Abstract
To assess whether breastfeeding protects against acute gastroenteritis (AGE) due to rotavirus (RV) infection compared to RV-negative AGE (RV−) in children age 0–12 months. Data from a community-based study of children with AGE from 30 pediatric practices in Germany, Switzerland, and Austria were evaluated. A case–control design was conducted with RV-positive AGE (RV+) cases and RV− AGE as controls. Odds ratios and 95% confidence intervals were estimated using log-linear regression models adjusting for child’s age, family size, number of siblings, child care attendance, and nationality. A total of 1,256 stool samples were collected from infants with AGE; 315 (25%) were RV+ and 941 RV−. Being breastfed in the period of disease inception reduced the risk of AGE due to RV+ (OR, 0.53; 95% CI, 0.37–0.76). In infants 0–6 months of age, the protective effect was stronger (OR, 0.33; 95% CI, 0.19–0.55) than in 7–12-month-old children. Our study adds to the evidence of a protective concurrent effect of breastfeeding against rotavirus infection in infants, particularly in children 6 months and younger. Breastfeeding is important to diminish rotavirus-related gastroenteritis in infants before vaccination can be introduced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotaviruses are one of the leading infectious agents causing gastroenteritis in children and are a relevant cause of community-acquired gastroenteritis in children aged 4 years and younger [12]. It has been estimated that about 3.6 million episodes of rotavirus (RV) disease occurs annually among the 23.6 million children younger than 5 years of age in the United States [32]. Prevention can be achieved by vaccination; however, not in the first 2 months. Breastfeeding is considered to protect against infections [15, 28]. However, epidemiological findings on the protective effect of breastfeeding are inconsistent. Some studies did not show an effect of breastfeeding against rotavirus infection [2, 14, 16, 23, 25] and others found that breastfeeding may alleviate the severity of symptoms [5, 35]. However, a majority of investigations reported a protective effect against RV infections [4, 6, 13, 20, 24, 26, 33].
Several studies did not report an association between breastfeeding and RV-related diarrhea [2, 14, 16, 25]. One study from India had a small sample size (n = 34); only three infants were not breastfed [25]. In another study from Brazil, the total sample included 403 infants, but only 46 were RV-positive. There was an overall statistically significant protective effect of breastfeeding; however, in the 46 RV-positive infants, the association did not gain statistical significance [2]. In a Canadian study, 16 of 29 infants not breastfed contracted a RV infection (55%), but only 29 of 75 breastfed infants (39%) [16]. Again, the sample size was too small to detect a statistically significant protective effect, but not in an investigation from Bangladesh (n = 2,276) that found that 77% of the infants 0–5 months of age without diarrhea were breastfed, but 88% of 89 children were with RV-related diarrhea. The respective proportions in children 6–11 months of age were 88% and 92%, respectively [14].
Two studies reported that breastfeeding alleviates the severity of symptoms compared to community-based healthy controls or controls in a cohort study [5, 35]. Six studies reported a protective effect of breastfeeding. Two of the investigations compared infants with RV infection with infants hospitalized with other diseases [20, 24]. Another two projects compared infants in newborn nurseries [4, 33] and one from 15 days to 2 years of age [13]. Finally, one study followed up children residing in Abu Homos, Egypt [26], and compared RV-infected infants under 1 year of age with those without RV infection.
Since the findings of these studies are inconsistent, the role of breastfeeding against RV infection is still inconclusive. The discrepancy of these studies may be due to the age of the children and the selected references (healthy controls, sick controls, and AGE controls). Contradictory findings were reported for infants [2, 13, 24, 25] and also mixed groups of infants and toddlers [5, 14, 16, 23].
The aim of this analysis was to determine whether concurrent breastfeeding (in the time window in which new infections occurred) reduced the risk of rotavirus positive (RV+) AGE in infants age 0–12 months compared to infants with other AGE.
Materials and methods
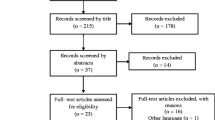
A community-based study of children 0–4 years of age with AGE from 30 pediatric practices in Germany in May 1997–April 1998 and Switzerland and Austria (December 1997–May 1998) was analyzed [9, 12, 22]. Stool samples of a total of 3,465 cases with AGE were tested. The analysis was restricted to children 0–12 months of age with 1,256 children. Study procedures and data handling were approved by the ethics committee of the main referral hospital in the different areas; the principal vote was obtained at the University of Freiburg.
Collection of data and sample testing
Written informed consent was obtained from the parents before the collection of data.
Acute gastroenteritis was defined as the occurrence of vomiting and/or diarrhea not resulting from other evident causes. Diarrhea was defined as passing of two or more liquid or semi-liquid stools or a single watery stool per day by a child [12]. The severity of diarrheal episodes was assessed using the numerical score of Vesikari et al. (0–20 points) [31], which took into account the duration and frequency of diarrhea and vomiting, fever, dehydration, and treatment. The assessment was conducted by the respective pediatrician, all following the same protocol. Stool specimens were obtained and analyzed by trained physician assistants to determine the presence of rotavirus using an enzyme-linked immunosorbent assay (ELISA) test kit (TestPack Rotavirus; Abbott, Delkenheim, Germany). The test was performed according to the manufacturer’s protocol. The sensitivity of this test was stated to be 95% and the specificity 90% [3]. Infants with missing stool samples or missing informed consent were not included.
Parents of children with AGE were asked using a standardized questionnaire. The following variables were considered in this analysis: child’s gender (female, male), child’s age (0–6 and 7–12 months), family size (two persons, three persons, and more than three persons), siblings (none, one and two or more), child care (parents and others versus only parents), nursing (nursed in the period of disease inception versus not nursed), nationality (foreign versus one of the three respective nationalities), season when the child had AGE (summer and winter), and date of visit.
Data quality assurance was done through weekly monitoring of data collected. Core checks for all patients (birth date and presence of AGE) and full check of 10% of data through the monitor and of all data simultaneously with the data entry for completeness and plausibility were performed. Data corrections were implemented through queries.
Data analysis
A nested case–control design within a cohort of AGE cases was applied to assess the effect of breastfeeding. Cases were RV+ AGE children, controls were RV-negative AGE (RV−). Odds ratios (OR) and 95% confidence intervals (CI) were estimated using logistic regression models. For rotavirus-infected children, the odd ratio provides the chance of being at risk compared to children with other gastrointestinal infections. Regarding breastfeeding, a lower odds ratio indicates that children with rotavirus infection had a lower chance of being exposed to breastfeeding compared to children with other AGEs. The regression models were adjusted for child’s sex and age, family size, number of siblings, child care, season, and nationality. In addition to using the whole sample, we stratified for age of the child (0–6 months and 7–12 months) and time of the year (October–March and April–September). The SAS statistical package, Version 9.2, was used to conduct the data analysis.
Results
Of 1,256 children with AGE, 315 cases with rotavirus antigen in stools were detected (25.1%). Infants between 0 and 6 months of age accounted for 35.6% of the RV+ AGE+ cases and infants between 7 and 12 months of age for 64.4% of all RV+ AGE+ cases (Table 1). For children 0–12 months of age, 17.1% of the RV+ cases and 28.6% of the RV− controls were breastfed. For the age group 0–6 months, 21.4% of the RV+ cases were breastfed and 45.0% of the controls. For the age group 7–12 months, the proportion of breastfed children was not different in the RV+ and RV− cases (14.8% compared to 16.7%). There was no difference in the odds ratios for breastfeeding in October–March and April–September (data not shown).
Of the confounders, nationality, child care, siblings, family size, season, and infants’ age had no measurable influence (Table 2). In the period of RV+ inception, for RV+ cases compared to RV− AGE+ controls, the odds of concurrent breastfeeding is lower (OR, 0.53; 95% CI, 0.37–0.76), indicating a protective effect. Stratification by age (0–6 and 7–12 months) showed that the protective effect of being breastfed for children 0–6 months of age (OR, 0.33; 95% CI, 0.19–0.55) is stronger than in the group of 7–12 months (OR, 0.83; 95% CI, 0.52–1.33). Testing the interaction between these two age groups and breastfeeding showed a statistically significant difference (p = 0.009).
In addition, all cases of gastroenteritis were characterized using the Vesikari Score. Among RV-positive infants who were not breastfed, 24.5% had a Vesikari score of more than 10; among those who were breastfed, only 9.3% of RV-positive infants had a Vesikari score more than 10 (p = 0.02). Using the score as continuous variable, the non-parametric Kruskal–Wallis test showed a statistically significant difference (p = 0.01).
Discussion
The results of this case–control analysis nested in a community-based study on rotavirus morbidity of infants 0–12 months of age suggest a protective role of concurrent breastfeeding on acute gastroenteritis caused by rotaviruses compared to other AGEs. The protective effect was confined to children 6 months and younger.
There is no indication of a selection bias. A total of 29,092 children age 0–4 years were under observation in 30 pediatric practices in Germany, Austria, and Switzerland—3,465 cases of AGE+ were detected. We focused on children 0–12 years of age with 1,256 children. Also, a recall bias is less likely because information on breastfeeding was recorded by the pediatrician at the first consultation. RV infection was determined by trained physician’s assistants by ELISA test kit, whose sensitivity and specificity provided by the manufacturer were 95% and 90%, respectively [3]. Since the ELISA kit used (TestPack Rotavirus) may have resulted in at least 10% false-positive RV children, we assessed the potential effect of this bias. We assume that the misclassification of the ELISA kit is not different in breastfed and non-breastfed children (non-differential misclassification). Originally, we have 315 infants who were RV-positive (54 breastfed) and 941 who were RV-negative (269 breastfed; Table 1). These numbers result in an unadjusted OR of 0.52 (54×672/261×269). Considering that 10% of the infants were RV false-positive, we would have 49 breastfed and 235 non-breastfed RV-positive children. The corrected numbers of RV-negative children thus comprise 274 breastfed and 698 non-breastfed infants. The adjusted numbers result in an odds ratio of 0.53 (49×698/235×274). Hence, when we correct for a 10% false-positive proportion, the OR does not deviate substantially (0.52 compared to 0.53), suggesting that the protective effect of breastfeeding cannot be explained by a misclassification due to the ELISA test used in this study.
A limitation of our study is that we do not have the intensity of breastfeeding. Also, information on breastfeeding duration does not exist if the child was not breastfed at the time when the diarrheal episode occurred.
Given the community-based screening for rotavirus cases among AGE, we did not compare RV+ AGE+ cases with children having no gastroenteritis but with RV− AGE+ children. The disadvantage of this approach is an underestimation of the protective effect of breastfeeding, since breastfeeding is known to protect AGE in general [29]. The advantage of this approach is that we exclude a Berkson’s bias that may result if we have compared different diseases with different probabilities of visiting pediatricians [11]. Given this setting, our approach assesses the protective effect of breastfeeding above and beyond the general protection of AGE by breastfeeding.
Our analyses focused on incidence, not on severity; however, using Vesikari scores, we additionally analyzed whether breastfeeding mitigates the severity of the infection. Our findings suggest that breastfeeding may diminish the symptom score of RV infection. Likewise, in a rotavirus vaccine study, children who received the vaccine had an infection prevented or its severity modified [30]. Also, a prior study demonstrated that children who received RV vaccine had lower hospitalization rates [7], a marker for severity. Regarding breastfeeding, in a case–control study from the United States, breastfeeding was protective against hospitalization for RV AGE for infants <6 months of age [8]. Comparing a community-based birth cohort in South India (n = 351) to a sample of children admitted to the hospital with gastroenteritis (n = 343), the proportion of breastfed participants was higher in the community cohort than in children admitted to the hospital (73% versus 34.8%) (P < 0.001) [1]. The authors suggested that increased viral replication in non-breastfed children led to a greater severity of rotavirus diarrhea resulting in hospital admission.
In addition, since all children were AGE+, all were likely to be exposed to some microbial agents. The majority of AGE cases were RV− (74.9%). Evidence suggests that microbial agents that cause AGE+ are predominately viruses (70%) [10]. The proportion of gastrointestinal infections with bacteria and parasites is higher in developing countries [34]. Acute gastrointestinal infections due to bacteria and parasites are acquired often by contaminated water or food. Regarding rotavirus, because it is stable in the environment, transmission can occur through ingestion of contaminated water or food and contact with contaminated surfaces. We adjusted to child care and number of siblings which may be sources of microbial contamination. Since a lower odds ratio for breastfeeding was identified for RV+ infants, our findings suggest that breastfeeding has a specific protection against rotavirus infections.
Possible explanations for the protective effect of breastfeeding on RV+ include a number of substances found in breastmilk. First, human milk possesses a protein known as lactoferrin which impairs the function of surface-expressed virulence factors, thereby decreasing the ability to adhere to mammalian cells in vitro. Hence, lactoferrin may protect infants by inhibiting the adhesion of rotavirus in their gut [27, 29]. Breastmilk is also believed to protect infants from infectious diseases through immunoglobulin A (IgA) and trypsin inhibitors [17–19]. Jajashree and colleagues found that the acquisition of rotavirus infection during early neonatal period (initial 5 days of life) depends on the concentrations of antirotavirus IgA and trypsin inhibitors in human milk [19]. In addition, the inhibitory effects of lactadhedrine, a human milk-fat globule protein, on the binding capability of rotavirus has been suggested [21]. Another study demonstrated that human milk mucin can bind to rotavirus and as a consequence inhibits viral replication [36].
In conclusion, our study adds to the evidence of a protective effect of breastfeeding against RV infection in infants. Of particular importance, the protective effect of breastfeeding was confined to children 6 months and younger. Currently, vaccination against rotavirus is offered at 2, 4, and 6 months of age. In the period from 0–2 months of age, infants seem to be best protected by breastfeeding. Hence, breastfeeding may diminish rotavirus-related gastroenteritis in infants before vaccination can be introduced. Promotion of breastfeeding and information on rotavirus vaccination should emphasize that also breastfeeding reduces the risk of RV infections.
Abbreviations
- AGE:
-
Acute gastrointestinal enteritis
- ELISA:
-
Enzyme-linked immunosorbent assay
- IgA:
-
Immunoglobulin A
- OR:
-
Odds ratio
- 95% CI:
-
95% confidence interval
- RV−:
-
Rotavirus negative
- RV+:
-
Rotavirus positive
References
Banerjee I, Ramani S, Primrose B et al (2006) Comparative study of the epidemiology of rotavirus in children from a community-based birth cohort and a hospital in South India. J Clin Microbiol 44:2468–2474
Blake PA, Ramos S, MacDonald KL et al (1993) Pathogen-specific risk factors and protective factors for acute diarrheal disease in urban Brazilian infants. J Infect Dis 167:627–632
Brooks RG, Brown L, Franklin RB (1989) Comparison of a new rapid test (TestPack Rotavirus) with standard enzyme immunoassay and electron microscopy for the detection of rotavirus in symptomatic hospitalized children. J Clin Microbiol 27:775–777
Chrystie IL, Totterdell BM, Banatvala JE (1978) Asymptomatic endemic rotavirus infections in the newborn. Lancet 1:1176–1178
Clemens J, Rao M, Ahmed F et al (1993) Breast-feeding and the risk of life-threatening rotavirus diarrhea: prevention or postponement? Pediatrics 92:680–685
Cunningham AS (1987) Breast-feeding and health. J Pediatr 110:658–659
Curns AT, Steiner CA, Barrett M et al (2010) Reduction in acute gastroenteritis hospitalizations among US children after introduction of rotavirus vaccine: analysis of hospital discharge data from 18 US states. J Infect Dis 201:1617–1624
Dennehy PH, Cortese MM, Begue RE et al (2006) A case–control study to determine risk factors for hospitalization for rotavirus gastroenteritis in U.S. children. Pediatr Infect Dis J 25:1123–1131
Ehlken B, Laubereau B, Karmaus W et al (2002) Prospective population-based study on rotavirus disease in Germany. Acta Paediatr 91:769–775
Elliott EJ (2007) Acute gastroenteritis in children. BMJ 334:35–40
Feinstein AR, Walter SD, Horwitz RI (1986) An analysis of Berkson’s bias in case–control studies. J Chronic Dis 39:495–504
Fruhwirth M, Karmaus W, Moll-Schuler I et al (2001) A prospective evaluation of community acquired gastroenteritis in paediatric practices: impact and disease burden of rotavirus infection. Arch Dis Child 84:393–397
Gendrel D, Akaga R, Ivanoff B et al (1984) Acute gastroenteritis and breast feeding in Gabon. Preliminary results. Med Trop (Mars) 44:323–325
Glass RI, Stoll BJ, Wyatt RG et al (1986) Observations questioning a protective role for breast-feeding in severe rotavirus diarrhea. Acta Paediatr Scand 75:713–718
Golding J, Emmett PM, Rogers IS (1997) Gastroenteritis, diarrhoea and breast feeding. Early Hum Dev 49(Suppl):S83–S103
Gurwith M, Wenman W, Hinde D et al (1981) A prospective study of rotavirus infection in infants and young children. J Infect Dis 144:218–224
Haffejee IE (1991) Neonatal rotavirus infections. Rev Infect Dis 13:957–962
Hanson LA, Hahn-Zoric M, Berndes M et al (1994) Breast feeding: overview and breast milk immunology. Acta Paediatr Jpn 36:557–561
Jayashree S, Bhan MK, Kumar R et al (1988) Protection against neonatal rotavirus infection by breast milk antibodies and trypsin inhibitors. J Med Virol 26:333–338
Kurugol Z, Geylani S, Karaca Y et al (2003) Rotavirus gastroenteritis among children under 5 years of age in Izmir, Turkey. Turk J Pediatr 45:290–294
Kvistgaard AS, Pallesen LT, Arias CF et al (2004) Inhibitory effects of human and bovine milk constituents on rotavirus infections. J Dairy Sci 87:4088–4096
Laubereau B, Gateau S, Ehlken B et al (1999) Rotavirus gastroenteritis in infants and children. Results of a prospective study in the area of Geneva and Basel 1997/1998 (RoMoS). RoMoS Study Group. Schweiz Med Wochenschr 129:1822–1830
Linhares AC, Gabbay YB, Freitas RB et al (1989) Longitudinal study of rotavirus infections among children from Belem, Brazil. Epidemiol Infect 102:129–145
Mastretta E, Longo P, Laccisaglia A et al (2002) Effect of Lactobacillus GG and breast-feeding in the prevention of rotavirus nosocomial infection. J Pediatr Gastroenterol Nutr 35:527–531
Misra S, Sabui TK, Basu S et al (2007) A prospective study of rotavirus diarrhea in children under 1 year of age. Clin Pediatr (Phila) 46:683–688
Naficy AB, Abu-Elyazeed R, Holmes JL et al (1999) Epidemiology of rotavirus diarrhea in Egyptian children and implications for disease control. Am J Epidemiol 150:770–777
Newburg DS, Peterson JA, Ruiz-Palacios GM et al (1998) Role of human-milk lactadherin in protection against symptomatic rotavirus infection. Lancet 351:1160–1164
Newburg DS, Ruiz-Palacios GM, Morrow AL (2005) Human milk glycans protect infants against enteric pathogens. Annu Rev Nutr 25:37–58
Ochoa TJ, Cleary TG (2009) Effect of lactoferrin on enteric pathogens. Biochimie 91:30–34
Plosker GL (2010) Pentavalent rotavirus vaccine (RotaTeq): a review of its use in the prevention of rotavirus gastroenteritis in Europe. Drugs 70:1165–1188
Ruuska T, Vesikari T (1990) Rotavirus disease in Finnish children: use of numerical scores for clinical severity of diarrhoeal episodes. Scand J Infect Dis 22:259–267
Soriano-Gabarro M, Mrukowicz J, Vesikari T et al (2006) Burden of rotavirus disease in European Union countries. Pediatr Infect Dis J 25:S7–S11
Totterdell BM, Chrystie IL, Banatvala JE (1976) Rotavirus infections in a maternity unit. Arch Dis Child 51:924–928
Webb A, Starr M (2005) Acute gastroenteritis in children. Aust Fam Physician 34:227–231
Weinberg RJ, Tipton G, Klish WJ et al (1984) Effect of breast-feeding on morbidity in rotavirus gastroenteritis. Pediatrics 74:250–253
Yolken RH, Peterson JA, Vonderfecht SL et al (1992) Human milk mucin inhibits rotavirus replication and prevents experimental gastroenteritis. J Clin Invest 90:1984–1991
Acknowledgments
This study was sponsored by Wyeth-Pharma, Münster, Germany. We thank Saroochi Agarwal, Alycia Albergottie, Kesinee Hanjangsit, and Olurinde Oni for editing previous versions of this manuscript. We are obliged to patients and parents who consented to take part in this study and the helpful cooperation of practice assistant, without whom this study would not have been feasible.
Conflicts of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Plenge-Bönig, A., Soto-Ramírez, N., Karmaus, W. et al. Breastfeeding protects against acute gastroenteritis due to rotavirus in infants. Eur J Pediatr 169, 1471–1476 (2010). https://doi.org/10.1007/s00431-010-1245-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-010-1245-0