Abstract
Introduction
Hypothermia at birth is strongly associated with mortality and morbidity in pre-term infants.
Background
A local audit showed limited effectiveness of occlusive wrapping in preventing admission hypothermia in very pre-term infants. Self-heating acetate gel mattresses were introduced as a result to prevent hypothermia at birth in infants born at or below 28 weeks gestation.
Methods
A retrospective audit was conducted to evaluate the effectiveness of self-heating acetate gel mattresses at resuscitation of infants born at or below 28 weeks to prevent hypothermia at birth. All infants born at or below 28 weeks gestation during 18 months before and 18 months after self-heating acetate gel mattresses were introduced during resuscitation were included.
Results
One hundred five babies were born when acetate gel mattresses were not used, and 124 were born during the period when they were. Four (3.3%) babies were hypothermic (temperature <36°C) at admission when the mattresses were used compared to 21 (22.6%) babies who were hypothermic during the period it was not (p < 0.001). Hyperthermia (temperature >37°C) rose from 30.1% prior to use of gel mattresses to 49.6% when they were used (p = 0.004).
Conclusions
Self-heating acetate gel mattresses are highly effective in reducing admission hypothermia in infants born at or below 28 weeks gestation. The use of these mattresses is associated with a significant increase in hyperthermia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pre-term infants are at an increased risk of hypothermia at birth [17]. The reported incidence of hypothermia at birth in these babies is between 42% and 73% [9, 13, 15]. Hypothermia at birth has been associated with increased morbidity and mortality [4, 5]. Various methods have been advocated to prevent heat loss at birth in pre-term infants. These include maintaining a high ambient temperature, drying and wrapping, use of radiant warmers, skin-to-skin care, use of gamgee-lined hats, plastic bags and pre-heated mattresses [1, 3, 9, 13, 15, 17].
This study was performed at the Liverpool Women’s Hospital which is a large tertiary maternity centre in the North West of England. Since January 2005, all infant born below 30 weeks were placed in a food grade polythene bag at birth to prevent hypothermia. A large retrospective audit was conducted to assess the impact of this intervention on the rates of hypothermia at admission in these babies. There was a significant reduction in the incidence of hypothermia in infants born between 28 and 30 weeks gestation in whom admission hypothermia fell from 19.4% to 3.9% (p = 0.017) with only a marginal, non-significant reduction in infants born below 28 weeks gestation (29.3% to 24.8%, p = 0.58) [8]. As a result, self-heating acetate gel mattresses (Transwarmer®, Cooper Surgical Inc., Trumbull, CT, USA) were introduced to prevent hypothermia at birth in infants born at or below 28 weeks gestation. There are no previously published studies on the use of self-heating acetate gel mattresses for this purpose apart from a small study which was included in a recent systematic review [13]. We report the findings of retrospective audit performed to assess the effectiveness of these mattresses in preventing hypothermia in pre-term infants.
Materials and methods
Intervention
A policy of placing all infants born below 30 weeks gestation in a food grade polythene bag without drying at birth under a pre-heated resuscitaire (radiant warmer) was in place at the study centre since January 2005. The heads of these infants were covered with a knitted woollen hat immediately after placing them in the polythene bag. Holes were cut through the bag if access was needed. Prior to moving the infants to the neonatal unit, they were covered with a pre-warmed towel over the polythene bag, and the radiant warmer was disconnected from the power supply. The babies were then transported to the neonatal unit on the resuscitaire. Since October 2007, all infants born at or below a gestational age of 28 weeks placed on a pre-activated self-heating acetate gel mattress in addition to placing inside a polythene bag. The mattress is activated by breaking a metal disc incorporated in the food grade sodium acetate gel within the mattresses. This leads to an exothermic crystallisation reaction which raises the temperature of the gel. When activated at an ambient temperature between 19°C and −28°C, the mattresses achieve a peak temperature of 38–42°C within 3 min [2]. A plateau temperature is maintained for a median duration of 68 min, and then it gradually cools down [2]. The babies were transported to the neonatal unit on the resuscitaire. Once the infant is admitted to the neonatal unit and transferred into a warmed, humidified incubator, the polythene bag and the heated mattress is removed. The standard practice on the unit is to measure the axillary temperature on admission to the unit using a Sure Temp® digital thermometer (Welch Allyn, San Diego, CA, USA). Subsequently, the temperature is measured using a temperature probe incorporated in a servo-controlled incubator (Giraffe®, GE Health Care, Laurel, MD, USA). If a servo-controlled incubator is not available, the temperature is the not measured again for 4 h unless the baby is hypothermic at admission.
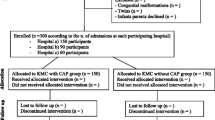
Subjects
All infants at or below 28 weeks gestation who were born at the Liverpool Women’s Hospital during 18 months before (period 1) and 18 months after (period 2) the introduction of self-heating acetate gel mattresses at resuscitation were included retrospectively. Hypothermia was defined as an admission axillary temperature less than 36°C. This standard was based on the recommendation in the Project 27/28 report published by the Confidential Enquiries into Stillbirths and Deaths in Infancy [7]. No other factors in labour room management of pre-term infants had changed over the period audited.
Data collection
Data were collected from two computer systems at the hospital: Badger 3.0 (Clevermed, UK) and Meditech (Medical Information Technology, Inc., USA). The items of data collected were gestation, gender, birth weight, mode of delivery, Apgar scores, cord pH and admission temperature.
Statistical analysis
Analysis was conducted using SPSS v16 (SPSS Inc., Chicago, IL, USA). Categorical data were analysed using the chi-square test and Fischer’s exact test where appropriate. Continuous data were analysed using the Mann–Whitney U test. A p value less than 0.05 was considered significant. Formal sample size calculation was not performed a priori. The intervention (use of self-heating mattresses) was introduced into our practice on the basis of clinical judgement. This audit was performed as a means of quality assurance.
Ethical approval
The Audit was approved by the hospital audit committee of the Liverpool Women’s Hospital.
Results
There were 105 infants born during period 1 (no mattress used) and 124 infants during period 2 (self-heating mattress used). There were no significant differences in demographic characteristics between the infants born during the two periods (Table 1). The median admission temperature was significantly higher in the infants who were born during the period when the mattresses were used (37.2°C vs. 36.6°C, p < 0.001; Fig. 1). Four (3.3%) of the infants born during the period when mattresses were used were hypothermic (axillary temperature <36°C) as compared to 21 (22.0%) of the infants in whom they were not used (p < 0.001).
Twelve (11.4%) infants born in period 1 and seven (5.6%) born in period 2 had no admission temperatures documented. There were no significant differences between the infants who had no temperatures documented compared to those with temperatures recorded (Table 2). Even if we assume that all the infants who had missing admission temperatures were normothermic (thereby reducing any effect on admission temperatures between the two groups associated with the use of the mattresses), the incidence of hypothermia in the group of infants who were placed on the self-heating mattresses would still have been significantly lower (20% vs. 3.2%, p = <0.001).
The World Health Organisation defines hyperthermia as a core temperature >37.5°C. Comparative studies in older children suggest that axillary temperature is about half a degree less than central temperature on average in the range of temperatures seen in our babies [6, 7]. Hence, we used a temperature of >37°C to define hyperthermia. Hyperthermia increased from 30.1% (period 1—no mattress used) to 49.6% (period 2—mattress used) using a definition of axillary temperature >37°C (p = 0.004; Fig. 2) and from 7.5% to 25.2% using a definition of axillary temperature of >37.5°C.
After admission to the neonatal unit, thermoregulation was maintained by nursing the babies in humidified incubators on servo control. A temperature probe was applied over the liver, and the target temperature for the servo control was 37°C. The babies’ skin temperatures were monitored continuously by this method, but the values have not been recorded in our patient data management system so it is not possible for us to tell accurately how long the hyperthermia persisted for. Axillary temperatures were measured manually by nursing staff at variable, infrequent times after admission. Of the 36 babies who had an admission temperature greater than 37.5°C, one died in the first few hours of life with fulminant Lancefield group B β-haemolytic streptococcal septicaemia. Subsequent axillary temperatures were measured in the remaining 35 babies at a median (range) of 6.75 (1.42–23.5) h. Only three babies had an axillary temperature above 37.5°C when next measured. The median (range) subsequent axillary temperature was 37°C (34.7°C to 38.3°C). Of the 17 babies who had an axillary temperature measurement within 6 h of admission, 14 were below 37.5°C. The three babies who had a temperature above 37.5°C on the measurement after the admission temperature all had an axillary temperature below 37.5°C when next measured at between 4 and 12 h later. Two of these babies survived with normal cranial ultrasound scans, and the other died early in the neonatal period with an elevated C-reactive protein although blood cultures were negative.
Discussion
The effectiveness of occlusive wrapping at birth at preventing hypothermia in pre-term babies has been shown clearly in recent randomised controlled trials and a meta-analysis [9, 12–15]. The majority of these studies were performed in infants with gestations at birth of less than 28 weeks and were found to be effective in either increasing the admission temperature or preventing hypothermia. Our experience, however, has been that, although the strategy of using polythene bags at delivery seems to have had a beneficial effect on admission temperatures for babies born between 28 and 30 weeks gestation, the benefit in infants below 28 weeks gestation has only been marginal [8]. As a consequence, a policy was introduced to use self-heating acetate gel mattresses (Transwarmer®) in addition to polythene bags at resuscitation at birth in pre-term babies born at or below 28 weeks gestation.
This study has demonstrated the effectiveness of self-heating acetate gel mattresses in preventing hypothermia at birth in pre-term infants born at or below 28 weeks gestation. In literature published on transcutaneous oxygen electrodes, it has been observed that pre-term babies can sustain skin burns at contact temperatures >42°C [11]. Theoretically, these mattresses can achieve a temperature more than 45°C when activated at high ambient temperatures [2]. Despite these concerns, none of our babies have sustained any skin burns as a consequence of using them. This is probably prevented by the relatively short period of time the babies are in contact with the heated mattress.
There was a statistically significant increase in admission hyperthermia amongst infants born during the period when self-heating acetate gel mattresses were used during resuscitation. The pyrexia seen on admission in our patients was usually transient and, we believe, not likely to be harmful in itself. Admission pyrexia can, of course, be caused by endogenous pathological processes, such as bacterial sepsis. There are concerns that endogenous perinatal fever in the context of infection and inflammation is associated with perinatal brain injury [16]. There are no published data on the effect of a brief period of iatrogenic hyperthermia on the developing brain. On the other hand, previous studies have shown a strong association between admission hypothermia and poor neonatal outcome. Hence, we continue to use the acetate gel mattresses to prevent hypothermia in very pre-term infants born at our hospital.
Self-heating gel mattresses have shown to be effective in reducing hypothermia during neonatal transport [10]. This is the single largest study which has examined the effectiveness of self-heating acetate gel mattresses in preventing hypothermia at admission in pre-term infants when used during initial resuscitation. This study has limitations of not having a randomised controlled design and using historical controls. Maternal temperature and the temperature of the delivery room are known to influence the admission temperature of pre-term babies. This study was a pragmatic audit of practice following introduction of a new policy, and hence, we did not document maternal and environmental temperature at the time of delivery. Because of the retrospective nature, it was also not known when the mattress was activated prior to placing the infant on it. During the initial phase of period 2 of the audit, there may have been a few infants who were not placed on the mattress due to oversight of attending staff. This has not been accounted for in the analysis, and the analysis was by ‘intention to treat’. But even with these limitations, we have been able to demonstrate that the use of self-heating acetate gel mattresses has been associated with the elimination of hypothermia at birth in very pre-term infants.
What is already known on this topic
-
Admission hypothermia is independently associated with increased mortality in pre-term infants.
-
Self-heating acetate gel mattresses are effective in preventing hypothermia during neonatal transport.
What this study adds
-
Self-heating acetate gel mattresses can be effectively used to reduce hypothermia at birth in very pre-term infants
References
Bergman NJ, Linley LL, Fawcus SR (2004) Randomized controlled trial of skin-to-skin contact from birth versus conventional incubator for physiological stabilization in 1200- to 2199-gram newborns. Acta Paediatr 93:779–785
Carmichael A, McCullough S, Kempley ST (2007) Critical dependence of acetate thermal mattress on gel activation temperature. Arch Dis Child Fetal Neonatal Ed 92:F44–F45
Chaput de Saintonge DM, Cross KW, Shathorn MK, Lewis SR et al (1979) Hats for the newborn infant. Br Med J 2:570–571
Confidential Enquiry into Stillbirths and Deaths in Infancy (2003) PROJECT 27/28, an enquiry into quality of care and its effect on the survival of babies born at 27–28 weeks. Maternal and Child Health Research Consortium, London
Costeloe K, Hennessy E, Gibson AT, Marlow N et al (2000) The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics 106:659–671
Craig JV, Lancaster GA, Williamson PR, Smyth RL (2000) Temperature measured at the axilla compared with rectum in children and young people: systematic review. Br Med J 320:1174–1178
Falzon A, Grech V, Caruana B, Magro A et al (2003) How reliable is axillary temperature measurement? Acta Paediatr 92:309–313
Ibrahim CPH, Yoxall CW (2009) Use of plastic bags to prevent hypothermia at birth in preterm infants—do they work at lower gestations? Acta Paedtr 98:256–260
Knobel RB, Wimmer JE Jr, Holbert D (2005) Heat loss prevention for preterm infants in the delivery room. J Perinatol 25:304–308
L'Herault J, Petroff L, Jeffrey J (2001) The effectiveness of a thermal mattress in stabilizing and maintaining body temperature during the transport of very low-birth weight newborns. Appl Nurs Res 14:210–219
Lofgren O, Jacobson L (1979) The influence of different electrode temperatures on recorded transcutaneous pO2 level. Pediatrics 64:892–897
Mathew B, Lakshminrusimha S, Cominsky K, Schroder E et al (2007) Vinyl bags prevent hypothermia at birth in preterm infants. Indian J Pediatr 74:249–253
McCall EM, Alderdice FA, Halliday HL, Jenkins JG et al (2008) Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No.: CD004210. doi:10.1002/14651858.CD004210.pub3
Vohra S, Frent G, Campbell V, Abbott M et al (1999) Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr 134:547–551
Vohra S, Roberts RS, Zhang B, Janes M et al (2004) Heat Loss Prevention (HeLP) in the delivery room: a randomized controlled trial of polyethylene occlusive skin wrapping in very preterm infants. J Pediatr 145:750–753
Wang W, Dow KE, Flavin MP (2008) Hyperthermia amplifies brain cytokine and reactive oxygen species response in a model of perinatal inflammation. Neurosci Lett 445:233–235
Watkinson M (2006) Temperature control of premature infants in the delivery room. Clin Perinatol 33:43–53
Competing interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ibrahim, C.P.H., Yoxall, C.W. Use of self-heating gel mattresses eliminates admission hypothermia in infants born below 28 weeks gestation. Eur J Pediatr 169, 795–799 (2010). https://doi.org/10.1007/s00431-009-1113-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-009-1113-y