Abstract
Pediatric HIV-1 infections are still being diagnosed in France, despite the efficacy of prophylactic treatment to prevent mother-to-child transmission. To describe the characteristics and mode of infection of these children, we retrospectively analysed data of 59 children diagnosed with the HIV-1 infection between January 2000 and June 2005 in a Parisian university hospital. Twenty of these children had been born in France, and none had received appropriate prophylaxis (insufficient, not taken or given too late). Six received no preventive treatment due to failures in screening: three mothers were HIV-seronegative at the start of pregnancy and no test was carried out for the other three. At diagnosis, four had a severe immune deficiency (CD4 cells <15%). The 39 children born abroad were diagnosed at a median age of 3 years (range: 3 months–16 years), sometimes several years after their arrival in France. The clinical, virological and immunological status of these children was poorer than that of the children born in France: 18 had less than 15% CD4 cells. In contrast, the response to treatment of the children born in France was not as good as that of the children born abroad. The HIV-1 screening and prevention programme for pregnant women could be improved. Some children infected following the failure of prevention are at high risk of subsequent treatment failure. HIV-1 infection should be taken into consideration in children born in countries with a high prevalence of HIV, even if they have been living in France for several years and present no symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The risk of HIV transmission from mother to child is now only 1–2% in Western countries due to the prophylactic use of antiretroviral drugs during pregnancy and the administration of these drugs to the baby during the first 6 weeks of life [1, 20]. Given the potential gravity of the disease and the efficacy of prevention, most countries have an active HIV-1 screening programme for pregnant women [5]. In France, doctors are legally obliged to offer HIV tests during the mandatory prenuptial consultation and/or during the first obstetric consultation during pregnancy [19]. While this screening policy has not been evaluated with any great degree of precision at the national level, it appears to be accepted and effective, such that the problem of HIV-1 infection in children is now widely considered to be under control. However, new cases of HIV-1 infection in children are regularly identified. These cases involve both children born in France for whom the prevention programme has failed and children born abroad, some of whom have been living in France for years before the diagnosis is made, sometimes at a very advanced stage of infection. The persistence over time of the number of such cases in our centres led us to investigate the circumstances in which infection and diagnosis occur. This may allow complementary preventive or therapeutic actions to be suggested.
Patients and methods
We retrospectively analysed all of the medical files of children younger than 18 years of age who had been diagnosed with HIV-1 infection between January 2000 and June 2005 and had regular follow-ups at Necker Enfants-Malades Hospital. The file of one young adult, who underwent a blood transfusion in 1984 and was diagnosed in 2002 at the age of 18 years, was not included in the analysis. The diagnosis of an HIV mother-to-child transmission was based – at the very latest – on the mother's positive HIV serology at the time of delivery. For orphaned children born abroad, circumstances of the mother's death were collected when possible. A nosocomial infection was presumed when the serology of the mother was negative and the child did not receive transfusion. Prophylaxy strategy for each mother who delivered in France was re-analysed within the framework of the latest French recommendations [19]. In brief, these guidelines state that an adequate prevention therapy must be initiated before the 34th week of pregnancy, with zidovudine monotherapy restricted to the mother with a plasma viral load of less than 1000 copies/ml. In this case, it must be associated with cesarean section. We subjectively assessed non-adherence to an adequate prescription on the basis of the obstetrical team report and persistent detectable viral load after the treatment. Antiviral use in infected children followed international guidelines [21] and always consisted of a combination of at least three molecules of two different classes. Plasma viral load was assessed each month until undetectable, then every 3 months according to the same guidelines. Virological success was defined as a viral load of less than 50 copies/ml.
Results
We identified 59 HIV-infected children who had been diagnosed during the study period. In this same time interval, the total number of HIV-infected children followed in our centre was around 300. As a tertiary university referral centre for the Paris area, recruitment is not limited to the local maternity unit. Although the numbers are not precisely known, indirect indicators suggest that the number of cases represents roughly one-half of the HIV-infected children in the region and one-quarter of the HIV-positive paediatric population at the national level.
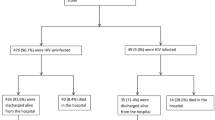
Children born in France
Of the 59 children newly diagnosed as being infected with HIV-1, 20 (nine girls, 11 boys) were born in France (five diagnosed in 2,000, three each in 2001 and 2002, four in 2003, five in 2004 and none in 2005). In all cases, the infection had clearly been transmitted from mother to child. All of the mothers of these children were themselves infected with HIV-1. Of the 20 mothers, six had not been identified by screening during pregnancy and their infection was discovered only after the birth, when the child was found to be infected; three of these six women had tested negative at the start of pregnancy and probably undergone subsequent seroconversion during the pregnancy. All of the remaining 14 women found to be seropositive before or during pregnancy received prophylaxis. Retrospectively, this treatment could be classified as having been given too late (initiated after the 34th week of pregnancy,n=4), as being unsuitable (zidovudine monotherapy when rates of viral replication were too high for the therapy to be effective,n=2) or poorly/not taken (n=8) (Table 1). Diagnosis of HIV infection in the children was made in the first few weeks of life for 17 children and at 8, 12 and 12 months for the remaining three children, respectively. At the time of diagnosis, 13 children had few or no symptoms (CDC stage N or A), four children had moderate symptoms (stage B) and three children (who were diagnosed late) already had AIDS (CDC stage C). Two children were in poor nutritional condition, with body weights more than two standard deviations below the mean for their age. The immune status of the children was assessed at the time of diagnosis: 12 had more than 25% CD4 (CDC I), four had 15–25% CD4 (CDC II) and four had severe immunodeficiency, with less than 15% CD4 (CDC III). At the time of this analysis, 18 of the children were on antiretroviral multitherapy. Only six of the 15 children with at least a 6-month follow-up had undetectable levels of viral replication (<50 copies of viral RNA/ml).
Children born abroad
A total of 39 children (18 girls and 21 boys) born outside France were diagnosed with HIV-1 infection during the same period (six in 2000, five each in 2001 and 2002, nine in 2003, nine in 2004 and five in 2005). Most originated from Sub-Saharan Africa (n=27), with the others coming from South-East Asia (n=4), South America (n=2), Haiti (n=2), Europe (n=2), North Africa (n=1) or the United States (n=1). The median age of the children at diagnosis was 3 years (3 months–16 years), and diagnosis was made at a median of 4.5 months (1 month–7 years) after arrival in France. Eleven children were diagnosed with the HIV-1 infection before their arrival in France. Five children had already received antiretroviral treatment; most of these children were from Europe and North America. The mode of transmission could not be established with certainty for these children. Mother-to-child transmission had clearly occurred in 35 of these children and had probably occurred in the remaining three. Nosocomial transmission was suspected, on reasonable grounds, in one case. At the time of diagnosis, 17 of the children had few or no symptoms (CDC stage N or A), two had moderate symptoms (CDC stage B) and 20 already had AIDS (CDC stage C), including one child who died from an opportunistic infection shortly after diagnosis. Twelve of the children had a poor nutritional status, with body weights two standard deviations below the mean for their age. Immune status was normal in ten children (>25% CD4; CDC I) and moderately poor in 11 (between 15 and 25% CD4; CDC II), but 18 children had severe immunodeficiency (<15% CD4) at the time of diagnosis. At the time of the analysis, 27 children were on multitherapy. Plasma viral load was undetectable (<50 copies of viral RNA/ml) for 15 of the 22 children with at least a 6-month follow-up.
Discussion
Between 10 and 15 children are diagnosed with HIV-1 infection at our centre each year. Although this observation has no statistical value at the national scale, this phenomenon merits further consideration and analysis. However, because this report is an uncontrolled case series, it is primarily descriptive and hypothesis-generating. Our observations are not consistent with the widely held view that the paediatric dimension of the HIV-1 epidemic has been brought under control in Europe – and in France in particular – since the introduction of an effective prevention programme. We have identified two distinct aspects to the problem of successfully meeting the challenge of paediatric HIV-1 infection, each requiring different responses.
The first is the failure to prevent mother-to-child HIV-1 transmission to children born in France. The frequency of these failures has yet to be precisely evaluated, given that about 1500 HIV-1-infected women give birth in France each year [22]. Various factors are responsible for these failures, the most frequent of which is insufficient antiretroviral treatment due to poor compliance on the part of the woman, the treatment being initiated too late in the pregnancy due to the late detection of HIV infection in the mother and/or the inappropriate prescription of monotherapy despite high levels of viral replication in the mother. It is now well established that a combination of antiviral drugs for a sufficiently long period of time is necessary to reduce the transmission rate to less than 1–2% [1, 2, 4, 7, 9, 13, 15]. For the children described here, scrupulous compliance with national or international recommendations for the prevention of mother-to-child transmission would probably have been sufficient to prevent infection. The potential efficacy of a combined treatment in the newborn at high risk of infection (i.e. mother insufficiently treated, complicated vaginal delivery) is not proven. Poor maternal adherence to the treatment could be detected by frequent evaluations of viral load during treatment. Unlike other potential foetal risks, the risk of HIV-1 transmission does not always lead to the optimal multidisciplinary follow-up of high-risk pregnancies and possible hospital admission for the administration of treatment for the mother or the child. Stronger preventive treatment for the child, in the form of bi- or tritherapy, is difficult to administer, particularly if the psychological, social and/or administrative context is unfavourable; this could also justify the use of different care structures, such as care at home or conventional hospitalisation [12].
True screening failure seems rare. Although never precisely evaluated, the current screening policy practiced in France is generally well applied and accepted by pregnant women. We observed several cases of probable seroconversion during pregnancy in women initially testing HIV-1-negative. It is clearly important to bear this possibility in mind and to repeat the test in women with a high exposure to the risk, particularly those having sexual relations with partners highly exposed. The efficacy and cost effectiveness of different screening strategies have been published [3, 5, 6, 11, 18, 23]. Data are not necessarily comparable from a country to another since individual or societal acceptance rates can be very different. To our knowledge, the cost effectiveness of repeated testing has not be evaluated in industrialised country.
The second aspect of the problem, and one which will probably become more important over the coming years, concerns the diagnosis of infected children born outside of France. The magnitude of the worldwide epidemic is considerable. The WHO estimates that 1500–2000 children worldwide are infected every day, mostly in Sub-Saharan Africa. However, some of the foreign-born children described here had lived in France for several years and gradually progressed to AIDS without the HIV-1 infection being diagnosed. These children therefore lost some of the benefits of multitherapy. The potential loss of efficacy of antiretroviral treatment initiated too late is widely recognised. It would be beneficial to offer screening tests for HIV-1 infection on a wider basis to children originating from countries in which HIV prevalence is high, even for children with few or no symptoms. While this test is often offered to children arriving as part of an international adoption procedure [10, 16], it should be expanded to children entering the country to live with their own family, given the very good therapeutic options currently available [8, 17, 21].
The therapeutic results with children of foreign origin may be considered to be satisfactory in terms of the results for multitherapy in children overall [8, 17, 21]. However, the same cannot be said for infected children born in France after the failure of prophylaxis. The formal comparison of these two groups of children was impossible because ages at diagnosis and at treatment differed between the groups, but such a comparison would be to the disadvantage of children born abroad who were diagnosed later and who often have the disease in an advanced state. However, virological results for children born in France are mediocre compared to what might be expected from multitherapy: less than half of the paediatric patients had plasma viral loads below the detection threshold after 6 months of treatment. Although we cannot provide precise details about the causes of this treatment failure, it seems likely that the particular conditions leading to the failure of prevention during pregnancy also lead to a comparative treatment failure in the child. In an earlier investigation carried out at the national level, we identified several indices suggesting that untreated women were often socially marginalised [14]. These factors could be also associated with treatment failures in their infected children and should be anticipated in order to increase compliance, thereby optimising the antiretroviral treatment.
References
Abrams EJ (2004) Prevention of mother-to-child transmission of HIV-successes, controversies and critical questions. AIDS Rev 6:131–143
Castilla J, Del Romero J, Hernando V, Marincovich B, Garcia S, Rodriguez C (2005) Effectiveness of highly active antiretroviral therapy in reducing heterosexual transmission of HIV. J Acquir Immune Defic Syndr 40:96–101
Chou R, Smits AK, Huffman LH, Fu R, Korthuis PT, US Preventive Services Task Force (2005) Prenatal screening for HIV: A review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 143:38–54
Cooper ER, Charurat M, Mofenson L, Hanson IC, Pitt J, Diaz C, et al (2002) Women and Infant’s Transmission Study Group. Combination antiretroviral strategies for the treatment of pregnant HIV-1-infected women and prevention of perinatal HIV-1 transmission. J Acquir Immune Defic Syndr 29:484–94
del Rio C, U.S. Preventive Services Task Force (2005) New USPSTF guidelines on HIV screening. AIDS Clin Care 17:74
European Collaborative Study (2003) Pregnancy-related changes in the longer-term management of HIV-infected women in Europe. Eur J Obstet Gynecol Reprod Biol 111:3–8
European Collaborative Study (2005) Mother-to-child transmission of HIV infection in the era of highly active antiretroviral therapy. Clin Infect Dis 40:458–465
Foster C, Lyall EG (2005) Children with HIV: improved mortality and morbidity with combination antiretroviral therapy. Curr Opin Infect Dis 18:253–259
Hawkins D, Blott M, Clayden P, de Ruiter A, Foster G, Gilling-Smith C, et al (2005) BHIVA Guidelines Writing Committee. Guidelines for the management of HIV infection in 12 pregnant women and the prevention of mother-to-child transmission of HIV. HIV Med 6[Suppl 2]:107–148
Jenista JA (2005) Special topics in international adoption. Pediatr Clin North Am 52:1479–1494
Kelly KA, Harrison CH (2004) Universal prenatal HIV screening: patient attitudes and perceptions. Women Health 40:41–57
King SM; American Academy of Pediatrics Committee on Pediatric AIDS; American Academy of Pediatrics Infectious Diseases and Immunization Committee (2004) Evaluation and treatment of the human immunodeficiency virus-1-exposed infant. Pediatrics 114:497–505
Loutfy MR, Walmsley SL (2004) Treatment of HIV infection in pregnant women: antiretroviral management options. Drugs 64:471–488
Mayaux MJ, Teglas JP, Blanche S, French Pediatric HIV Infection Study Group (2003) Characteristics of HIV-infected women who do not receive preventive antiretroviral therapy in the French Perinatal Cohort. J Acquir Immune Defic Syndr 34:338–343
Morris AB, Dobles AR, Cu-Uvin S, Zorrilla C, Anderson J, Harwell JI, Keller J, Garb J (2005) Protease inhibitor use in 233 pregnancies. J Acquir Immune Defic Syndr 40:30–33
Murray TS, Groth ME, Weitzman C, Cappello M (2005) Epidemiology and management of infectious diseases in international adoptees. Clin Microbiol Rev 18:510–520
Neely M, Kovacs A (2004) Management of antiretroviral therapy in neonates, children, and adolescents. Curr HIV/AIDS Rep 1:97–104
Pearlman DN, Averbach AR, Zierler S, Cranston K (2005) Disparities in prenatal HIV testing: evidence for improving implementation of CDC screening guidelines. J Natl Med Assoc 97[Suppl 7]:44S–51S
Prise en charge thérapeutique des personnes infectées par le VIH. Recommandations du groupe d.experts http://www.sante.gouv.fr/htm/actu/delfraissy_2004/rapport.pdf
Public Health Service Task Force Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV-1 Transmission in the United States – November 17, 2005 http://aidsinfo.nih.gov/ContentFiles/PerinatalGL.pdf
Sharland M, Blanche S, Castelli G, Ramos J, Gibb DM, PENTA Steering Committee (2004) PENTA guidelines for the use of antiretroviral therapy, 2004. HIV Med 5:61–86
Surveillance de l.infection à VIH-SIDA en France, 2003–2004. Bulletin Epidémiologique Hebdomadaire 2005;46–47:230–2 (http://www.invs.sante.fr/beh/2005/46_47/beh_46_47_2005.pdf)
Wortley PM, Lindegren ML, Fleming PL (2001) Successful implementation of perinatal HIV prevention guidelines. A multistate surveillance evaluation. MMWR Morb Mort Wkly Rep 11,50(RR-6):17–28
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Macassa, E., Burgard, M., Veber, F. et al. Characteristics of HIV-infected children recently diagnosed in Paris, France. Eur J Pediatr 165, 684–687 (2006). https://doi.org/10.1007/s00431-006-0091-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-006-0091-6