Abstract
There is increasing evidence that obesity may damage the kidney in otherwise healthy individuals. Our study investigated the effect of childhood obesity on urinary albumin and beta-2-microglobulin excretion, and the association of these with obesity-related cardiovascular risk factors. Random morning spot urine samples were collected from clinically healthy obese ( n =86; median age 12.9 years, range 8.9–17.2 years; median weight 80.6 kg, range 46.1–136.8 kg; median body mass index 30.4 kg/m2, range 24.5–43.2 kg/m2) and normal weight children ( n =79; median age 13.5 years, range 10.7–14.9 years; median weight 51.0 kg, range 27.3–72.5 kg; median body mass index 18.2 kg/m2, range 13.2–23.9 kg/m2). The obese children were examined for the presence of common obesity-related cardiovascular risk factors including hyperinsulinaemia, impaired glucose tolerance (IGT), dyslipidaemia, hypercholesterolaemia, and hypertension. Obese children had a significantly higher urinary albumin/creatinine ratio (U-ACR) (median 11.7 mg/g, interquartile range 12.9 mg/g versus median 9.0 mg/g, interquartile range 5.1 mg/g; P =0.003) and urinary beta-2-microglobulin/creatinine ratio (U-BMCR) (median 63.9 µg/g, interquartile range 34.7 µg/g versus median 34.6 µg/g, interquartile range 44.1 µg/g; P <0.001) than normal weight children. Among the obese children, the U-ACR was associated with fasting hyperinsulinaemia, IGT, and hypercholesterolaemia (all P <0.05), and significantly correlated with the fasting ( r =0.23, P <0.05) and 2-h ( r =0.37, P <0.001) plasma glucose levels measured during an oral glucose tolerance test. Obese children with no more than one of the features of the metabolic syndrome had significantly lower U-ACRs than obese children with two or more features (median 10.4 mg/g, interquartile range 5.8 mg/g versus median 15.3 mg/g, interquartile range 14.9 mg/g; P <0.05). Conclusion:According to our results, clinically healthy obese children have a higher degree of albuminuria and beta-2-microglobulinuria than normal weight children, indicating early renal glomerular and tubular dysfunction as a consequence of childhood obesity. The urinary albumin/creatinine ratio in the obese children was associated with certain metabolic derangements linked to obesity, and also with the clustering of features of the metabolic syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The dramatically increasing rate of childhood obesity in paediatric populations throughout the world has triggered intensive research, focusing on the development and consequences of obesity in children. It is clear by now that damage to different organs as well as obesity-related cardiovascular risk factors can already accompany overweight during childhood and adolescence [6,25].
The impact of obesity on metabolic and cardiovascular diseases has been well documented and now there is increasing evidence that obesity may also damage the kidney. Enhanced excretion of urinary proteins, particularly that of albumin indicating hyperfiltration and early renal damage, has been shown to be associated with adult obesity [19, 20,23]. Furthermore, slightly increased urinary albumin excretion (micro-albuminuria), an indicator of disturbed glomerular permeability, is not only a marker of renal damage, but may also represent the renal expression of systematically increased transcapillary albumin leaking reflecting general endothelial dysfunction [17] and leading to vascular damage. Major epidemiological studies in adults have established micro-albuminuria as an independent predictor of premature atherosclerosis and cardiovascular disease in both diabetic and non-diabetic adults [9, 12, 18,33]. Data concerning the presence of micro-albuminuria in obese children and its association with cardiovascular risk factors are lacking.
Beta-2-microglobulin is a low molecular weight protein that is freely filtered through the glomerular barrier and is normally almost completely reabsorbed and catabolised by the renal proximal tubuli. Increased urinary beta-2-microglobulin excretion is a sensitive marker of proximal tubular dysfunction [15]. Prospective data regarding the association between markers of renal tubular dysfunction and obesity are limited and so far controversial [11, 26,27], and data pertaining to children are very scarce.
In the present study we investigated urinary albumin and beta-2-microglobulin excretion by measuring the urinary albumin/creatinine ratio (U-ACR) and urinary beta-2-microglobulin/creatinine ratio (U-BMCR) in clinically healthy obese and normal weight children. We also evaluated the relationship between the U-ACR and U-BMCR and multiple obesity-related cardiovascular risk factors among the obese children.
Subjects and methods
Subjects
Our study included obese children referred to the childhood obesity clinic of the Department of Paediatrics, University of Pécs, Hungary, because of their overweight. All obese patients underwent a clinical examination aimed at determining the aetiology and consequences of their obese state. Children with secondary obesity were excluded. We considered children as obese if their relative body weight (calculated as the ratio between actual body weight and the ideal body weight for age, gender and height [7]) exceeded 1.2. The body mass index (BMI, weight in kilograms divided by the square of the height in meters) of all obese children exceeded the international cut-off BMI values for overweight by sex and age [5]. As part of this examination, we performed anthropometric (weight, height, waist and hip circumference, skinfolds) measurements, an oral glucose tolerance test (OGTT), determination of fasting serum lipid levels, determination of blood pressure levels, and we collected random morning spot urine samples. Random morning spot urine samples were also collected from age-matched, healthy, normal weight children participating in a urinary screening programme conducted among students of an elementary school. For ethical reasons, blood samples were not taken from the control children and only their weight and height were measured. The study was approved by the ethics committee of our institution.
Examinations
Anthropometric measurements were carried out by the same investigator. Body weight was determined to the nearest 0.5 kg, height to the nearest 0.1 cm by a standard beam scale and Holtain stadiometer, respectively. The waist and hip circumferences were measured with the subject in the supine position. Skinfold thicknesses (biceps, triceps, subscapular, suprailiac, and calf) were measured on the left hand side of the body three consecutive times with the help of a Holtain caliper. Obese children were examined for the presence of obesity-related metabolic and cardiovascular derangements. Blood samples were drawn after an overnight fast for measurement of total cholesterol, HDL-cholesterol and triglyceride concentrations, and a standard 180 min OGTT was performed with administration of 1.75 g/kg (maximum 75 g) glucose, during which venous blood samples were taken for determination of plasma glucose and serum insulin concentrations. Definitions used for the obesity-related metabolic cardiovascular risk factors were as follows: fasting hyperinsulinaemia: fasting serum insulin concentration >20 µIU/ml (mean + 2SD value of 100 control Hungarian children); post-prandial hyperinsulinaemia: peak serum insulin concentration during OGTT >150 µIU/ml [30]; impaired glucose tolerance (IGT): fasting plasma glucose >6.1 mmol/l (110 mg/dl) or 2-h plasma glucose >7.8 mmol/l (140 mg/dl) (according to WHO criteria [8]); dyslipidaemia: high fasting triglyceride >1.5 mmol/l (130 mg/dl) or low fasting HDL-cholesterol <0.9 mmol/l (35 mg/dl) concentration (criteria of the Hungarian Lipid Consensus Conference [28]); hypercholesterolaemia: total fasting serum cholesterol concentration >5.2 mmol/l (200 mg/dl) (criteria of the Hungarian Lipid Consensus Conference [28]). Blood pressure was measured according to published recommendations [31] at least three times in each subject on separate days by the same observer, using a mercury-gravity manometer with proper cuff size under standard conditions. If the average of the three blood pressure values was above the 95th percentile for age and sex, 24-h ambulatory blood pressure monitoring (ABPM) was carried out. Those children whose ABPM values exceeded the 95th percentile value for height and sex [29] were considered to be hypertensive.
Laboratory analyses
Plasma glucose, serum total cholesterol, HDL-cholesterol and triglyceride concentrations were determined by enzymatic methods using a Merck Selectra chemistry analyser and reagents from Randox Ltd (England). Serum insulin was determined by radioimmunoassay with a commercially available kit (Isotope Institute of the Hungarian Academy of Sciences, Budapest, Hungary).
Routine urinalysis by dip stick test and microscopic examination was performed on all urine samples, and protein- or haemoglobin-positive samples or those showing erythrocytes, leukocytes or cylinders were excluded from further assessment, leaving a total of 86 samples from obese children and 79 from normal weight children for further analysis. Urinary albumin concentration was determined by immunoturbidimetry and beta-2-microglobulin concentration by an enzyme immunoassay kit (Abbott Laboratories, IL., USA). Since time and temperature dependent degradation of beta-2-microglobulin occurs at a urine pH <5.5 [15], results for beta-2-microglobulin were considered only for urine samples with pH greater than 5.5 (obese n =56, controls n =62). To compensate for the variations in the concentration of random urine samples, we determined the urinary creatinine concentration (Jaffe method) and used the U-ACR and U-BMCR as an estimation of the urinary excretion of albumin and beta-2-microglobulin.
Statistical analysis
Data are reported as median and range or median and interquartile range. Bivariate analyses included both parametric (Student t -test) and non-parametric (Mann-Whitney U test) methods as appropriate, to assess differences in characteristics and in the U-ACR and U-BMCR between the obese and control groups, and between the obese groups defined by the presence or absence of obesity-related cardiovascular risk factors. Correlations between the U-ACR and U-BMCR and anthropometric and metabolic parameters of the obese children were evaluated by calculation of Spearman’s correlation coefficients. Statistical analyses were performed using the SPSS 11.5 statistical software (SPSS Inc., Chicago, IL). A two-sided P -value of less than 0.05 was considered significant.
Results
The main characteristics of the study population are presented in Table 1. The groups were well matched for age and sex, although the age range of the obese children was wider than that of the normal weight children.
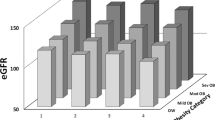
Obese children had a significantly higher U-ACR (median 11.7 mg/g, interquartile range 12.9 mg/g versus median 9.0 mg/g, interquartile range 5.1 mg/g; P =0.003) and U-BMCR (median 63.9 µg/g, interquartile range 34.7 µg/g versus median 34.6 mg/g, interquartile range 44.1 µg/g; P <0.001) as compared to the normal weight children (Fig. 1).
Associations between the U-ACR and U-BMCR and the presence of obesity-related cardiovascular risk factors were investigated in the obese children by performing bivariate comparisons between the U-ACR and U-BMCR values of the obese children with or without a certain risk factor. Among the obese children, 25 (29%) had fasting hyperinsulinaemia, 56 (65%) had post-prandial hyperinsulinaemia, 20 (23%) had IGT, 45 (52%) had dyslipidaemia, 17 (20%) had hypercholesterolaemia, and 10 (12%) had hypertension. The presence of all tested cardiovascular risk factors was associated with a higher mean U-ACR (Table 2), but the difference was significant only in the case of three factors. Obese children with fasting hyperinsulinaemia had a significantly higher U-ACR than obese children with normal fasting insulin. The same was true for obese children with or without IGT, and for those with or without hypercholesterolaemia. The U-BMCR in the obese children was not significantly influenced by any of the cardiovascular risk factors studied.
The relationship between the degree of albuminuria and beta-2-microglobulinuria and the clustering of the cardiovascular risk factors that comprise the metabolic syndrome (hyperinsulinaemia, fasting or post-prandial, IGT, dyslipidaemia and hypertension) was further investigated. Obese children with no more than one of these traits had a significantly lower U-ACR, than those with two or more traits (median 10.4 mg/g, interquartile range 5.8 mg/g versus median 15.3 mg/g, interquartile range 14.9 mg/g; P <0.05). There were no differences in the U-BMCR between these groups.
When analysing both the obese and normal weight groups together, the U-ACR as well as the U-BMCR ratio was positively correlated with body weight ( r =0.16; P <0.05 and 0.34; P <0.001, respectively), BMI ( r =0.22; P <0.05 and 0.23; P <0.05, respectively), and relative body weight ( r =0.23; P <0.05 and 0.31; P <0.001, respectively). When analysing the normal weight and obese children separately, no correlations were found between the U-ACR or U-BMCR and these anthropometric measures. Among the obese children, no significant correlations were found between the U-ACR or U-BMCR and skinfold thicknesses or waist-to-hip ratio either.
Among the obese children, the U-ACR was positively correlated with the fasting ( r =0.225; P <0.05) and 2-h ( r =0.368; P <0.001) plasma glucose concentrations measured during the OGTT. No correlations were found between the U-ACR of the obese children and other metabolic parameters measured (fasting insulin, peak insulin, serum total cholesterol, triglyceride, HDL-cholesterol) or the systolic and diastolic blood pressure. Among the obese children, no significant correlations were found between the U-BMCR and any of the metabolic parameters or blood pressure values.
Discussion
Enhanced urinary albumin excretion is an indicator of systemic endothelial dysfunction [17] and an independent predictor of atherosclerosis and increased cardiovascular morbidity and mortality in the diabetic and general adult population [9, 12,33]. Previous studies have demonstrated that albuminuria is a continuous risk factor. Urinary albumin excretion levels relevant for cardiovascular risk have been shown to be substantially lower than the cut-off for the original definition of micro-albuminuria as a marker of early diabetic nephropathy [9,12]. A progressive graded relationship has been demonstrated between different degrees of albuminuria below the arbitrary threshold for defining micro-albuminuria and cardiovascular events, extending to a U-ACR as low as 0.5 mg/mmol (4.4 mg/g). Therefore, reconsideration of the lower limit defining a “pathological” albuminuria had been suggested earlier, but no consensus has been reached on such a cut-off value so far. For this reason, we have not used a definition for micro-albuminuria, but instead have compared the U-ACR of obese and normal weight children.
The association between excessive albuminuria and common cardiovascular risk factors has been studied extensively in adults [14, 16, 19, 23,24], with somewhat conflicting results. In the present study, increased albuminuria was observed in obese children and it was related to the presence of some features of the metabolic syndrome, but not with others. In particular, significant associations were found with the disorders of carbohydrate metabolism (hyperinsulinaemia and IGT). This finding is in agreement with previous studies in adults demonstrating an association between micro-albuminuria and insulin resistance [18,23] or increased blood glucose levels [13,22], and provides further evidence for the hypothesised central role of insulin resistance in the development of the metabolic syndrome and in the increased cardiovascular risk of subjects with excess urinary albumin excretion. The link between elevated insulin concentrations and the phenotypic traits of the metabolic syndrome are still only partially understood; mechanisms that might link hyperinsulinaemia to greater urinary albumin excretion include increased glomerular haemodynamic pressure [26,32] and endothelial dysfunction [17] that results in increased transcapillary albumin leak.
Obesity is associated with atherogenic changes in lipoproteins and high lipid levels have previously been suggested to contribute to the obesity-associated pathological changes of the kidneys [32]. Several studies have emphasised that increased total cholesterol may be associated with excessive albuminuria in some adult patient groups [2,26], and also with obesity-associated proteinuria and focal segmental glomerulosclerosis in children [1]. A protective effect of dietary prevention of hypercholesterolaemia in preventing obesity-linked renal disease has been demonstrated in animals [21]. Our results have shown association between elevated serum cholesterol levels and enhanced albuminuria. The U-ACR was almost 2-fold increased in obese children with hypercholesterolaemia compared to obese children with normal cholesterol levels, underlining the importance of high cholesterol levels in the development of obesity-related renal damage. We could not demonstrate a significant relationship between the U-ACR and serum triglyceride or HDL-cholesterol levels.
The synergistic effect of obesity and hypertension on renal function and albumin excretion in adults has been investigated in numerous studies, and the observations are controversial [2, 19, 26,27]. In our paediatric population, we could not demonstrate any significant influence of hypertension on the level of albuminuria in obese children, which is in accordance with the results of some of the adult studies [19] and might also be explained by the relatively mild degree of hypertension associated with childhood obesity or the relatively few cases of obesity-associated hypertension we have identified among our obese patients.
We have found an association between excessive albuminuria and clustering of the traits of the metabolic syndrome in obese children. In 1998, the World Health Organisation designated micro-albuminuria as a feature of the metabolic syndrome [10], but this extension of the definition has raised debate, since results contradicting this relationship have also emerged [16,34]. Our results, on the other hand, reinforce this association by demonstrating a link between enhanced albuminuria and presence of the features of the metabolic syndrome in children. Further longitudinal research is needed to evaluate the significance of the increased urinary albumin excretion of obese children in relation to the development of cardiovascular disease in adulthood.
Aside from the direct effects of obesity and associated metabolic disorders, glomerular proteinuria may also be a causative factor of tubulointerstitial dysfunction in obesity, since proteinuria has been shown to increase the turnover of tubular cells [4]. On the other hand, infusion of albumin in proteinuric patients had no relevant effect on the tubular reabsorption of beta-2-microglobulin [3], and thus beta-2-microglobulin can be useful as a parameter to detect tubular injury and alterations in tubular handling of proteins in patients with glomerular proteinuria. Our finding of a significantly and greatly increased U-BMCR in obese children therefore indicates that there is also a tubular component to the renal dysfunction caused by childhood obesity. Unlike in the case of the level of albuminuria, we have not found any associations between the investigated cardiovascular risk factors and the level of beta-2-microglobulinuria among the obese children, which indicates a different mechanism for obesity-linked glomerular and tubular dysfunction.
Our results show that increased levels of albuminuria and beta-2-microglobulinuria indicating early glomerular and tubular dysfunction, respectively, are features of childhood obesity. The significance of this in relation to later development of obesity-related cardiovascular and renal disease should be further investigated.
Abbreviations
- ABPM :
-
ambulatory blood pressure monitoring
- BMI :
-
body mass index
- IGT :
-
impaired glucose tolerance
- OGTT :
-
oral glucose tolerance test
- U-ACR :
-
urinary albumin/creatinine ratio
- U-BMCR :
-
urinary beta-2-microglobulin/creatinine ratio
References
Adelman RD, Restaino IG, Alon US, Blowey DL (2001) Proteinuria and focal segmental glomerulosclerosis in severely obese adolescents. J Pediatr 138: 481–485
Bianchi S, Bigazzi R, Valtriani C, Chiapponi I, Sgherri G, Baldari G, Natali A, Ferrannini E, Campese VM (1994) Elevated serum insulin levels in patients with essential hypertension and microalbuminuria. Hypertension 23: 681–687
Branten AJ, Wetzels JF (1999) Influence of albumin infusion on the urinary excretion of beta-2-microglobulin in patients with proteinuria. Nephron 81: 329–333
Burton CJ, Harper SJ, Bailey E, Feehally J, Harris KP, Walls J (2001) Turnover of human tubular cells exposed to proteins in vivo and in vitro. Kidney Int 59: 507–514
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320: 1240–1243
Csabi G, Torok K, Jeges S, Molnar D (2000) Presence of metabolic cardiovascular syndrome in obese children. Eur J Pediatr 159: 91–94
Eiben O, Pantó E (1987) Body measurement in the Hungarian youth at the 1980s, based on the Hungarian National Growth Study. Antropol Közl 31: 49–68
Expert Committee on the diagnosis and classification of diabetes mellitus (1997) Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20: 1183–1197
Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, Halle JP, Young J, Rashkow A, Joyce C, Nawaz S, Yusuf S (2001) Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286: 421–426
Groop L, Orho-Melander M (2001) The dysmetabolic syndrome. J Intern Med 250: 105–120
Hidaka S, Kaneko O, Shirai M, Kojima K, Igarashi Y, Oda K, Chimata M, Nakamura K, Nagase M (1998) Do obesity and non-insulin dependent diabetes mellitus aggravate exercise-induced microproteinuria? Clin Chim Acta 275: 115–126
Hillege HL, Janssen WM, Bak AA, Diercks GF, Grobbee DE, Crijns HJ, Van Gilst WH, De Zeeuw D, De Jong PE (2001) Microalbuminuria is common, also in a nondiabetic, nonhypertensive population, and an independent indicator of cardiovascular risk factors and cardiovascular morbidity. J Intern Med 249: 519–526
Hiratsuka N, Shiba K, Nishida K, Iizima S, Kimura M, Kobayashi S (1998) Analysis of urinary albumin, transferrin, N-acetyl-beta-D-glucosaminidase and beta-2-microglobulin in patients with impaired glucose tolerance. J Clin Lab Anal 12: 351–355
Hoffmann IS, Jimenez E, Cubeddu LX (2001) Urinary albumin excretion in lean, overweight and obese glucose tolerant individuals: its relationship with dyslipidaemia, hyperinsulinaemia and blood pressure. J Hum Hypertens 15: 407–412
Hong CY, Chia KS (1998) Markers of diabetic nephropathy. J Diabetes Complications 12: 43–60
Jager A, Kostense PJ, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD (1998) Microalbuminuria is strongly associated with NIDDM and hypertension, but not with the insulin resistance syndrome: the Hoorn Study. Diabetologia 41: 649–700
Jensen JS, Borch-Johnsen K, Jensen G, Feldt-Rasmussen B (1995) Microalbuminuria reflects a generalized transvascular albumin leakiness in clinically healthy subjects. Clin Sci 88: 629–633
Kuusisto J, Mykkanen L, Pyorala K, Laakso M (1995) Hyperinsulinemic microalbuminuria: a new risk indicator for coronary heart disease. Circulation 91: 831–837
Liese AD, Hense HW, Doring A, Stieber J, Keil U (2001) Microalbuminuria, central adiposity and hypertension in the non-diabetic urban population of the MONICA Augsburg survey 1994/95. J Hum Hypertens 15: 799–804
Lokkegaard N, Haupter I, Kristensen TB (1992) Microalbuminuria in obesity. Scand J Urol Nephrol 26: 275–278
Maddox DA, Alavi FK, Silbernick EM, Zawada ET (2002) Protective effects of soy diet in preventing obesity-linked renal disease. Kidney Int 61: 96–104
Meigs JB, D’Agostino RB Sr, Nathan DM, Rifai N, Wilson PW (2002) Longitudinal association of glycemia and microalbuminuria: the Framingham Offspring Study. Diabetes Care 25: 977–983
Mykkanen L, Zaccaro DJ, Wagenknecht LE, Robbins DC, Gabriel M, Haffner SM (1998) Microalbuminuria is associated with insulin resistance in nondiabetic subjects – the insulin resistance atherosclerosis study. Diabetes 47: 793–800
Palaniappan L, Carnethon M, Fortmann SP (2003) Association between microalbuminuria and the metabolic syndrome: NHANES III. Am J Hypertens 16: 952–958
Reilly JJ, Mefhren E, McDowell ZC, Hacking B, Alexander D, Stewart L, Kelnar CJH (2003) Health consequences of obesity. Arch Dis Child 88: 748–752
Reisin E, Messerli FG, Ventura HO, Froflich ED (1987) Renal hemodynamic studies in obesity hypertension. J Hypertens 5: 397–400
Ribstein J, du Cailar G, Mimran A (1995) Combined renal effects of overweight and hypertension. Hypertension 26: 610–615
Romics L, Szollar L, Zajkas G (1993) Treatment of disturbances of fat metabolism associated with atherosclerosis (in Hungarian). Orv Hetil 134: 227–238
Soergel M, Kirschstein M, Busch C, Danne T, Gellermann J, Holl R, Krull F, Reichert H, Reusz GS, Rascher W (1997) Oscillometric twenty-four-hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J Pediatr 130: 178–184
Tritos NA, Mantzoros CS (1998) Syndromes of severe insulin resistance. J Clin Endocrinol Metab 83: 3025–3030
Update on the task force report on high blood pressure in children and adolescents: a working group report from the national high blood pressure education program (1996) Pediatrics 98: 649–658
Verani RR (1992) Obesity-associated focal segmental glomerulosclerosis: pathological features of the lesion and relationship with cardiomegaly and hyperlipidaemia. Am J Kidney Dis 20: 629–634
Yudkin JS, Forrest RD, Jackson CA (1988) Microalbuminuria as predictor of vascular disease in non-diabetic subjects. Islington Diabetes Survey. Lancet 2: 530–533
Zavaroni I, Bonini L, Gasparini P, Zuccarelli A, Dall’Aglio E, Barilli L, Cioni F, Strata A, Reaven GM (1996) Dissociation between urinary albumin excretion and variables associated with insulin resistance in a healthy population. J Intern Med 240: 151–156
Acknowledgements
Support was provided by Hungarian National Research Grant (OTKA T033066/2000) to D. Molnar, the Hungarian Ministry of Welfare (ETT 113/2003) to D. Molnar and the Agency for Research Fund Management and Research Exploitation (BIO-00023/2002) to D. Molnar.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Csernus, K., Lanyi, E., Erhardt, E. et al. Effect of childhood obesity and obesity-related cardiovascular risk factors on glomerular and tubular protein excretion. Eur J Pediatr 164, 44–49 (2005). https://doi.org/10.1007/s00431-004-1546-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-004-1546-2