Abstract
Fabry disease (FD) is a debilitating progressive multisystem X-linked lysosomal storage disorder. It was generally believed that the disease affects only adult males. Through systematic pedigree analysis, we identified 35 paediatric FD patients (age 1 to 21 years, mean 12.6 years) in 25 families. Predominant signs in this cohort were: acroparesthesia, hypohidrosis, and cornea verticillata. Neurological and psychological changes, such as tinnitus, recurrent vertigo, headache, diminished level of activity, fatigue, and depression were often observed. Angiokeratoma and gastrointestinal symptoms were frequent. Some patients also showed cardiac abnormalities. Six children and adolescents (three males and three females) over 14 years of age had renal involvement (all with proteinuria, one male had a decreased creatinine clearance of 62 ml/min). No males, but three females (1.5, 4 and 9 years of age), were free of signs and symptoms. Males (n=15, age 1 to 21 years, mean 12.4 years) and females (n=20, age 1.5 to 20 years, mean 12.7 years) showed comparable disease severity. However, the clinical courses demonstrated a wide intra- and interfamilial variability and tended to be more heterogeneous in the girls. Female patients are frequently affected at an early age, not much differently than males. They should be carefully examined because most carriers are symptomatic. Conclusion: Fabry disease usually becomes clinically manifest in childhood. Renal involvement can begin in adolescence. The diagnosis is made following a high level of suspicion or systematic pedigree analysis. It is crucial for paediatric Fabry disease patients to have early access to optimal supportive symptomatic management. Enzyme replacement therapy has shown promising effectiveness in adults. Considering its widespread therapeutic and potential preventive benefits, enzyme replacement therapy should be initiated at an early stage, prior to the onset of irreversible complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fabry disease (FD; OMIM 301500) is an X chromosomal linked inherited lysosomal storage disorder, due to partial or complete deficiency of ceramidetrihexosidase, commonly referred to as α-galactosidase A (GALA) [3]. This results in progressive storage of glycosphingolipids including globotriaosylceramide (Gb3), digalactosylceramide, blood group B, B1, and P1 glycolipids. The accumulation occurs in many types of cell, such as dorsal root ganglia, neuronal cells of the autonomic nervous system, glomerular epithelial cells (podocytes), tubular epithelial cells, mesangial cells in the kidney, myocardial cells, valvular fibroblasts as well as endothelial cells, pericytes, and smooth muscle of the vascular system. FD is a multi-system disorder, with a wide spectrum of physical signs and symptoms predominantly affecting the nervous system, skin, heart, kidneys and the eyes. In the first two decades, acute and chronic neuropathic pain, hypohidrosis, angiokeratoma and gastrointestinal symptoms significantly reduce the quality of life. Lifespan is shortened by late complications in adulthood that include heart failure, renal failure and cerebrovascular accidents. A detailed analysis of clinical picture of this disease in male and female adults has recently been reported by MacDermot et al. [17, 18]. The GALA gene is localized on Xq22.1. Although heterozygous, females are often severely affected [27], due but probably not limited to random X-inactivation, as it is in few other X-linked conditions, e.g. ornithine transcarbamylase deficiency, an inborn error of metabolism in the urea cycle.
To elucidate the natural history of FD and its implications for the paediatric population, we investigated 35 patients from Mainz (n=20), Cambridge (n=6), Milan (n=6), and Göteborg (n=3).
Patients and methods
The patients (age 1 to 21 years, mean 12.6 years) were identified by systematic pedigree studies from 25 families, investigating subjects at genetic risk for FD. After a comprehensive history, thorough physical and neurological examinations were performed. Ophthalmological examination, ECG, cardiac ultrasound and creatinine clearance were done. To confirm the diagnosis, mutation analysis was performed except for patients 9, 22, and 34. Patients 9 and 22 had decreased GALA activity, assayed in leucocytes with an artificial 4-methylumbelliferyl-substrate [19]. Patient 34, having an affected father, is a symptomatic obligate carrier; however, the identification of this family's mutation is still pending. To determine severity, patients were classified according to the previously described Mainz Severity Score Index (MSSI) quantifying general, neurological-psychological, cardiovascular, and renal abnormalities in each patient. In this scoring system the physical signs or symptoms are weighted according to their contribution to the morbidity of the disease and quantified by numbers. The MSSI scores are then divided into severity bands of mild (<20), moderate (20–40) and severe (>40) affliction, to reflect the clinical spectrum of FD [28].
Results
Physical signs and symptoms found in our patients are listed in detail in Table 1 and Fig. 1.
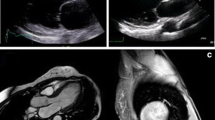
In the group of male patients (n=15, age between 1 and 21 years, mean 12.4 years), 93% had hypohidrosis. Cream-coloured, whorl-shaped corneal opacities, also known as cornea verticillata, were found in 73%. Acroparaesthesias, often triggered by changes of the environmental or body temperature as well as by emotional stress, were present in 67%. Neurological and psychological findings, such as headache, tinnitus, recurrent vertigo, diminished level of activity, fatigue, or depression could be identified in 67%. Of males, 53% had angiokeratoma. Gastrointestinal symptoms, including diarrhoea, recurrent nausea or vomiting were reported by 40%. Cardiac abnormalities, such as cardiomyopathy, or mitral valve prolapse, could be detected in 13%. Renal complications of the disease, i.e. proteinuria, were already present in 13% of the male patients. Patient 10 had, in addition, a decreased creatinine clearance of 62 ml/min. The MSSI (Fig. 2) ranged from 6 to 27 (mean 11.9). No boy was free of physical signs and symptoms.
The females (n=20) were between 1.5 and 20 years (mean 12.7 years) old of whom 70% had cornea verticillata and 65% reported acroparaesthesias. Angiokeratoma were found in 30%. Hypohidrosis was present in 25% of the female patients. Comparable to the group of male patients, although less frequent, a wide range of neurological/psychological findings, such as diminished level of activity, fatigue, tinnitus, recurrent vertigo, headache, or depression was documented in 25% of the females. Gastrointestinal problems consisting of abdominal pain and constipation were reported by 20%. The overall prevalence of cardiac abnormalities was 20%. We found a short PR interval, mitral valve regurgitation, and septum enlargement; one patient had a partial atrioventricular septal defect. Of the female patients, 15% had renal involvement manifesting with proteinuria. The MSSI (Fig. 2) ranged from 0 to 17 (mean 6.5). Three girls (1.5, 4 and 9 years of age) did not have a clinical manifestation of the disease.
Discussion
It was generally believed that FD clinically affects only adult males. The present study, on the contrary, demonstrates that FD is a burdensome condition already in childhood, not only for males but also for females. Diagnostic delay is frequent, probably due both to the rarity of the disease and to the fact that the first complaints of the disease are only subjective symptoms difficult to understand and evaluate.
Acroparaesthesia is agonising pain of burning and tingling character, often associated with a deep ache, predominantly seen in the palms and soles of the feet and radiating proximally. It can be continuously present or consist of episodic attacks, aggravated by body or environmental temperature changes, illness or physical as well as emotional stress. Rest, temperature changes, or medication may alleviate it. This pain can be severe, especially in boys, and often makes them cry. In 23/35 patients it was the first reported symptom with onset as early as 3 years of age in boys and 6 years of age in girls. The presumed explanation for this nerve pain is a structural damage, caused by deposition of Gb3 in nerve axons and dorsal root ganglia, to which long unmyelinated fibres are primarily susceptible [4]. An alternative explanation is that exposure to cold induces local vasoconstriction and small-fibre mal-perfusion due to accumulation of storage material in cutaneous vessels and vasa vasorum [9]. Luciano et al. [16] found a length-dependent dysfunction of a-delta and c-fibres resulting in greater impairment of cold than warm sensation. Of the 28 adult patients in that study, 6 had median nerve entrapment at the wrist [16]. However, significantly decreased cold and warm sensation on physical examination is primarily a phenomenon associated with adults. It is usually normal in paediatric patients. Other possible causes of neuropathic pain include molecular mechanisms resulting in accumulation of sodium channels in injured nerves, pathological sympatho-afferent coupling, disinhibition of nocioception, and central or peripheral nocioceptive sensitisation. Identification of the specific mechanism of neuropathic pain in each patient would be advantageous for a more precise selection of analgesic therapy [2]. Anticonvulsants, for example carbamazepine [14], phenytoin [15], neurotropin combined with carbamazepine [10], and gabapentin [24] have been used for treatment of the chronic neuropathic pain associated with FD.
A wide spectrum of other neurological and psychological findings could be documented in most of the males and females. The range of these symptoms was wide, producing diminished level of activity, fatigue, tinnitus, recurrent vertigo, headache and depression.
Hypohidrosis, due to the accumulation of Gb3 in the eccrine sweat glands and their associated blood vessels [13], is very common in boys and was also observed to a lesser degree in female patients. In many of our patients it interfered with normal physical exercise mainly in the summer. As body temperature changes are a triggering factor, the inability to cool the body during exercise may even increase neuropathic pain.
Angiokeratoma (Fig. 3), appearing as small, raised, dark-red spots, were not always present. Although not specific for FD, it can be idiopathic or associated with other diseases [7, 8, 12, 20, 26]. It is the only objective sign that may present early and usually allows prompt diagnosis. In the absence of angiokeratoma, early clinical diagnosis is often difficult to establish.
Gastrointestinal symptoms are quite frequent, presenting with diarrhoea, constipation, recurrent nausea or vomiting and abdominal pain. These symptoms often lead to hospitalisation and are sometimes mistaken for chronic inflammatory bowel disease. Malabsorption can be caused by storage deposition in the small intestine, while diarrhoea and altered intestinal motility may be due to lipid accumulation in intestinal autonomic nerve ganglia [21]. Argoff et al. [1] described improvement in gastrointestinal emptying with oral metoclopropamide. According to our experience, supplementation with pancreatic enzyme preparations has resulted in improvement of the symptoms. Some patients with episodes of vomiting responded satisfactorily to ondansetrone.
Cardiac [11] and renal involvement can manifest in childhood; hence early diagnosis and careful monitoring is necessary. Proteinuria, i.e. albuminuria, is usually the first indication of renal dysfunction [29]. Progressive renal insufficiency occurs in older patients, although significant renal involvement has previously been reported in a 19-year-old female [5].
On the basis of the MSSI, 3/35 patients were unaffected, 30/35 children and adolescence were mildly affected (MSSI <20), with severity of symptoms in both males and females being very similar. Two boys were affected moderately (MSSI >20). MSSI increases with age as the severity of symptoms worsens. In the males, the correlation of increasing MSSI with age tended to be more striking than in the females. This could be explained by the heterogeneity in disease severity amongst females due to X-chromosome inactivation and also the later presentation of clinical symptoms when compared to males. There also appeared to be significant inter- and intrafamilial variability. Difficulties often arise in making the diagnosis when no adult index patient is present. This is due to the fact that many more frequent conditions mimic signs and symptoms of FD [23], i.e. "growth pain", rheumatological diseases, fibromyalgia, chronic inflammatory bowel disease, and meningitis (fever, pain, red punctuate skin lesions). Common symptoms in the paediatric Fabry patient, like pain, diarrhoea, nausea, vomiting, headache and fatigue are often misinterpreted as non-specific. In these cases, the diagnosis may be missed in the paediatric stage and finally be made in the latter course of the disease when cardiac, cerebrovascular, or renal complications are present.
Of the 25 families, GALA mutations were detected in 23 (92%). In our cohort, a total of 22 different mutations were detected, only two apparently unrelated patients carried the same mutation (R220X in patients 24 and 28) suggesting that it is a recurrent gene defect. The high frequency of 'private' mutations is typical for an X-linked trait with reduced reproductive fitness in affected males. More than 50% of the GALA mutations (13/22, i.e. 59%) predict a truncated protein due to an early in frame nonsense mutation or a premature stop codon following a DNA change with frame shift. Clearly, some of these mutations may represent functional null alleles with complete absence of the enzyme. Nevertheless, no obvious correlation exists between the genotype and phenotype that makes any prediction on the clinical course of the disease difficult.
To ensure early diagnosis, a strong clinical suspicion and systematic investigation of potentially affected family members are essential. The high prevalence and relative specificity of cornea verticillata might suggest its value as a screening method, for example in the context of ophthalmological evaluations of school children or candidates for the driving licence. The skin of the paediatric pain patient needs to be evaluated for angiokeratoma (Fig. 3) although their absence does not exclude FD. Early diagnosis enables optimal supportive symptomatic management, which, in combination with the now available enzyme replacement therapy [6, 25] has the potential to improve the quality of life, prevent late complications and decrease the premature death rate. We therefore believe that treatment with enzyme replacement should be initiated at an early stage, prior to the onset of irreversible complications. Current paediatric enzyme replacement trials will extend the knowledge about the potential of reversibility or prevention with this promising therapy approach. Given the phenotypic heterogeneity, the elaboration of therapy monitoring strategies may provide an indication of the quantity and frequency of administration of the therapeutic enzyme on an individual base. In the future, gene therapy could be a novel therapeutic option to treat this debilitating chronic progressive multisystemic disorder [22].
Abbreviations
- FD :
-
Fabry disease
- GALA :
-
α-galactosidase A
- Gb 3 :
-
globotriaosylceramide
References
Argoff CE, Barton NW, Brady RO, Ziessman HA (1998) Gastrointestinal symptoms and delayed gastric emptying in Fabry's disease: response to metoclopramide. Nucl Med Commun 19: 887–891
Birklein F (2002) Mechanism-based treatment principles of neuropathic pain. Fortschr Neurol Psychiatr 70: 88–94
Brady RO, Gal AE, Bradley RM, Martensson E, Warshaw AL, Laster L (1967) Enzymatic defect in Fabry's disease. Ceramidetrihexosidase deficiency. N Engl J Med 276: 1163–1167
Cable WJ, Dvorak AM, Osage JE, Kolodny EH (1982) Fabry disease: significance of ultrastructural localization of lipid inclusions in dermal nerves. Neurology 32: 347–353
El-Shahawy MA, Mesa C, Koss M, Campese VM (1996) A 19-year-old female with fever, acroparesthesia, and progressive deterioration of renal function. Am J Nephrol 16: 417–424
Eng CM, Guffon N, Wilcox WR, Germain DP, Lee P, Waldek S, Caplan L, Linthorst GE, Desnick RJ (2001) Safety and efficacy of recombinant human alpha-galactosidase A replacement therapy in Fabry's disease. N Engl J Med 345: 9–16
Epinette WW, Norins AL, Drew AL, Zeman W, Patel V (1973) Angiokeratoma corporis diffusum with α-L-fucosidase deficiency. Arch Dermatol 107: 754–757
Gehler J, Sewell AC, Becker C, Hartmann J, Spranger J (1981) Clinical and biochemical delineation of aspartyl-glycosaminuria as observed in two members of an Italian family. Helv Paediatr Acta 36: 179–189
Hilz MJ, Stemper B, Kolodny EH (2000) Lower limb cold exposure induces pain and prolonged small fiber dysfunction in Fabry patients. Pain 84: 361–365
Inagaki M, Ohno K, Ohta S, Sakuraba H, Takeshita K (1990) Relief of chronic burning pain in Fabry disease with neurotropin. Pediatr Neurol 6: 211–213
Kampmann C, Baehner F, Whybra C, Martin C, Wiethoff CM, Ries M, Gal A, Beck M (2002) Cardiac manifestations of Anderson-Fabry disease in heterozygous females. J Am Coll Cardiol 40: 1668–1674
Kanzaki T, Yokota M, Mizuno N, Matsumoto Y, Hirabayashi Y (1989) Novel lysosomal glycoaminoacid storage disease with angiokeratoma corporis diffusum. Lancet 1: 875–877
Lao LM, Kumakiri M, Mima H, Kuwahara H, Ishida H, Ishiguro K, Fujita T, Ueda K (1998) The ultrastructural characteristics of eccrine sweat glands in a Fabry disease patient with hypohidrosis. J Dermatol Sci 18: 109–117
Lenoir G, Rivron M, Gubler MC, Dufier JL, Tome FS, Guivarch M (1977) Fabry's disease. Carbamazepine therapy in acrodyniform syndrome. Arch Fr Pediatr 34: 704–716
Lockman LA, Hunninghake DB, Krivit W, Desnick RJ (1973) Relief of pain of Fabry's disease by diphenylhydantoin. Neurology 23: 871–875
Luciano CA, Russell JW, Banerjee TK, Quirk JM, Scott LJ, Dambrosia JM, Barton NW, Schiffmann R (2002) Physiological characterization of neuropathy in Fabry's disease. Muscle Nerve 26: 622–629
MacDermot KD, Holmes A, Miners AH (2001) Anderson-Fabry disease: clinical manifestations and impact of disease in a cohort of 60 obligate carrier females. J Med Genet 38: 769–775
MacDermot KD, Holmes A, Miners AH (2001) Anderson-Fabry disease: clinical manifestations and impact of disease in a cohort of 98 hemizygous males. J Med Genet 38: 750–760
Mayes JS, Scheerer JB, Sifers RN, Donaldson ML (1981) Differential assay for lysosomal alpha-galactosidases in human tissues and its application to Fabry's disease. Clin Chim Acta 112: 247–251
Miyatake T, Atsumi T, Obayashi T, Mizuno Y, Ando S, Ariga T, Matsui-Nakamura K, Yamada T (1979) Adult type neuronal storage disease with neuraminidase deficiency. Ann Neurol 6: 232–244
O'Brien BD, Shnitka TK, McDougall R, Walker K, Costopoulos L, Lentle B, Anholt L, Freeman H, Thomson AB (1982) Pathophysiologic and ultrastructural basis for intestinal symptoms in Fabry's disease. Gastroenterology 82: 957–962
Qin G, Takenaka T, Telsch K, Kelley L, Howard T, Levade T, Deans R, Howard BH, Malech HL, Brady RO, Medin JA (2001) Preselective gene therapy for Fabry disease. Proc Natl Acad Sci USA 98: 3428–3433
Ries M, Wendrich K, Whybra C, Kampmann C, Gal A, Beck M (2001) Angiokeratoma and pain, but not Fabry's disease: considerations for differential diagnosis. Contrib Nephrol 136: 256–259
Ries M, Mengel M, Kutschke G, Kim KS, Birklein F, Krummenauer F, Beck M (2003) Use of gabapentin to reduce chronic neuropathic pain in Fabry disease. J Inherit Metab Dis 26: 413–414
Schiffmann R, Kopp JB, Austin HA 3rd, Sabnis S, Moore DF, Weibel T, Balow JE, Brady RO (2001) Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA 285: 2743–2749
Wenger DA, Sattler M, Mueller OT, Myers GG, Schneiman RS, Nixon GW (1980) Adult GM1 gangliosidosis: clinical and biochemical studies on two patients and comparison to other patients called variant or adult GM1 gangliosidosis. Clin Genet 17: 323–334
Whybra C, Kampmann C, Willers I, Davies J, Winchester B, Kriegsmann J, Bruhl K, Gal A, Bunge S, Beck M (2001) Anderson-Fabry disease: clinical manifestations of disease in female heterozygotes. J Inherit Metab Dis 24: 715–724
Whybra C, Wendrich K, Miebach E, Baehner F, Ries M, Schmiedeskamp C, Kampmann C, Beck M (2001) Fabry disease: Mainz Severity Score Index (MSSI). J Inherit Metab Dis 24[Suppl.2]: 133–134
Yuen NW, Lam CW, Chow TC, Chiu MC (1997) A characteristic dissection microscopy appearance of a renal biopsy of a Fabry heterozygote. Nephron 77: 354–356
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ries, M., Ramaswami, U., Parini, R. et al. The early clinical phenotype of Fabry disease: a study on 35 European children and adolescents. Eur J Pediatr 162, 767–772 (2003). https://doi.org/10.1007/s00431-003-1299-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-003-1299-3