Abstract
The SnoB study analysed the variability of the integrase (IN) gene of non-B viruses from treatment-naïve patients to determine whether non-B subtypes carry natural resistance mutations to raltegravir (RAL). Plasma viral RNA from 427 patients was gained, and IN sequences were subtyped and screened for subtype-specific highly-variable residues. Seven viruses of different subtypes were phenotypically tested for RAL susceptibility; 359/427 samples could be sequenced. One hundred and seventy samples (47%) were classified as non-B subtypes. No primary RAL resistance–associated mutations (RRAMs) were detected. Certain secondary mutations were found, mostly related to specific non-B subtypes. L74 M was significantly more prevalent in subtype 02_AG, T97A in A and 06_cpx, V151I in 06_cpx, and G163R in 12_BF. Various additional mutations were also detected and could be associated with the subtype too. While K156 N and S230 N were correlated with B subtype, V72I, L74I, T112I, T125A, V201I and T206S were more frequent in certain non-B subtypes. The resistance factors (RF) of 7 viral strains of different subtypes ranged from 1.0 to 1.9. No primary or secondary but subtype-associated additional RRAMs were present. No correlation between RF and additional RRAMs was found. The prevalence of RRAMs was higher in non-B samples. However, the RFs for the analysed non-B subtypes showed lower values to those reported relevant to clinical failure. As the role of baseline secondary and additional mutations on RAL therapy failure is actually not known, baseline IN screening is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The HIV-1 integrase inhibitor (INI) raltegravir (RAL, MK-0518, Isentress®) is indicated for the treatment of adult HIV-infected patients in combination with other antiretroviral agents. RAL blocks the strand-transfer activity of the viral integrase (IN), necessary for the integration of the proviral DNA into the host genome. In addition, other strand-transfer inhibitors are already in clinical studies [1–7].
So far, clinical studies illustrating the effectiveness of RAL were focused on HIV-1 subtype B [3, 4, 8–11]. However, more than 90% of HIV-1-infected people worldwide harbour non-B subtypes [12]. Caused by migration movements and international tourism, a large number of HIV-positive patients with different non-B subtypes are meanwhile treated in Germany. The non-B prevalence in the German State of NRW (RESINA Study) from 2001 to 2009 was on average 28% (SD 3.9%).
As known for the protease and the reverse transcriptase, subtype-specific mutations in the target gene may also have an impact on the activity of antiretroviral drugs [13, 14].
The purpose of the SnoB study was to analyse the variability of the HIV-1 IN gene of non-B subtypes from antiretroviral treatment-naïve patients to determine whether non-B subtypes carry natural resistance-associated mutations to RAL.
Methods
The SnoB study is a prospective cohort study enrolling HIV-1-infected patients being treated in 24 German centres. Patients included in this study were suspected to carry non-B subtype viruses, therapy-naïve for all classes of antiretroviral drugs and signed an informed consent prior to any study procedures.
At the Institute of Virology of the University of Cologne, 427 plasma samples were analysed centrally. Viral RNA was isolated, amplified and sequenced as described recently [15]. Each IN sequence was subtyped with the geno2pheno[integrase] tool (http://integrase.bioinf.mpi-inf.mpg.de/index.php) and screened for mutations in comparison with the subtype B reference strain HXB2 to identify subtype-specific polymorphisms. It was analysed whether the detected variations corresponded to reported RAL resistance–associated mutations (RRAMs). The detected B sequences served as comparison group.
RRAMs were classified in primary, secondary and additional mutations, according to Sichtig et al. [15]. Briefly, primary RRAMs significantly increase the IC50 for RAL and are selected in vivo under RAL treatment. Secondary RRAMs further increase the IC50 for RAL and/or restore the viral fitness of viruses carrying primary mutations. Additional mutations have been selected under RAL treatment in vitro, and their importance for RAL resistance in vivo is still not clear.
M7 cells were used for the phenotypic determination of RAL resistance of 12 viral isolates comprising different subtypes. M7 cells contain a luciferase gene under the control of the HIV-1-LTR so that after integration of proviral DNA into the host cell genome, luciferase is produced. For the RAL susceptibility assay, infectious doses inducing approximately 10,000 relative light units within 3 days were used to infect 25,000 M7 cells cultivated in 200 μl RPMI media supplemented with SPG, 10% FCS, and either without or with increasing concentrations of RAL (from 3.2nM to 1 μM). The IC50 values were calculated via the luciferase activity. The IC50 shown are mean values from three valid runs.
Clinical data like gender, birth date, country of origin, year of first HIV diagnosis, transmission risk, suspected place of infection, CDC stage, CD4+-T-cell counts and viral loads were collected. Clinical data and results of the genotypic and phenotypic tests were compared with each other.
P-values were calculated by Fisher′s exact probability test, 2010 (http://faculty.vassar.edu/lowry/tab2x2.html).
Results
Subtyping
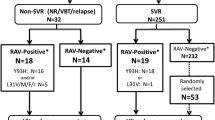
In this study, 427 patients were included; 359/427 samples could be amplified and sequenced; 189 (52.6%) were classified as B; and 170 (47.4%) as non-B subtypes by the geno2pheno[integrase] tool (Fig. 1). The most frequent non-B subtype was the circulating recombinant form (CRF) 02_AG with 26.5% followed by the A subtype with 25.3%. Subtype C was found in 13.5% and the 01_AE in 10% of the analysed non-B samples. The subtypes D and G were also detected in high percentages (D: 8.8%; G: 6.5%). All other subtypes were found in frequencies less than 5%.
Clinical characteristics
The clinical characteristics of the 427 patients are summarised in Table 1.
Although the patients included in our SnoB study were predominantly men (64.2%), the proportion of men and women differed depending on viral subtypes they were carrying; while 88.4% of the patients with B viruses were men, only 51.8% of the patients with non-B viruses were men, so the percentage of women infected with non-B subtypes was 6.5-fold higher than B-infected women.
Subtype B-infected patients had in median higher viral loads than patients with non-B subtypes.
Patients harbouring subtype-B strains originated mainly from Europe (83.6%), while those with non-B viruses, comprising many different subtypes, came from all over the world. The CRFs 06_CPX and 10_CD were only detected in patients with an African origin (Fig. 2).
RRAMs
Subtype B viruses displayed a median of 2 (range 0–6) RRAMs per genome while non-Bs showed 3 (0–6). No primary RRAMs were detected (Table 2).
The secondary mutations L74 M, T97A Y143H, V151I and G163R were detected in frequencies ≤2.5% and limited to ≤1 per genome. They statistically correlated with specific non-B subtypes (Table 3). L74 M was present in 8.9% of the CRF 02_AG samples, T97A in 7.0% and 33.3% of the A and 06_cpx isolates (respectively), V151I in 66.7% of the 06_cpx, and G163R in 50% of the 12_BF samples. Y143H was not detected in clade B viruses but in 4.3% of the C viruses, although the different prevalence lacked statistical significance.
Additional RRAMs were also detected, yet in a higher prevalence (≤73.8%) and with a median prevalence of 3 (0–7) mutations/genome in B isolates and 4 (0–6) in non-Bs. Certain additional mutations were associated with specific HIV-1 subtypes. The mutations K156 N and S230 N were present in a significantly higher proportion in the B isolates (Table 2). S119GPRT and V72I were more frequent in subtype B isolates than the total of non-B sequences (Table 2), although they significantly correlated with specific non-B subtypes (Table 3). S119GPRT was found in 51.2% of the subtype A isolates, and V72I was more frequent in subtype C (91.3%). The mutations L74I, T112I, T125A, V201I and T206S were more prevalent in non-B subtypes. The L74I, found in 20% of the non-B isolates (Table 2), had a higher prevalence in subtype A (46.5%) and 02_AG (20.9%). T112I was found in 17.6% of the non-B samples, but in 71.4 and 54.5% of F and G isolates, respectively, and the T206S, detected in only 42.4% of the non-B subtypes, was predominant in the subtypes 02_AG (95.6%), G (90.9%) and F (57.1%). The mutations T125A and V201I, with the highest frequencies in our analysed non-B samples (T125A = 86.5%; V201I = 95.3%), associated with most non-B subtypes. The prevalence of the mutations A128T, M154I, E157Q, V165I, and I203 M could not be significantly associated with any specific subtype.
Phenotypic RAL resistance determination
Twelve viral strains corresponding to different subtypes were analysed for phenotypic susceptibility to RAL.
Nine of twelve viral supernatants induced sufficient amounts of luciferase activities after initial infection and could be used for to infect M7 cells in the presence of increasing concentrations of RAL. Six independent runs were performed for each viral supernatant and twelve for the reference virus NL4-3. For the isolate corresponding to the subtype 01_AE, the IC50 value could not be calculated due to too low luciferase activities. For all other supernatants, IC50 values from at least three independent runs could be calculated. All other runs had to be excluded because the curves cut 50% more than once. The resistance factors (RF) ranged from 1.0 to 1.9 (Fig. 3).
The genotypic analysis of the phenotypic tested samples revealed no primary or secondary but different additional mutations. No correlation between RF and additional RRAMs could be found.
Discussion
The clinical studies conducted to analyse the effectiveness of RAL have been focused on HIV-1 subtype B [3, 4, 8–11]. However, over 90% of HIV-1 infections worldwide and 26.2% of the infected patients in Germany carry non-B viruses.
The SnoB study confirmed the distribution of non-B viruses circulating in therapy-naïve patients in Germany. The high proportion of detected 02_AG isolates in Germany can be related to the high migration rate of patients with an African origin. The total prevalence of B viruses (44.3%) in this study is exceptionally low as predominantly patients with known or assumed non-B infection were enrolled in this study.
Three primary mutations N155H, Q148RHK or Y143RC conferring RAL resistance in vivo have been described [3, 4, 10, 15–17]. In addition, the replacement of one resistance mutational pattern by another has been observed in patients experiencing prolonged virological failure of a RAL-containing regimen [15, 18–20]. Secondary mutations, which further increase the RAL resistance level, are frequently observed in these profiles. E92Q, in addition to being a secondary mutation for RAL resistance in vivo and in vitro, may play a critical role in the development of resistance to another INI, namely elvitegravir (EVG) [21].
No primary but certain secondary and additional RRAMs were detected in this cohort of therapy-naïve patients, in accordance with previous reports [15, 20, 22–26]. The number and type of RRAMs varied between B and non-B subtypes. B isolates displayed, on average, less RRAMs per genome than non-Bs. No secondary RRAMs correlated with the B subtype, while L74 M, T97A, V151I and G163R could be significantly associated with specific non-B subtypes. For all the subtypes analysed, only the CRF 06_cpx correlated with more than one baseline secondary RRAMs. Concerning the additional mutations, V72I, L74I, T112I, T125A, V201I and T206S could also be related to certain non-B subtypes, and only K156 N and S230RN were significantly more prevalent in B isolates.
In a first attempt to investigate whether these mutational patterns led to different RAL susceptibilities among subtypes, 12 viral isolates corresponding to different HIV-1 clades were tested in a phenotypic resistance assay. The RFs detected in 7 viral isolates ranged from 1.0–1.9, values far below to those reported for the single primary mutations (RF~13 for N155H and Y143RC and 18 < RF < 38 for Q148RHK), which correlate with in vivo RAL treatment failure [19, 27, 28]. Taken together, our results support the idea that baseline RRAMs do not seem to severely reduce RAL susceptibility and that RAL may be safely administrated to most patients carrying non-B viruses [3, 4, 29].
However, to date, it is not clear whether baseline RRAMs may have a role in the development of resistance under RAL therapy, as it has been described for PIs, where certain baseline mutations lower the genetic barrier [14]. In fact, secondary and additional mutations do not only affect the RF but also restore or even increase the viral fitness, facilitating the appearance of primary resistance mutations such as the Q148H and the N155H that lead to a 3.4–13.7-fold reduction in the relative viral fitness in comparison with the wild type in the absence of RAL [19, 27, 30]. Indeed, certain studies suggest that baseline RRAMs may have an influence on future RAL resistance development. In a study by Sichtig and colleagues [15], it has been shown that the baseline T206S was not detectable in isolates harbouring the G148HR at RAL failure, but was present in 3/7 samples presenting the N155H mutation. The appearance of the Y143CR at RAL failure correlated with the baseline T97A in 3/4 patients or 1/1 in two previous studies [15, 31]. Ceccerini-Silberstein and colleagues also showed that all three viruses displaying the V165I at baseline developed the N155H at therapy failure. In addition to this, other studies have found RAL therapy failure without the emergence of primary RRAMs [32, 33]. These studies illustrate the potential importance of secondary and additional mutations in contributing to resistance to RAL regimens.
Therefore, although RAL may be safely administrated to most patients carrying non-B viruses, baseline screening should be always performed, in order to identify RRAMs that may influence future RAL resistance development. In addition, prospective studies analysing large numbers of antiretroviral therapy naïve patients taking raltegravir as part of a first-line regimen are mandatory to clarify the clinical significance of baseline RRAMs.
References
Markowitz M, Morales-Ramirez JO, Nguyen BY, Kovacs CM, Steigbigel RT, Cooper DA, Liporace R, Schwartz R, Isaacs R, Gilde LR, Wenning L, Zhao J, Teppler H (2006) Antiretroviral activity, pharmacokinetics, and tolerability of MK-0518, a novel inhibitor of HIV-1 integrase, dosed as monotherapy for 10 days in treatment-naive HIV-1-infected individuals. J Acquir Immune Defic Syndr 43(5):509–515
Grinsztejn B, Nguyen BY, Katlama C, Gatell J, Lazzarin A, Vittecoq D, Gonzalez C, Chen J, Isaacs R, Team Tps (2006) Potent antiretroviral effect of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus. In: 13th conference on retroviruses and opportunistic infections (CROI), Denver, USA, 5–8 February 2006. p Abstract 159LB
Cooper D, Gatell J, Rockstroh J, Katlama C, Yeni P, Lazzarin A, Chen J, Isaacs R, Teppler H, Nguyen B, Group B-S (2007) Results of BENCHMRK-1, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus. In: 14th conference on retroviruses and opportunistic infections (CROI), Los Angeles, CA, USA, 25–28 February 2007. p Abstract 105aLB
Steigbigel R, Kumar P, Eron J, Schechter M, Markowitz M, Loufty M, Zhao J, Isaacs R, Nguyen BY, Teppler H, Group tB-S (2007) Results of BENCHMRK-2, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus. In: 14th conference on retroviruses and opportunistic infections (CROI), Los Angeles, CA, USA, 25–28 February 2007. p Abstract 105bLB
Zolopa AR, Berger DS, Lampiris H, Zhong L, Chuck SL, Enejosa JV, Kearney BP, Cheng AK (2010) Activity of elvitegravir, a once-daily integrase inhibitor, against resistant HIV Type 1: results of a phase 2, randomized, controlled, dose-ranging clinical trial. J Infect Dis 201(6):814–822. doi:10.1086/650698
Arribas J, Lazzarin A, Raffi F, Rakhmanova A, Richmond G, Rockstroh J, van Lunzen J, Young B, Almond S, Brothers C, Min S, Nichols G (2010) Once-daily S/GSK1349572 as part of combination therapy in antiretroviral naïve adults: rapid and potent antiviral responses in the interim 16-week analysis from SPRING-1 (ING112276). In: 18th international conference on AIDS, Vienna, Austria, 2010. p Abstract THLBB205
Eron J, Durant J, Poizot-Martin I, Reynes J, Soriano V, Kumar P, Richmond G, Vittecoq D, Fujiwara T, Ait-Khaled M, Min S, Thomas D, Cuffe R, Yeo J (2010) Activity of a next generation integrase inhibitor (INI), S/GSK1349572, in subjects with HIV exhibiting raltegravir resistance: initial results of VIKING study (ING112961). In: 18th international conference on AIDS, Vienna, Austria, 2010. p Abstract MOAB0105
DeJesus E, Berger D, Markowitz M, Cohen C, Hawkins T, Ruane P, Elion R, Farthing C, Zhong L, Cheng AK, McColl D, Kearney BP (2006) Antiviral activity, pharmacokinetics, and dose response of the HIV-1 integrase inhibitor GS-9137 (JTK-303) in treatment-naive and treatment-experienced patients. J Acquir Immune Defic Syndr 43(1):1–5
Grinsztejn B, Nguyen B, Katlama CB, Gatell J, Lazzarin A, Vittecoq D, Gonzalez C, Chen J, Isaacs R, Team TP (2007) 48 week efficacy and safety of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus. In: 47th ICAAC, Chicago, 2007. Abstract H-713
Hazuda DJ, Miller MD, Nguyen BY, Zhao J (2007) Resistance to HIV-integrase inhibitor raltegravir: analysis of protocol 005, a Phase II study in patients with triple-class resistant HIV-1 infection. Antiviral Ther 12:10
Lennox J, DeJesus E, Lazzarin A, Pollard R, Madruga JVR, Zhao J, Xu X, Williams-Diaz A, Rodgers A, DiNubile M, Nguyen BY, Leavitt R, Sklar P, Investigators tS (2008) Safety and efficacy of Raltegravir-based versus Efavirenz-based combination therapy in treatment naive HIV-1 infected patients. STARTMRK protocol 021. In: ICAAC-IDSA Washington DC, USA, 2008. Abstract H-896a
Taylor BS, Sobieszczyk ME, McCutchan FE, Hammer SM (2008) The challenge of HIV-1 subtype diversity. N Engl J Med 358(15):1590–1602
Deforche K, Silander T, Camacho R, Grossman Z, Soares MA, Van Laethem K, Kantor R, Moreau Y, Vandamme AM (2006) Analysis of HIV-1 pol sequences using Bayesian networks: implications for drug resistance. Bioinformatics 22(24):2975–2979
Kantor R, Katzenstein DA, Efron B, Carvalho AP, Wynhoven B, Cane P, Clarke J, Sirivichayakul S, Soares MA, Snoeck J, Pillay C, Rudich H, Rodrigues R, Holguin A, Ariyoshi K, Bouzas MB, Cahn P, Sugiura W, Soriano V, Brigido LF, Grossman Z, Morris L, Vandamme AM, Tanuri A, Phanuphak P, Weber JN, Pillay D, Harrigan PR, Camacho R, Schapiro JM, Shafer RW (2005) Impact of HIV-1 subtype and antiretroviral therapy on protease and reverse transcriptase genotype: results of a global collaboration. PLoS Med 2(4):e112
Sichtig N, Sierra S, Kaiser R, Däumer MP, Reuter S, Schülter E, Altmann A, Fäktenheuer G, Dittmer U, Pfister H, Esser S (2009) Raltegravir resistance mutation profiles: baseline situation and modification during treatment. J Antimicrob Chemother 64(1):25–32
Stürmer M, Doerr HM, Gürtler L (2009) Human immunodeficiency virus: 25 years of diagnostic and therapeutic strategies and their impact on hepatitis B and C virus. Med Microbiol Immunol 198(3):147–155. doi:10.1007/s00430-009-0117-6
Fransen S, Grupta S, Danovich R, Hazuda DJ, Miller M, Witmer M, Petropoulos CJ, Parkin NT, Huang W (2008) Loss of raltegravir susceptibility in treated patients is conferred by multiple non-overlapping genetic pathways. Antiviral Ther 13(Suppl 3):A9
Fransen S, Karmochkine M, Huang W, Weiss L, Petropoulos CJ, Charpentier C (2009) Longitudinal analysis of raltegravir susceptibility and integrase replication capacity of human immunodeficiency virus type 1 during virologic failure. Antimicrob Agents Chemother 53(10):4522–4524. doi:10.1128/AAC.00651-09
Miller MD, Danovich RM, Ke Y, Witmer M, Zhao J, Harvey CM, Nguyen BY, Hazuda DJ (2008) Longitudinal analysis of resistance to the HIV-1 integrase inhibitor reltegravir: results from P005 a phase II study in treatment-experienced patients. Antiviral Ther 13(Suppl 3):A8
Anies G, da Silva D, Recordon-Pinson P, Reigadas S, Wittkop L, Neau D, Morlat P, Fleury H, Masquelier B (2009) Analysis of raltegravir-resistant patterns including mutations at positions 143 and 155 in the HIV-1 integrase. In: 16th conference on retroviruses and opportunistic infections (CROI), San Francisco, CA, USA, February 16–19, 2009. Abstract 619
Jones G, Ledford R, Yu F, Miller M, Tsiang M, McColl D (2007) Resistance profile of HIV-1 mutants in vitro selected by the HIV-1 integrase inhibitor, GS-9137 (JTK-303). In: 14th conference on retroviruses and opportunistic infections (CROI), Los Angeles, CA, USA, 25–28 February 2007. Foundation for retrovirology and human health, Alexandria, VA, USA, p Abstract 627
Hackett Jr J, Harris B, Holzmayer V, Yamaguchi J, Luk KC, Brennan C, Schochetman G, Devare S, Swanson P (2008) Naturally occurring polymorphisms in HIV-1 group M, N, and O integrase: implications for integrase inhibitors. In: 15th conference on retroviruses and opportunistic infections (CROI), Boston, MA, USA, 3–6 February 2008. Foundation for retrovirology and human health, Alexandria, VA, USA, p Abstract 872
Garrido C, Geretti AM, de Mendoza C, Booth C, Strang A, Soriano V Polymorphisms at the integrase gene in distinct HIV populations may influence the susceptibility to integrase inhibitors. In: 6th European HIV Drug Resistance Workshop, Budapest, Hungary, 26-28 March 2008. Virology Education, BJ Utrecht, Netherlands, p Abstract 12
Yerly S, Hirschel B, Gaille C, Kaiser L, Perrin L (2007) Polymorphism of HIV-1 subtypes B and non-B integrase gene. In: 14th conference on retroviruses and opportunistic infections (CROI), Los Angeles, CA, USA, 25–28 February 2007. Foundation for retrovirology and human health, Alexandria, VA, USA, p Abstract 626
Lataillade M, Chiarella J, Kozal MJ (2007) Natural polymorphism of the HIV-1 integrase gene and mutations associated with integrase inhibitor resistance. Antivir Ther 12(4):563–570
Myers RE, Pillay D (2007) HIV-1 integrase sequence variation and covariation. Antiviral Ther 12:5
Van Baelen K, Rondelez E, Van Eygen V, Smits V, Van den Zegel P, Stuyver LJ (2008) Validation of a genotypic and phenotypic recombinant viruses assay to determine resistance against HIV-1 inhibitors. Antiviral Ther 13(Suppl 3):A127
Goodman D, Hluhanich R, Waters J, Margot NA, Fransen S, Gupta S, Huang W, Parkin N, Borroto-Esoda K, Svarovskaia ES, Miller MD, McColl DJ (2008) Integrase inhibitor resistance involves complex interactions among primary and secondary resistance mutations: a novel mutation L68 V/I associates with E92Q and increases resistance. In: XVII international HIV drug resistance workshop sitges, Spain, 2008. p Abstract 7
Van Baelen K, Van Eygen V, Rondelez E, Stuyver LJ (2008) Clade-specific HIV-1 integrase polymorphisms do not reduce raltegravir and elvitegravir phenotypic susceptibility. AIDS 22(14):1877–1880. doi:10.1097/QAD.0b013e32830f9703
Hu Z, Kuritzkes DR (2010) Effect of raltegravir resistance mutations in HIV-1 integrase on viral fitness. J Acquir Immune Defic Syndr 55(2):148–155. doi:10.1097/QAI.0b013e3181e9a87a
Ceccherini-Silberstein F, Armenia D, D’Arrigo R, Micheli V, Fabeni L, Meraviglia P, Capetti A, Zaccarelli M, Trotta MP, Narciso P, Antinori A, Perno CF (2008) Virological response and resistance in multi-experienced patients treated with raltegravir. Antiviral ther 13(Suppl 3):A15
Brenner BG, Lowe M, Moisi D, Hardy I, Gagnon S, Charest H, Baril JG, Wainberg MA, Roger M (2011) Subtype diversity associated with the development of HIV-1 resistance to integrase inhibitors. J Med Virol
da Silva D, Van Wesenbeeck L, Breilh D, Reigadas S, Anies G, Van Baelen K, Morlat P, Neau D, Dupon M, Wittkop L, Fleury H, Masquelier B (2010) HIV-1 resistance patterns to integrase inhibitors in antiretroviral-experienced patients with virological failure on raltegravir-containing regimens. J Antimicrob Chemother 65(6):1262–1269
Acknowledgments
The authors thank Dörte Hammerschmidt for invaluable help in sample processing and MSD for supporting this study.
Ethical standards
Ethics approval was given from the responsible ethics committees.
Conflicts of interest
The authors have not any commercial or other association that may pose a conflict of interest with this manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Sierra, S., Lübke, N., Walter, H. et al. The SnoB study: frequency of baseline raltegravir resistance mutations prevalence in different non-B subtypes. Med Microbiol Immunol 200, 225–232 (2011). https://doi.org/10.1007/s00430-011-0194-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-011-0194-1