Abstract
Viral infections of the central nervous system (CNS) mostly represent clinically important, often life-threatening complications of systemic viral infections. After acute measles, CNS complications may occur early (acute postinfectious measles encephalitis, APME) or after years of viral persistence (subacute sclerosing panencephalitis, SSPE). In spite of a presumably functional cell-mediated immunity and high antiviral antibody titers, an immunological control of the CNS infection is not achieved in patients suffering from SSPE. There is still no specific therapy for acute complications and persistent MV infections of the CNS. Hamsters, rats, and (genetically unmodified and modified) mice have been used as model systems to study mechanisms of MV-induced CNS infections. Functional CD4+ and CD8+ T cells together with IFN-γ are required to overcome the infection. With the help of recombinant measles viruses and mice expressing endogenous or transgenic receptors, interesting aspects such as receptor-dependent viral spread and viral determinants of virulence have been investigated. However, many questions concerning the lack of efficient immune control in the CNS are still open. Recent research opened new perspectives using specific antivirals such as short interfering RNA (siRNA) or small molecule inhibitors. In spite of obvious hurdles, these treatments are the most promising approaches to future therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Measles virus (MV) belongs to the genus Morbillivirus of the family Paramyxoviridae [1]. After entering the upper respiratory tract, MV exhibits a pronounced tropism for mono- and lymphocytic cells, and soon viral replication is detected in draining lymph nodes [2]. In the course of its spread, MV remains highly cell associated and can be isolated from blood leukocytes early during infection. During measles, patients develop a pronounced leukopenia that may be due to an enhanced adhesion of lymphocytes in secondary lymphoid organs [3]. In immunocompetent patients, the MV infection is usually cleared by the virus-specific immune response, while the general immune response to other antigens is suppressed for several weeks after the rash (for review see: [4]).
Following replication in lymphoid tissues, virus spreads to various organs can be detected in the skin, where viral antigen is concentrated near blood vessels, and in endothelial cells of dermal capillaries, and may also enter the brain (for review see: [5]). Various routes of CNS invasion of MV (or other Morbilliviruses in their respective hosts) may be utilized, such as the blood stream and transmigration of infected leukocytes across the blood brain barrier (BBB), migration through the choroid plexus, infection of microvascular endothelial cells and basolateral virus release, or viral transport in infected nerves of the olfactory bulb [6–9]. We found that enhanced adhesion of infected leukocytes may play a role in the establishment of acute and persistent CNS complications, since in vitro experiments demonstrated that MV infection of leukocytes not only induced a block in their transmigratory capacity across endothelial barriers, but also enhanced their adhesion to endothelial cells and thus enabled the endothelial cell infection [10]. CNS invasion has also been investigated using canine distemper virus (CDV), another Morbillivirus, in ferrets. Here, after massive infection of the lymphatic system, CDV used both the anterograde and the hematogenous pathway for neuroinvasion [9].
As the most frequent CNS complication APME occurs in approximately 0.1% of cases with a lethality of approximately 20% [11], it is likely that a clinically inapparent cerebral dysfunction is common in uncomplicated measles as documented by abnormalities of the electro encephalogram (EEG) and pleocytosis in the cerebrospinal fluid (CSF) in about 50% of patients. Since MV-specific nucleic acids have been detected only with highly sensitive methods within the CNS of patients suffering from APME [12], the observed clinical signs are thought to result from a virally induced pathogenic immune response in the brain with autoimmune components [13, 14]. This inflammatory immune reaction may be triggered by infected leukocytes adhering to brain microvascular endothelial cells, or by infected endothelial cells in the brain.
In contrast to APME, MV is abundantly present in brain cells of patients with SSPE and measles inclusion body encephalitis (MIBE), both of which develop after clinically silent periods of months to years after acute measles and are inevitably fatal [15]. Whereas MIBE is confined to immunosuppressed or -deficient patients, and may thus be considered as an opportunistic infection of the CNS, SSPE develops with a frequency of 1:10000–20000 approximately 6–12 years after primary infection with wild-type MV in patients with an apparently normal antiviral immune response [11, 16–18]. As revealed by molecular epidemiological studies, the primary MV infection of patients with SSPE takes place predominantly below the age of 2, when the immune system of the host is still immature and residual maternal antibodies may be absent or not sufficient for complete virus neutralization. This immature immune response in conjunction with a transient immunosuppression due to other infections may favor the establishment of a persistent MV infection (see below: animal models). SSPE is characterized by an excessive intrathecal synthesis of MV-specific antibodies. Oligoclonal IgG bands detected by isoelectric focusing with MV-specific immunoblotting are present in the cerebrospinal fluid and the MV-specific IgG index is elevated [19, 20]. Serum titers of MV-specific IgG usually are also substantially elevated.
MV-specific sequences obtained from SSPE autopsy material are, except from mutations accumulated in certain regions of the genome (predominantly the matrix gene), homologous to the corresponding gene sequences of genotypes circulating at the time of primary exposure of the patients to MV [21–23]. In few cases, infectious viruses could be isolated from SSPE brains that conserved their highly neurovirulent properties after propagation in vitro in animal models [24–26]. However, recombinant MV containing the matrix gene from an SSPE isolate grows considerably less efficient in tissue culture and transgenic mice [27]. This strongly supports the notion that there are no circulating MV genotypes, which are particularly neurovirulent, and that persistent brain infections are established initially by ‘normal’ wild-type MV strains. After measles vaccination, SSPE is not observed [28, 29].
Mechanisms contributing to measles virus persistence and pathogenesis
The establishment of a viral CNS infection depends not only on the biological properties of the invading agent but also on the breakdown of the host defence mechanisms that normally protect cells in the CNS from infection. Due to existence of the BBB and absence of lymphatic tissues in the CNS, the immune response in this organ is peculiar. In addition, an unbalanced immune response in the immature host may play a decisive role for the early establishment of a persistent MV infection. As mentioned above, MV spread in brains of paients with SSPE occurs in the presence of extremely high titers of anti-measles antibodies. However, these antibodies fail to control the infection. Interestingly, it has been observed in tissue culture experiments that virus-neutralizing antibodies are capable of interfering with intracellular viral gene expression particularly in neural cells. In the presence of polyclonal anti-MV antibodies, a selective reduction of the viral P and M proteins was found in infected HeLa cells [30, 31]. A complete downregulation of intracellular viral transcription and protein expression following the treatment with neutralizing anti-H monoclonal antibodies was observed in persistently MV-infected rat glioma and mouse neuroblastoma cells, but not in persistently infected Vero and lung fibroblast cells [32, 33]. This so called antibody-induced antigenic modulation (AIAM) has been linked to a so far unidentified transmembrane signal, which leads intracellularly to the downregulation of the viral gene expression, and may support the establishment of a slow persistent viral infection.
The involvement of single nucleotide polymorphisms of immunologically important genes encoding molecules such as IL-2, IL-4, IL-12, MxA, and TLR-3 in the susceptibility to the establishment of SSPE is controversially discussed [34–38]. In the CSF of patients with SSPE, elevated levels of type I IFN have been detected and were suggested to play a role in the establishment of the slowly progressing persistent brain infection. The IFN-α/β-inducible human MxA protein, which interferes with transcription and/or translation of various viruses, exerts a direct antiviral activity against MV in tissue culture, and has been shown to be expressed in glial cells around active lesions in the brain of patients with SSPE [39–42]. In tissue culture, MV infection of neuroblastoma cells (in contrast to astrocytoma cells) failed to activate NF-kB, and to induce IFN-α/β and MHC class I expression [43, 44]. This failure may provide a potential mechanism allowing MV to persist preferentially in neurons. In addition, it has been found that wild-type MV-isolates have a considerably lower capacity to induce type I IFN in human peripheral blood lymphocytes than vaccine strains [45]. A different specific antiviral mechanism appears to be exerted by type II interferon (IFN-γ) in patients with SSPE, where an inverse correlation between IFN-γ production by peripheral blood mononuclear cells and disease progression was found [46]. Interestingly, IFN-γ exerts a direct antiviral role in tissue culture mediated to a large extent by indolamine-2,3-dioxigenase [47], an enzyme that has also immunoregulatory properties [48]. The importance of IFN-γ was confirmed in animal models (see below, [49, 50]). Discrepancies between various reports in the literature concerning IFN-γ, IL-6, IL-12, and IL-10 expression in patients with SSPE might be due to different ages of patients, stages of the disease, and treatments of the patients studied [51–54].
CD150 was identified as receptor for both, vaccine and wild-type MV strains [55–57], whereas CD46 acts as cellular receptor only for vaccine strains [58, 59]. In concordance with the lymphotropism of MV, the costimulatory molecule CD150 is expressed on activated T and B lymphocytes, memory cells, activated dendritic, and monocytic cells [60–62], but has not been found on epithelial, endothelial, and various brain cell types [8, 63]. However, in SSPE brains, neurons, oligodendrocytes, astrocytes, and few microvascular endothelial cells are infected [7]. Therefore, it is likely that wild-type MV utilizes additional molecule(s) as receptors on these cells as well as on epithelial cells [64–66], the nature of which is still unknown. Within heavily infected MV-positive brain lesions of patients with SSPE, CD46 was undetectable, independent of whether MV antigens were present in these individual cells, whereas in SSPE brain tissue distant from the lesion, normal levels of CD46 were found suggesting that CD46 expression was reduced by the MV infection [8, 63].
As documented by immunohistochemistry and later by sequence analyses from autopsies, the expression of MV envelope proteins is strongly reduced in brains of patients with SSPE and MIBE. Transcriptional restrictions of the corresponding genes and mutations within the coding sequences interfering with the synthesis of functional gene products were found [67]. As a consequence, the expression of viral envelope proteins (matrix (M), fusion (F), and haemagglutinin (H) protein) is restricted by various means. In particular the M and the cytoplasmic part of the F protein harbor single or hyper-mutations or deletions, which prevent their proper expression, reduce budding, support cell fusion, and enhance intracellular RNP replication [68–70]. Cell-to-cell spread of virus appears to be an important mechanism supporting persistence in the human and animal models of measles encephalitis [7, 71–73]. MV spreads in differentiated human neuronal cells lacking CD150 and CD46, as well as in CD46-positive human neuroblastoma cells, in astrocytoma, and in oligodendroglioma cells by an intracellular route, most likely involving local microfusion events at cell contact points [74]. Vesicular stomatitis viruses pseudotyped with viral envelope proteins from patients with SSPE infected target cells in a CD150- and CD46-independent manner, confirming that for infection of neural cells, other unknown receptors are used [75].
Taken together, an early infection in life, a genetic predisposition, the IFN-response in glial cells and its possible lack in neurons, the antibody-induced antigenic modulation, and a steep viral expression gradient, the accumulation of point- and hypermutations within envelope genes associated with enhanced intracellular replication of RNPs, and the cell-to-cell spread of RNPs support the persistent brain infection and the failure of the immune response to eliminate the virus.
Animal models of the CNS infection
Resistance and susceptibility to MV-induced encephalitis in rodents correlate with the MHC haplotype of the respective inbred strain [76–78]. In resistant mouse strains, depletion of the CD4+ T-cell subset by monoclonal antibodies led to a breakdown of resistance, whereas depletion of CD8+ T cells had no effect [79]. This may be different in the human, since in vitro experiments demonstrated that CD8+ T lymphocytes control the dissemination of virus [80]. The importance of antigen presentation for the immune defense became evident in TAP-transporter-deficient mice, which cannot present antigen on MHC class I molecules [72]. Under these conditions, MV was found to spread considerably more transneuronally to the next order of neurons. This indicates that infected neurons are indeed target cells of cytotoxic T lymphocytes (CTL), and that brain infections to some extent can be inhibited by CTL activity. A breakdown of resistance is also observed after neutralization of IFN-γ leading to the generation of a TH2 response [49, 81]. Further investigation into this measles encephalitis model revealed that CD4+ T cells are able to protect either alone, through cooperation with CD8+ T cells, or after immunization as secondary T cells (depending on the mouse strain used), and CD8+ T cells are able to protect alone after immunization if they are cytolytic [81, 82]. As found earlier in non-transgenic mice, IFN-γ has also a critical role for the protection of CD46-transgenic mice against MV encephalitis [50]. Interestingly, this protection functions in a non-cytolytic manner without neuronal loss. Hyperthermic pre-conditioning of mice enhanced the efficacy of the cell-mediated immune response and promoted virus clearance from the brains of persistently infected mice [83].
Interestingly, MV lacking the complete matrix protein is functional and spreads even more efficiently in the brain of CD46-transgenic IFN-α/β-receptor-deficient mice [84]. When a matrix gene of an SSPE isolate was introduced in a recombinant MV, this virus replicated at a reduced level, but led to a protracted CNS infection in CD46-transgenic mice [27]. MV spreads also in rat hippocampal neurons by cell-to-cell contact and in a polarized fashion [85].
We investigated importance of the viral H protein for virus spread and neurovirulence using a recombinant MV in which the H gene of MV Edmonston had been replaced by the H gene of the neurovirulent strain CAM/RB. After intracerebral injection into suckling C57BL/6 mice, this recombinant virus-induced neurological disease and MV antigen were found in neurons and neuronal processes of the hippocampus, frontal, and olfactory cortices and neostriatum [86, 87]. Replacement of only two amino acids in the CAMH-protein at positions 195 G → R and 200 S → N caused the complete loss of neurovirulence, which points to the usage of unknown neuron-specific receptors by CAMH [88, 89]. The viral H protein plays also an important role for the neurovirulence of CDV in ferrets, in which the disease duration was determined by the viral H protein [90].
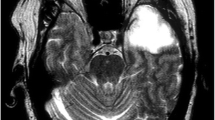
In order to investigate aspects of immune control, we established a model of persistent brain infection in fully immunocompetent mice using 2-weeks-old normal C57BL/6 mice, an age at which the mice survived the intracerebral (i.c.) infection, while the immune system is still not fully mature [91]. After i.c. infection with 1000 PFU recombinant MV-CAMH, virus spread is maximal after 1 week (Fig. 1), and later, approximately 80% of mice carry a persistent infection. These mice can be used to study the role of the immune response for the persistent CNS infection and to assess antivirals in the brain. In this mouse model, neither rodent CD46- and CD150-homologues function as MV receptors nor are required, and also transgenic human receptors are dispensible. This allows the use of any genetically modified mouse on C57BL/6 background to study immunologically relevant questions.
GFP expression in a brain of a 2-week-old mouse infected with recombinant measles virus MV-eGFP-CAMH [91]. The overview (coronal section) of the left hemisphere (a), enlargement (b), and GFP/marker co-localizations with neurofilament in neurons (red) (c), and absence of colocalization with GFAP in astrocytes (red) (d) demonstrates the exclusive infection of neurons
Other investigations were performed using mice expressing the human MV-receptors CD46 and/or CD150. Transgenic expression of CD46 in mice has been used to define the role of a cellular receptor for neurovirulence and pathogenicity. A similar susceptibility of newborn mice for infection with MV strain Edmonston as in non-transgenic animals was found in such mice expressing CD46 ubiquitously [92–95]. In the periphery of adult CD46-transgenic mice or rats, the receptor expression did not lead to a significant increase in susceptibility for MV [96, 97], whereas in IFN-α/β-receptor-deficient mice expressing CD46, intracerebral inoculation of adult animals with low doses of MV-Edm caused encephalitis with mostly lethal outcome [98]. Recent findings using CD46-transgenic neurokinin-1-deficient mice suggest that the substance P receptor is involved in trans-synaptic virus spread [99]. The ubiquitous expression of transgenic CD150 rendered suckling mice suceptible to intranasal infection with wildtype MV. Virus spreads to different organs including the brain, and these animals develop a neurologic disease leading to death within 3 weeks [100]. CD4+ CD25+ FoxP3+ regulatory T cells are enriched following infection, both in the periphery and in the brain [101].
Cytokines induced by the infection of neurons (or neural cells in general) are early important mediators of leukocyte recruitment to sites of viral infection. In brains of CD46-transgenic mice expressing CD46 exclusively in neurons, infiltrating leukocytes, the upregulation of MHC class I and II, and increased levels of RANTES, IP-10, IL-6, TNF-α, and IL-1β have been observed that preceded the infiltration of reactive T lymphocytes [102, 103]. Using CD46-transgenic Rag-deficient mice, adoptive transfer of lymphocytes revealed that the combined activity of CD4+ T lymphocytes with CD8+ T cells or B cells is required to control the intracerebral infection [104]. Furthermore, transgenic expression of CD150 alone or in combination with CD46 can mediate a substantial systemic MV infection only in conjunction with a defect in the innate immune system [105–107]. Thus, both the innate and the adaptive immune system play important roles to overcome MV-induced neuropathogenesis. CD46-transgenic Rag-deficient mice have also been used to test a hypothesis for the establishment of SSPE, which has been set up earlier in a hamster model [108], i.e. the role of a transient immunosuppression by another virus preceding the infection with MV (dual viral hits) [109]. According to these findings, the young immature immune system and transient immunosuppression during the acute MV infection may also in the human favor the establishment of the persistent brain infection and subsequent development of SSPE.
Approaches to a specific therapy
Newborn mice can be protected against MV infection by injection of monoclonal antibodies to the viral envelope proteins, or by vaccination with vaccinia virus recombinants expressing the corresponding antigens [110–112]. However, anti-MV antibodies can also support the establishment of a persistent infection [113]. In weanling Lewis rats, such monoclonal antibodies did not fully protect against encephalitis, but converted an acute into a subacute persistent infection, whereas the untreated control group succumbed invariably to a fatal encephalopathy within few days (for review see: [14]). Intraperitoneal vaccination with MV protected 2-weeks-old mice from intracerebral infection and subsequent persistent infection. However, when already persistently infected mice were vaccinated, this did not alter the extent of persistent CNS infection [91]. These findings and the fact that patients with SSPE have high concentrations of antiviral antibodies in both, serum and cerebrospinal fluid, suggest that antibodies against viral proteins cannot be used for a specific therapy of the human disease SSPE.
An effective treatment of SSPE is still not available and the usual treatment with ribavirin (RBV), inosiplex (isoprinosine), and intraventricular interferon-α (IFN-α) may at best prolong the disease course. Inosiplex is a drug that may activate the host immune system by increasing the number of effector lymphocytes, the function of interferons, and the production of IL-1 and IL-2, but its usage is controversial due to conflicting results. A possible treatment regimen for intraventricular IFN-α (with or without inosiplex) consists of 6-week courses started with 105 units/m2 of body surface area and subsequently increased to 106 units/m2 per day given for 5 days a week. Courses are repeated up to six times at 2–6 months intervals (for review, see: [114]).
RBV is a water-soluble synthetic nucleoside with broad spectrum of antiviral properties [115]. It has been shown to be active against MV and improved the survival of i.c. infected hamsters in an SSPE model when administered intracranially (10 mg/kg/day for 10 days), but did not improve the survival when administered intraperitoneally suggesting a failure to cross the BBB [116, 117]. Complexation of RBV with cyclodextrin-alpha leads to a five-fold decrease in the 50% inhibitory concentration (IC50) against MV in vitro [118]. Interestingly, the cyclodextrin complexation enabled the effective intraperitoneal administration of RBV in mice indicating an improved crossing of the BBB and bioavailability [119, 120]. The lethal dose for mice was determined to be 55 mg/kg RBV, and mice could be treated successfully with 40 mg/kg [119]. Although the high concentrations of RBV required have undesired side effects, its complexation with cyclodextrin could possibly improve the treatment of viral CNS infections with RBV-susceptible viruses.
It has been known for quite a while that MV-associated mortality can be decreased in children by treatment with vitamin A, which is recommended by the WHO [121–123]. There are manyfold effects of vitamin A on the immune system [124]; however, retinoids also directly inhibit MV replication in vitro in a number of cell lines and human peripheral blood mononuclear cells through nuclear retinoid receptor signaling [125]. The molecular mechanism has recently been described as a type I IFN-dependent bystander effect [126]. In a CDV infection model of ferrets, the effects of vitamin A could be demonstrated impressively [127]. Interestingly, low levels of serum vitamin A and beta-carotene have been observed in a fraction of patients with SSPE [128] suggesting that vitamin A supplementation may also support the interferon treatment of patients with SSPE.
Neurodegeneration caused by infection of mice with the hamster neurotropic strain of MV (HNT) could be inhibited by the N-methyl-d-aspartate (NMDA)-receptor antagonist MK801 suggesting that the virus may have indirect NMDA-receptor-dependent effects in the brain leading to the neuronal loss [129].
RNA interference has been described to be active against MV infections [70, 130, 131] and is principally applicable against the intracellularly replicating viral RNPs in SSPE brains. In our own studies [70, 133], we found that silencing of the viral RNP-mRNAs was highly efficient in reducing viral messenger and genomic RNA, whereas siRNA-mediated knockdown of the M protein not only enhanced cell–cell fusion, but also increased the levels of both, viral messenger and genomic RNAs by a factor of 2 to 2.5. These findings support older findings that the M protein acts as a negative regulator of the viral polymerase [132], a mechanism that probably contributes to the efficient replication and spread of M-defective RNPs in SSPE brains. Recently, the efficacy of lentiviral vector-constructs, which integrate after transduction into the cellular genome and permanently express antiviral short hairpin RNAs (shRNA), was tested using persistently MV-infected NT2 cells (human teratocarcinoma cells that can be terminally differentiated into neuronal cells by retinoic acid treatment)[133]. ShRNA against N, P and L –mRNAs led to a reduction of viral proteins below detectable levels in a high percentage of transduced cells and complete virus elimination within 2 weeks [133]. This demonstrated in tissue culture that persistently MV-infected neural cells can be cured by transduction of lentiviral vectors mediating long lasting expression of virus-specific shRNA. However, before antiviral siRNA is applicable in vivo in the brain, several problems must be solved, such as the usage of an optimal vector system for neurons and glial cells, the lack of even distribution in the CNS, and the problem that RNA interference requires the knowledge of exact target sequences in spite of the high frequency of mutations in MV genomes of patients with SSPE.
During the last years, new potent small molecules have successfully been selected that inhibit either MV entry, or the viral RNA-dependent RNA polymerase (RdRp). Virus entry can be inhibited with compounds interacting with the viral fusion protein [134, 135]. Five substituted anilides showed effective blockade of MV entry, one of which (AS-48) exhibited a 50% inhibitor concentration (IC50) of 0.6–3.0 μM against a panel of wild-type MV strains [136]. However, with respect to a persistent infection, it remains to be investigated if such entry inhibitors can control viral cell-to-cell spread in the brain under conditions, when only small amounts of envelope proteins are expressed. In contrast, inhibitors of the viral polymerase, the activity of which is required for the replication of intracellular viral RNPs, may be more promising therapeuticals. A high-throughput screening led to an active compound, which was further chemically improved to achieve the lead compound AS-136A that blocked viral RNA synthesis with IC50 values of as low as 12 nM, and no detectable cytotoxicity at concentrations below 300 μM [137–139]. Adaptation of different MV strains to growth in the presence of this compound identified three candidate hot spots for interaction with AS-136A that are located in conserved domains of the viral L-protein [140]. Recombinant MVs harboring individual resistance mutations showed some delay in the onset of viral growth in vitro suggesting that mutations in these L-protein domains may reduce viral fitness [140]. However, these findings also demonstrated that resistance mutations that enable viral escape may well be present or emerge in vivo.
Taken together, intracellular virus replication by the viral polymerase appears to be the optimal target for specific inhibitors that should be able to eliminate the infectivity from the infected brain. In spite of obvious hurdles, such as the escape of mutant viruses or the bioavailability, treatments with siRNA and small compounds are the most promising approaches to a successful therapy.
References
Rima BK, Duprex WP (2006) Morbilliviruses and human disease. J Pathol 208(2):199–214
de Swart RL, Ludlow M, de Witte L, Yanagi Y, van Amerongen G, McQuaid S, Yuksel S, Geijtenbeek TB, Duprex WP, Osterhaus AD (2007) Predominant infection of CD150(+) lymphocytes and dendritic cells during measles virus infection of macaques. PLoS Pathog 3(11):e178
Nanan R, Chittka B, Hadam M, Kreth HW (1999) Measles virus infection causes transient depletion of activated T cells from peripheral circulation. J Clin Virol 12:201–210
Schneider-Schaulies S, Schneider-Schaulies J (2009) Measles virus-induced immunosuppression. Curr Top Microbiol Immunol 330:243–269
Ludlow M, Allen I, Schneider-Schaulies J (2009) Systemic spread of measles virus: overcoming the epithelial and endothelial barriers. Thromb Haemost 102(6):1050–1056
Kirk J, Zhou AL, McQuaid S, Cosby SL, Allen IV (1991) Cerebral endothelial cell infection by measles virus in subacute sclerosing panencephalitis: ultrastructural and in situ hybridization evidence. Neuropathol Appl Neurobiol 17:289–297
Allen IV, McQuaid S, McMahon J, Kirk J, McConnell R (1996) The significance of measles virus antigen and genome distribution in the CNS in SSPE for mechanisms of viral spread and demyelination. J Neuropathol Exp Neurol 55:471–480
McQuaid S, Cosby SL (2002) An immunohistochemical study of the distribution of the measles virus receptors, CD46 and SLAM, in normal human tissues and subacute sclerosing panencephalitis. Lab Invest 82:1–7
Rudd PA, Cattaneo R, von Messling V (2006) Canine distemper virus uses both the anterograde and the hematogenous pathway for neuroinvasion. J Virol 80(19):9361–9370
Dittmar S, Harms H, Runkler N, Maisner A, Kim KS, Schneider-Schaulies J (2008) Measles virus-induced block of transendothelial migration of T lymphocytes and infection-mediated virus spread across endothelial cell barriers. J Virol 82(22):11273–11282
Weissbrich B, Schneider-Schaulies J, ter Meulen V (2003) Measles and its neurological complications. Marcel Dekker, New York
Nakayama T, Mori T, Yamaguchi S, Sonoda S, Asamura S, Yamashity R, Takeuchi Y, Urano T (1995) Detection of measles virus genome directly from clinical samples by reverse transcriptase-polymerase chain reaction and genetic variability. Virus Res 35:1–16
Esolen LM, Takahashi K, Johnson RT, Vaisberg A, Moench TR, Wesselingh SL, Griffin DE (1995) Brain endothelial cell infection in children with acute fatal measles. J Clin Invest 96:2478–2481
Liebert UG (1997) Measles virus infections of the central nervous system. Intervirology 40:176–184
ter Meulen V, Stephenson JR, Kreth HW (1983) Subacute sclerosing panencephalitis. In: Fraenkel-Conrat H, Wagner RR (eds) Comprehensive virology. Plenum Press, New York, pp 105–159
Takasu T, Mgone JM, Mgone CS, Miki K, Komase K, Namae H, Saito Y, Kokubun Y, Nishimura T, Kawanishi R, Mizutani T, Markus TJ, Kono J, Asuo PG, Alpers MP (2003) A continuing high incidence of subacute sclerosing panencephalitis (SSPE) in the eastern highlands of Papua New Guinea. Epidemiol Infect 131:887–898
Bellini WJ, Rota JS, Lowe LE, Katz RS, Dyken PR, Zaki SR, Shieh W-J, Rota PA (2005) Subacute sclerosing panencephalitis: More cases of this fatal disease are prevented by measles immunization than previously recognized. J Infect Dis 192:1686–1693
Garg RK (2008) Subacute sclerosing panencephalitis. J Neurol 255(12):1861–1871
Dörries R, ter Meulen V (1984) Detection and identification of virus specific oligoclonal IgG in unconcentrated cerebrospinal fluid by immuno blot technique. J Neuroimmunol 7:77–89
Pohl-Koppe A, Kaiser R, Meulen VT, Liebert UG (1995) Antibody reactivity to individual structural proteins of measles virus in the CSF of SSPE and MS patients. Clin Diagn Virol 4(2):135–147
Rima BK, Earle JAP, Baczko K, ter Meulen V, Carabana J, Caballero M, Celma ML, Fernandez-Munoz R (1997) Sequence divergence of measles virus haemagglutinin during natural evolution and adaptation to cell culture. J Gen Virol 78:97–106
Jin L, Beard S, Hunjan R, Brown D, Miller E (2002) Characterization of measles virus strains causing SSPE: a study of 11 cases. J Neurovirol 8:335–344
Forcic D, Baricevic M, Zgorelec R, Kruzic V, Kaic B, Marina BM, Sojat LC, Tesovic G, Mazuran R (2004) Detection and characterization of measles virus strains in cases of subacute sclerosing panencephalitis in Croatia. Virus Res 99(1):51–56
Ogura H, Ayata M, Hayashi K, Seto T, Matsuoka O, Hattori H, Tanaka K, Tanaka K, Takano Y, Murata R (1997) Efficient isolation of subacute sclerosing panencephalitis virus from patient brains by reference to magnetic resonance and computed tomographic images. J Neurovirol 3:304–309
Ito N, Ayata M, Shingai M, Furukawa K, Seto T, Matsunaga I, Muraoka M, Ogura H (2002) Comparison of the neuropathogenicity of two SSPE sibling viruses of the Osaka-2 strain isolated with Vero and B95a cells. J Neurovirol 8:6–13
Hotta H, Nihei K, Abe Y, Kato S, Jiang DP, Nagano-Fujii M, Sada K (2006) Full-length sequence analysis of subacute sclerosing panencephalitis (SSPE) virus, a mutant of measles virus, isolated from brain tissues of a patient shortly after onset of SSPE. Microbiol Immunol 50(7):525–534
Patterson JB, Cornu TI, Redwine J, Dales S, Lewicki H, Holz A, Thomas D, Billeter MA, Oldstone MBA (2001) Evidence that hypermutated M protein of a subacute sclerosing panencephalitis measles virus actively contributes to the chronic progressive CNS disease. Virology 291:215–225
Duclos P, Ward BJ (1998) Measles vaccines. A review of adverse events. Drug Experience 6:435–454
Campbell H, Andrews N, Brown KE, Miller E (2007) Review of the effect of measles vaccination on the epidemiology of SSPE. Int J Epidemiol 36(6):1334–1348
Joseph B, Oldstone M (1974) Antibody-induced redistribution of measles virus antigens on the cell surface. J Immunol 113(4):1205–1209
Fujinami RS, Oldstone MB (1980) Alterations in expression of measles virus polypeptides by antibody: molecular events in antibody-induced antigenic modulation. J Immunol 125(1):78–85
Barrett PN, Koschel K, Carter M, ter Meulen V (1985) Effect of measles virus antibodies on a measles SSPE virus persistently infected C6 rat glioma cell line. J Gen Virol 66:1411–1421
Schneider-Schaulies S, Liebert UG, Segev Y, Rager-Zisman B, Wolfson M, ter Meulen V (1992) Antibody-dependent transcriptional regulation of measles virus in persistently infected neural cells. J Virol 66(9):5534–5541
Inoue T, Kira R, Nakao F, Ihara K, Bassuny WM, Kusuhara K, Nihei K, Takeshita K, Hara T (2002) Contribution of the interleukin 4 gene to susceptibility to subacute sclerosing panencephalitis. Arch Neurol 59(5):822–827
Torisu H, Kusuhara K, Kira R, Bassuny WM, Sakai Y, Sanefuji M, Takemoto M, Hara T (2004) Functional MxA promoter polymorphism associated with subacute sclerosing panencephalitis. Neurology 62(3):457–460
Pipo-Deveza JR, Kusuhara K, Silao CL, Lukban MB, Salonga AM, Sanchez BC, Kira R, Takemoto M, Torisu H, Hara T (2006) Analysis of MxA, IL-4, and IRF-1 genes in Filipino patients with subacute sclerosing panencephalitis. Neuropediatrics 37(4):222–228
Yilmaz V, Demirbilek V, Gurses C, Yentur SP, Uysal S, Yapici Z, Yilmaz G, Muncey A, Cokar O, Onal E, Gokyigit A, Saruhan-Direskeneli G (2007) Interleukin (IL)-12, IL-2, interferon-gamma gene polymorphisms in subacute sclerosing panencephalitis patients. J Neurovirol 13(5):410–415
Ishizaki Y, Takemoto M, Kira R, Kusuhara K, Torisu H, Sakai Y, Sanefuji M, Yukaya N, Hara T (2008) Association of toll-like receptor 3 gene polymorphism with subacute sclerosing panencephalitis. J Neurovirol 1–6
Schnorr JJ, Schneider-Schaulies S, Simon-Jodicke A, Pavlovic J, Horisberger MA, ter Meulen V (1993) MxA-dependent inhibition of measles virus glycoprotein synthesis in a stably transfected human monocytic cell line. J Virol 67(8):4760–4768
Schneider-Schaulies S, Schneider-Schaulies J, Schuster A, Bayer M, Pavlovic J, ter Meulen V (1994) Cell type-specific MxA-mediated inhibition of measles virus transcription in human brain cells. J Virol 68(11):6910–6917
Lampe JB, Schneider-Schaulies S, Aguzzi A (2003) Expression of the interferon-induced MxA protein in viral encephalitis. Neuropathol Appl Neurobiol 29:273–279
Ogata S, Ogata A, Schneider-Schaulies S, Schneider-Schaulies J (2004) Expression of the interferon-a/b-inducible MxA protein in and around lesions of subacute sclerosing panencephalitis (SSPE) brains. Acta Neuropathol 223:113–119
Dhib-Jalbut S, Xia J, Rangaviggula H, Fang Y-Y, Lee T (1999) Failure of measles virus to activate nuclear factor-KB in neuronal cells: implications on the immune response to viral infections in the central nervous system. J Immunol 162:4024–4029
Fang Y-Y, Song Z-M, Dhib-Jalbut S (2001) Mechanism of measles virus failure to activate NFk-B in neuronal cells. J Neurovirol 7:25–34
Naniche D, Yeh A, Eto D, Manchester M, Friedman RM, Oldstone MBA (2000) Evasion of host defenses by measles virus: wild-type measles virus infection interferes with induction of alpha/beta interferon production. J Virol 74:7478–7484
Hara T, Yamashita S, Aiba H, Nihei K, Koide N, Good RA, Takeshita K (2000) Measles virus-specific T helper 1/T helper 2-cytokine production in subacute sclerosing panencephalitis. J Neurovirol 6:121–126
Obojes K, Andres O, Däubener W, Schneider-Schaulies J (2005) Indoleamine 2, 3 dioxygenase (IDO) mediates cell type specific anti-measles virus effects of interferon-gamma. J Virol 79:7768–7776
Mellor AL, Sivakumar J, Chandler P, Smith K, Molina H, Moao D, Munn DH (2001) Prevention of T cell-driven complement activation and inflammation by tryptophan catabolism during pregnancy. Nature Immunol 2:64–68
Finke D, Brinckmann UG, ter Meulen V, Liebert UG (1995) Gamma interferon is a major mediator of the antiviral defense in experimental measles virus-induced encephalitis. J Virol 69:5469–5474
Patterson CE, Lawrence DMP, Echols LA, Rall GF (2002) Immune-mediated protection from measles virus-induced central nervous system disease is non-cytolytic and gamma interferon dependent. J Virol 76:4497–4506
Saruhan-Direskeneli G, Gurses C, Demirbilek V, Yentur SP, Yilmaz G, Onal E, Yapici Z, Yalcinkaya C, Cokar O, Akman-Demir G, Gokyigit A (2005) Elevated interleukin-12 and CXCL10 in subacute sclerosing panencephalitis. Cytokine 32(2):104–110
Yentur SP, Gurses C, Demirbilek V, Yilmaz G, Onal AE, Yapici Z, Yalcinkaya C, Cokar O, Gokyigit A, Saruhan-Direskeneli G (2005) Alterations in cell-mediated immune response in subacute sclerosing panencephalitis. J Neuroimmunol 170(1–2):179–185
Ichiyama T, Siba P, Suarkia D, Reeder J, Takasu T, Miki K, Maeba S, Furukawa S (2006) Analysis of serum and cerebrospinal fluid cytokine levels in subacute sclerosing panencephalitis in Papua New Guinea. Cytokine 33(1):17–20
Aydin OF, Ichiyama T, Anlar B (2009) Serum and cerebrospinal fluid cytokine concentrations in subacute sclerosing panencephalitis. Brain Dev
Tatsuo H, Ono N, Tanaka K, Yanagi Y (2000) SLAM (CDw150) is a cellular receptor for measles virus. Nature 406:893–897
Erlenhoefer C, Wurzer WJ, Löffler S, Schneider-Schaulies S, ter Meulen V, Schneider-Schaulies J (2001) CD150 (SLAM) is a receptor for measles virus, but is not involved in viral contact-mediated proliferation inhibition. J Virol 75:4499–4505
Hsu EC, Iorio C, Sarangi F, Khine AA, Richardson CD (2001) CDw150(SLAM) is a receptor for a lymphotropic strain of measles virus and may account for the immunosuppressive properties of this virus. Virology 279:9–21
Dörig RE, Marcil A, Chopra A, Richardson CD (1993) The human CD46 molecule is a receptor for measles virus (Edmonston strain). Cell 75(2):295–305
Naniche D, Varior-Krishnan G, Cervoni F, Wild TF, Rossi B, Rabourdin-Combe C, Gerlier D (1993) Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J Virol 67(10):6025–6032
Cocks BG, Chang C-CJ, Carballido JM, Yssel H, de Vries JE, Aversa G (1995) A novel receptor involved in T-cell activation. Nature 376:260–263
Minagawa H, Tanaka K, Ono N, Tatsuo H, Yanagi Y (2001) Induction of the measles virus receptor SLAM (CD150) on monocytes. J Gen Virol 82:2913–2917
Ohgimoto S, Ohgimoto K, Niewiesk S, Klagge IM, Pfeuffer J, Johnston ICD, Schneider-Schaulies J, Weidmann A, ter Meulen V, Schneider-Schaulies S (2001) The hemagglutinin protein is an important determinant for measles virus tropism for dendritic cells in vitro and immunosuppression in vivo. J Gen Virol 82:1835–1844
Ogata A, Czub S, Ogata S, Cosby SL, McQuaid S, Budka H, ter Meulen V, Schneider-Schaulies J (1997) Absence of measles virus receptor (CD46) in lesions of subacute sclerosing panencephalitis brains. Acta Neuropathol 94(5):444–449
Takeda M, Tahara M, Hashiguchi T, Sato TA, Jinnouchi F, Ueki S, Ohno S, Yanagi Y (2007) A human lung carcinoma cell line supports efficient measles virus growth and syncytium formation via a SLAM- and CD46-independent mechanism. J Virol 81(21):12091–12096
Leonard VH, Sinn PL, Hodge G, Miest T, Devaux P, Oezguen N, Braun W, McCray PB, McChesney MB, Cattaneo R (2008) Measles virus blind to its epithelial cell receptor remains virulent in rhesus monkeys but cannot cross the airway epithelium and is not shed. J Clin Invest 118:2448–2458
Tahara M, Takeda M, Shirogane Y, Hashiguchi T, Ohno S, Yanagi Y (2008) Measles virus infects both polarized epithelial and immune cells by using distinctive receptor-binding sites on its hemagglutinin. J Virol 82(9):4630–4637
Cattaneo R, Schmid A, Billeter MA, Sheppard RD, Udem SA (1988) Multiple viral mutations rather than host factors cause defective measles virus gene expression in a subacute sclerosing panencephalitis cell line. J Virol 62:1388–1397
Baczko K, Liebert UG, Billeter MA, Cattaneo R, Budka H, ter Meulen V (1986) Expression of defective measles virus genes in brain tissues of patients with subacute sclerosing panencephalitis. J Virol 59:472–478
Cattaneo R, Schmid A, Eschle D, Baczko K, ter Meulen V, Billeter MA (1988) Biased hypermutation and other genetic changes in defective measles viruses in human brain infections. Cell 55:255–265
Reuter T, Weissbrich B, Schneider-Schaulies S, Schneider-Schaulies J (2006) RNA interference with measles virus N-, P-, and L-mRNAs efficiently prevents, and with matrix protein-mRNA enhances viral transcription. J Virol 80:5951–5957
Meissner NN, Koschel K (1995) Downregulation of endothelin receptor mRNA synthesis in C6 rat astrocytoma cells by persistent measles virus and canine distemper virus infections. J Virol 69(8):5191–5194
Urbanska EM, Chambers BJ, Ljunggren HG, Norrby E, Kristensson K (1997) Spread of measles virus through axonal pathways into limbic structures in the brain of TAP -/- mice. J Med Virol 52:362–369
Lawrence DMP, Patterson CE, Gales TL, D’Orazio JL, Vaughn MM, Rall GF (2000) Measles virus spread between neurons requires cell contact but not CD46 expression, syncytium formation, or extracellular virus production. J Virol 74:1908–1918
Duprex WP, McQuaid S, Hangartner L, Billeter MA, Rima BK (1999) Observation of measles virus cell-to-cell spread in astrocytoma cells by using a green fluorescent protein-expressing recombinant virus. J Virol 73:9568–9575
Shingai M, Ayata M, Ishida H, Matsunaga I, Katayama Y, Seya T, Tatsuo H, Yanagi Y, Ogura H (2003) Receptor use by vesicular stomatitis virus pseudotypes with glycoproteins of defective variants of measles virus isolated from brains of patients with subacute sclerosing panencephalitis. J Gen Virol 84(Pt 8):2133–2143
Carsillo T, Carsillo M, Traylor Z, Rajala-Schultz P, Popovich P, Niewiesk S, Oglesbee M (2009) Major histocompatibility complex haplotype determines hsp70-dependent protection against measles virus neurovirulence. J Virol 83(11):5544–5555
Niewiesk S, Brinckmann U, Bankamp B, Sirak S, Liebert UG, ter Meulen V (1993) Susceptibility to measles virus-induced encephalitis in mice correlates with impaired antigen presentation to cytotoxic T lymphocytes. J Virol 67:75–81
Neumeister C, Niewiesk S (1998) Recognition of measles virus-infected cells by CD8+ T cells depends on the H-2 molecule. J Gen Virol 79:2583–2591
Finke D, Liebert UG (1994) CD4+ T cells are essential in overcoming experimental murine measles encephalitis. Immunology 83:184–189
de Vries RD, Yuksel S, Osterhaus AD, de Swart RL (2009) Specific CD8(+) T-lymphocytes control dissemination of measles virus. Eur J Immunol
Weidinger G, Henning G, ter Meulen V, Niewiesk S (2001) Inhibition of major histocompatibility complex class II-dependent antigen presentation by neutralization of gamma interferon leads to breakdown of resistance against measles-induced encephalitis in mice. J Virol 75:3059–3065
Weidinger G, Czub S, Neumeister C, Harriott P, ter Meulen V, Niewiesk S (2000) Role of CD4+ and CD8+ T cells in the prevention of measles virus-induced encephalitis in mice. J Gen Virol 81:2707–2713
Carsillo T, Carsillo M, Niewiesk S, Vasconcelos D, Oglesbee M (2004) Hyperthermic pre-conditioning promotes measles virus clearance from brain in a mouse model of persistent infection. Brain Res 1004:73–82
Cathomen T, Mrkic B, Spehner D, Drillien R, Naef R, Pavlovic J, Aguzzi A, Billeter MA, Cattaneo R (1998) A matrix-less measles virus is infectious and elicits extensive cell fusion: consequences for propagation in the brain. EMBO J 17:3899–3908
Ehrengruber M, Ehler E, Billeter M, Naim HY (2002) Measles virus spreads in rat hippocampal neurons by cell-to-cell contact and in a polarized fashion. J Virol 76:5720–5728
Duprex WP, Duffy I, McQuaid S, Hamill L, Schneider-Schaulies J, Cosby L, Billeter M, ter Meulen V, Rima B (1999) The H gene of rodent brain-adapted measles virus confers neurovirulence to the Edmonston vaccine strain. J Virol 73:6916–6922
Ludlow M, Duprex WP, Cosby SL, Allen IV, McQuaid S (2008) Advantages of using recombinant measles viruses expressing a fluorescent reporter gene with vibratome slice technology in experimental measles neuropathogenesis. Neuropathol Appl Neurobiol 34(4):424–434
Moeller K, Duffy I, Duprex P, Rima B, Beschorner R, Fauser S, Meyermann R, Niewiesk S, ter Meulen V, Schneider-Schaulies J (2001) Recombinant measles viruses expressing altered hemagglutinin (H) genes: functional separation of mutations determining H antibody escape from neurovirulence. J Virol 75:7612–7620
Moeller-Ehrlich K, Ludlow M, Beschorner R, Meyermann R, Rima BK, Duprex WP, Niewiesk S, Schneider-Schaulies J (2007) Two functionally linked amino acids in the stem 2 region of measles virus haemagglutinin determine infectivity and virulence in the rodent central nervous system. J Gen Virol 88:3112–3120
Bonami F, Rudd PA, von Messling V (2007) Disease duration determines canine distemper virus neurovirulence. J Virol 81(21):12066–12070
Schubert S, Möller-Ehrlich K, Singethan K, Wiese S, Duprex WP, Rima BK, Niewiesk S, Schneider-Schaulies J (2006) A mouse model of persistent brain infection with recombinant measles virus. J Gen Virol 87:2011–2019
Rall GF, Manchester M, Daniels LR, Callahan EM, Belman AR, Oldstone MB (1997) A transgenic mouse model for measles virus infection of the brain. Proc Natl Acad Sci USA 94(9):4659–4663
Lawrence DM, Vaughn MM, Belman AR, Cole JS, Rall GF (1999) Immune response-mediated protection of adult but not neonatal mice from neuron-restricted measles virus infection and central nervous system disease. J Virol 73(3):1795–1801
Oldstone MBA, Lewicki H, Thomas D, Tishon A, Dales S, Patterson J, Manchester M, Homann D, Naniche D, Holz A (1999) Measles virus infection in a transgenic model: virus-induced immunosuppresion and central nervous system disease. Cell 98:629–640
Evlashev A, Moyse E, Valentin H, Azocar O, Trescol-Biemont M-C, Marie JC, Rabourdin-Combe C, Horvat B (2000) Productive measles virus brain infection and apoptosis in CD46 transgenic mice. J Virol 74:1373–1382
Horvat B, Rivailler P, Varior-Krishnan G, Cardoso A, Gerlier D, Rarourdin-Combe C (1996) Transgenic mice expressing human measles virus (MV) receptor CD46 provide cells exhibiting different permissivities to MV infections. J Virol 70(10):6673–6681
Niewiesk S, Schneider-Schaulies J, Ohnimus H, Jassoy C, Schneider-Schaulies S, Diamond L, Logan JS, ter Meulen V (1997) CD46 expression does not overcome the intracellular block of measles virus replication in transgenic rats. J Virol 71(10):7969–7973
Mrkic B, Pavlovic J, Rulicke T, Volpe P, Buchholz CJ, Hourcade D, Atkinson JP, Aguzzi A, Cattaneo R (1998) Measles virus spread and pathogenesis in genetically modified mice. J Virol 72(9):7420–7427
Makhortova NR, Askovich P, Patterson CE, Gechman LA, Gerard NP, Rall GF (2007) Neurokinin-1 enables measles virus trans-synaptic spread in neurons. Virology 362(1):235–244
Sellin CI, Davoust N, Guillaume V, Baas D, Belin MF, Buckland R, Wild TF, Horvat B (2006) High pathogenicity of wild-type measles virus infection in CD150 (SLAM) transgenic mice. J Virol 80(13):6420–6429
Sellin CI, Jegou JF, Renneson J, Druelle J, Wild TF, Marie JC, Horvat B (2009) Interplay between virus-specific effector response and Foxp3 regulatory T cells in measles virus immunopathogenesis. PLoS One 4(3):e4948
Manchester M, Eto DS, Oldstone MBA (1999) Characterization of the inflammatory response during acute measles encephalitis in NSE-CD46 transgenic mice. J Neuroimmunol 96:207–217
Patterson CE, Daley JK, Echols LA, Lane TE, Rall GF (2003) Measles virus infection induces chemokine synthesis by neurons. J Immunol 171:3102–3109
Tishon A, Lewicki H, Andaya A, McGavern D, Martin L, Oldstone MB (2006) CD4 T cell control primary measles virus infection of the CNS: regulation is dependent on combined activity with either CD8 T cells or with B cells: CD4, CD8 or B cells alone are ineffective. Virology 347(1):234–245
Shingai M, Inoue N, Okuno T, Okabe M, Akazawa T, Miyamoto Y, Ayata M, Honda K, Kurita-Taniguchi M, Matsumoto M, Ogura H, Taniguchi T, Seya T (2005) Wild-type measles virus infection in human CD46/CD150-transgenic mice: CD11c-positive dendritic cells establish systemic viral infection. J Immunol 175:3252–3261
Welstead GG, Iorio C, Draker R, Bayani J, Squire J, Vonpunsawad S, Cattaneo R, Richardson CD (2005) Measles virus replication in lymphatic cells and organs of CD150 (SLAM) transgenic mice. Proc Natl Acad Sci USA 102:16415–16420
Hahm B, Cho JH, Oldstone MB (2007) Measles virus-dendritic cell interaction via SLAM inhibits innate immunity: selective signaling through TLR4 but not other TLRs mediates suppression of IL-12 synthesis. Virology 358(2):251–257
Johnson KP, Byington DP, Gaddis L (1977) Virological and immunological studies in experimental SSPE. Neurol Neurocir Psiquiatr 18(2–3 Suppl):495–507
Oldstone MBA, Dales S, Tishon A, Lewicki H, Martin L (2005) A role for dual hits in causation of subacute sclerosing panencephalitis. J Exp Med 202:1185–1190
Drillien R, Spehner D, Kirn A, Giraudon P, Buckland R, Wild F, Lecocq J-P (1988) Protection of mice from fatal measles encephalitis by vaccination with vaccinia virus recombinants encoding either the hemagglutinin or the fusion protein. Proc Natl Acad Sci 85:1252–1256
Fournier P, Brons NH, Berbers GA, Wiesmuller KH, Fleckenstein BT, Schneider F, Jung G, Muller CP (1997) Antibodies to a new linear site at the topographical or functional interface between the haemagglutinin and fusion proteins protect against measles encephalitis. J Gen Virol 78:1295–1302
Partidos CD, Ripley J, Delmas A, Obeid OE, Denbury A, Steward MW (1997) Fine specificity of the antibody response to a synthetic peptide from the fusion protein and protection against measles virus-induced encephalitis in a mouse model. J Gen Virol 78:3227–3232
Rammohan KW, McFarland HF, McFarlin DE (1981) Induction of subacute murine measles encephalitis by monoclonal antibody to virus haemagglutinin. Nature 290:588–589
Garg RK (2002) Subacute sclerosing panencephalitis. Postgrad Med J 78(916):63–70
Huffman JH, Sidwell RW, Khare GP, Witkowski JT, Allen LB, Robins RK (1973) In vitro effect of 1-beta-D-ribofuranosyl-1, 2, 4-triazole-3-carboxamide (virazole, ICN 1229) on deoxyribonucleic acid and ribonucleic acid viruses. Antimicrob Agents Chemother 3(2):235–241
Honda Y, Hosoya M, Ishii T, Shigeta S, Suzuki H (1994) Effect of ribavirin on subacute sclerosing panencephalitis virus infections in hamsters. Antimicrob Agents Chemother 38(4):653–655
Ishii T, Hosoya M, Mori S, Shigeta S, Suzuki H (1996) Effective ribavirin concentration in hamster brains for antiviral chemotherapy for subacute sclerosing panencephalitis. Antimicrob Agents Chemother 40(1):241–243
Grancher N, Venard V, Kedzierewicz F, Ammerlaan W, Finance C, Muller CP, Le Faou A (2004) Improved antiviral activity in vitro of ribavirin against measles virus after complexation with cyclodextrins. Antiviral Res 62(3):135–137
Jeulin H, Grancher N, Kedzierewicz F, Finance C, Le Faou AE, Venard V (2008) In vivo antiviral activity of ribavirin/alpha-cyclodextrin complex: evaluation on experimental measles virus encephalitis in mice. Int J Pharm 357(1–2):148–153
Jeulin H, Venard V, Carapito D, Finance C, Kedzierewicz F (2009) Effective ribavirin concentration in mice brain using cyclodextrin as a drug carrier: evaluation in a measles encephalitis model. Antiviral Res 81(3):261–266
Statement JWU (1987) Vitamin A for measles. Lancet 1(8541):1067–1068
D’Souza RM, D’Souza R (2002) Vitamin A for preventing secondary infections in children with measles–a systematic review. J Trop Pediatr 48(2):72–77
Huiming Y, Chaomin W, Meng M (2005) Vitamin A for treating measles in children. Cochrane Database Syst Rev (4): CD001479
Mora JR, Iwata M, von Andrian UH (2008) Vitamin effects on the immune system: vitamins A and D take centre stage. Nat Rev Immunol
Trottier C, Chabot S, Mann KK, Colombo M, Chatterjee A, Miller WH Jr, Ward BJ (2008) Retinoids inhibit measles virus in vitro via nuclear retinoid receptor signaling pathways. Antiviral Res 80(1):45–53
Trottier C, Colombo M, Mann KK, Miller WH Jr, Ward BJ (2009) Retinoids inhibit measles virus through a type I IFN-dependent bystander effect. Faseb J 23(9):3203–3212
Rodeheffer C, von Messling V, Milot S, Lepine F, Manges AR, Ward BJ (2007) Disease manifestations of canine distemper virus infection in ferrets are modulated by vitamin A status. J Nutr 137(8):1916–1922
Gungor S, Olmez A, Pinar Arikan F, Haliloglu G, Anlar B (2007) Serum retinol and beta-carotene levels in subacute sclerosing panencephalitis. J Child Neurol 22(3):341–343
Andersson T, Schultzberg M, Schwarz R, Löve A, Wickman C, Kristensson K (1991) NMDA-receptor antagonist prevents measles virus-induced neurodegeneration. Eur J Neurosci 3:66–71
Otaki M, Sada K, Kadoya H, Nagano-Fujii M, Hotta H (2006) Inhibition of measles virus and subacute sclerosing panencephalitis virus by RNA interference. Antiviral Res 70(3):105–111
Keita D, Servan de Almeida R, Libeau G, Albina E (2008) Identification and mapping of a region on the mRNA of Morbillivirus nucleoprotein susceptible to RNA interference. Antiviral Res 80(2):158–167
Suryanarayana K, Baczko K, ter Meulen V, Wagner RR (1994) Transcription inhibition and other properties of matrix proteins expressed by M genes cloned from measles viruses and diseased human brain tissue. J Virol 68:1532–1543
Zinke M, Kendl S, Singethan K, Fehrholz M, Reuter D, Rennick L, Herold MJ, Schneider-Schaulies J (2009) Clearance of measles virus from persistently infected cells by short hairpin RNA. J Virol 83(18):9423–9431
Plemper RK, Erlandson KJ, Lakdawala AS, Sun A, Prussia A, Boonsombat J, Aki-Sener E, Yalcin I, Yildiz I, Temiz-Arpaci O, Tekiner B, Liotta DC, Snyder JP, Compans RW (2004) A target site for template-based design of measles virus entry inhibitors. Proc Natl Acad Sci USA 101(15):5628–5633
Plemper RK, Doyle J, Sun A, Prussia A, Cheng LT, Rota PA, Liotta DC, Snyder JP, Compans RW (2005) Design of a small-molecule entry inhibitor with activity against primary measles virus strains. Antimicrob Agents Chemother 49(9):3755–3761
Sun A, Prussia A, Zhan W, Murray EE, Doyle J, Cheng LT, Yoon JJ, Radchenko EV, Palyulin VA, Compans RW, Liotta DC, Plemper RK, Snyder JP (2006) Nonpeptide inhibitors of measles virus entry. J Med Chem 49(17):5080–5092
Sun A, Chandrakumar N, Yoon JJ, Plemper RK, Snyder JP (2007) Non-nucleoside inhibitors of the measles virus RNA-dependent RNA polymerase complex activity: synthesis and in vitro evaluation. Bioorg Med Chem Lett 17(18):5199–5203
White LK, Yoon JJ, Lee JK, Sun A, Du Y, Fu H, Snyder JP, Plemper RK (2007) Nonnucleoside inhibitor of measles virus RNA-dependent RNA polymerase complex activity. Antimicrob Agents Chemother 51(7):2293–2303
Sun A, Yoon JJ, Yin Y, Prussia A, Yang Y, Min J, Plemper RK, Snyder JP (2008) Potent non-nucleoside inhibitors of the measles virus RNA-dependent RNA polymerase complex. J Med Chem 51(13):3731–3741
Yoon JJ, Krumm SA, Ndungu JM, Hoffman V, Bankamp B, Rota PA, Sun A, Snyder JP, Plemper RK (2009) Target analysis of the experimental measles therapeutic AS-136A. Antimicrob Agents Chemother 53(9):3860–3870
Acknowledgments
Work of the authors was supported by the Deutsche Forschungsgemeinschaft through Sonderforschungsbereich 479.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of a Special Issue on Pathogen Variation and Host Response in Infectious Disease.
Rights and permissions
About this article
Cite this article
Reuter, D., Schneider-Schaulies, J. Measles virus infection of the CNS: human disease, animal models, and approaches to therapy. Med Microbiol Immunol 199, 261–271 (2010). https://doi.org/10.1007/s00430-010-0153-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-010-0153-2