Abstract
Dietary and serum total antioxidant capacity (TAC) are considered appropriate tools for investigating the potential health effects of dietary antioxidants consumed in mixed diets. The aim was to analyze the impact of a dietary intervention on macronutrient intakes and to evaluate the improvement on oxidative status after weight loss (WL) by measuring dietary and serum TAC, and urinary F2-isoprostane levels as markers of oxidative stress. Forty-four overweight/obese children (mean age 11.5 years) were enrolled to undergo a 10-week WL program. They were dichotomized at the median of body mass index–standard deviation score (BMI-SDS) change, as high (HR) and low responders (LR) after intervention. Subjects were prescribed with a fixed full-day meal diet, calculated according to their basal metabolic rate and physical activity levels. A validated food-frequency questionnaire was used to retrospectively calculate TAC and daily nutrient intake. The HR subjects were able to reduce anthropometric indices and to improve lipid and glucose profile. They also significantly diminished fat intake (p = 0.013). Moreover, baseline serum TAC values did significantly predict the reduction in urinary F2 isoprostane (B = −0.236 (−0.393 to −0.078); p = 0.014) in the HR group after the WL program. Notably, changes in dietary TAC after the treatment were associated with a decrease in body weight after the 10-week intervention (B = −2.815 (−5.313 to −0.318), p = 0.029) in the HR group. The -ΔSerumTAC/ΔDietaryTAC and the -ΔF2Isoprostane/ΔDietaryTAC ratios revealed that the relationships between oxidative markers and antioxidants dietary intake were more favorable in the HR than in the LR group. Conclusion: Our study showed that a 10-week WL program was able to reduce adiposity indices in obese children. Moreover, after the intervention changes in dietary TAC and WL were significantly associated. Our result suggests that specific food with a high TAC content (such as fruits, vegetables, and legumes) could be recommended to improve WL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oxidative stress, which is attributed to an excessive production of reactive oxygen species and/or an impaired antioxidant defense system in body cells, is often augmented in obese subjects [4, 13, 29]. Isoprostanes are products of free radical-catalyzed lipid peroxidation of arachidonic acid [11]. They are formed in situ, esterified to phospholipids, and released by phospholipases into the plasma. They are subsequently removed from the plasma via the kidney, excreted in urine, and used as reliable markers of oxidative stress. Thus, 8-epi-prostaglandin (PG)-F2α or F2 isoprostane is reported to be a greater in obese children [10, 20]. Furthermore, F2 isoprostane is related to obesity complications such as atherosclerosis and insulin resistance in obese adults [8, 16, 48, 52].
Furthermore, it has been suggested that dietary antioxidant intake is able to protect against oxidative damage and related inflammatory complications [5, 9, 39, 40]. Moreover, given that the concentration of a single antioxidant may not reflect the total antioxidant value of food, the concept of dietary total antioxidant capacity (TAC) has emerged [47]. In fact, dietary TAC has been suggested as a tool for investigating the potential beneficial effects of dietary antioxidants occurring in mixed diets [3].
Since some dietary intervention programs in obese children demonstrated an oxidative status improvement after a weight loss (WL) process [14, 27], we hypothesized that by modifying the dietary TAC, a 10-week moderate caloric restriction intervention could influence the oxidative status in obese children. Our aim was to analyze the impact of a WL intervention program on macronutrient intakes and oxidative status by measuring the dietary and serum TAC, as well as the urinary F2 isoprostane levels.
Subjects and methods
Subjects
For the study, 71 children between the ages of 7 and 15, categorized as overweight or obese according to the Cole et al. criteria [6], were invited to participate in an information session. Children were recruited from the Endocrinology Pediatric Units of the University of Navarra Clinic and Navarra’s Hospital Complex in Pamplona, Navarra. They were Spanish, or foreign nationals being schooled in Spain for at least a year. Participants with a major psychiatric illness, significant neurological disease, bulimia nervosa, familiar hyperlipidemia, or any sort of either major cardiovascular or respiratory complication were excluded. Children and their parents signed a written informed consent. The study protocol was performed in accordance with the ethical standards of the Declaration of Helsinki, and was approved by the ethics committee of the University of Navarra (reference number 038/2009).
From the initial 71 volunteers, 54 successfully underwent baseline anthropometric measurements and 44 participants (22 boys, 22 girls) concluded the 10-week dietary intervention. The dropout rate was 18.5 % and the reasons for dropout were discouragement, social causes, forgetfulness, exams periods, and inability to be accompanied by a family member to the dietician’s weekly visit, as described in other children trials. Body mass index (BMI) was calculated from weight and height measurements. BMI Z-scores or standard deviation score (SDS) for sex and age were derived from Spanish reference data according to specific cutoff points for BMI [30]. The response of participants to the intervention program was based in changes in BMI-SDS. The sample (n = 44) was dichotomized at the median of their BMI-SDS change (equal to 0.5) for analyzing the response depending on the WL outcome. Thus, children who lost ≥0.50 BMI-SDS were considered “high responders” (HR; n = 22) and those who lost <0.50 BMI-SDS were considered “low responders” (LR; n = 22) to the dietary intervention. Dropouts were similar in both experimental groups.
Anthropometric, clinical, and biochemical measurements
All anthropometric and biochemical measures were carried out at baseline and after the 10-week intervention, following standardized procedures [19]. Measurements were carried out by trained personnel, and all participants were barefoot and wearing light clothes. All measurements were performed three times and the final data were the mean from the values obtained.
Body weight was determined using a digital scale (TBF-410, TANITA, Tokyo, Japan). Height was measured using a stadiometer (Seca 220, Vogel & Halke, Germany). To measure height, hair ornaments were removed. The participants were asked to stand on the stadiometer with the feet placed parallel and slightly apart, and heels, buttocks, scapula, and occipital head area touching the vertical board at the same time.
Waist circumference (WC) and hip circumference (HC) were measured using a non-stretchable measuring tape (type SECA 200). The subjects were asked to stand erect on a flat surface in a relaxed position with both feet together. WC was measured as the smallest horizontal girth between the costal margins and the iliac crests at minimal respiration. HC was taken as the greatest circumference at the level of the greater trochanter (the widest portion of the hip) on both sides. For both WC and HC, three measurements were made, and the mean of the three readings was taken as the final value. The waist-to-hip and waist-to-height ratios were also calculated.
Blood pressure was measured using an electronic sphygmomanometer (Minimus II, Riester, Germany) on the right arm with a cuff that covered more than two thirds of the upper arm, at a point midway between the olecranon and the acromion, following WHO criteria. Blood pressure was measured twice and the blood pressure value was the mean of the two measurements.
Venous blood samples were obtained by trained nurses at the hospital after an overnight fast. Glucose, insulin, and lipid profile were determined by standard autoanalyzer techniques as described elsewhere [28]. Insulin resistance was calculated from fasting glucose and insulin values according to the homeostasis model assessment of insulin resistance (HOMA-IR) [24].
Serum TAC was determined, at baseline and at the end of the treatment, based on the Trolox equivalent antioxidant capacity assay using a colorimetric commercial kit (Cayman Chemical Corp., Ann Arbor, MI, USA). To determine the level of urinary F2 isoprostane, the first void of the morning urine was collected in plastic vessels for three consecutive days. Morning urine—rather than 24-h urine collection—was obtained based on previous data which indicated that 24-h measurements expressed per milligram creatinine were not statistically different from values obtained from morning urine [50]. Urinary F2 isoprostane was measured using an ELISA kit according to the manufacturer’s protocol (Oxford Biomedical Research, Oxford, MI, USA), and was expressed in nanograms per milligram creatinine.
In addition to the anthropometry and biochemical determinations, the children’s body composition was measured before and after the intervention program using bioelectrical impedance analysis equipment (TBF-410, TANITA, Tokyo, Japan). Pubertal development was assessed according to the five established Tanner stages [49]. Each stage describes breast and pubic hair development in girls and genital and pubic hair development in boys.
Information on the levels of physical activity was collected with the “Seguimiento Universidad de Navarra” (SUN) validated questionnaire and total metabolic equivalents–minutes per day (METs-min/day) for each participant were derived from the different physical activities indicated and their typical average energy expenditure, as described elsewhere [45].
Dietary treatment and intake assessment
Dietary follow-ups, weight control, and nutritional education were performed weekly through individual sessions with a registered dietician (RD). The adherence to the ten weekly appointments with the RD was 93 % in all participants. Subjects were prescribed a fixed full-day meal diet, calculated according to their basal metabolic rate and physical activity levels [45]. Energy expenditure was estimated taking into account basal metabolism using the Schofield equation [31, 46], according to sex and body growth period. Children and their parents received personal training in nutritional and physical education throughout the whole intervention period. In all cases, diets were not lower than 1,500 kcal per day and not higher than 2,000 kcal/day. Dietary intake information was obtained at baseline and at the end of the intervention, with the semiquantitative 136-item SUN food–frequency questionnaire (FFQ), previously validated and applied in children [22, 23, 32]. Daily food consumption was estimated as frequency × portion size for each consumed food item. Nutrient intake was estimated using an ad hoc computer program specifically developed for this aim, which displays the latest available information, included in the food composition tables for Spain.
Furthermore, dietary TAC value was calculated based on the SUN FFQ by adding TAC values from the ferric reducing–antioxidant power assay of each food, as previously reported [17, 18, 34, 35, 37, 44], and was expressed as TAC in millimoles per 100 g of food. To assign a value to TAC-providing foods not available in previous reports, the data for a similar food item (e.g., same botanical group) were used as a proxy. When TAC values of cooked food were not available, TAC values of fresh food were used to calculate dietary TAC. The mean of TAC values of food contained in each item of the SUN FFQ was used to calculate the dietary TAC value from this questionnaire [38].
Statistical analyses
Results are shown as mean ± standard error of the mean. Unpaired and paired t tests were used as appropriate to assess anthropometric and other studied variables at baseline and after the WL intervention. Multivariable lineal regression analyses were performed to estimate associations between basal serum TAC and the change in urinary F2 isoprostane, and between dietary TAC changes and WL, after adjustment for potential confounders when indicated. Confidence intervals are used to describe the lineal regression coefficient (B) values. The following potential confounders were considered: sex, Tanner stage, baseline BMI-SDS, total energy intake, or physical activity levels as indicated. Partial correlations were performed after the 10-week dietary intervention to further explain relationships between dietary TAC and consumption of several food items. Statistical analyses were performed using SPSS for Windows 15.0 software (SPSS Inc., Chicago, IL). A p value less than 0.05 is considered as statistically significant.
Results
Forty-four obese children (mean age 11.5 years), with a BMI-SDS equal to 4.0 and 37.3 % of fat mass, were enrolled in the program. They were distributed in HR and LR groups according to the response (change in BMI-SDS) (Table 1). The HR and LR subjects presented similar anthropometric parameters and plasma profile at baseline. Serum and dietary TAC values and urinary F2 isoprostane as markers of oxidative stress from participants are also indicated in Table 1. With regard to physical activity, no differences between both groups were observed after the intervention program (HR 0.97 ± 5.90 METs-min/day and LR −1.01 ± 4.89 METs-min/day; p = 0.871 and 0.840, respectively, data not shown).
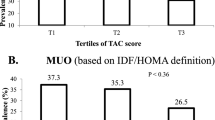
Our obese children (n = 44) did exceed most of the dietary reference intakes at baseline, except for fiber. Moreover, Fig. 1 shows that there are no differences in macronutrient intake (expressed as %E) between groups. After the intervention, there was a tendency to lower energy and macronutrients intake in both groups (Table 2). Interestingly, total fat intake was significantly lower (p = 0.013) after the 10-week WL program in the HR group. No association was found between fat intake and WL or oxidative status markers in our trial. However, a strong association between dietary TAC and consumption of vegetables, cereals, fruits, vitamin C, and folic acid was found in the HR group, regardless of BMI-SDS and total energy intake (Tables 3 and 4).
Consequently, significant changes were observed in anthropometric and clinical parameters in the HR group (Table 3). The mean WL in the HR group was −3.73 ± 0.24 kg (p < 0.001). Moreover, a significant reduction in BMI-SDS (−0.78 ± 0.07, p < 0.001), body fat mass (−2.95 ± 0.65 %, p < 0.001), and waist circumference (−5.40 ± 0.55 cm, p < 0.001) were seen in HR subjects. The decrease in adiposity measurements in the HR group was associated with a reduction in serum glucose (−6.00 ± 1.27 mg/dL, p < 0.001), total cholesterol (−20.95 ± 5.02 mg/dL, p < 0.001), insulin levels (−4.53 ± 1.59 μU/mL, p = 0.010), and HOMA-IR (−1.23 ± 0.37, p = 0.003). But, no statistical associations between oxidative status markers and changes in adiposity indices or biochemical parameters were found.
In a multivariable linear regression, basal serum TAC values did significantly predict the change in urinary F2 isoprostane after the WL (B = −0.236 (−0.393 to −0.078); p = 0.014) in the HR group, after adjusting for potential confounders. Moreover, changes in dietary TAC after the treatment were associated with a decrease in body weight after the 10-week intervention (B = −2.815 (−5.313 to −0.318), p = 0.029) in the HR group.
Interestingly, the reduction in the dietary TAC in the HR group was slightly greater than in the LR group, but the decrease in serum TAC was lower (Table 3). The -ΔSerumTAC/ΔDietaryTAC ratio was similar in HR and LR subjects (Fig. 2), but the -ΔF2Isoprostane/ΔDietaryTAC ratio was quite different (p = 0.026) between HR and LR groups, being more favorable in HR subjects.
Discussion
Our study was designed to evaluate oxidative status changes in obese children after a WL intervention program by assessing dietary and serum TAC, and F2 isoprostane levels.
The WL program consisted in a moderate calorie restriction, not to interfere with children growth, which was able to reduce anthropometric indices and to improve lipid and glucose profile as reported elsewhere [43]. Previous studies have shown that an improvement in body composition and cardiometabolic risk can be seen with a BMI-SDS reduction of ≥0.25 in obese children, while greater benefits occurs when losing at least 0.5 BMI-SDS [12]. Our results suggest that a WL intervention as short as 10-week can improve metabolic syndrome parameters in obese children, as seen in other studies [7, 42].
Initially, a higher macronutrient intake especially for fat intake was found in our population compared to dietary reference intakes. Similar findings are reported for obese children in other trials [15, 21]. After the WL intervention program, a modest reduction in fat intake was observed in the HR group, as observed in several intervention studies [53, 54].
There is evidence that the dietary intake information derived from a FFQ is appropriate to calculate the dietary TAC in a reliable manner in children and adults [33, 41]. Dietary TAC has been highly related to the consumption of some specific food groups as vegetables, fruits, and legumes [41], which are an important source of dietary antioxidant nutrients or components [1, 17].
Furthermore, a recent study showed that dietary TAC is positively associated with plasma TAC in healthy young adults [38], suggesting that dietary TAC may constitute a useful tool in antioxidant intake assessment, although this outcome was not found in our trial. In our obese children, it seems that baseline serum TAC predicts the reduction in urinary F2 isoprostane after the WL program.
No changes in oxidative stress markers were found in our obese population after the WL program. We could not find studies performed in children. In adults, Tsai et al. (2009) showed similar findings; a 4 % reduction in body weight did not change either plasma or urinary F(2)-isoprostane [51]. Moreover, Melissas et al. (2006) did not observe any changes in serum TAC after surgical weight reduction [25].
Nevertheless, after the intervention changes in dietary TAC and WL were significantly associated in the HR group. This could suggest that specific food with a high TAC content (such as fruits, vegetables, and legumes) are to be recommended to improve WL. In a similar way, Bahadoran et al. (2012) showed that a higher intake of dietary antioxidants also resulted in lower body weight and abdominal fat gain in adults [2]. Moreover, Puchau et al. (2010) showed an inverse association between adiposity (BMI-SDS, total body fat) and dietary TAC in obese children [36]. It seems that the potential effects of food antioxidants may occur through modification of lipids and carbohydrates metabolism, increased insulin sensitivity, and regulation of both appetite and adipocytokines [26].
Strengths of our study include (1) measurements in young subjects less exposed to chronic oxidative stress, (2) the overweight/obese subjects in the HR group, achieved substantial WL (higher than 5 % of initial body weight) after a short dietary intervention, (3) a standardized intervention with similar dietary conditions applied to a relatively homogeneous group, and (4) the assessment of markers of oxidative stress at baseline and after the intervention. On the other hand, some weaknesses of the study are (1) our design of a “case-only” approach without normal weight subjects, (2) the limited number of children per group, (3) bias in reporting of food intake, and (3) the pre-pubertal stage of the volunteers, with an intense growth and endocrine changes which may influence the outcome.
In summary, our study demonstrates that a 10-week WL program had a positive impact on changes in body composition and biochemical profile in obese children (HR group). Our data suggest that dietary TAC, as a measure of antioxidant intake, could be a potential marker of diet quality in obese children with a successful response to a WL program.
References
Agudo A, Cabrera L, Amiano P, Ardanaz E, Barricarte A, Berenguer T, Chirlaque MD, Dorronsoro M, Jakszyn P, Larranaga N, Martinez C, Navarro C, Quiros JR, Sanchez MJ, Tormo MJ, Gonzalez CA (2007) Fruit and vegetable intakes, dietary antioxidant nutrients, and total mortality in Spanish adults: findings from the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain). Am J Clin Nutr 85(6):1634–1642
Bahadoran Z, Golzarand M, Mirmiran P, Shiva N, Azizi F (2012) Dietary total antioxidant capacity and the occurrence of metabolic syndrome and its components after a 3-year follow-up in adults: Tehran Lipid and Glucose Study. Nutr Metab (Lond) 9(1):70. doi:10.1186/1743-7075-9-70
Brighenti F, Valtuena S, Pellegrini N, Ardigo D, Del Rio D, Salvatore S, Piatti P, Serafini M, Zavaroni I (2005) Total antioxidant capacity of the diet is inversely and independently related to plasma concentration of high-sensitivity C-reactive protein in adult Italian subjects. Br J Nutr 93(5):619–625
Codoner-Franch P, Boix-Garcia L, Simo-Jorda R, Del Castillo-Villaescusa C, Maset-Maldonado J, Valls-Belles V (2010) Is obesity associated with oxidative stress in children? Int J Pediatr Obes 5(1):56–63. doi:10.3109/17477160903055945
Codoner-Franch P, Lopez-Jaen AB, De La Mano-Hernandez A, Sentandreu E, Simo-Jorda R, Valls-Belles V (2010) Oxidative markers in children with severe obesity following low-calorie diets supplemented with mandarin juice. Acta Paediatr 99(12):1841–1846. doi:10.1111/j.1651-2227.2010.01903.x
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320(7244):1240–1243
Coppen AM, Risser JA, Vash PD (2008) Metabolic syndrome resolution in children and adolescents after 10 weeks of weight loss. J Cardiometab Syndr 3(4):205–210. doi:10.1111/j.1559-4572.2008.00016.x
Cracowski JL, Durand T, Bessard G (2002) Isoprostanes as a biomarker of lipid peroxidation in humans: physiology, pharmacology, and clinical implications. Trends Pharmacol Sci 23(8):360–366
Dandona P, Aljada A, Bandyopadhyay A (2004) Inflammation: the link between insulin resistance, obesity, and diabetes. Trends Immunol 25(1):4–7
Desideri G, De Simone M, Iughetti L, Rosato T, Iezzi ML, Marinucci MC, Cofini V, Croce G, Passacquale G, Necozione S, Ferri C (2005) Early activation of vascular endothelial cells and platelets in obese children. J Clin Endocrinol Metab 90(6):3145–3152. doi:10.1210/jc.2004-1741
Fam SS, Morrow JD (2003) The isoprostanes: unique products of arachidonic acid oxidation—a review. Curr Med Chem 10(17):1723–1740
Ford AL, Hunt LP, Cooper A, Shield JP (2010) What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child 95(4):256–261. doi:10.1136/adc.2009.165340
Fulop T, Tessier D, Carpentier A (2006) The metabolic syndrome. Pathol Biol (Paris) 54(7):375–386. doi:10.1016/j.patbio.2006.07.002
Gao Z, Novick M, Muller MD, Williams RJ, Spilk S, Leuenberger UA, Sinoway LI (2012) Exercise and diet-induced weight loss attenuates oxidative stress related-coronary vasoconstriction in obese adolescents. Eur J Appl Physiol. doi:10.1007/s00421-012-2459-9
Gharib N, Rasheed P (2011) Energy and macronutrient intake and dietary pattern among school children in Bahrain: a cross-sectional study. Nutr J 10:62. doi:10.1186/1475-2891-10-62
Gopaul NK, Anggard EE, Mallet AI, Betteridge DJ, Wolff SP, Nourooz-Zadeh J (1995) Plasma 8-epi-PGF2 alpha levels are elevated in individuals with noninsulin-dependent diabetes mellitus. FEBS Lett 368(2):225–229
Halvorsen BL, Carlsen MH, Phillips KM, Bohn SK, Holte K, Jacobs DR Jr, Blomhoff R (2006) Content of redox-active compounds (i.e., antioxidants) in foods consumed in the United States. Am J Clin Nutr 84(1):95–135
Halvorsen BL, Holte K, Myhrstad MC, Barikmo I, Hvattum E, Remberg SF, Wold AB, Haffner K, Baugerod H, Andersen LF, Moskaug O, Jacobs DR Jr, Blomhoff R (2002) A systematic screening of total antioxidants in dietary plants. J Nutr 132(3):461–471
Ruiz H, de Eguílaz M, Pérez-Diez S, Navas-Carretero S, Martínez J (2010) Comparative study of body composition measures by dual X-ray absorptiometry, bioimpedance, and skinfolds in women. An R Acad Nac Farm 76(2):209–222
Kelly AS, Steinberger J, Kaiser DR, Olson TP, Bank AJ, Dengel DR (2006) Oxidative stress and adverse adipokine profile characterize the metabolic syndrome in children. J Cardiometab Syndr 1(4):248–252
Koletzko B, Dokoupil K, Reitmayr S, Weimert-Harendza B, Keller E (2000) Dietary fat intakes in infants and primary school children in Germany. Am J Clin Nutr 72(5 Suppl):1392S–1398S
Marques M, Moleres A, Rendo-Urteaga T, Gomez-Martinez S, Zapatera B, Romero P, de Miguel-Etayo P, Campoy C, Alfredo Martinez J, Azcona-San Julian C, Marcos A, Marti A, Warnberg J (2012) Design of the nutritional therapy for overweight and obese Spanish adolescents conducted by registered dieticians: the EVASYON study. Nutr Hosp 27(1):165–176. doi:10.1590/S0212-16112012000100020
Martin-Moreno JM, Boyle P, Gorgojo L, Maisonneuve P, Fernandez-Rodriguez JC, Salvini S, Willett WC (1993) Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol 22(3):512–519
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Melissas J, Malliaraki N, Papadakis JA, Taflampas P, Kampa M, Castanas E (2006) Plasma antioxidant capacity in morbidly obese patients before and after weight loss. Obes Surg 16(3):314–320. doi:10.1381/096089206776116444
Meydani M, Hasan ST (2010) Dietary polyphenols and obesity. Nutrients 2(7):737–751. doi:10.3390/nu2070737
Mohn A, Catino M, Capanna R, Giannini C, Marcovecchio M, Chiarelli F (2005) Increased oxidative stress in prepubertal severely obese children: effect of a dietary restriction-weight loss program. J Clin Endocrinol Metab 90(5):2653–2658. doi:10.1210/jc.2004-2178
Moleres A, Rendo-Urteaga T, Azcona C, Martinez JA, Gomez-Martinez S, Ruiz JR, Moreno LA, Marcos A, Marti A (2009) Il6 gene promoter polymorphism (-174G/C) influences the association between fat mass and cardiovascular risk factors. J Physiol Biochem 65(4):405–413. doi:10.1007/BF03185936
Molnar D, Decsi T, Koletzko B (2004) Reduced antioxidant status in obese children with multimetabolic syndrome. Int J Obes Relat Metab Disord 28(10):1197–1202. doi:10.1038/sj.ijo.0802719
Moreno LA, Fleta J, Mur L, Feja C, Sarria A, Bueno M (1997) Indices of body fat distribution in Spanish children aged 4.0 to 14.9 years. J Pediatr Gastroenterol Nutr 25(2):175–181
Moreno LA, Ochoa MC, Warnberg J, Marti A, Martinez JA, Marcos A (2008) Treatment of obesity in children and adolescents. How nutrition can work? Int J Pediatr Obes 3(Suppl 1):72–77. doi:10.1080/17477160801897158
Ochoa MC, Moreno-Aliaga MJ, Martinez-Gonzalez MA, Martinez JA, Marti A (2007) Predictor factors for childhood obesity in a Spanish case–control study. Nutrition 23(5):379–384. doi:10.1016/j.nut.2007.02.004
Pellegrini N, Salvatore S, Valtuena S, Bedogni G, Porrini M, Pala V, Del Rio D, Sieri S, Miglio C, Krogh V, Zavaroni I, Brighenti F (2007) Development and validation of a food frequency questionnaire for the assessment of dietary total antioxidant capacity. J Nutr 137(1):93–98
Pellegrini N, Serafini M, Colombi B, Del Rio D, Salvatore S, Bianchi M, Brighenti F (2003) Total antioxidant capacity of plant foods, beverages, and oils consumed in Italy assessed by three different in vitro assays. J Nutr 133(9):2812–2819
Pellegrini N, Serafini M, Salvatore S, Del Rio D, Bianchi M, Brighenti F (2006) Total antioxidant capacity of spices, dried fruits, nuts, pulses, cereals, and sweets consumed in Italy assessed by three different in vitro assays. Mol Nutr Food Res 50(11):1030–1038. doi:10.1002/mnfr.200600067
Puchau B, Ochoa MC, Zulet MA, Marti A, Martinez JA, Members G (2010) Dietary total antioxidant capacity and obesity in children and adolescents. Int J Food Sci Nutr 61(7):713–721. doi:10.3109/09637481003757860
Puchau B, Zulet MA, de Echavarri AG, Hermsdorff HH, Martinez JA (2009) Dietary total antioxidant capacity: a novel indicator of diet quality in healthy young adults. J Am Coll Nutr 28(6):648–656
Puchau B, Zulet MA, de Echavarri AG, Hermsdorff HH, Martinez JA (2010) Dietary total antioxidant capacity is negatively associated with some metabolic syndrome features in healthy young adults. Nutrition 26(5):534–541. doi:10.1016/j.nut.2009.06.017
Puchau B, Zulet MA, Gonzalez de Echavarri A, Navarro-Blasco I, Martinez JA (2009) Selenium intake reduces serum C3, an early marker of metabolic syndrome manifestations, in healthy young adults. Eur J Clin Nutr 63(7):858–864. doi:10.1038/ejcn.2008.48
Puchau B, Zulet MA, Urtiaga G, Navarro-Blasco I, Martinez JA (2009) Asymmetric dimethylarginine association with antioxidants intake in healthy young adults: a role as an indicator of metabolic syndrome features. Metabolism 58(10):1483–1488. doi:10.1016/j.metabol.2009.04.037
Rautiainen S, Serafini M, Morgenstern R, Prior RL, Wolk A (2008) The validity and reproducibility of food-frequency questionnaire-based total antioxidant capacity estimates in Swedish women. Am J Clin Nutr 87(5):1247–1253
Reinehr T, Kleber M, Toschke AM (2009) Lifestyle intervention in obese children is associated with a decrease of the metabolic syndrome prevalence. Atherosclerosis 207(1):174–180. doi:10.1016/j.atherosclerosis.2009.03.041
Rendo-Urteaga T, Garcia-Calzon S, Martinez-Anso E, Chueca M, Oyarzabal M, Azcona-Sanjulian MC, Bustos M, Moreno-Aliaga MJ, Martinez JA, Marti A (2013) Decreased cardiotrophin-1 levels are associated with a lower risk of developing the metabolic syndrome in overweight/obese children after a weight loss program. Metabolism 62(10):1429–1436. doi:10.1016/j.metabol.2013.05.011
Salvatore S, Pellegrini N, Brenna OV, Del Rio D, Frasca G, Brighenti F, Tumino R (2005) Antioxidant characterization of some Sicilian edible wild greens. J Agric Food Chem 53(24):9465–9471. doi:10.1021/jf051806r
Sanchez-Villegas A, Ara I, Dierssen T, de la Fuente C, Ruano C, Martinez-Gonzalez MA (2012) Physical activity during leisure time and quality of life in a Spanish cohort: SUN (Seguimiento Universidad de Navarra) project. Br J Sports Med 46(6):443–448. doi:10.1136/bjsm.2010.081836
Schofield WN (1985) Predicting basal metabolic rate, new standards, and review of previous work. Hum Nutr Clin Nutr 39(Suppl 1):5–41
Serafini M, Del Rio D (2004) Understanding the association between dietary antioxidants, redox status, and disease: is the total antioxidant capacity the right tool? Redox Rep 9(3):145–152. doi:10.1179/135100004225004814
Sinaiko AR, Steinberger J, Moran A, Prineas RJ, Vessby B, Basu S, Tracy R, Jacobs DR Jr (2005) Relation of body mass index and insulin resistance to cardiovascular risk factors, inflammatory factors, and oxidative stress during adolescence. Circulation 111(15):1985–1991. doi:10.1161/01.CIR.0000161837.23846.57
Tanner JM, Whitehouse RH (1976) Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child 51(3):170–179
Thompson HJ, Heimendinger J, Sedlacek S, Haegele A, Diker A, O’Neill C, Meinecke B, Wolfe P, Zhu Z, Jiang W (2005) 8-Isoprostane F2alpha excretion is reduced in women by increased vegetable and fruit intake. Am J Clin Nutr 82(4):768–776
Tsai IJ, Croft KD, Mori TA, Falck JR, Beilin LJ, Puddey IB, Barden AE (2009) 20-HETE and F2-isoprostanes in the metabolic syndrome: the effect of weight reduction. Free Radic Biol Med 46(2):263–270. doi:10.1016/j.freeradbiomed.2008.10.028
Urakawa H, Katsuki A, Sumida Y, Gabazza EC, Murashima S, Morioka K, Maruyama N, Kitagawa N, Tanaka T, Hori Y, Nakatani K, Yano Y, Adachi Y (2003) Oxidative stress is associated with adiposity and insulin resistance in men. J Clin Endocrinol Metab 88(10):4673–4676
Waling M, Lind T, Hernell O, Larsson C (2010) A 1-year intervention has modest effects on energy and macronutrient intakes of overweight and obese Swedish children. J Nutr 140(10):1793–1798. doi:10.3945/jn.110.125435
Weker H (2006) Simple obesity in children. A study on the role of nutritional factors. Med Wieku Rozwoj 10(1):3–191
Acknowledgments
We thank the children and their parents for their participation in this study. Research relating to this article was funded by grants from the Navarra Government, Departamento de Salud (grant PI 54/2009), Linea Especial, Nutrición y Obesidad (University of Navarra), Carlos III Health Institute (CIBER project, CB06/03/1017). The scholarships to T. Rendo-Urteaga from the Asociación de Amigos de la Universidad de Navarra is fully acknowledged. The proofreading of the final version by Massimiliano Marinoni is gratefully acknowledged.
Disclosure statement
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rendo-Urteaga, T., Puchau, B., Chueca, M. et al. Total antioxidant capacity and oxidative stress after a 10-week dietary intervention program in obese children. Eur J Pediatr 173, 609–616 (2014). https://doi.org/10.1007/s00431-013-2229-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-013-2229-7