Abstract
Central venous devices are frequently used in children to monitor haemodynamic status, to administer fluids, medication, parenteral nutrition and for blood sampling. Life-threatening complications that may occur on insertion if the central venous catheter (CVC) is misplaced, are cardiac tamponade or a hydro-/haemopericardium. There is still controversy over the optimum catheter tip position in paediatric patients, whether to place the CVC tip in the superior vena cava, outside the pericardial boundaries or in the right atrium. However, the exact location of the pericardium cannot be seen on a normal chest x-ray. The carina is a radiographic marker for CVC placement, suggested on the basis of studies with conserved and fresh adult cadavers. In order to confirm this landmark for children, the present study was performed with 31 fresh cadavers of small children (mean age 12.5±3.4 months) that had been selected for autopsy in the Institute of Legal Medicine. Results clearly demonstrate that the carina was 0.5±0.04 cm above the pericardial duplication as it transversed the SVC. In no infant cadaver was the carina inferior to the pericardium. Thus, the results are analogous to those in adults and confirm that the carina is a simple anatomical-radiological landmark, superior to the pericardial reflection, that can be used to identify the placement of CVC even in newborn and small children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central venous catheterisation is a routine procedure in daily intensive therapy, e.g. to measure central venous pressure, to administer fluids and medication or for blood sampling. Furthermore, the widespread use of central venous catheters (CVC) has increased in children (and adults) with chronic illnesses that require long-term parenteral nutrition [6, 12]. However, the migration and dislocation of CVC can be a life-threatening complication [4, 13, 16]. Cardiac tamponade after CVC placement, first reported in 1956, is one of the most serious complications [2]. With the increased use of CVC in neonatal and infant intensive therapies, there have been some case reports of fatal complications, such as intrapericardial infusion associated with parenteral nutrition [11, 12, 20]. In addition to fatal pericardial tamponade, the tip of the catheter can perforate great veins such as the superior vena cava (SVC) or the myocardium of the right heart [3, 9, 10, 15]. Other complications both in adults and children are sepsis, vessel perforations, and hydro-, haemo- or pneumothorax [7, 14, 19]. In addition, Suarez-Penaranda et al. [18] reported an unexpected death from coronary sinus thrombosis after a direct trauma of the coronary endothelium in relation to a malpositioned CVC. During insertion, the localisation of the CVC can be estimated by marks on the catheter or by ECG guidance. The final position of the catheter tip should be located in the lower superior vena cava or in the upper right atrium, checked by x-ray to avoid complications. In the last few years, various helpful radiographic landmarks for safe positioning have been described [3, 5, 8, 15]. Schuster et al. [17] suggested the carina as a reliable radiographic marker for the correct placement of CVC, based on the examination of formalin-conserved cadavers. Albrecht et al. [1] confirmed these results by investigating fresh adult cadavers. The present study was performed to systematically identify and confirm this simple and reliable radiographic landmark in fresh infant cadavers with smaller anatomical dimensions, enabling a safer CVC placement in newborn and small children also.
Materials and methods
Thirty-one subjects (20 females and 11 males; infants not born prematurely; no anomalies of the heart and the great vessels) undergoing forensic autopsy were investigated. The causes of death were varied: SIDS (sudden infant death syndrome), intoxication, septic shock, central paralysis. The autopsies were carried out within 72 h postmortem and excluded cadavers with signs of advanced autolysis. All examinations were carried out by one person (K. A.) to guarantee reproducible results. The mean age at the time of death was 12.5±3.4 months (mean±SEM; range: stillborn–60 months) and the mean body length was 67.2±3.3 cm (range: 47 cm–108 cm). The investigated cadavers were subdivided into three groups: 47–57 cm (n=11), 58–68 cm (n=11) and >68 cm (n=9).
After incision of the skin, the rib cage was opened by keeping the pericardium intact; the sternum, the medial parts of the ribs and the thymus gland were removed and a lambda-shaped incision was made in the pericardial sac. Great care was taken to avoid any stretching effects of the heart, the blood vessels and the soft tissue. Initially, the anatomical dimensions of the intrapericardial part of the SVC and the medial side of the vessel, where a reflection of the pericardium strengthens the vessel wall, were measured in situ, then the thoracic organs (tongue, the organs of the neck, heart and lungs) were removed en bloc. While observing these organs from the dorsal view, the carina was palpated and a cannula was inserted and pushed anteriorly towards the carina. Afterwards the organs were turned to inspect the ventral aspect and the distance was measured between the cannula tip (at a right angle) and the pericardium where it transversed the SVC (Fig. 1).
Autopsy: male infant, 55 d, cause of death: sudden infant death syndrome (SIDS). The heart, great blood vessels and opened pericardium: A intrapericardial part of the superior vena cava, B medial side of the superior vena cava, attached to the pericardium, C longitudinal distance between the carina and the pericardium as it transverses the superior vena cava. The anatomical location of the carina is shown by dotted lines. Black arrows indicate small epicardial bleedings, often occurring in sudden infant death syndrome. * Superior vena cava, P pericardium, Aa ascending aorta, ra right atrium, la left atrium, rvright ventricle, lv left ventricle, Ac apex of the heart, Ptpulmonary trunk
Data are expressed as means±SEM (standard error of the mean). Differences between the four age groups were examined for statistical significance using Student's t-test for unpaired data and one-way ANOVA. A value of p<0.05 was assumed to be significant.
Results
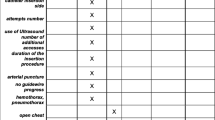
The duplication of the pericardium crossed the SVC at a diagonal to horizontal angle (range 0–15°). The pericardium was fixed to the medial wall of the SVC up to the beginning of the aortic arch, near to the brachiocephalic trunk. The intrapericardial part of the SVC (A in Fig. 1) was 1.7±0.1 cm (range 0.4–2.8 cm). The length of the medial side of the SVC, fused with the pericardium (B in Fig. 1), was 1.0±0.1 cm (range 0.3–2.0 cm). The carina was located at a distance of 0.5±0.04 cm (range 0.2–1.0 cm) above the pericardial reflection (C in Fig. 1). In no case was the carina located below the pericardial reflection on the medial side of the SVC. Figure 2 shows the relation between the body length of the children and the three measured distances. The maximum distance from the carina to the beginning of the medial side of the SVC attached to the pericardium (the difference between B and C) was 1.0 cm.
Body length-dependent distances (A–C; see Fig. 1) in fresh infant cadavers. Significant differences between the groups are indicated by *, p<0.01
Discussion
CVC insertion is a common procedure in modern medicine. However, complications may occur during catheter insertions. To prevent such fatal complications, especially cardiac tamponade, many suggestions have been published to prevent the displacement of CVC [8, 17]. Most studies were based on clinical investigations and analysis of x-rays of the chest, such as the verification of the sixth thoracic vertebral level as a safe fluoroscopic landmark [5]. However, the pericardium cannot be seen on radiographic images, thus visible landmarks are needed to allow reliable radiographic validation of adequate positioning. In adults, Schuster et al. [17] showed, and Albrecht et al. [1] confirmed, that the carina can be used as a landmark because in all the investigated adult formalin-conserved and fresh cadavers, the pericardial boundaries crossed the SVC below this cartilaginous part of the bifurcation of the trachea point, which can be reliably seen on standard x-rays. The placement of the CVC tip outside the pericardium will avoid perforation of the intrapericardial part of the SVC or the right atrium or ventricle. Thus, radiological confirmation that the CVC tip is above the level of the carina reduces the risk of pericardial perforation.
To date, information on anatomical-radiological landmarks for the safe placement of CVC in children is rare. The present study was performed to investigate whether the carina is also valid for newborn and small children, though there might be a difficulty in viewing the carina in some cases. The three distances described in the studies by Schuster et al. [17] and Albrecht et al. [1] were measured and the results confirmed the previous investigations in adults. Naturally, smaller distances were found; however, in all cases the pericardial boundaries were below the border of the carina [0.3 cm in children with a body length of 47 cm–57 cm, 0.5 cm in children with a body length of 58 cm–68 cm and 0.6 cm in children with a body length of >68 cm (compared to 0.8 cm in adults)]. Thus, to position the CVC safely, the catheter tip should be localised at least 0.5 cm (BL: 47–57 cm) and 1 cm (BL: 58–108 cm) above the carina (4 cm in adults [1]). A recent study of Yoon et al., who investigated 57 right internal jugular vein catheterisations in infants and children with help of transoesophageal echocardiography and chest radiographs, confirmed our results [21].
Although, the radiographic diagnosis may be more difficult in children (e.g. because of a large thymus gland) this study confirms the carina as a safe radiographic landmark in CVC placement even in small children. Rare but life-threatening complications such as pericardial tamponade or hydropericardium after insertion of an CVC will decrease if all catheter tips are localised above the carina on chest x-rays. In future studies, the findings that were measured here in autopsies should be verified with x-rays taken from infants that are alive.
Abbreviations
- CVC:
-
Central venous catheter
- SVC:
-
Superior vena cava
- SIDS:
-
Sudden infant death syndrome
- BL:
-
Body length
References
Albrecht K, Nave H, Breitmeier D, Panning B, Tröger HD (2004) Applied anatomy of the superior vena cava - the carina as a landmark to guide central venous catheter placement. Brit J Anaesth 92:75-77
Brown CA, Kent A (1956) Perforation of right ventricle by polyethylene catheter. South Med J 49:466-467
Collier PE, Goodman GB (1995) Cardiac tamponade caused by central venous catheter perforation of the heart: a preventable complication. J Am Coll Surg 181:459-463
Collier PE, Blocker SH, Graff DM, Doyle P (1998) Cardiac tamponade from central venous catheters. Am J Surg 176:212-214
Connolly B, Mawson JB, MacDonald CE, Chait P, Mikailian H (2000) Fluoroscopic landmark for SVC-RA junction for central venous catheter placement in children. Pediatr Radiol 30:692-695
Dollery CM, Sullivan ID, Bauraind O, Bull C, Milla PJ (1994) Thrombosis and embolism in long-term central venous access for parenteral nutrition. Lancet 344:1043–1045
Flatley ME, Schapira RM (1993) Hydromediastinum and bilateral hydropneumothorax as delayed complications of central venous catheterization. Chest 103:1914–1916
Fletcher SJ, Bodenham AR (2000) Safe placement of central venous catheters: where should the tip of the catheter lie? Br J Anaesth 85:188–191
Hayden L, Steward GR, Johnson DC, Fisher MM (1981) Transthoracic right atrial cannulation for total parenteral nutrition-case report. Anaesth Intens Care 9:53–57
Hunt R, Hunter TB (1988) Cardiac tamponade and death from perforation of the right atrium by a central venous catheter. Am J Roentgenol 151:1250
Leibovitz E, Ashkenazi A, Levin S, Nissim F (1988) Fatal pericardial tamponade complicating total parenteral nutrition via a silastic central vein catheter. J Pediatr Gastroenterol Nutr 7:306–307
Marcoux C, Fisher S, Wong D (1990) Central venous access devices in children. Pedriatr Nurs 16:123–133
Quiney NF (1994) Sudden death after central venous cannulation. Can J Anaesth 41:513–515
Raad II, Khalil SM, Costerton JW, Lam C, Bodey GP (1994) The relationship between the thrombotic and infectious complications of central venous catheters. JAMA 271:1014–1016
Rutherford JS, Merry AF, Occleshaw CJ (1994) Depth of central venous catheterization: an audit of practice in a cardiac surgical unit. Anaesth Intens Care 22:267–271
Schneider V, Maxeiner H (1983) Herzbeuteltamponade durch zentralen Venenkatheter. In: Barz J, Bösche J, Frohberg H, Joachim H, Käppner R, Mattern R (eds) Fortschritte der Rechtsmedizin – Festschrift für Georg Schmidt. Springer, Berlin, Heidelberg, New York, pp 116–122
Schuster M, Nave H, Piepenbrock S, Pabst R, Panning B (2000) The carina as a landmark in central venous catheter placement. Br J Anaesth 85:192–194
Suarez-Penaranda JM, Rico-Boquete R, Munoz JI, Rodriguez-Nunez A, Martinez Soto MI, Rodriguez-Calvo M, Concheiro-Carro L (2000) Unexpected sudden death from coronary sinus thrombosis. An unusual complication of central venous catheterization. J Forensic Sci 45:920–922
Timsit JF, Farkas JC, Boyer JM, Martin JB, Misset B, Renaud B, Carlet J (1998) Central vein catheter-related thrombosis in intensive care patients: incidence, risk factors and relationship with catheter-related sepsis. Chest 114:207–213
van Ditzhuyzen O, Ronayette D (1996) Cardiac tamponade after central venous catheterization in a newborn infant. Arch Pediatr 3:463–465
Yoon SZ, Shin JH, Hahn S, Oh AY, Kim HS, Kim SD, Kim CS (2005) Usefulness of the carina as a radiographic landmark for central venous catheter placement in paediatric patients. Br J Anaesth 95:514–517
Acknowledgements
We are very grateful to Prof. Dr. R. Pabst (Head of the Department of Functional and Applied Anatomy, Hannover Medical School) for critical comments and helpful discussions. The authors would like to thank Ms. Sheila Fryk for correcting the English.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Albrecht, K., Breitmeier, D., Panning, B. et al. The carina as a landmark for central venous catheter placement in small children. Eur J Pediatr 165, 264–266 (2006). https://doi.org/10.1007/s00431-005-0044-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-005-0044-5