Abstract
Rickets remains a common problem among infants and children in many countries worldwide. Although the classical presentation associated with bone abnormalities is well known, paediatricians need to be aware of atypical presentations, especially in the first 6 months of life. Furthermore, although vitamin D deficiency rickets remains the commonest form of rickets in most countries, health care providers need to be aware of other possible causes and their typical clinical and biochemical presentations. This article discusses these and highlights the characteristic features of various forms of rickets and possible pitfalls clinicians should be aware of when confronted with a patient with suspected rickets. In conclusion, the recent advances made in understanding the underlying pathogeneses of the various forms of rickets has helped to delineate the diagnostic tests that assist in the diagnosis and management of the disease in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physicians worldwide need to be familiar with a diagnostic approach to the rachitic infant or child as nutritional rickets (vitamin D deficiency and calcium deficiency) is still prevalent or re-emergent in different parts of the world [15, 25], and the disease is prevalent among new immigrant populations in some countries where rickets traditionally had been combated [8, 17]. In addition, genetic causes are more prevalent in consanguineous communities and also communities where vitamin D fortication of foods is practised. An early diagnosis with proper treatment ensures an optimal outcome and minimises skeletal deformities, more so in cases of resistant rickets. The treatment of the rachitic infant in many situations is also rewarding as dramatic improvement ensues in a relatively short period of time. However, separating the easily treatable cases of nutritional rickets from the less easily treatable forms of resistant rickets may prove a challenge in specific instances. For example, the clinical and biochemical parameters may have been significantly altered by earlier treatment (e.g. by the use of vitamin D analogues, vitamin D or phosphate), and the patient referred only after a failure of therapy. Recognition of whether the patient falls into the calciopenic or phosphopenic category is of paramount importance, but not always easily recognisable (Table 1). Since pattern recognition is rarely useful, e.g. the presence of alopecia, which occurs in 50% of VDDR type 2 rickets or with secondary causes of rickets (e.g. liver disease with cholestasis), the cornerstone of diagnosis is a detailed history (nutritional, breastfeeding, sunlight exposure and family history), anthropometric measurements, skeletal examination and biochemical investigations of mineral homeostasis. The aim of this paper is to provide a practical and clinical approach to children with suspected rickets.
Case 1: nutritional rickets—failure to thrive
A 22-month-old female toddler with clinical rickets was referred from a peripheral hospital for evaluation. Growth percentiles revealed growth failure: weight-for-age (W/A) Z score of −4.04, height-for-age Z score (H/A) of −2.46 and weight-for-height (W/H) Z score of −2.54. She had been prescribed 3 months previously with alphacalcidol (1α-hydroxyvitamin D3) at a dose of 0.4 mcg daily, which was later increased to 0.8 mcg daily without clinical or biochemical healing. She was exclusively breastfeeding and had had poor weight gain since the age of 6 months. Parents were second cousins, and the mother was P7G7. No prior sibling had had rickets. Classic rachitic findings including bow legs, rachitic rosary, a wide open anterior fontanelle and a Harrison sulcus were present. On laboratory investigation, the toddler had a mild microcytic anaemia and a low serum vitamin B12. The relevant perturbations in biochemical assessment of mineral homeostasis are shown in Table 2. A radiograph of the left wrist documented classical features of rickets (Fig. 1).
The child was treated on vitamin D (ergocalciferol) 2,000 IU/day for 3 months and showed a rapid and complete response. Thus, a final diagnosis of severe vitamin D deficiency rickets in a breastfed infant, who had limited exposure to UVB radiation, was made.
Discussion
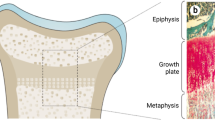
The toddler presented as a classical case of vitamin D deficiency rickets. Children with calciopenic rickets may have a normal or low calcium concentration depending on the stage of presentation of rickets and the compensatory parathyroid hormone (PTH) response [10]. Phosphate concentrations are typically decreased due to the phosphaturic response to an elevated PTH. Unlike children with calciopenic rickets, children with phosphopenic rickets typically have a low serum phosphate with normal calcium and PTH concentrations (Fig. 2).
Algorithm for the differential diagnosis of rickets and its different types. P phosphate; ALP alcaline phosphatase; Ca calcium; CRF chronic renal failure; ROD renal osteodystrophy; 25OHD 25 hydroxyvitamin D; TmP/GFR tubular maximum for phosphate corrected for glomerular filtration rate; 1,25-(OH) 2 D 1–25 dihydroxy vitamin D; FGF23 fibroblast growth factor 23, Ugluc glucosuria; Uprot proteinuria; Uca calciuria; VDDR vitamin-D-dependent rickets; XLH X-linked hypophosphataemic rickets; ADHR autosomal dominant hypophosphataemic rickets; ARHR autosomal recessive hypophosphataemic rickets; HHRH hereditary hypophosphataemic rickets with hypercalciuria; dRTA distal renal tubular acidosis
Clinical pointers to nutritional rickets in this child were exclusive breastfeeding (breastmilk contains the equivalent of approximately 40 IU/L vitamin D [11], as compared to infant milk formulas, which are fortified to 400 IU/L), associated iron deficiency and poor growth. Failure to thrive should also alert the physician to the possibility of renal tubular disorders, such a renal tubular acidosis or complex proximal renal tubular problems, such as Fanconi syndrome. In many instances of nutritional rickets, the child may have an associated mild hyperchloraemic normal anion gap metabolic acidosis, which may mislead the physician into diagnosing a primary tubular dysfunction. This functional tubular disorder is a consequence of hyperparathyroidism inducing defective renal conservation of bicarbonate [18].
As mentioned earlier, serum phosphate is typically low in association with elevated PTH in nutritional rickets. Levels may be as low as 03–0.4 mmol/L in rare instances; thus, serum Pi alone should not be used to make a diagnosis of hypophosphataemic rickets.
Infants with vitamin D deficiency rickets typically have normal weight trajectories, although growth may be adversely affected. It has been stated that rickets does not occur in malnourished children as it is a disease that manifests with abnormalities at the growth plates; however, this is not true, as the disease has been well described in severely malnourished infants [27].
The use of alphacalcidol in the treatment of vitamin D deficiency rickets is not recommended, as it is an expensive form of therapy, is less effective than the parent vitamin D [21], does not achieve the supra-physiological levels of 1,25(OH)2D that are achieved by vitamin D and fails to replenish vitamin D stores (25-OHD < 10 nmol/L in the affected child after 3 months of treatment). Furthermore, a response to therapy may mask vitamin D dependency rickets. In this child, alphacalcidol clearly failed to cause biochemical or radiological healing.
The earliest evidence of a response to vitamin D is a rising phosphate concentration, followed by a decrease in PTH, both of which are reassuring trends [14]. ALP may rise initially and remain elevated for a prolonged period before decreasing to normal values, usually between 3 and 6 months after initiation of therapy. A zone of provisional calcification at the growth plate may be noted on radiographs after 3–4 weeks of onset of therapy.
Case 2: nutritional rickets—normal growth and hypocalcaemic seizures
This 5-month-old male infant presented with afebrile generalised seizures 1 day prior to admission. They were characterised by abnormal eye movements, generalised jerking and involuntary muscle movements (symmetrical, flexed arms). The child was born to a P1G1 mother, with a birth weight of 3.25 kg and was exclusively breastfeeding. Growth parameters were normal: W/A Z score, 0.98; H/A Z score, 0.33; and W/H Z score, 1.07. No craniotabes was detected, but mild widening at the wrist was thought to be present on palpation. Developmental milestones were appropriate. Abdominal examination revealed a 2-cm hepatomegaly and 3-cm splenomegaly, which were thought to represent extramedullary haematopoeisis in the presence of iron deficiency anaemia. A radiograph of the wrist showed some osteopenia and radiolucency of the distal end of the radial metaphysis. The ECG revealed a prolonged QTc interval of 0.491 s (normal, <0.43 s).
Based on the clinical presentation, biochemistry (Table 2) and vitamin D status, a diagnosis of hypocalcaemia and seizures due to vitamin D deficiency was made. The infant was successfully treated with intravenous calcium and alphacalcidol (administered at a dose of 0.2 mcg/kg daily to rapidly increase the calcium level) until the total calcium was >1.8 mmol/L, and the QTc interval had begun to normalise and subsequently discharged on ergocalciferol and calcium supplementation for 3 months.
Discussion
Infants (typically <6 months) may present as a clinical emergency with signs and symptoms related to hypocalcaemia. These include late neonatal hypocalcaemia, tetany, seizures, laryngospasm (stridor), apnoea and rarely cardiomyopathy [16]. As these infants generally do not have other signs of vitamin D deficiency, it is imperative that paediatricians should always consider the possibility of hypocalcaemia due to vitamin D deficiency in the mother and her offspring in the differential diagnosis of these clinical presentations in the young infant. Two other important differential diagnoses to consider in hypocalcaemic infants are hypoparathyroidism, including Di-George syndrome (22q11.2 deletion), and pseudohypoparathyroidism, which may be difficult to differentiate from vitamin D deficiency in this age as vitamin D deficient young infants may not have an appropriate PTH response to the hypocalcaemia [5]. These latter conditions typically have elevated serum Pi and normal ALP concentrations.
The staging of vitamin D deficiency as proposed by Fraser provides a useful guide to conceptualise the physiologic derangements that occur during the development of vitamin D deficiency and rickets [10]. Even though there is not always a clear delineation between the three stages of rickets, it is likely that most young infants with hypocalcaemia are in stage 1 (without adequate PTH compensation).
Case 3: vitamin D dependent rickets type 1A
This 6-year-old girl presented with the following key features: a prolonged history of rickets (Fig. 3), an unremarkable family history for rickets in parents who are second cousins, an early age of presentation (6 months), delayed motor milestones and dentition and failed conventional vitamin D therapy for rickets. She was subsequently diagnosed as having XLH and treated with vitamin D analogues (alphacalcidol and calcitriol) and phosphorus supplementation with marginal improvement. Her acute issues included non-compliance to medication, difficult ambulation, severe persistent bone pain, severe skeletal deformities (Fig. 4), severe dental caries, recent tetany, a recent tibia fracture and severe stunting. Her biochemical profile (Table 2) over the last 6 months revealed persistently low calcium (2.12 mmol/L), low phosphate blood levels (range, 0.55–0.8 mmol/L), severe hyperparathyroidism (range, 34–76 pmol/L), low levels of 1,25(OH)2D (<50 pmol/L when off vitamin D analogues), normal 25OHD (50–150 nmol/L), increased ALP (range, 1,500–3,000 IU/L), normal renal function and low TmPi/GFR (0.61 mmol/L) (Table 2). Genetic testing revealed no mutations in the PHEX (XLH), FGF23 (ADHR) or in the coding region of VDR (VDDR II).
Discussion
Incomplete treatment of calciopenic forms of rickets may make the diagnosis of the underlying condition difficult. The inappropriate diagnosis of XLH was probably based on a normal Ca and low serum Pi at that time (normocalcaemia could have been due to therapy with vitamin D analogues, the dose of which were insufficient to correct the hyperparathyroidism and resultant hypophosphataemia). However, cognisance was clearly not taken of the markedly elevated PTH, which is not consistent with the diagnosis of XLH, even though in XLH PTH values might be marginally elevated on initial presentation or more markedly so as a result of phosphate supplementation as part of therapy [22]. The patient presents with features of stage 3 rickets (low calcium, markedly increased PTH and ALP and severe rickets radiologically).
In the presence of severe active rickets with severe secondary hyperparathyroidism and hypocalcaemia and the presence of adequate substrate (a normal 25OHD level), the normal compensatory response is to produce 1,25(OH)2D at supraphysiological levels (as seen in nutritional rickets once therapy with vitamin D is started) [24]. Therefore, the finding of normal or low 1,25(OH)2D values, as in this case, is physiologically inappropriate, suggesting a defect in the conversion of 25OHD to 1,25(OH)2D. The onset and symptoms resemble those of vitamin D deficiency, except that, at presentation, symptoms were severe and myopathy a very marked feature. The presumptive diagnosis of VDDR type1A was made on the failure of conventional treatment for rickets, exclusion of other causes and the child’s complete recovery when treated on vitamin D analogues (alphacalcidol or calcitriol) and compliance to therapy had been ensured.
Case 4: hypophosphataemic rickets
This 4-year-8-month-old child with a presumptive diagnosis of hypophosphatemic rickets was referred because of a poor response to therapy with phosphate and alphacalcidol on which she had been treated for the past 6 months. Growth percentiles reflected marked short stature: W/A Z score, −0.31; H/A Z score, −3.69; and W/H Z score, 2.16. Her birth weight was 3 kg; she began walking at 2 years, had a negative family history and was previously extensively investigated at other hospitals. She has never had seizures, muscle weakness or tetany. She had obvious short stature, knock knees, wide splaying at wrists and mild plagiocephaly. Poor dentition with extensive caries was noted. Her parents are first cousins, and she had two other normal siblings. Radiographs revealed the presence of active rickets and bowing. Biochemistry confirmed hypophosphataemia with mildly elevated ALP and PTH (Table 2). Her renal function was normal, and her TmPi/GFR was low at 0.3 mmol/L. The clinical picture, radiographic changes and the biochemistry supported the diagnosis of X-linked hypophosphataemic rickets, and she was treated accordingly.
Discussion
The classic clinical trial for XLH is hypophosphataemia, progressive lower limb deformities and stunted growth. Notably, the children do not have muscle weakness or tetany. Since the hypophosphataemia does not cause symptoms, their presentation with lower limb deformities typically occurs only after they start weight bearing. ALP is usually moderately elevated and PTH typically within the normal range, although the latter may be marginally elevated at the time of initial diagnosis. The mechanism for the elevated PTH in XLH is unknown [22]. It has been suggested that the parathyroid gland in XLH is resistant to the elevated fibroblast growth factor 23 (FGF23) concentrations typically found [1], thus limiting FGF23’s ability to inhibit PTH secretion [7]. Furthermore, phosphate supplements, which may cause a decrease in ionised calcium and a compensatory increase in PTH concentration, may partially be responsible [22]. Recently, the possibility of the use of calcimimetics (cinacalcet) in controlling hyperparathyroidism in XLH has been considered [2, 28]; however, there are no formal trials reported utilising this adjuvant therapy.
Typically in XLH, the radiographs do not show evidence of osteopenia despite having typical rachitic changes at the growth plates. Few studies have formally studied bone mass in XLH, but in a small study some years ago, bone mass at the lumbar spine was found to be increased in both treated and untreated patients, while radial bone mass tended to be lower than controls [19]
The lack of a family history is not unusual in patients with XLH as sporadic mutations occur in some 30%. In addition, the inheritance pattern is X-linked dominant; therefore, girls are affected more frequently than boys. Some evidence suggests that hemizygote male may be more affected than the heterozygote female (whose clinical manifestation may vary in severity), but this finding is disputed [26]. XLH is linked to defects in PHEX, which is involved in the control of FGF23, whose levels are elevated in XLH [7]. These elevated levels of FGF23 suppress 1,25-(OH)2D formation; thus, patients may have inappropriately low 1,25-(OH)2D in the face of hypophosphataemia. Recent evidence in the mouse model has indicated that elevated FGF23 concentrations play a pivotal role in the hypophosphataemia, depressed 1,25-(OH)2D concentrations and rachitic abnormalities seen in XLH and that the use of anti-FGF23 antibodies corrects the biochemical perturbations and ameliorates the rachitic bone lesions [4], offering hope that a more appropriate therapeutic approach to the management of XLH patients may be available in the future.
The diagnosis of phosphopenic rickets due to renal or FGF23-dependent causes needs to demonstrate renal phosphate wasting. This is accomplished by collecting an untimed fasting urine specimen (typically the second voided urine specimen in the morning) and a blood sample at the same time for the measurement of Pi and creatinine (Cr), after which the phosphate clearance is calculated: FePi = (uPi × pCR/uCR × pPi). The tubular reabsorption of phosphate [TRP% = (1 − FePi) × 100] or TmPi/GFR [6] is typically inappropriately low in the face of hypophosphataemia. The TmPi/GFR (or TRP%) may be low in both phosphopenic and calciopenic forms of rickets and cannot be interpreted without assessing other biochemical parameters.
Case 5: tumour-induced osteomalacia
A 16-year-old teenager presented with joint pains and proximal muscle weakness affecting the pelvic girdle more than the shoulders for 6 months duration. She was a well-nourished adolescent with a weight of 46 kg (BMI Z score, −0.63) and height of 155.5 cm (Z score, −1.04) and in Tanner stage 4 pubertal development. Clinical examination and radiological investigations revealed features of rickets with marked osteopenia. Relevant biochemistry is provided in Table 2. Urine dipstix and renal function was normal. The TmPi/GFR was 0.4 mmol/L GFR and urinary calcium excretion 1.2 mg/kg/24 h (normal, 2–5 mg/kg/24 h). Because of the recent onset and severity of the myopathy, the initial diagnosis was that of acquired hypophosphataemia with rickets/osteomalacia [20].
She was started on phosphate replacement and alphacalcidol, but despite treatment, the condition worsened. She developed bilateral femoral shaft fractures and had corrective osteotomies and rod insertions. Muscle weakness became progressively worse; she developed persistent back and limb pain and a kyphosis as a result of numerous vertebral fractures and became wheelchair bound. FGF23 levels were elevated (198 RU/mL). An octreotide scintigraphy scan was done and revealed a localised hot spot in the distal left femoral metaphysis (Fig. 5) [13]. A biopsy of the distal femur revealed a focus of characteristic calcification and fibrous proliferation along with a loosely textured spindle cell proliferation. Giant cells are also noted. The histology was compatible with a mesenchymal phosphaturic tumour. Although an initial orthopaedic biopsy and curette of the distal femoral metaphysis resulted in an improvement in serum Pi values, these again deteriorated, and the patient subsequently had a distal femoral resection with insertion of knee prosthesis. This resulted in clinical improvement of the myopathy and bone pain and a temporary rise in Pi, although this has decreased again, and a repeat octreotide scintigraphy scan revealed residual uptake around the prosthesis.
Discussion
Tumour-induced osteomalacia (TIO) is an acquired debilitating osteomalacic or rachitic condition associated with a usually benign mesenchymal tumour secreting mainly FG23 [1, 12]. Patients present with osteomalacia/rickets, fractures, severe bone pain and muscle weakness, which help to differentiate TIO from XLH despite similar biochemical phenotypes. The age of presentation of TIO varies, but is considered to be very unusual in children [9] and is not in keeping with XLH and other phosphopenic forms of rickets, which typically present with features of rickets in the first 2 years of life. Careful search for a tumour is an important step in confirming the diagnosis. Tumours generally arise in the neck and head regions or in the skeleton and are usually described as mixed connective tissue tumours, haemangiopericytomas or chondroblastic–osteoblastic fibromas. Localisation of the tumour using octreotide scintigraphy is often successful; however, in certain situations, selective venous sampling for FGF23 concentrations may assist [3]. Removal of tumour after successful localisation results in resolution of symptoms, normalisation of phosphate within hours postoperatively and a decrease in FGF-23 levels. If the tumour is not localised, long-term treatment with phosphate and calcitriol is recommended. Octreotide therapy has been suggested as an alternative option, but is very expensive [23].
Conclusions
We have attempted in this overview to provide an insight into the various clinical and biochemical clues, which can be used to help differentiate the various causes of rickets. Although the various causes of rickets are not dealt with comprehensively, it is intended that the discussion will provide a guide to help categorise the problematic patient, narrowing down the differential diagnosis and reducing the need for often expensive investigations.
References
Alon U (2011) Fibroblast growth factor (FGF) 23: a new hormone. Eur J Pediatr 170:545–554
Alon US, Levy-Olomucki R, Moore WV et al (2008) Calcimimetics as an adjuvant treatment for familial hypophosphatemic rickets. Clin J Am Soc Nephrol 3:658–664
Andreopoulou P, Dumitrescu CE, Kelly MH et al (2011) Selective venous catheterization for the localization of phosphaturic mesenchymal tumors. J Bone Miner Res 26:1295–1302
Aono Y, Yamazaki Y, Yasutake J et al (2009) Therapeutic effects of anti-FGF23 antibodies in hypophosphatemic rickets/osteomalacia. J Bone Miner Res 24:1879–1888
Bonnici F (1978) Functional hypoparathyroidism in infantile hypocalcaemic stage I vitamin D deficiency rickets. S Afr Med J 54:611–612
Brodehl J, Krause A, Hoyer PF (1988) Assessment of maximal tubular phosphate reabsorption: comparison of direct measurement with the nomogram of Bijvoet. Pediatr Nephrol 2:183–189
Carpenter TO, Insogna KL, Zhang JH et al (2010) Circulating levels of soluble klotho and FGF23 in X-linked hypophosphatemia: circadian variance, effects of treatment, and relationship to parathyroid status. J Clin Endocrinol Metab 95:E352–E357
Dijkstra SH, van Beek A, Janssen JW et al (2007) High prevalence of vitamin D deficiency in newborn infants of high-risk mothers. Arch Dis Child 92:750–753
Eyskens B, Proesmans W, Van Damme B et al (1995) Tumour-induced rickets: a case report and review of the literature. Eur J Pediatr 154:462–468
Fraser D, Kooh SW, Scriver CR (1967) Hyperparathyroidism as the cause of hyperaminoaciduria and phosphaturia in human vitamin D deficiency. Pediat Res 1:425–435
Hollis BW, Roos BA, Draper HH, Lambert PW (1981) Vitamin D and its metabolites in human and bovine milk. J Nutr 111:1240–1248
Imel EA, Peacock M, Pitukcheewanont P et al (2006) Sensitivity of fibroblast growth factor 23 measurements in tumor-induced osteomalacia. J Clin Endocrinol Metab 91:2055–2061
Jan de Beur SM, Streeten EA, Civelek AC et al (2002) Localisation of mesenchymal tumours by somatostatin receptor imaging. Lancet 359:761–763
Kruse K (1995) Pathophysiology of calcium metabolism in children with vitamin D- deficiency rickets. J Pediatr 126:736–741
Liang L, Chantry C, Styne D, Stephensen C (2010) Prevalence and risk factors for vitamin D deficiency among healthy infants and young children in Sacramento, California. Eur J Pediatr 169:1337–1344
Maiya S, Sullivan I, Allgrove J et al (2008) Hypocalcaemia and vitamin D deficiency: an important, but preventable, cause of life-threatening infant heart failure. Heart 94:581–584
Mason RS, Diamond TH (2001) Vitamin D deficiency and multicultural Australia. Med J Aust 175:236–237
Muldowney FP, Freaney R, McGeeney D (1968) Renal tubular acidosis and amino-aciduria in osteomalacia of dietary or intestinal origin. Quart J Med 37:517–539
Oliveri MB, Cassinelli H, Bergada C, Mautalen CA (1991) Bone mineral density of the spine and radius shaft in children with X-linked hypophosphatemic rickets (XLH). Bone Miner 12:91–100
Pettifor JM, Ross FP, Quirk M et al (1986) Acquired hypophosphataemic vitamin D resistant rickets in black children. Bone Miner 1:307–319
Rajah J, Abdel-Wareth L, Haq A (2010) Failure of alphacalcidol (1alpha-hydroxyvitamin D3) in treating nutritional rickets and the biochemical response to ergocalciferol. J Steroid Biochem Mol Biol 121:273–276
Schmitt CP, Mehls O (2004) The enigma of hyperparathyroidism in hypophosphatemic rickets. Pediatr Nephrol 19:473–477
Seufert J, Ebert K, Muller J et al (2001) Octreotide therapy for tumor-induced osteomalacia. N Engl J Med 345:1883–1888
Stanbury SW, Taylor CM, Lumb GA et al (1981) Formation of vitamin D metabolites following correction of human vitamin D deficiency: observations in patients with nutritional osteomalacia. Miner Electrolyte Metab 5:212–227
Thacher TD, Fischer PR, Strand MA, Pettifor JM (2006) Nutritional rickets around the world: causes and future directions. Ann Trop Paediatr 26:1–16
Whyte MP, Schranck FW, Armamento-Villareal R (1996) X-linked hypophosphatemia: a search for gender, race, anticipation, or parent of origin effects on disease expression in children. J Clin Endocrinol Metab 81:4075–4080
Wondale Y, Shiferaw F, Lulseged S (2005) A systematic review of nutritional rickets in Ethiopia: status and prospects. Ethiop Med J 43:203–210
Yavropoulou MP, Kotsa K, Gotzamani PA et al (2010) Cinacalcet in hyperparathyroidism secondary to X-linked hypophosphatemic rickets: case report and brief literature review. Hormones (Athens ) 9:274–278
Conflict of interest
The authors declare they have no conflicts of interest and that there were no sponsors of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajah, J., Thandrayen, K. & Pettifor, J.M. Clinical practice. Eur J Pediatr 170, 1089–1096 (2011). https://doi.org/10.1007/s00431-011-1529-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-011-1529-z