Abstract
Primary ciliary dyskinesia (PCD) is an inherited disease related to ciliary dysfunction, with heterogeneity in clinical presentation and in ciliary ultrastructural defect. Our study intended to determine if there are phenotypic differences in patients with PCD based on ciliary ultrastructural abnormality. In this retrospective study carried out among 60 children with a definitive diagnosis of PCD, we analyzed clinical, radiological, and functional features at diagnosis and at last recorded visit, according to cilia defect (absence of dynein arms: DAD group, n = 36; abnormalities of the central complex: CCA group, n = 24). Onset of respiratory symptoms occurred later in the CCA than in the DAD group (9.5 versus 0.5 months, p = 0.03). Situs inversus was only observed in the DAD group, while respiratory disease in siblings were more frequent in the CCA group (p = 0.003). At diagnosis, clinical presentation was more severe in the CCA group: frequency of respiratory tract infections (p = 0.008), rhinosinusitis (p = 0.02), otitis complications (p = 0.0001), bilateral bronchiectasis (p = 0.04), and number of hypoxemic patients (p = 0.03). Pulmonary function remained stable in both groups, but outcome was better in the CCA than in the DAD group: less antibiotic therapy and hypoxemic patients (p = 0.004). In conclusion, our results underlined the relationship between the severity of clinical presentation and the ultrastructural ciliary defect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary ciliary dyskinesia (PCD) is an inherited respiratory disease, related to defective ciliary structure and function [1]. Ciliary dysfunction is responsible for impaired mucociliary transport leading to chronic respiratory tract infections usually beginning in the first year of life. PCD is classically considered as a rare disease with reported prevalence of diagnosed cases in 5–14-year-olds between 1/10,000 and 1/20,000 in European countries [5, 23].
In children with recurrent respiratory infections, PCD is naturally more common and might account for up to 5 % [9]. In the presence of a suggestive clinical presentation, functional and structural analyses of respiratory cilia are therefore justified and may confirm the diagnosis of PCD in case of specific axonemal defects [2, 7, 29, 30].
The axoneme, core of the motile cilium, includes nine peripheral microtubules with attached dynein arms and radial spokes, around the central complex composed of two single microtubules surrounded by the central sheath [1, 4]. The earliest and commonest axonemal defect in PCD patients concerns dynein arms essential for ciliary motion. Less frequently, abnormalities of the central complex, sometimes named central microtubular agenesis [31], have been reported in PCD patients [3, 10, 17, 31–33]. In fact, these various axonemal defects reflect the genetic heterogeneity of PCD [1] and may explain at least in part differences in term of severity observed between patients.
In the literature, the relationship between PCD presentation and specific ciliary defects has been rarely analyzed, especially in large series exclusively composed of children [11, 12, 22, 26, 33]. The present retrospective study has been carried out among a large cohort of 60 children with a definitive diagnosis of PCD, in whom we intended to determine if the clinical, radiological, and functional features of the disease could differ according to the defect of their respiratory cilia concerning either dynein arms or central complex.
Patients and methods
Patients
In the pediatric respiratory department of Trousseau Hospital (Paris), ciliary investigations are part of the diagnostic procedures in children with recurrent respiratory tract infections (i.e., occurring more than once a month for at least six consecutive months), since 1985 [9, 17, 33]. Our study population consisted of 60 children with a definitive diagnosis of PCD made by the association of suggestive clinical symptoms (i.e., recurrent upper and lower respiratory tract infections), typical axonemal defects concerning either the dynein arms or the central complex associated, and dyskinetic and/or immotile cilia. All known pathologic conditions, such as cystic fibrosis or immunodeficiency, were excluded in these children. The patients and/or their parents were informed of the exact nature and the goal of the investigations and gave their written informed consent. All evaluation and investigations were performed when patients have been free of symptomatic airway tract infection or respiratory exacerbation (i.e., increase in or new onset of more than one pulmonary symptom, such as cough, sputum volume and/or purulence, dyspnea, requiring treatment with antibiotic) for at least 6 weeks.
First evaluation at diagnosis
Family history of PCD in siblings and familial consanguinity were recorded at the first visit. Patient history was reviewed for unexplained neonatal respiratory distress, age of onset of respiratory symptoms, and frequency of airway infections since birth. Sinus symptoms (mucopurulent rhinosinusitis, nasal polyposis) and chronic otitis media (requiring ventilation tubes, complicated otitis) were recorded.
Chest X-ray and computerized tomography (CT) scan were performed at diagnosis in all cases. Situs inversus was noted on chest radiograph. The presence of bronchiectasis was assessed on CT scan, and its topography was classified as unilateral or bilateral.
In children older than 5 years of age, spirometry was performed according to the ATS/ERS recommendations [25], using a Masterscreen (Jaeger Ltd, Hoechberg, Germany) by fully trained pediatric respiratory technicians. At least three curves reproducible for forced vital capacity and forced expiratory volume in 1 s (FEV1) were recorded, and the best curve was retained for analysis. Functional residual capacity (FRC) was measured using the helium dilution technique (Spirometer 5500, Exp’Air software, Medisoft Ltd, Sorinnes, Belgium). Results were expressed as a percentage of the predicted value for height and age. Volumes and flows were considered as normal when >80 % of the expected value [36].
Similarly to the management of cystic fibrosis patients, arterialized capillary blood gases were regularly determined in all patients to look for hypoxemia, using a non-invasive method used since long in our laboratory. Arterialized capillary blood gases were measured using an ABL800 Flex Radiometer (Copenhagen Ltd, Denmark). Hypoxemia was defined as a value of PaO2 below the lower limit of normality defined as 2 standard deviations below predicted measured in age-matched healthy children [19] .
Evaluation at last recorded visit
Patients were reviewed by pediatric respiratory specialists at least every 6 months in our institution. During the study period, children were prescribed standard aggressive treatment, including airway clearance with physiotherapy, oral or rarely intravenous antibiotic therapy, depending on the nature and frequency of bacterial isolates. In the absence of any validated protocols, the decision of prophylactic antibiotic therapy was based on a clinical assessment of the severity, frequency, and duration of exacerbations.
Each year, the frequency of airway infections was evaluated as well as the antibiotic need (no need for antibiotic therapy, intermittent or continuous antibiotic therapy). Continuous antibiotic therapy could be stopped in the absence of exacerbation for more than 6 months. The presence of bronchiectasis was evaluated by CT scan every 3 to 5 years, depending on the severity of the symptoms and/or the decline of respiratory function. Bronchiectasis was classified as stable or progressive (i.e., increasing diameter and/or extension to a new segment). Radiological deterioration was defined as the extension of bronchiectasis. Each year, upper respiratory tract symptoms were assessed by the occurrence of rhinosinusitis and otitis (absent, controlled, or not by antibiotherapy). Otitis complications were defined as the need for ventilation tubes during more than 1.5 year, and sinus complications were defined as the persistence of mucopurulent nasal discharge despite continuous antibiotic therapy or the need of sinus surgery.
A high frequency of respiratory tract infections, otitis and rhinosinusitis complications, bilateral or progressive bronchiectasis, presence of hypoxemia, or the need for continuous antibiotherapy were all considered as criteria of severity. We compared the clinical, radiological, and functional parameters collected during the last recorded visit to those of the first evaluation at diagnosis.
Ciliary ultrastructure and beat frequency
Biopsies were obtained from either the inferior turbinate or the bronchi and processed for ciliary investigations as described previously [33, 34]. Airway biopsies were immersed in glutaraldehyde and processed as usual for ultrastructural analysis as previously described [17, 33]. A cutoff value of >15 % of abnormal cilia was considered to be abnormal. Axonemal abnormalities were expressed as a percentage of each ultrastructural defect among the total number of abnormal cilia. Dynein arms were considered to be absent from sections when the structure was missing from at least six of the nine peripheral doublets. For questionable inner dynein arms in micrographs obtained by transmission electron microscopy, computerized analysis of cilia was systematically performed to improve inner dynein arm visualization, as previously reported [18]. In cases of abnormalities of the central complex (absence of central pair without axonemal disorganization, i.e., central microtubular agenesis [31]), the axonemal defect was confirmed by repeated ciliary biopsy performed at least 6 months later, during a stable period, and when possible at an another airway level (i.e., nasal versus bronchial sampling), in order to exclude a transient acquired ciliary defect.
For ciliary beat frequency (CBF) evaluation, the respiratory cells obtained by brushing were suspended in Menezo’s B2 medium, and the sample was examined as previously described [11, 33]. When only immotile cilia were observed, CBF was considered to be 0 Hz.
Statistical analysis
Results were expressed as medians and interquartile range (IQR) or percentages when appropriate. Comparisons between groups used Mann–Whitney non-parametric test for quantitative data and chi-square test or Fisher’s exact test where appropriate for categorical data. All tests were two-tailed and p values of less than 0.05 were considered significant. All analyses were performed using SPSS V.12.
Results
Patient characteristics
The 60 patients (29 boys, 31 girls, aged 0–15 years) of the study population belonged to 53 unrelated families, including 14 consanguineous families. This population was divided into two groups according to the ciliary ultrastructural results.
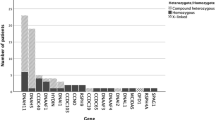
The group of patients with dynein arm defects (DAD group) consisted of 36 patients from 33 families (15 boys, 21 girls, age 0–15 years). In this group, all cilia were abnormal with the defect in outer dynein arms alone (n = 15) (Fig. 1b), of inner dynein arms with axonemal disorganization (n = 10) (Fig. 1c), or of both dynein arms (n = 11) (Fig. 1d). In all cases of absence of inner dynein arms, the ultrastructural defect was confirmed by a repeated ciliary biopsy as recommended [28]. CBF, measured in 35 of 36 patients, showed totally immotile cilia in all but two patients of whom one had an absence in both dynein arms and very slow CBF and the other had an absence of inner dynein arms with normal CBF but with a stiff flickering beat pattern (Fig. 2).
Ultrastructural defects of respiratory cilia (bars = 0.1 mm). a Cross section of cilia showing the “9 + 2” microtubule doublet configuration with presence of dynein arms. b Absence of outer dynein arms alone. c Absence of inner dynein arms with axonemal disorganization. d Absence of both dynein arms. e Absence of central complex
Results of ciliary beat frequency (CBF) according to the percentage of abnormal cilia and to the type of ciliary defects. The dotted line indicates the limit of normal CBF (>8 Hz). Circles indicate patients belonging to the CCA group. Squares indicate the two patients belonging to the DAD group: with reduced CBF for the patient with absence of both dynein arms; normal CBF for the patient with absence of inner dynein arms. The 33 patients of the DAD group with immotile cilia are not represented on this figure. Gray symbols indicate the children with neonatal respiratory distress, and hatched symbols indicate patients requiring continuous antibiotic therapy
The group of patients with abnormalities of the central complex (CCA group) included 24 patients from 20 families (14 boys, 10 girls, aged 1–12 years). Twelve patients of the CCA group had previously been reported in a study evaluating the outcome of patients with partial ciliary defects [33]. In all cases, the abnormalities of the central complex were confirmed by repeated ciliary biopsy. In this group, the dynein arms were present and the ciliary defect never concerned all the cilia, as already reported [11, 29, 33]. For six patients, the movement of some cilia appeared abnormal, but the CBF was within normal range. The CBF was reduced in seven patients, and 11 patients showed immotile cilia (Fig. 2).
Clinical, radiological, and functional parameters collected at diagnosis and at the most recent visit were compared between the two groups (Tables 1 and 2). Sex ratio (male/female) was not different between the two groups (0.7 and 1.4 for the DAD and the CCA group, respectively, p = 0.21).
Evaluation at diagnosis (Table 1)
For the population as a whole, median age at diagnosis was 6 (3–11) years and was similar in the two groups. The incidence of neonatal respiratory distress was lower in the CCA group than in the DAD group (six of 24 and 18 of 36, respectively), but the difference was not significant. The median age of onset of respiratory symptoms was significantly higher in the CCA group than in the DAD group (9.5 versus 0.5 months, p = 0.03). Situs inversus was only observed in the DAD group while respiratory disease in siblings was more common in the CCA group than in the DAD group (11 of 20 versus five of 33 families, p = 0.003). For five and two families from the CCA and DAD groups, respectively, the respiratory disease in siblings corresponded to PCD confirmed by TEM.
At diagnosis, the clinical presentation was more severe in the CCA group than in the DAD group, regarding frequency of lower respiratory tract infections (p = 0.008), of rhinosinusitis (p = 0.02), and of otitis media complications (p = 0.0001). The incidence of bronchiectasis was frequent and similar in the two groups, but bronchiectasis were more frequently bilateral in the CC group (p = 0.04).
For the population as a whole, the first pulmonary function test was performed at a median age of 6 (3–11) years, and values were similar in the two groups (Table 2). The median arterialized capillary partial pressure of oxygen was in the normal range in the two groups; however, more patients were hypoxemic in the CCA group compared to the DAD group (ten of 24 and six of 36 of patients, respectively, p = 0.03) but not severe enough for requiring supplemental oxygen. Mean FRC was within the normal range in the two groups; however, 14 patients had pulmonary hyperinflation with no difference between the two groups. Median FEV1 was within the normal range in the two groups; however, 24 patients had FEV1 < 80 % of the predicted values, with no difference between the two groups.
Evaluation at last recorded visit
For the population as a whole, the median duration of follow-up was 5 (3–8) years (range from 1 to 17 years) and was similar in the two groups (Table 1). During the study period, all patients of the DAD group required antibiotic therapy (with continuous treatment in 28 of 36 of the cases) while antibiotic therapy could be stopped in six of 24 of the patients of the CCA group (p = 0.003). The incidence and severity of ear–nasal–throat symptoms, and radiological deterioration (patients with extension of bronchiectasis) were similar between the two groups.
The most recent pulmonary function tests were performed at similar mean age in the two groups (Table 2). For the population as a whole, the pulmonary function remained within the normal ranges. At last recorded visit, the ten hypoxemic patients all belonged to the DAD group (p = 0.004). Moreover, in the DAD group, the number of patients with bronchial obstruction increased (from 15 to 20) and was higher than that of the CCA group. Interestingly, we noted that all the patients with bronchial obstruction at first evaluation still had abnormal FEV1 at the last recorded visit (eight of eight in the DAD group and four of four in the CCA group). No relationship was observed within the DAD group between the type of dynein arm defects (i.e., involving outer, inner or both dynein arms) and the PCD presentation (data not shown).
Discussion
This study is the first to show a relationship between the ciliary ultrastructural defect and the PCD phenotype. Even though the clinical presentation at diagnosis was more severe in patients with abnormalities of the central complex, children with absence of dynein arms experienced a more severe upper and lower airway course of disease.
The ultrastructural defects underlying PCD have been mostly described in mixed populations of adults and children [7, 27, 29]. In this large pediatric series, the most frequent ultrastructural defect concerns dynein arms, mainly the outer one (43.3 % in our study; 60 to 75 % in other series), whereas the absence of the inner dynein arms alone is less frequent (16.7 % in our study; 13 to 53 % in other series) [3, 11, 22, 27]. As reported in the literature and in the present study, only the absence of dynein arms was associated with immotile cilia except in two patients [11, 14, 22, 27]. It must be noted that in the DAD group, different subclasses of dynein deficiencies caused by mutations in different genes are lumped, perhaps leading to differences in the phenotypic expression.
Besides the classical absence of dynein arms, we found numerous defects of the central complex. Absence of the central complex without axonemal disorganization has already been reported in patients with PCD, but is not associated with situs inversus [11, 14, 29, 31, 33]. In the CCA group, the high incidence of affected siblings with PCD diagnosis confirmed by TEM supports the constitutional nature of this defect, as suggested by similar abnormalities of the central microtubules described in human spermatozoa, Chlamydomonas, and mice mutants [15, 21]. Finally, as RSPH4A and RSPH9 mutations have been reported in some families with a PCD phenotype characterized by abnormalities of the central pair [8, 37], we analyzed this gene in seven unrelated families (11 patients) of the CCA group for which DNA samples were available; the identification of RSPH4A and RSPH9 mutations (in three and one families, respectively) clearly demonstrated the inherited origin of this ultrastructural defect (unpublished data). In the CCA group, cilia were motile in about half of the children, resulting in a difficult assert diagnosis. Using high-speed videomicroscopy, abnormalities of the central complex have been shown to result in an abnormal circular movement of the cilium as opposed to the typical forward and backward motion [11, 30, 31]. Unfortunately, at the time of the study, this technology as well as nasal nitric oxide measurement that have been found to allow distinguish between PCD and non-PCD patients or healthy subjects [2, 6, 35] were not available in our laboratory.
At diagnosis, children of both groups had respiratory symptoms developed early in life with a high incidence of neonatal respiratory distress. The current study supports the hypothesis [3, 12, 13, 22] that neonatal respiratory distress is related to cilia immobility in the CCA group (Fig. 2), which suggests the important role of cilia not only for mucus transport but also for clearing alveolar liquid fluid during the first hours of life.
Despite the presence of respiratory symptoms during the first year of life, the diagnosis of PCD is often delayed, especially in the absence of situs inversus. In our series, a situs inversus was only present in about one third of patients from the DAD group and, as expected, was never observed in the CCA group [6, 11, 22, 27]. In the absence of situs inversus, the diagnosis of PCD might be suspected in more symptomatic patients. As the age of diagnosis did not depend on ciliary defect, we presume that the severity of the respiratory symptoms probably leads to the diagnosis of PCD in the patients of the CCA group. Bronchiectasis was present at diagnosis in most of the children and bilateral in almost half of the children of the CCA group. In the literature, the frequency of bronchiectasis varies from 20 to 100 % of the cases [3, 12, 22, 27] according to the age of the patients [22, 27] or the radiology.
In contrast with the high frequency of lower airway infections, pulmonary function remained stable in most of the patients of the two groups, as observed in adults [3, 13, 16, 20]. However, about half of the children showed a mild airway obstruction at first evaluation and persistent at last recorded visit in the two groups. Our results confirm the early alteration in lung function in PCD [24]. We observed no relationship between the severity of airway obstruction and the underlying ultrastructural defect, the incidence of respiratory infections, or the extension of bronchiectasis (data not shown). Whatever the group, it would be interesting to determine if children with persistent obstruction will have a more severe disease in adulthood, defined as a FEV1 below 40 % as found in 25 % of adults with PCD [27].
At diagnosis, most of the hypoxemic patients belonged to the CCA group. During the follow-up, all the children of the DAD group required antibiotic therapy, and hypoxemia was present only in children belonging to the DAD group. It is therefore tempting to speculate that hypoxemic children from the DAD group (ten of 36) may evolve toward a more severe adult phenotype (concerning about 25 % of the patients) [27] justifying therefore an aggressive therapeutic management.
Most importantly, we observed a relationship between the severity of the clinical presentation and the ciliary ultrastructural defect. Initially, the clinical presentation of the patients with abnormalities of the central complex was more severe in term of high frequency of respiratory tract infections, otitis and rhinosinusitis complications, bilateral bronchiectasis, hypoxemia, and continuous antibiotic therapy. In contrast, during the study period, patients of the CCA group greatly improved (including four of six patients with identified mutations) while a significant proportion of patients with absence of dynein arms experiments a more severe clinical course. The difference in PCD presentation may be explained by a different mechanism of airway damage. In cases of absence of dynein arms, as the cilia are immotile, the absence of mucociliary clearance leads to mucus stagnation with proliferation of bacteria and airway infection, which translates into pulmonary tissue destruction. In cases of abnormalities of the central complex, tissue damages occur rapidly, as judged on the early onset of bilateral bronchiectasis, whereas ciliary motility may be preserved in those patients. This suggests that the molecular defect responsible for the abnormality of the central complex could affect lung maturation and/or airway defenses through other mechanisms than the sole ciliary beating dysfunction.
Conclusion
The present study provides information that could help to orientate the diagnosis and prognosis of PCD. The relationship between the severity of the clinical presentation and the ultrastructural ciliary defect showed in our study may be of a significant importance in diagnosis, management, and future clinical studies. However, the variability of severity observed in PCD might be also due to differences in treatment compliance, environmental factors, and/or modifier genes expression.
References
Afzelius BA (1976) A human syndrome caused by immotile cilia. Science 193:317–9
Barbato A, Frischer T, Kuehni CE, Snijders D, Azevedo I, Baktai G, Bartoloni L, Eber E, Escribano A, Haarman E, Hesselmar B, Hogg C, Jorissen M, Lucas J, Nielsen KG, O’Callaghan C, Omran H, Pohunek P, Strippoli MP, Bush A (2009) Primary ciliary dyskinesia: a consensus statement on diagnostic and treatment approaches in children. Eur Respir J 34:1264–76
Barlocco EG, Valletta EA, Canciani M, Lungarella G, Gardi C, De Santi MM, Mastella G (1991) Ultrastructural ciliary defects in children with recurrent infections of the lower respiratory tract. Pediatr Pulmonol 10:11–7
Bergmann C (2012) Educational paper: ciliopathies. Eur J Pediatr 171(9):1285–1300
Boon M, Jorissen M, Proesmans M, De Boeck K (2013) Primary ciliary dyskinesia, an orphan disease. Eur J Pediatr 172(2):151–162
Bush A, Chodhari R, Collins N, Copeland F, Hall P, Harcourt J, Hariri M, Hogg C, Lucas J, Mitchison HM, O’Callaghan C, Phillips G (2007) Primary ciliary dyskinesia: current state of the art. Arch Dis Child 92:1136–40
Bush A, Cole P, Hariri M, Mackay I, Phillips G, O’Callaghan C, Wilson R, Warner JO (1998) Primary ciliary dyskinesia: diagnosis and standards of care. Eur Respir J 12:982–8
Castleman VH, Romio L, Chodhari R, Hirst RA, de Castro SC, Parker KA, Ybot-Gonzalez P, Emes RD, Wilson SW, Wallis C, Johnson CA, Herrera RJ, Rutman A, Dixon M, Shoemark A, Bush A, Hogg C, Gardiner RM, Reish O, Greene ND, O’Callaghan C, Purton S, Chung EM, Mitchison HM (2009) Mutations in radial spoke head protein genes RSPH9 and RSPH4A cause primary ciliary dyskinesia with central-microtubular-pair abnormalities. Am J Hum Genet 84(2):197–209
Chapelin C, Coste A, Reinert P, Boucherat M, Millepied MC, Poron F, Escudier E (1997) Incidence of primary ciliary dyskinesia in children with recurrent respiratory diseases. Ann Otol Rhinol Laryngol 106:854–8
Chilvers MA, Rutman A, O’Callaghan C (2003) Functional analysis of cilia and ciliated epithelial ultrastructure in healthy children and young adults. Thorax 58:333–8
Chilvers MA, Rutman A, O’Callaghan C (2003) Ciliary beat pattern is associated with specific ultrastructural defects in primary ciliary dyskinesia. J Allergy Clin Immunol 112:518–24
Coren ME, Meeks M, Morrison I, Buchdahl RM, Bush A (2002) Primary ciliary dyskinesia: age at diagnosis and symptom history. Acta Paediatr 91:667–9
Corkey CW, Levison H, Turner JA (1981) The immotile cilia syndrome. A longitudinal survey. Am Rev Respir Dis 124(5):544–548
De Iongh RU, Rutland J (1995) Ciliary defects in healthy subjects, bronchiectasis, and primary ciliary dyskinesia. Am J Respir Crit Care Med 151:1559–67
El Zein L, Omran H, Bouvagnet P (2003) Lateralization defects and ciliary dyskinesia: lessons from algae. Trends Genet 19:162–7
Ellerman A, Bisgaard H (1997) Longitudinal study of lung function in a cohort of primary ciliary dyskinesia. Eur Respir J 10:2376–9
Escalier D, Jouannet P, David G (1982) Abnormalities of the ciliary axonemal complex in children: an ultrastructural and cinetic study in a series of 34 cases. Biol Cell 44:271–282
Escudier E, Couprie M, Duriez B, Roudot-Thoraval F, Millepied MC, Pruliere-Escabasse V, Labatte L, Coste A (2002) Computer-assisted analysis helps detect inner dynein arm abnormalities. Am J Respir Crit Care Med 166:1257–62
Gaultier C, Boulé M, Allaire Y, Clément A, Buvry A, Girard F (1979) Determination of capillary oxygen tension in infants and children: assessment of methodology and normal values during growth. Bull Eur Physiopathol Respir 14(3):287–297
Hellinckx J, Demedts M, De Boeck K (1998) Primary ciliary dyskinesia: evolution of pulmonary function. Eur J Pediatr 157:422–6
Huang B, Piperno G, Luck DJ (1979) Paralyzed flagella mutants of Chlamydomonas reinhardtii. Defective for axonemal doublet microtubule arms. J Biol Chem 254(8):3091–3099
Jain K, Padley SP, Goldstraw EJ, Kidd SJ, Hogg C, Biggart E, Bush A (2007) Primary ciliary dyskinesia in the paediatric population: range and severity of radiological findings in a cohort of patients receiving tertiary care. Clin Radiol 62:986–93
Kuehni CE, Frischer T, Strippoli M-PF, Maurer E, Bush A, Nielsen KG, Escribano A, Lucas JS, Yiallouros P, Omran H, Eber E, O’Callaghan C, Snijders D, Barbato A (2010) Factors influencing age at diagnosis of primary ciliary dyskinesia in European children. Eur Respir J 36(6):1248–1258
Marthin JK, Petersen N, Skovgaard LT, Nielsen KG (2010) Lung function in patients with primary ciliary dyskinesia. A cross sectional and three-decade longitudinal study. Am J Respir Crit Care Med 181(11):1262–1268
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338
Min YG, Shin JS, Choi SH, Chi JG, Yoon CJ (1995) Primary ciliary dyskinesia: ultrastructural defects and clinical features. Rhinology 33:189–93
Noone PG, Leigh MW, Sannuti A, Minnix SL, Carson JL, Hazucha M, Zariwala MA, Knowles MR (2004) Primary ciliary dyskinesia: diagnostic and phenotypic features. Am J Respir Crit Care Med 169:459–67
O’Callaghan C, Rutman A, Williams GM, Hirst RA (2011) Inner dynein arm defects causing primary ciliary dyskinesia: repeat testing required. Eur Respir J 38(3):603–607
Papon JF, Coste A, Roudot-Thoraval F, Boucherat M, Roger G, Tamalet A, Vojtek AM, Amselem S, Escudier E (2010) A 20-year experience of electron microscopy in the diagnosis of primary ciliary dyskinesia. Eur Respir J 35(5):1057–1063
Stannard WA, Chilvers MA, Rutman AR, Williams CD, O’Callaghan C (2010) Diagnostic testing of patients suspected of primary ciliary dyskinesia. Am J Respir Crit Care Med 181:307–14
Stannard W, Rutman A, Wallis C, O’Callaghan C (2004) Central microtubular agenesis causing primary ciliary dyskinesia. Am J Respir Crit Care Med 169:634–7
Sturgess JM, Chao J, Turner JA (1980) Transposition of ciliary microtubules: another cause of impaired ciliary motility. N Engl J Med 303:318–22
Tamalet A, Clement A, Roudot-Thoraval F, Desmarquest P, Roger G, Boule M, Millepied MC, Baculard TA, Escudier E (2001) Abnormal central complex is a marker of severity in the presence of partial ciliary defect. Pediatrics 108:E86
Verra F, Fleury-Feith J, Boucherat M, Pinchon MC, Bignon J, Escudier E (1993) Do nasal ciliary changes reflect bronchial changes? An ultrastructural study. Am Rev Respir Dis 147(4):908–913
Wodehouse T, Kharitonov SA, Mackay IS, Barnes PJ, Wilson R, Cole PJ (2003) Nasal nitric oxide measurements for the screening of primary ciliary dyskinesia. Eur Respir J 21:43–7
Zapletal A, Samánek M, Paul T (1987) Lung function in children and adolescents: methods, reference values. Karger, Basel, pp 10–45
Ziętkiewicz E, Bukowy-Bieryłło Z, Voelkel K, Klimek B, Dmeńska H, Pogorzelski A, Sulikowska-Rowińska A, Rutkiewicz E, Witt M (2012) Mutations in radial spoke head genes and ultrastructural cilia defects in East-European cohort of primary ciliary dyskinesia patients. PLoS One 7(3):e33667
Acknowledgments
The authors are grateful to the children and their families who participated in this study and thank all referring physicians. This work was supported by grants from the Legs Poix from the Chancellerie des Universités, the Assistance Publique-Hôpitaux de Paris (PHRC AOM06053, P060245), the Milena Carvajal ProKartagener Foundation, and the Fondation pour la Recherche Médicale (DEQ20120323689).
Conflict of interest
All of the authors are aware and agree to the content of the paper and approve its submission. None of the authors have any financial relationship with commercial or other associations that might pose a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vallet, C., Escudier, E., Roudot-Thoraval, F. et al. Primary ciliary dyskinesia presentation in 60 children according to ciliary ultrastructure. Eur J Pediatr 172, 1053–1060 (2013). https://doi.org/10.1007/s00431-013-1996-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-013-1996-5