Abstract
We report the French experience regarding pregnancies in maternal phenylketonuria (PKU). In 2001, a questionnaire was sent to each referring PKU specialist in the 20 centres of each region of France, collecting reports on 135 pregnancies in 79 women born between 1958 and 1980. The majority of the 135 pregnancies occurred after 1990. A total of 42 women were informed of the risks of untreated pregnancy, while 26 were not informed (no data for 11). A strict diet was achieved in 83% of informed and in 16% of uninformed mothers prior to conception. Healthy offspring were observed in 43% of the 135 pregnancies, spontaneous abortions in 10.4%, elective abortions in 4.4%, therapeutic abortions in 12.6%, and embryopathies (EP) in 21.5%. In 8.1% of cases, the outcomes (in earliest pregnancies) are unknown. The proportion of healthy children increased over time and reached 80% of the pregnancies of informed females. There were seven heart defects, all in cases of EP, but although microcephaly and intrauterine growth retardation (IUGR) were almost constant in EP, we also found nine healthy children with IUGR. A continuum between EP and healthy children is suggested. The anthropometric data of the mothers showed that their body mass index (BMI) distribution was shifted to the left compared to women of the general population. This lower BMI and poor weight gain during pregnancy could contribute to the IUGR observed in normal babies whose mothers received a phenylalanine-restricted diet during pregnancy. Conclusion:the information and the preconception diet are effective for avoiding embryopathies in maternal phenylketonuria. Nutritional parameters can influence fetal growth and the nutritional state must be closely monitored throughout pregnancies of women with phenylketonuria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The devastating effects of untreated maternal phenylketonuria (OMIM: 261600) (MPKU) on fetus and offspring were first described by Dent in 1957 [4] and a collaborative study (MPKUCS) has been extensively published on this very important topic [8]. In France, neonatal screening has identified about 44 PKU patients per year since the beginning of the 1970s, with increasingly better clinical outcome [1]. Like other countries, we have observed offspring with embryopathy (EP) born to PKU mothers [15, 16, 18]. Several procedures have been initiated to prevent this embryological risk. Prevention included contacting females who have been lost of follow-up, informing precocious PKU adolescents, and circulating to gynaecologists data concerning this rare cause of embryopathy that can occur in unscreened PKU mothers [2, 5, 12, 17]. In this retrospective study, we report comprehensive data regarding pregnancies in PKU females in France. We collected data from the 20 regional associations of the AFDPHE (French association for screening and treatment of handicaps in infancy), who are in charge of PKU screening and management. We confirmed the positive impact on well-informed PKU females regarding compliance with the preconception diet and the outcome of the pregnancy. We analysed the birth parameters and malformations of the offspring and assessed the risk and potential causes of intrauterine growth retardation (IUGR), taking into account the body mass index (BMI) of the mothers and their weight gain during pregnancy.
Subjects and methods
Study design
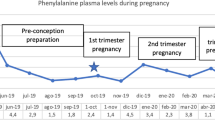
This national retrospective study was performed in order to identify all women with PKU who had begun a pregnancy. In 2001, we sent a questionnaire to each PKU specialist to collect data about all known pregnancies in PKU females, whatever their outcome. We recorded the following data: mother’s date of birth, PKU phenotype, and the degree of information women had received at diet initiation. We analysed the outcome of the offspring as a function of the percentage of mothers on a preconception diet, of the mother’s age, and whether the adolescents had been informed about the risks of untreated pregnancy. To study metabolic control, we analysed the phenylalanine (Phe) levels during the pregnancy, using the number of Phe levels in the target range (120–300 µmol/l) per trimester. We analysed the offsprings’ birth parameters as a function of the metabolic control, the mothers’ BMI before pregnancy, and their weight gain during pregnancy. We classified the outcome of the pregnancies as: spontaneous abortion (SA), elective abortion (EA), therapeutic abortion (TA), hyperphenylalaninaemic embryopathy (EP), and normal outcome (Norm). The criteria for diagnosing EP were at least one malformation (congenital heart disease, oesophageal anomaly), microcephaly, or IUGR, i.e. one birth parameter (weight, length, or head circumference) below the 5th percentile (Swedish standards). The presence of EP was also estimated by analysis of the neurological follow-up of the children, when available.
Statistical analysis
The chi-squared test was used to determine whether the information status and the number of females on the preconception diet rate differed over time. The Student’s unpaired t-test was used to determine difference between two variables. Spearman rank correlation was used to analyse the relation between two variables. Data are expressed as mean ± standard deviation and as median and range for the anthropometry of offspring at birth. Significance was set at P<0.05.
Results
Status of the women studied
We recorded 135 pregnancies in 79 women born between 1958 and 1980 (median age 29 years, range 16–38 years). Of the women in our population, 50% were born before the advent of neonatal screening. All women whose PKU was diagnosed because of EP were born before 1970. Four pregnancies (3%) occurred in teenage girls (≤18 years). Out of the 79 PKU women, 53 were diagnosed by neonatal screening (74%), 13 during infancy (18%), and 6 were diagnosed because of the embryopathy of their child (8%). Data were missing for seven women. Out of the 79 women, 53 had classical PKU (73%), 14 had atypical PKU (19%), 6 had mild hyperphenylalaninaemia (8%), and for 6, data were missing. This proportion of phenotypes is similar to that in the French PKU population [1].
Number of PKU females who had been informed
Information whether they had been informed about the risks of untreated pregnancy was missing for 11 women, all born before 1970. A total of 29 women were not informed (36%), 27 of whom were born before 1974, and 25 before 1970. Only two uninformed women were born after the beginning of systematic neonatal screening (in 1978 and 1980 respectively). These two mentally retarded women withdrew from follow-up very early and their outcomes were a TA and a child born with EP. The number of uninformed women decreased over time and the great majority are now informed. For women born after the beginning of the systematic neonatal screening (1978), the rate of informed women was 80%.
Number of mothers on preconception diet
A preconception diet was followed in 57/135 pregnancies (42.2%). Diet initiation prior to conception strongly depended on the information the mother had received regarding MPKU. In the group of uninformed women, 84% did not follow a preconception diet, whereas 83% of informed women were on a controlled diet prior to conception. The 16% of uninformed mothers who were on a diet prior to conception are those who had a second pregnancy after PKU had been diagnosed after the first pregnancy. We also observed a significant increase over time in the number of informed mothers (P<0.001) and of preconception dieting (P<0.05) by comparing pregnancies initiated before and after 1997 (this date splits the number of pregnancies into two equal groups).
Pregnancy outcomes
The outcome of pregnancies was available in 124 cases. The rate of SA (10.4%) was comparable to that of the general French population whereas the rate of EA (4.4%) was lower (22%) and remained stable over time [3]. TA occurred in 12.6% of pregnancies, which is higher than in the general population, and also remained stable over time. We recorded 29 EP (21.2% of pregnancies), but 6 of them led to the diagnosis of PKU, which reduces the percentage of EP to 17% if we exclude these cases from the calculation. The level of EP decreased sharply over time, and we did not observe EP after 2001 (Fig. 1). Heart defects were found only in EP babies (n=7). We did not note any other malformation. Overall, TA and embryopathies represented 34.1% of results that can be considered to be poor (Table 1). Of offspring, 43% were healthy (50% if SA and EP leading to PKU diagnosis are excluded). The percentage of healthy offspring constantly increased over time (Fig. 1) and with the increase in the number of informed mothers, 80% of pregnancies led to healthy children in the informed group.
The outcome of offspring varied with the PKU phenotype. We recorded 38% of good outcomes for children born to mothers with typical PKU, 50% with atypical PKU, and in four children of mothers with mild hyperphenylalaninaemia (n=7). Three outcomes are unknown.
Regarding laboratory tests, we recorded data for only 47 pregnancies, mainly with normal outcome (n=41). We recorded the Phe levels for only four pregnancies leading to EP or TA; that is why we give individual data for these observations. We observed that most Phe levels were below 300 µmol/l when the outcome was good (Table 2). The second observation of supposed EP (Table 2) is interesting, because, despite good Phe controls during the first and second trimester, the child had IUGR (birth weight 2500 g, length 47 cm, head circumference 32 cm). His psychomotor milestones at 6 years of age are strictly normal, suggesting that for this child, IUGR was not due to PKU embryopathy.
All children (n=72) for whom we had data were born at term (median 40 weeks, range 36–42 weeks) (Table 3). We found no difference in the birth term of the two groups: normal (n=57) versus EP (n=15), but the weight, height, and head circumference were significantly lower in the EP group (P<0.0001 for the three parameters). We observed a continuum between the two groups for the three parameters, with the largest overlap between the two groups for birth weight and the smallest for head circumference (Fig. 2a,b,c). IUGR was always present in EP, microcephaly was found in 18 out of 20 EP, while nine healthy children had moderate IUGR (birth measurements <2SD).
In order to explain the IUGR observed in healthy children, we studied the anthropometry of the mothers and observed a distribution shifted to the left for weight and BMI but not for height (Fig. 3). We failed to show a correlation between birth weight and maternal BMI z-score or between birth parameters and maternal weight gain during pregnancy.
Discussion
This comprehensive retrospective national study enabled us to record 135 pregnancies in 79 PKU women. A total of 42 women were born before 1972 (the date of the start of neonatal screening in France) and 37 women were born thereafter. The high proportion of women born before 1972 can explain most of the poor outcomes. These women did not benefit from information about the risk of unplanned pregnancy. Moreover, this group of earliest PKU patients had had a shorter time of strict diet (some until 5 years of age) and had lower intellectual levels than those of later patients. These factors can explain the high rate of “lost to follow-up” and consequently of unplanned pregnancies [3, 19, 20]. In our population, there was a very low rate of pregnancies in teenage women (3%) compared to the MPKUCS (19%). This low rate of teenage pregnancies can reflect the good adolescent information in our population and/or the later average age of the first pregnancy in French women (29.2 years) [3].
Hence, our results show the marked impact of good information on the success of the preconception diet. The majority of informed women (83%) were on the controlled diet prior to conception. Our results agree with the results of the University College London Hospitals who achieved a good rate of 78% of pregnancies with preconception dietary control [9]. Overall in 2003, the MPKUCS reported that 25.9% (148/582 pregnancies) of mothers followed a preconception diet [8]. The present policy in the United States is to prescribe the PKU diet for life, in order to improve the level of compliance and pregnancy outcome [11, 14]. In our population, the majority of women had not been on a diet before planning pregnancy. This did not influence their preconception diet status. We consider that the quality of information and follow-up are much more important than the type of diet patients followed before planning pregnancy.
Our results for pregnancy outcome show that the rates of SA and EA are rather constant over time. The rate of SA was around 10%, as usually observed in the general population [3]. With improving information, non-planned pregnancies now lead to TA, while in the past, they led to EP. We observed fewer voluntary terminations (4.4%) than in the general French population (22%) [3]. After adequate information, women with PKU take effective contraception. Since EA is often related to unplanned pregnancies, the relative obligation to plan pregnancies in our population probably explains the low level of EA in this group of women.
We clearly showed a regular decrease in EP rate over time. The present rate of EP is below 10% and is tending to zero, which is the objective of MPKU management. In 2001 and 2002, we had no cases of EP but we had two TA for unplanned pregnancies and major risk of EP.
Our data on Phe levels mainly concerned pregnancies with normal outcome, thus we could not correlate the birth parameters with the biological data, but the links between these two factors no longer need to be demonstrated. In most other reports, biological data are expressed as “weeks to achieve diet control” [6, 11, 13]. Because of the fluctuation of Phe levels, the average of the number of Phe monitorings seems to us a better marker than the date when dietary control is achieved. For pregnancies with good outcome, the number of Phe monitorings was around ten in the first trimester. Bearing in mind that pregnancy was usually diagnosed at about the end of the 1st month, this means that these women had at least one Phe analysis per week. The present policy of the French PKU workgroup recommends a Phe monitoring once or twice a week until the end of the second trimester.
In this study, the PKU phenotype clearly influenced the outcome of the pregnancies. We noted seven pregnancies in six women with mild hyperphenylalaninaemia. This resulted in seven babies; four were normal and three outcomes are unknown. Similar results were also observed by Levy et al. [10] in 86 mothers with 219 untreated pregnancies. These authors concluded that dieting during pregnancy appears not to be indicated in this group with mildly raised Phe if levels remain under 400 µmol/l (6.6 mg/dl). As expected, for PKU mothers, we observed better outcomes in atypical PKU than in typical PKU.
Our results suggest that anthropometric parameters at birth, especially weight, are not good markers for determining outcome. In the second observation of suspected EP, parameters at birth were low (weight 2500 g, length 47 cm and head circumference 32 cm) despite excellent Phe levels during pregnancy. The child was classified as potentially EP, but at 6 years of age he has a normal intellectual level and good school results. Therefore, in that case, the good levels of Phe during pregnancy were more relevant than birth measurements for predicting the neurological outcome. In our population, if we consider birth parameters, there is a continuum between EP and normal offspring (Fig. 2a,b,c). It is likely that hyperphenylalaninaemia is not the only factor leading to IUGR in offspring of PKU mothers. Similarly, Michals et al. [12] showed that maternal weight gain and dietary intake of protein, energy, and fat were correlated with the offspring’s birth parameters. Our data show that PKU females had a nutritional status shifted to the left if we consider weight and BMI. We failed to demonstrate a correlation between this low nutritional status and the weight of children at birth, probably because many factors affect fetal growth. It is likely that more subtle nutritional markers are necessary to show the link between maternal nutritional imbalance and fetal growth. In 2000, Koch et al. [7] observed that the offspring from well-controlled pregnancies had less good anthropometric data than controls. In this study, in the group of non-PKU hyperphenylalaninaemic mothers, the offspring of treated pregnancies had lower birth weights than the untreated ones [7]. These results suggest a maternal nutritional origin for IUGR when Phe levels are well controlled. We must be very aware of the calorie intake and must verify the correct amount of micronutrients (cobalamin, iron, carnitine, selenium) to be sure that, despite the diet, the recommended dietary allowances for pregnancy are achieved. In addition, maternal weight gain during pregnancy should be controlled since the diet potentially decreases calorie intake. Furthermore, episodes of Phe levels below 120 µmol/l could influence fetal growth. We did not record the number of Phe levels below 120 µmol/l so we do not have these data. Nevertheless, this point must be stressed in the nutritional follow-up of PKU women during pregnancy.
MPKU remains a problem in many countries, although the results of most groups are improving with time. Information and follow-up are the main weapons for preventing EP. The nutritional status of the mother must be carefully verified as it is a prerequisite for good child growth and long-term intellectual outcome. As a result of this study, the French organisation for PKU screening (AFDPHE) has published a national booklet regarding the follow-up of each pregnancy in PKU women, with systematic biological and clinical sections, that serve as guidelines and will help answer remaining questions.
Abbreviations
- BMI :
-
body mass index
- EA :
-
elective abortion
- EP :
-
embryopathy
- IUGR :
-
intrauterine growth retardation
- MPKU :
-
maternal phenylketonuria
- MPKUCS :
-
maternal phenylketonuria collaborative study
- Phe :
-
phenylalanine
- PKU :
-
phenylketonuria
- SA :
-
spontaneous abortion
- TA :
-
therapeutic abortion
References
Abadie V, Berthelot J, Feillet F, Maurin N, Mercier A, Ogier de Baulny H, de Parscau L (2001) Neonatal screening and long-term follow-up of phenylketonuria: the French database. Early Hum Dev 65: 149–158
Acosta PB, Blascovics M, Cloud H, Lis E, Stroud E, Wenz E (1982) Nutrition in pregnancy in women with hyperphenylalaninemia. J Am Diet Assoc 80: 443–450
Cohen J, Madelenat P, Levy-Toledano R (2000) La demande de soins–grossesse. Gynécologie et santé des femmes, quel avenir en France. ESKA Eds, pp 84–102
Dent CE (1957) Discussion of Armstrong MD, the relation of biochemical abnormality to the development of mental defect in phenylketonuria. Etiologic factors in mental retardation. 23rd Ross Pediatric Research Conference. Ross Laboratories, Columbus, pp 32–33
Güttler F, Lou H, Andresen J, Kok K, Mikkelsen I, Nielsen KB, Nielsen JB (1990) Cognitive development in offspring of untreated and preconceptionally treated maternal phenylketonuria. J Inherit Metab Dis 13: 665–671
Hanley WB, Platt LD, Bachman RP, Buist N, Geraghty MT, Isaacs J, O’Flynn ME, Rhead WJ, Seidlitz G, Tishler B (1999) Undiagnosed maternal phenylketonuria: the need for prenatal selective screening or case finding. Am J Obstet Gynecol 180: 986–994
Koch R, Friedman E, Azen C, Hanley W, Levy H, Matalon R, Rouse B, Trefz F, Waisbren S, Michals-Matalon K, Acosta P, Güttler F, Ullrich K, Platt L, de la Cruz F (2000) The international collaborative study of maternal phenylketonuria. Eur J Pediatr 159: S156–S160
Koch R, Hanley W, Levy H, Matalon K, Matalon R, Rouse B, Trefz F, Güttler F, Azen C, Platt L, Waisbren S, Widaman K, Ning J, Friedman EG, de la Cruz F (2003) The maternal phenylketonuria international study: 1984–2002. Pediatrics 112: 1523–1529
Lee PJ (2000) Comments on the international collaborative study of maternal phenylketonuria status report 1998. Eur J Pediatr 159: S161–S162
Levy HL, Waisbren SE, Lobbregt D, Alfred E, Leviton A, KochR, Hanley WB, Rouse B, Matalon R, de la Cruz F (1996) Maternal non-phenylketonuric mild hyperphenylalaninemia. Eur J Pediatr 155: S20–S25
Matalon R (2000) Maternal PKU: Pregnancy and child outcomes in relation to dietary control. In consensus development conference on phenylketonuria (PKU): screening and management. NIH Bethesda, October 16–18, pp 97–101
Michals K, Acosta PB, Austin V, Castiglioni L, Rohr F, Wenz E, Azen C (1996) Nutrition and reproductive outcome in maternal phenylketonuria. Eur J Pediatr 155[Suppl 1]: S165–S168
Platt LD, Koch R, Hanley WB, Levy HL, Matalon R, Rouse B et al (2000) The international study of pregnancy outcome in women with maternal phenylketonuria: report of a 12-year study. Am J Obstet Gynecol 182: 326–333
Rouse B, Azen C (2004) Effect of high maternal blood phenylalanine on offspring congenital anomalies and developmental outcome at ages 4 and 6 years: the importance of strict dietary control preconception and throughout pregnancy. J Pediatr 144: 235–239
Rouse B, Azen C, Koch R, Matalon R, Hanley W, de la Cruz F, Trefz F, Friedman E, Shifrin H (1997) Maternal phenylketonuria collaborative study (MPKUCS) offspring: facial anomalies, malformations and early neurological sequelae. Am J Med Genet 69: 89–95
Saliba Z, Bah G, Martin D, Abadie V, Azar Z, Fraisse A, Sidi D, Kachaner J, Bonnet D (2000) Pseudo-inherited form of left heart obstructive defects revealing maternal phenylketonuria. Arch Mal Coeur Vaiss 93: 649–652
Salize HJ, Funders-Bucker B, Knorrek U, Kolbe S, Pietsch V, Seidlitz G, Ullrich K, Trefz FK (1992) Maternal phenylketonuria. Problems in detecting and risk educating identified females. Monatsschr Kinderheilkd 140: 42–46
Thibaud D, Ploussard JP, Vaquant PO, Chemouny S, Kleitz T (1998) Diagnosis of phenylketonuria in a 35-year-old mother in relation to prenatal diagnosis of intrauterine growth retardation with microcephaly. Arch Pédiatr 5: 1229–1231
Vidailhet M, Feillet F (2002) Dépistage neonatal. Le défi médical:du malade à sa descendance. Arch Pediatr 9[Suppl 2]: 154s–156 s
Vidailhet M, Feillet F, Abadie V (2002) Grossesse chez la femme atteinte de phénylcétonurie. Mise à jour en gynécologie et obstétrique, pp 93-99
Acknowledgements
We thank all the French referring PKU specialists who participated in this study and the Association Française pour le Dépistage et la Prévention des Handicaps de l’Enfant for its support of this study. We also thank Alan Strickland for his help in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the PKU workgroup of the Association Française pour le Dépistage et la Prévention des Handicaps de l’Enfant (AFDPHE)
Rights and permissions
About this article
Cite this article
Feillet, F., Abadie, V., Berthelot, J. et al. Maternal phenylketonuria: the French survey. Eur J Pediatr 163, 540–546 (2004). https://doi.org/10.1007/s00431-004-1482-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-004-1482-1