Abstract
Background
Foreign body inhalation is a common and life-threatening emergency, and is most prevalent in young children. The traditional view is that tracheobronchial anatomy determines that an inhaled foreign body is more likely to enter the right main bronchus. This view has been challenged in young children, in whom the distribution of inhaled objects is more evenly distributed between the bronchi. We, therefore, investigated tracheobronchial anatomy relevant to foreign body inhalation in children.
Materials and methods
One hundred and fifty-six normal pediatric chest radiographs were selected from a large electronic database. Eight groups of radiographs were identified: supine (n=76) and erect; males (n=84) and females; aged <3 years (median age 12 [0.5–29] months) and ≥3 years (median age 126 [48–180] months). Tracheobronchial widths and angles were determined using a standardized technique with good reproducibility.
Results
Overall, children had a proximal right main bronchus that was consistently steeper and slightly wider than the left (P<0.001), becoming more vertical in the erect position (P=0.0001). In most children, the carina was positioned to the left of the mid-trachea, but in 34% of cases (40% of infants), it was to the right of the mid-trachea. The effects of age and gender were otherwise minimal.
Conclusion
On the basis of tracheobronchial anatomy, an inhaled foreign body is more likely to enter the right bronchial tree than the left in children of all ages. However, the variability in the position of the carina with respect to the mid-trachea may explain why this right-sided preference is less marked in children compared to adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Foreign body inhalation is a common and life-threatening emergency. Standard teaching in major anatomical [14, 17] and clinical textbooks [8, 12] is that an inhaled foreign body is more likely to enter the right main bronchus than the left because the right bronchus is wider and more vertical than the left. Some researchers have cited the greater airflow through the right lung and the position of the carina slightly to the left of the mid-trachea as additional factors predisposing to right bronchial aspiration [7, 13, 18]. However, this view has been challenged by others, who argue that, in small children (under 3 years of age), an inhaled object is at least as likely to enter the left main bronchus as the right [6, 9, 20]. An indication of how widespread this view has become is the fact that one popular textbook of pediatrics states that, contrary to popular belief, inhaled foreign bodies in young children are evenly distributed between both sides of the bronchial tree [16].
Knowing whether an inhaled object is more likely to enter the right or left main bronchus is clinically important, since the object has to be extracted via a bronchoscope to avoid the development of serious complications. The majority of inhaled foreign bodies in children are single and radiolucent, and the chest radiograph is normal in 20–35% of cases [10, 15, 18, 19]. Consequently, knowing whether the object is more likely to have gone down the right or the left main bronchus may help the bronchoscopist prioritize the search area, thereby, reducing the potential for bronchial irritation and trauma from instrumentation of the airways.
With this question in mind, we decided to investigate the anatomy of the trachea and main bronchi in children, as it relates to an inhaled foreign body. Our hypothesis was that tracheobronchial anatomy relevant to foreign body inhalation is different in children under 3 years of age compared to older children.
Materials and methods
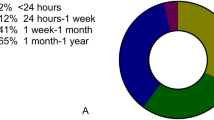
Following institutional ethical approval (REC reference 07/H1306/130), archival pediatric chest radiographs were selected from a large radiology department’s electronic image database. Only those radiographs that had previously been reported as normal by a radiologist were included. Poor quality images in which the tracheobronchial anatomy could not be clearly visualized were excluded. So too were chest radiographs that were obviously rotated, as determined by the position of the medial ends of the clavicles in relation to the vertebral column. Eight groups of chest radiographs were identified: supine and erect; males and females; aged less than 3 years or 3 years and over (Fig. 1). Appropriate images were retrieved from the database working chronologically backwards until at least 15 patients had been selected for each study group.
Figure 1 shows the measurements taken for each radiograph. These were performed using a soft-copy reporting station equipped with an EIZO RadiForce R22 (21.3-inch) medical LCD monitor and Agfa IMPAX DS3000 version 52.02.04.00 software (Agfa Healthcare, Belgium). The images were initially ‘windowed’ to allow for optimal visualization of the tracheobronchial anatomy. The images were then magnified and the tracheobronchial bifurcation outlined on screen using the software tools before taking the individual measurements (Fig. 2). The type of projection (anteroposterior or posteroanterior) was also recorded. Intra-observer variation was assessed by repeat measurements in a randomly selected sample of radiographs. All of the recorded data were anonymized.
Statistical analysis
All data were expressed as medians and ranges and analyzed using non-parametric statistical methods (Mann-Whitney two-tailed test). An intra-class correlation coefficient was calculated to assess the intra-observer consistency. Fisher’s exact test was used to compare the categorical data. Statistical significance was taken as P<0.05.
Results
A total of 156 chest radiographs were evaluated from 156 children aged less than 16 years. In 97 cases, the projection was anteroposterior, in 43 posteroanterior, and the projection was not recorded in 16 patients. One patient was noted to have a nasogastric tube in situ, one had a central venous catheter, and one a ventriculoperitoneal shunt. All chest radiographs were otherwise normal.
The results are shown in Tables 1, 2, and 3. The results in each column were derived from the original raw data of individual patients, including the ratios of right to left tracheal width and right to left main bronchi widths. Ratios were used to account for any differences in magnification related to radiographic projection. Age distributions within comparable subgroups were similar, except that in girls aged less than 3 years, erect chest radiographs were from a slightly older age group than those with supine radiographs (14 months vs. 7 months, P=0.03). While only a small number of radiographs were assessed twice (n=5), all of the measures except angle C2 showed good reliability (intra-class correlation coefficient >0.89 for tracheal dimensions, >0.94 for main bronchi, 0.81 for C1, and 0.21 for C2).
The main findings of the study were as follows:
-
1.
The position of the carina in relation to the midline of the trachea (Table 1) in most children was to the left of the midline of the trachea, as shown by a right to left tracheal ratio of >1.0. There was a trend towards a significant difference in this overall position between infants (≤1 year of age) and older children (median ratio 1.2 in infants vs. 1.4 in older children, P=0.11), but not between children younger or older than 3 years (median ratios 1.3 and 1.4, respectively, P=0.22). A striking feature of this parameter was its variability (Fig. 3); the carina was positioned to the right of the mid-trachea (right to left tracheal ratio <1.0) in 53 (34%) of all children. This applied to 35 of 111 (32%) children aged more than 1 year and 18 of 45 (40%) infants (P=0.35).
-
2.
The median width of the right main bronchus was significantly greater than the left in the study population as a whole (P=0.0002); the P-values in the male and female subgroups were 0.0007 and 0.069, respectively. The median right main bronchus to left main bronchus width ratio was remarkably consistent at about 1.1 to 1 in almost all subgroups (Table 1).
-
3.
The right main bronchus was highly significantly (P<0.001 in all cases) and consistently more vertical than the left main bronchus in all subgroups (Table 1).
-
4.
Although the right main bronchus was significantly steeper (more acute C1 angle) in children age 3 years and older compared to younger children (25° vs. 28°, two-tailed P-value =0.001) (Table 2), this finding is confounded by a slightly greater proportion of erect chest radiographs in children aged 3 years or more compared to younger children (55% and 47%, respectively; Table 1) (see point 5 below).
-
5.
There were no gender differences in the position of the carina in relation to the midline of the trachea or in the median right to left main bronchus width ratios (Table 3). Compared to girls, boys had a significantly wider trachea (P=0.02) and right main bronchus (P=0.02), but there was no significant difference in the left main bronchus widths (P=0.26). These differences were not due to differences in the proportion of posteroanterior and anteroposterior projections in boys and girls that were similar (26% posteroanterior in boys, 29% in girls). Girls had a slightly steeper C1 compared to boys (26° vs. 28°; P=0.08), but this difference was not statistically significant (Table 3).
-
6.
Regarding postural changes (Table 3), the right main bronchus was more vertical on erect radiographs than on supine films (25° vs. 30°, P<0.0001), but no other parameters were significantly different with posture. This right main bronchus postural change was evident from an early age; in the infant group, there were 15 erect chest radiographs with a median C1 angle of 26° compared to 30 supine radiographs with an angle of 32° (P=0.047).
Discussion
Choking on foods is a major cause of accidental death. In the year 2000 in the United States, inhaled or ingested foreign bodies accounted for more than 17,000 emergency department visits and 160 deaths from respiratory obstruction in children aged 14 years or younger [4]. Children under 3 years of age account for the majority of cases. Reasons for this include the lack of molar teeth and poorer mastication, a tendency to put things in the mouth, crying, running, or playing with objects in the mouth, and less mature protective laryngeal reflexes [2, 3, 6, 20].
In adults, more than 70% of inhaled foreign bodies are found in the right main bronchus [5, 22]. Although this is usually stated to be because the right main bronchus is significantly wider and steeper than the left main bronchus, the position of the carina to the left of the mid-trachea may be a much more important factor, since this increases the ‘catchment area’ of the right main bronchus. In one study in 25 adult cadavers, the carina was positioned to the left of the mid-trachea in 21 (84%) cases [13]. In children, some larger studies of inhaled foreign bodies also report a preference for right-sided aspiration [2, 3, 10, 18, 21]. Nevertheless, others document an equal distribution between right and left bronchi [1], and still others a preference for the left bronchial system [6, 9]. Few of these reports have analyzed the effect of age on the distribution of inhaled foreign bodies in children. One exception, a retrospective study of 96 children undergoing bronchoscopy for foreign body aspiration [20], found no significant difference in the right to left bronchial distribution of objects in children less than 3 years of age compared to a right-sided bronchial preference in children aged more than 3 years. Despite this report, a summary of recent larger studies (Table 4) shows an overall right-sided bronchial predisposition in children of all ages [1, 2, 10, 19, 20]. The key difference in young children appears to be the greater variability in the right to left distribution pattern compared to adults.
Our study does not support the hypothesis that tracheobronchial anatomy relevant to foreign body inhalation is significantly different in children under 3 years of age compared to older children. We confirm that children have a proximal right main bronchus that is consistently steeper and wider than the left. We have also shown, for the first time in children, that the carina is usually positioned to the left of the midline of the trachea, as in adults. Thus, an inhaled foreign body progressing beyond the trachea in a child would be expected to pass down the right main bronchus more often than the left. Inhaling a foreign body in the erect position may increase this tendency because the right main bronchus is even more vertical with upright posture. However, if the position of the carina is the most critical factor in determining the distribution of an inhaled foreign body, as suggested by one study [13], then the position of the carina to the right of the mid-trachea in one third of all children (and an even higher proportion of infants) could account for the wide variations in the distribution of inhaled foreign bodies reported in different pediatric series.
Other factors, some of which are non-anatomical, might also contribute to this observed variability in small children. Some of these, such as the size, shape, and density of the object, have not been studied in detail. Daniilidis et al. [9] suggested that the preference for the left main bronchus found in their study might be due to inhalation in the supine position, with the child holding the object in the right hand, thereby, straightening the angle between the trachea and the left main bronchus. Whilst there is some evidence to suggest that the head position in neonates may affect bronchial angles [11], there is no other support for this theory. Van Looij et al. [20] offered an alternative explanation to account for the equal bronchial distribution of inhaled foreign bodies observed in children aged less than 3 years in their series. They considered that most parents react to a choking child by holding the prone toddler head-down over their left arm and giving back blows. This posture tilts the child to the left side and might encourage an inhaled object to move into the left bronchus.
Our study has some limitations, which we attempted to minimize. Paired erect and supine chest radiographs from individual patients were not available, but the study groups were matched for age and sex. Chest radiographs with pathologies that could affect our overall results were excluded. We avoided the use of computed tomographic scans because these are often performed under general anesthesia with endotracheal intubation and hyperinflation of the lungs in small children. Intra-observer reproducibility was evaluated and found to be high for most measurements. We did not examine the inter-observer accuracy, preferring instead to adopt a consistent approach by using one investigator. Although differences in the radiographic projections could have affected absolute measurements, most of the critical parameters in this study were either calculated ratios or measured angles, neither of which should be affected by this factor. Only tracheobronchial widths were measured; a circular cross section would have to be assumed for these to represent diameters. Finally, there was no control for the degree of inspiration on chest radiographs, but any errors related to this are likely to be random in all patient groups and, to some extent, compensated for by the sample size.
References
Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO (1999) Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 115:1357–1362
Brkić F, Umihanić S (2007) Tracheobronchial foreign bodies in children. Experience at ORL clinic Tuzla, 1954–2004. Int J Pediatr Otorhinolaryngol 71:909–915
Cataneo AJ, Reibscheid SM, Ruiz Júnior RL, Ferrari GF (1997) Foreign body in the tracheobronchial tree. Clin Pediatr (Phila) 36:701–705
Center for Disease Control and Prevention (CDC) (2002) Nonfatal choking-related episodes among children—United States, 2001. MMWR Morb Mortal Wkly Rep 51:945–958
Chen CH, Lai CL, Tsai TT, Lee YC, Perng RP (1997) Foreign body aspiration into the lower airway in Chinese adults. Chest 112:129–33
Cohen SR, Lewis GB Jr, Herbert WI, Geller KA (1980) Foreign bodies in the airway. Five-year retrospective study with special reference to management. Ann Otol Rhinol Laryngol 89:437–442
Cohen BS, Sussman RG, Lippmann M (1993) Factors affecting distribution of airflow in a human tracheobronchial cast. Respir Physiol 93:261–278
Cotton RT, Rutter MJ (2006) Foreign body aspiration. In: Chernick V, Boat TF, Wilmott RW, Bush A (eds) Kendig’s disorders of the respiratory tract in children, 7th edn. Elsevier Saunders, Philadelphia, pp 610–615
Daniilidis J, Symeonidis B, Triaridis K, Kouloulas A (1977) Foreign body in the airways: a review of 90 cases. Arch Otolaryngol 103:570–573
Divisi D, Di Tommaso S, Garramone M, Di Francescantonio W, Crisci RM, Costa AM, Gravina GL, Crisci R (2007) Foreign bodies aspirated in children: role of bronchoscopy. Thorac Cardiovasc Surg 55:249–252
Fewell J, Arrington R, Seibert J (1979) The effect of head position and angle of tracheal bifurcation on bronchus catheterization in the intubated neonate. Pediatrics 64:318–20
Landsman IS, Werkhaven JA, Motoyama EK (2006) Anesthesia for pediatric otorhinolaryngologic surgery. In: Motoyama EK, Davis PJ (eds) Smith’s anesthesia for infants and children, 7th edn. Mosby Elsevier, Philadelphia, p 816
Lowe D, Russell RI (1984) Tracheobronchial foreign bodies—the position of the carina. J Laryngol Otol 98:499–501
Moore KL, Dalley AF (2005) Clinically oriented anatomy, 5th edn. Lippincott, Williams & Wilkins, Philadelphia, p 126
Mu L, He P, Sun D (1991) Inhalation of foreign bodies in Chinese children: a review of 400 cases. Laryngoscope 101:657–660
Robinson MJ, Roberton DM (eds) (2003) Practical paediatrics, 5th edn. Churchill Livingstone, Edinburgh, pp 479 and 481
Standring S (ed) (2005) Gray’s anatomy: the anatomical basis of clinical practice, 39th edn. Elsevier/Churchill Livingstone, Philadelphia, pp 1075–1076
Tan HKK, Brown K, McGill T, Kenna MA, Lund DP, Healy GB (2000) Airway foreign bodies (FB): a 10-year review. Int J Pediatr Otorhinolaryngol 56:91–99
Tokar B, Ozkan R, Ilhan H (2004) Tracheobronchial foreign bodies in children: importance of accurate history and plain chest radiography in delayed presentation. Clin Radiol 59:609–615
Van Looij MAJ, Rood PPM, Hoeve LJ, Borgstein JA (2003) Aspirated foreign bodies in children: why are they more commonly found on the left? Clin Otolaryngol Allied Sci 28:364–367
Wiseman NE (1984) The diagnosis of foreign body aspiration in childhood. J Pediatr Surg 19:531–535
Zissin R, Shapiro-Feinberg M, Rozenman J, Apter S, Smorjik J, Hertz M (2001) CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol 11:606–611
Acknowledgment
We wish to thank Dr. Baran Tokar of the Eskisehir Osmangazi University Faculty of Medicine, Turkey, for kindly providing the supplementary data from his publication cited in Table 4.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding: none.
Rights and permissions
About this article
Cite this article
Tahir, N., Ramsden, W.H. & Stringer, M.D. Tracheobronchial anatomy and the distribution of inhaled foreign bodies in children. Eur J Pediatr 168, 289–295 (2009). https://doi.org/10.1007/s00431-008-0751-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-008-0751-9