a critical bibliographic review, 2nd edn. CRC Press, Boca Raton, 1001 p
Prescott LF, Illingworth RN, Critchley JA, Stewart MJ, Adam RD, Proudfoot AT (1979) Intravenous N-acetylcystine: the treatment of choice for paracetamol poisoning. Br Med J 2:1097–10100
Price VF, Jollow DJ (1989) Effect of glucose and gluconeogenic substrates on fasting-induced suppression of acetaminophen glucuronidation in the rat. Biochem Pharmacol 38:289–297
Rivera-Penera T, Gugig R, Davis J, McDiarmid S, Vargas J, Rosenthal P, Berquist W, Heyman MB, Ament ME (1997) Outcome of acetaminophen overdose in pediatric patients and factors contributing to hepatotoxicity. J Pediatr 130:300–304
Rumack BH (1984) Acetaminophen overdose in young children. Treatment and effects of alcohol and other additional ingestants in 417 cases. Am J Dis Child 138:428–433
Rygnestad T, Zahlsen K, Samdal FA (2000) Absorption of effervescent paracetamol tablets relative to ordinary paracetamol tablets in healthy volunteers. Eur J Clin Pharmacol 56:141–143
Sauerwein RW, Mulder JA, Mulder L, Lowe B, Peshu N, Demacker PN, van der Meer JW, Marsh K (1997) Inflammatory mediators in children with protein-energy malnutrition. Am J Clin Nutr 65:1534–1539
Scolnik D, Kozer E, Jacobson S, Diamond S, Young NL (2002) Comparison of oral versus normal and high-dose rectal acetaminophen in the treatment of febrile children. Pediatrics 110:553–556
Section on Clinical Pharmacology and Therapeutics, Committee on Drugs, Sullivan JE, Farrar HC (2011) Fever and antipyretic use in children. Pediatrics 127:580–587
Shaheen SO, Newson RB, Henderson AJ, Headley JE, Stratton FD, Jones RW, Strachan DP, ALSPAC Study Team (2005) Prenatal paracetamol exposure and risk of asthma and elevated immunoglobulin E in childhood. Clin Exp Allergy 35:18–25
Singla NK, Parulan C, Samson R, Hutchinson J, Bushnell R, Beja EG, Ang R, Royal MA (2012) Plasma and cerebrospinal fluid pharmacokinetic parameters after single-dose administration of intravenous, oral, or rectal acetaminophen. Pain Pract 12:523–532
Song BJ, Veech RL, Saenger P (1990) Cytochrome P450IIE1 is elevated in lymphocytes from poorly controlled insulin-dependent diabetics. J Clin Endocrinol Metab 71:1036–1040
Squires RH Jr, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, Dhawan A, Rosenthal P, Rodriguez-Baez N, Murray KF, Horslen S, Martin MG, Lopez MJ, Soriano H, McGuire BM, Jonas MM, Yazigi N, Shepherd RW, Schwarz K, Lobritto S, Thomas DW, Lavine JE, Karpen S, Ng V, Kelly D, Simonds N, Hynan LS (2006) Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr 148:652–658
Steering Committee on Quality Improvement and Management, Subcommittee on Febrile Seizures American Academy of Pediatrics (2008) Febrile seizures: clinical practice guideline for the long-term management of the child with simple febrile seizures. Pediatrics 121:1281–1286
Temple AR, Temple BR, Kuffner EK (2013) Dosing and antipyretic efficacy of oral acetaminophen in children. Clin Ther
Tréluyer JM, Tonnelier S, d’Athis P, Leclerc B, Jolivet-Landreau I, Pons G (2001) Antipyretic efficacy of an initial 30-mg/kg loading dose of acetaminophen versus a 15-mg/kg maintenance dose. Pediatrics 108:E73
Ueshima Y, Tsutsumi M, Takase S, Matsuda Y, Kawahara H (1996) Acetaminophen metabolism in patients with different cytochrome P-4502E1 genotypes. Alcohol Clin Exp Res 20:25A–28A
Updated guidance to help assess children with fever, NICE clinical guidelines, 22 May 2013
van de Beek D, Brouwer MC, Thwaites GE, Tunkel AR (2012) Advances in treatment of bacterial meningitis. Lancet 380:1693–1702
van der Marel CD, Anderson BJ, van Lingen RA, Holford NH, Pluim MA, Jansman FG, van den Anker JN, Tibboel D (2003) Paracetamol and metabolite pharmacokinetics in infants. Eur J Clin Pharmacol 59:243–251
Vieira I, Sonnier M, Cresteil T (1996) Developmental expression of CYP2E1 in the human liver. Hypermethylation control of gene expression during the neonatal period. Eur J Biochem 238:476–483
Wallace JL (2006) COX-2: a pivotal enzyme in mucosal protection and resolution of inflammation. Sci World J 6:577–588
Watkins PB, Kaplowitz N, Slattery JT, Colonese CR, Colucci SV, Stewart PW, Harris SC (2006) Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial. JAMA 296:87–93
Whitcomb DC, Block GD (1994) Association of acetaminophen hepatotoxicity with fasting and ethanol use. JAMA 272:1845–1850
Wilson JT, Brown RD, Bocchini JA Jr, Kearns G (1982) Efficacy, disposition and pharmacodynamics of aspirin, acetaminophen and choline salicylate in young febrile children. Ther Drug Monit 4:147–180
Wright AD, Liebelt EL (2011) Alternating antipyretics for fever reduction in children: an unfounded practice passed down to parents from pediatricians. Arch Dis Child 96:1175–1179
Yang CC, Deng JF, Lin TJ (2001) Pancytopenia, hyperglycemia, shock, coma, rhabdomyolysis, and pancreatitis associated with acetaminophen poisoning. Vet Hum Toxicol 43:344–348
Zernikow B, Hechler T (2008) Pain therapy in children and adolescents. Dtsch Arztebl Int 105:511–521
Zhang W, Parentau H, Greenly RL, Metz CA, Aggarwal S, Wainer IW, Tracy TS (1999) Effect of protein-calorie malnutrition on cytochromes P450 and glutathione S-transferase. Eur J Drug Metab Pharmacokinet 24:141–147
Zuppa AF, Hammer GB, Barrett JS, Kenney BF, Kassir N, Mouksassi S, Royal MA (2011) Safety and population pharmacokinetic analysis of intravenous acetaminophen in neonates, infants, children, and adolescents with pain or fever. J Pediatr Pharmacol Ther 16:246–261
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marzuillo, P., Guarino, S. & Barbi, E. Paracetamol: a focus for the general pediatrician. Eur J Pediatr 173, 415–425 (2014). https://doi.org/10.1007/s00431-013-2239-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-013-2239-5