Abstract
The aims of this study were to evaluate the implication of food allergy as a cause of paediatric constipation and to determine the diet period needed to tolerate the constipation-causing foods. Fifty-four children aged 6 months to 14 years (median, 42 months) suffering from chronic constipation (without anatomic abnormalities, cοeliac disease or hypothyroidism), unresponsive to a 3-month laxative therapy, were prospectively evaluated. All participants were evaluated for allergy to cow's milk, egg, wheat, rice, corn, potato, chicken, beef and soy, using skin tests (SPT), serum specific IgE and atopy patch test (APT). A withdrawal of the APT-positive foods was instructed. Thirty-two children had positive APT; 15 were positive to one; six, to two and 11, to three or more food allergens, wheat and egg being the commonest. After withdrawing the APT-positive foods for an 8-week period, constipation had improved in 28/32 children, but a relapse of constipation was noticed after an oral food challenge, so they continued the elimination diet. Tolerance to food allergens was achieved in only 6/28 after 6 months, compared to 25/28 after 12 months and to all after a 2-year-long elimination. Food allergy seems to be a significant etiologic factor for chronic constipation not responding to treatment, in infants and young children. APT was found to be useful in evaluating non-IgE allergy-mediated constipation, and there was no correlation of APT with IgE detection. Tolerance was adequately achieved after 12 months of strict food allergen elimination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic constipation is a common problem in children, particularly in the younger ones; it has been calculated to affect 2.9% of infants and up to 10.9% of toddlers during the second year of life [10, 14]. It can shortly be described as a difficulty in defaecation present for two or more weeks with scybalous, pebble-like, mainly hard stools or firm stools two or fewer times per week, in the absence of structural, endocrine or metabolic disease [1].
Immunologic mechanisms have been proposed as the basis of chronic constipation in some children [15]. Allergy can cause gastrointestinal symptoms through IgE-mediated or late-onset cell-mediated pathways. Unlike IgE-mediated allergy that can be studied with in vivo and in vitro tests, there are no well-standardized diagnostic tools for the detection of late-onset gastrointestinal allergies, therefore making the diagnosis and dietary advices difficult. However, there is a growing interest in atopy patch test (APT) that is aimed at detecting delayed-type allergic reactions such as atopic dermatitis and digestive disorders.
The aims of the following study were to detect food allergy in children with chronic constipation and to evaluate the effect of an allergen-free diet, based on the outcome of the performed diagnostic tests [skin tests, detection of specific IgE (sIgE) and APT]. We also studied possible differences between infants and older children regarding the effect of allergy on constipation and the time lapse between the introduction of the elimination diet and the achievement of tolerance.
Methods
Subjects
Children with chronic constipation who were followed up in the outpatient Gastroenterology Clinic of the 1st Dept of Paediatrics of Athens' University were evaluated prospectively. A chart reporting the criteria of constipation was filled upon their original visit. The Rome III inclusion criteria were used in our study (Table 1). Functional constipation was defined as the occurrence of two or more of the six Rome III criteria during 2 months in children with a developmental age of at least 4 years or during 1 month in infants up to 4 years of age [7, 13]. All patients fulfilled the Rome III criteria of chronic constipation (Table 1), and they had failed to respond to a 3-month laxative therapy with lactulose, mineral oil, senna or polyethylene glycol before participating in this study. Exclusion criteria were anatomic abnormalities; any evidence of an inflammatory, metabolic or neoplasmic process; a history of hypothyroidism or of cοeliac disease. Information regarding personal and family (parents and/or siblings) histories of atopy were recorded upon first evaluation. Parental informed consent was obtained for all children.
Tests
All children were subjected to detection of specific IgE, to skin tests and to APTs. The tested foods were cow's milk, egg white, egg yolk, wheat, rice, corn, potato, chicken, beef and soy. The ImmunoCAP System (Phadia, Uppsala, Sweden), considered the most accurate method for sIgE detection, was used. Skin tests were performed using commercial extracts with the skin prick test (SPT) method (ALK Diagnostics, Hørsholm, Denmark for cow's milk, potato and chicken; Alyostal-Stallergens for egg white, egg yolk, wheat, rice, corn and soy; Allergopharma for beef) and with the prick-to-prick method (using the same preparations made for APT). Skin tests were carried out on the volar surface of the right (SPT to commercial extracts) and the left (prick-to-prick to fresh preparations) forearms. Negative (50% glycerinated HAS-saline) and positive (histamine dihydrochloride, 10mg/ml) controls were used.
Patients with a sIgE level >0.35 kU/l (ImmunoCAP detection limit) were considered sensitized to the relative allergen. The results of the skin tests were interpreted according to the EAACI standards; a skin test response was considered positive when the wheal diameter was larger than 3 mm compared to the negative control [17]. A patient testing positive to both sIgE and SPT or to either of them was considered IgE sensitized, taking into consideration that sensitized is not synonymous to allergic.
APTs to all the above-mentioned allergens were performed using fresh foods: fresh cow's milk containing 3.5% fat, whisked hen's egg (white and yolk), wheat, rice, corn, potato, chicken, beef and soy powder dissolved in water (1 g/10ml). The mixtures were then placed in 12-mm aluminium cups (Finn Chambers on Scanpore, Tuunsula, Finland) on uninvolved areas of the patient's back. The patch test occlusion time and its readings followed the revised European Task Force on Atopic Dermatitis recommendations [18]. A first reading was done 20 min after the application of the allergens so as to exclude an immediate skin reaction. Responses to APT were evaluated 48 h (20 min after removing the patch) and 72 h after the application.
Clinical follow-up
Children with positive APT were advised to follow an elimination (allergen-free) diet during the next 8 weeks, avoiding completely the foods that were found positive to APT or to sIgE and/or SPT. No laxative treatment was prescribed during the follow-up phase. Clinical re-evaluation was scheduled 8 weeks, 6 months, 12 months and 2 years after enrollment, and a chart reporting the criteria of constipation (as described in Rome III) before testing and after the dietary manipulation was completed each time, so as to follow the clinical outcome.
An elimination diet was also advised to children with negative APT but testing positive for sIgE and/or SPT. The foods that resulted positive were excluded from their diet, and a re-evaluation was programmed as above mentioned.
In children showing improvement of symptoms after an 8-week elimination diet (either based on APT or sIgE/SPT results), an open food challenge was performed. Children presenting relapse of constipation after the challenges were advised to keep on avoiding the suspected foods, and oral food challenges with open provocation tests were performed again at the sixth month of the study. Open provocation tests were performed under medical surveillance with a gradual updosing of the foods (1 gr, 5 gr, 10 gr, 20 gr). Foods were given in the form that had been ingested before the diet, keeping 30-min intervals among doses and a 2-h long surveillance period after the last dose.
Personalized instructions about the way of further dose addition were given for the following days. In the case that constipation reappeared in the following 3 weeks, the former elimination diet was followed again, and new provocation tests were performed at the 12th and 24th months of the study. In cases of multiple allergic sensitizations, provocation tests to each food were performed with a 1-week interval, so as not to expand the protocol's intervals too much. In cases of relapse in multi-sensitive patients, all foods challenged up to that moment were considered responsible.
Statistical analysis
The non-parametric Mann–Whitney U test was used to compare the results of IgE detection (negative or positive) between children aged up to 2 years and children older than 2 years. The level of significance was p = 0.05. The degree of agreement between IgE-based methods and APT was evaluated by Fisher's exact test. Analyses were performed using the STATISTICA, version 5.0 (Stat Soft Inc., USA) software.
Results
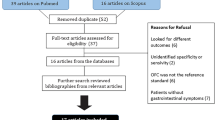
Fifty-four children (25 boys) aged 6 months to 14 years (median, 3.5 years) were enrolled in this study. Thirty-two children had positive APT upon the first evaluation, and among them, 15 were mono-sensitized (8 to wheat, 5 to egg and 2 to rice), six were positive to two food allergens and the remaining 11 were sensitive to three or more foods. Surprisingly, wheat was found to be the most common allergen testing positive in 21/32 APTs, followed by egg that was positive in 16/32, while cow's milk was positive in only 3 cases (Table 2). sIgE and/or SPT were positive in 29/54 children (Fig. 1).
In 13 children, both IgE-mediated and cell-mediated sensitizations were detected (positive APT and sIgE and/or SPT), while only IgE-mediated sensitization was detected in the remaining 16. All children with IgE-mediated sensitization had a sIgE level >0.7 kU/l. Thirty children had a personal history of atopy, while 25 had a family history of atopy.
A total of 307 test results were pooled and analyzed. As seen in Table 3, there was no association between IgE tests and APT. There was no significant difference in the presence of positive sIgE and/or SPT to food allergens between children older than 2 years (23/41) and those younger than 2 years (6/13).
Upon re-examination, 8 weeks after following an elimination diet, an improvement of constipation was observed in 28/32 of the APT+ children that did not fulfil the Rome III criteria anymore (Fig. 2). The open food challenge was positive in all 28, so they were advised to continue the elimination diet. The four non-responders to the elimination diet were released to a free diet again. Only one infant out of the 16 APT-negative atopic children, who was IgE positive to milk (both sIgE and SPT), had an improvement of his constipation after milk elimination and relapse at the eighth week's challenge. A food reintroduction was recommended to the rest.
Clinical and laboratory evaluation over the study period. Patients with either a positive APT or any positive sIgE and/or SPT (even if APT negative) were advised to follow an elimination diet to the food(s) that resulted positive. After 8 weeks on elimination diet, they were followed by a clinical re-evaluation and oral food challenge. When, after clinical improvement on the diet, the OFC was positive, the diet was continued; after a negative OFC, the child returned to a normal diet. This procedure was repeated after 6, 12 and 24 months
Upon re-evaluation, at their sixth month visit, the same clinical–laboratory examination was repeated to the 28 children who were on elimination diet (Fig. 2). Six children tolerated the food, while the rest presented a relapse of their symptoms upon oral food challenge within 21 days. Five out of six children who tolerated the allergenic food had negative or doubtful APT. Twenty-two children with positive oral food challenges were advised to keep their allergen-free diet (All had positive APT, and nine had also positive sIgE and/or SPT). The child with positive IgE test, being on a hypoallergenic milk formula, had a negative oral food challenge (OFC); he tolerated milk and continued on a milk-containing diet, although his SPT was still positive. On the 12th month re-examination, 19 more patients had achieved tolerance to the offending food allergens, and only three patients relapsed and went on with their diets. No correlation was found between the APT result and OFC outcome (data not shown). No change in the results of sIgE and/or SPT was noticed in the patients. The three patients with positive OFC after 12 months had negative OFC after 24 months (APT negative in 3/3, IgE negative in 2/3) and were advised to reintroduce the offending food.
Discussion
In this prospective study, about half of a group of children with constipation not responsive to laxative treatment were found to have positive APT and obtained resolution of their symptoms after the elimination of the relative food allergen(s). The effect of dietary manipulation on symptoms of constipation in infants has been investigated before, but not with nine different food allergens and with both IgE tests and APT. In an Italian study, symptoms of constipation resolved in 21 out of 27 infants on a cow's milk-free diet, reappearing after the reintroduction of milk [8]. The same research team reported that a resolution of peri-anal lesions and anal fissures (noticed in 75% of their study group) was achieved after replacing cow's milk with soy milk [9].
In another paper, referring to constipation in a group of 185 children with constipation aged less than 2 years, a very low prevalence of food allergy (2%) was found, but the study was based on a retrospective computer search, and no accurate allergy testing, elimination diets or OFC were conducted [10]. In a further study, 28% of children (aged up to 11 years) suffering from chronic constipation was symptom free after a 4-week period of milk-free diet. However, the authors had not performed APT, and based on IgE testing, they reported that there was no relation between resolution of constipation and IgE-mediated milk allergy [4].
There are many findings suggesting that allergy is one of the causes of constipation during childhood; lymphonodular hyperplasia in the colon and in the terminal ileum is proved to be a macroscopic marker of cow's milk allergy-associated constipation, while there has been noticed a higher number of eosinophils and γδ+ T lymphocytes in samples of colonic and ileal biopsies of constipated patients compared with controls [19]. A cell-mediated allergy can be the underlying immunologic mechanism in many cases of constipation, and it has been shown that allergy to proteins, such as cow's milk, may induce constipation in association with an eosinophilic proctitis [3].
Cell-mediated allergy was shown to be the common parameter causing constipation in some of our patients, and the APT results were shown to be much more helpful than the rather irrelevant IgE detection. The APT is an easy-to-perform and much-promising test based on the epicutaneous application of food or airborne allergens, performed with a method similar to the one used for the diagnosis of contact dermatitis [20]. Due to its mechanism of T lymphocyte-mediated cutaneous late-phase reaction, the APT is more sensitive to detect late-phase food allergy reactions than the in vitro determination of sIgE and the in vivo SPT that are IgE-dependent diagnostic methods [11].
In the present study, symptoms of constipation resolved after an elimination diet in a high percentage of children not responsive to laxatives. No resolution of constipation was noticed in the absence of positive APT, and elimination-diet decisions based on IgE detection were proved to be unsuccessful, with the exception of an infant allergic to cow's milk. The age range of our patients was wider compared to the ones studied in previous studies, leading to the conclusion that dietary manipulations based on positive APT can be useful in all children with constipation not responding to laxatives.
It seems clear that IgE tests are of no use in the diagnosis of constipation or other digestive disorders with a suspected non-IgE-mediated mechanism [2, 16]. Our study suggests that SPT and sIgE tests should not be used as reliable indicators for diet manipulations in cases of chronic constipation not responding to conventional laxative treatment. The history of atopy was also shown to be of no use, since–although a high percentage of our patients were atopic–there was no correlation between the history of atopy and the diet's outcome. The APT is nowadays the main diagnostic tool in atopic eczema, but it is also proposed for the diagnosis of gastrointestinal milk allergy and eosinophilic oesophagitis [5, 16].
APT is a promising decision marker for elimination diets, and it is shown to have a very high sensitivity (78–99%) in the study of eosinophilic oesophagitis [10, 16]. The evaluation of single skin signs at 72 h has been reported to increase the diagnostic value of APT [6]. APT is not influenced by age (infancy or childhood); the responsible food allergens depend on the age group and on the patient's diet [12].
A point that differentiates our data from the ones of former studies is in regard to the responsible food allergens. Wheat was found to be the main allergen, followed by egg, while milk–that is usually the allergen of reference in APT studies–in most of the cases yielded negative results and seems not to be involved in the constipation of our patients. A possible explanation for this finding is the age of the participants, since only 12/54 were younger than 24 months.
Apparently, the effect of immunoregulation on constipation is more similar to the one present in eosinophilic oesophagitis than in atopic eczema, where a combination of IgE-mediated and non-IgE-mediated immune mechanisms are involved. The lack of correlation between atopic history and diet outcome in constipated patients indicates that APT can be used in all cases fulfilling the Rome III criteria and not responding to laxatives, no matter whether a history of atopy exists or not.
On follow-up, APT turned negative or became weaker, almost in parallel with the clinical course and the tolerance. This may be a phenomenon of the non-IgE-mediated allergy.
Our results suggest that, with a 12-month period of strict allergen avoidance, tolerance is achieved in most children; however, the study of a larger number of monosensitive patients would lead to more accurate conclusions. Nevertheless, it appears that APT can be of great help, guiding an allergen-free diet.
In conclusion, we have shown that laxative-resistant constipated children can become symptom free with the use of an elimination diet based on APT results, regardless of their age. Tolerance to the offending food(s) was obtained within 1 year in most children and within 2 years in all.
References
Baker SS, Liptak GS, Colletti RB et al (1999) Constipation in infants and children evaluation and treatment. J Pediatr Gastroenterol Nutr 29:612–626
Caffarelli C, Coscia A, Baldi F et al (2007) Characterization of irritable bowel syndrome and constipation in children with allergic diseases. Eur J Pediatr 166:1245–1252
Carroccio A, Scalici C, Maresi E et al (2005) Chronic constipation and food intolerance: a model of proctitis causing constipation. Scand J Gastroenterol 40:33–42
Daher S, Tahan S, Solé D et al (2001) Cow's milk protein intolerance and chronic constipation in children. Pediatr Allergy Immunol 12:339–342
De Boissieu D, Waguet JC, Dupont C (2003) The atopy patch tests for detection of cow's milk allergy with digestive symptoms. J Pediatr 142:203–205
Heine RG, Verstege A, Mehl A et al (2006) Proposal for a standardized interpretation of the atopy patch test in children with atopic dermatitis and suspected food allergy. Pediatr Allergy Clin Immunol 17:213–217
Hyman PE, Milla PJ, Benninga MA et al (2006) Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology 130:1519–1526
Iacono G, Carroccio A, Cavataio F et al (1995) Chronic constipation as a symptom of cow milk allergy. J Pediatr 126:34–39
Iacono G, Cavataio F, Montalto G et al (1998) Intolerance of cow's milk and chronic constipation in children. N Engl J Med 339:1100–1104
Loening-Baucke V (2005) Prevalence, symptoms and outcome of constipation in infants and toddlers. J Pediatr 146:359–363
Mehl A, Rolinck-Werninghaus C, Staden U et al (2006) The atopy patch test in the diagnostic workup of suspected food-related symptoms in children. J Allergy Clin Immunol 118:923–929
Perackis K, Celik-Bilgili S, Staden U et al (2003) Influence of age on the outcome of the atopy patch test with food in children with atopic dermatitis. J Allergy Clin Immunol 112:625–627
Rasquin A, Di Lorenzo C, Forbes D et al (2006) Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 130:1527–1537
Roma-Giannikou E, Adamidis D, Gianniou M et al (1999) Epidemiology of chronic constipation in Greek children. Hell J Gastroenterol 12:58–62
Sicherer SH (2003) Clinical aspects of gastrointestinal food allergy in childhood. Pediatrics 111:1609–1616
Spergel JM, Brown-Whitehorn T, Beausoleil JL et al (2007) Predictive values for skin prick test and atopy patch test for eosinophilic esophagitis. J Allergy Clin Immunol 119:509–511
Sub-Committee on Skin Tests of the European Academy of Allergology and Clinical Immunology (1989) Skin tests used in type I allergy testing Position paper. Allergy 44:1–59
Turjanmma K, Darsow U, Niggemann B et al (2006) EAACI/GA2LEN position paper: present status of the atopy patch test. Allergy 61:1377–1384
Turunen S, Karttunen TJ, Kokkonen J (2004) Lymphoid nodular hyperplasia and cow's milk hypersensitivity in children with chronic constipation. J Pediatr 145:606–611
Wistokat-Wülfing A, Schmidt D, Darsow U et al (1999) Atopy patch test reactions are associated with T lymphocyte-mediated allergen-specific immune responses in atopic dermatitis. Clin Exp Allergy 29:513–521
Conflict of interest
No financial sponsorship was used for the research. The authors do not have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Syrigou, E.I., Pitsios, C., Panagiotou, I. et al. Food allergy-related paediatric constipation: the usefulness of atopy patch test. Eur J Pediatr 170, 1173–1178 (2011). https://doi.org/10.1007/s00431-011-1417-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-011-1417-6