Abstract
We try to find the association of cytomegalovirus (CMV) infection and anti-β2 glycoprotein 1 autoantibodies (anti-β2 GP1), a key antibody in antiphospholipid syndrome (APS), among systemic lupus erythematosus (SLE) and cerebral vascular accident (CVA) patients. This retrospective study enrolled serum samples obtained from 87 SLE and 97 CVA patients who have been checked for the existence of anti-β2 GP1. First, the prevalence rate of anti-CMV IgG and IgM in patients with and without anti-β2 GP1 were compared. Second, the prevalence of anti-CMV IgG and IgM were compared between SLE and CVA patients. Last, this study analyzed the clinical characteristics and disease activity in SLE patients with positive anti-CMV IgM and IgG. No difference existed in the prevalence rate of anti-CMV IgG and IgM between positive or negative anti-β2 GP1 serum samples in both SLE and CVA patients. However, the prevalence of anti-CMV IgM was significantly higher in the SLE group than in the CVA group. Severity of clinical features and SLEDAI scores were considerably higher in patients with positive anti-CMV IgM than in SLE patients with negative anti-CMV IgM. Very impressively, all IgM-positive SLE samples (9/9) carrying highest levels of anti-CMV IgG, indicated reactivation of the latent CMV infection. Hence, it suggests that CMV reactivation might contribute toward the disease flare in some SLE patients. In future, a prospective and longitudinal study is stongly indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiphospholipid syndrome (APS) has been recognized as a major catastrophic manifestation of systemic lupus erythematosus (SLE) [1]. APS is characterized by antibodies directed against either phospholipids or plasma proteins bound to anionic phospholipids, combined with various clinical manifestations including venous and arterial thrombosis, recurrent fetal loss, and neurological events. This disorder is considered primary APS when it occurs alone, such as cerebral vascular accident (CVA), and secondary APS when in association with SLE or other rheumatic or autoimmune disorders.
One autoantibody contributing to APS is anti-β2 glycoprotein 1 autoantibodies (anti-β2 GP1) [2]. The factors causing production of anti-β2 GP1 remain unclear, however, an association with infectious agents, such as cytomegalovirus (CMV) and EBV infection, has been described in sporadic cases [3–7].
This study attempted to determine whether CMV infection is associated with anti-β2 GP1, one of the principal antibodies in APS, and whether CMV infection or reactivation affect clinical severity and disease activity in SLE patients.
Materials and methods
Patients and controls
All 184 serum samples from SLE and CVA patients were collected between June 1, 2005, and March 31, 2006. These samples were assigned to a SLE group or a CVA group based on patient diagnosis (Table 1). Clinical diagnosis and disease severity were accessed via a review of medical records.
SLE group
Twenty-four serum samples from 24 adult SLE patients positive for anti-β2 GP1 were enrolled. All 24 patients were diagnosed with SLE and fulfilled the 1997 revised classification criteria of the American College of Rheumatology [8]. Of these 24 patients, 22 were female and 2 were male. Sixty-three serum samples from 63 SLE patients negative for anti-β2 GP1 were enrolled as controls. Of these control patients, 56 were female and 8 were male. Mean ages of the SLE and control groups were 33.3 ± 11.67 years and 30.8 ± 11.95 years, respectively (P = 0.47) (Table 1).
CVA group
In the CVA group, all patients, including those who were positive and negative for anti-β2 GP1, were diagnosed by a neurologist as cases of recent cerebral vascular infarction in the last 1 year. Eighteen serum samples from 18 patients positive for anti-β2 GP1, including 9 serum samples from male patients and 9 serum samples from female patients were analyzed. Seventy-nine serum samples from 79 patients negative for anti-β2 GP1 were enrolled as controls. The mean age in the SLE and CVA groups were 31.3 ± 11.49 years and 52.5 ± 18.03 years, respectively (P = 0.001) (Table 1). All patients were Chinese.
Serum anti-β2 glycoprotein 1 antibodies
Presence of anti-β2 GP1 was determined using a Varelisa enzyme immunoassay commercial kit. The positive and negative controls tests were included following the manufacturer’s instructions (Pharmacia Diagnostics, Denville, NJ, USA). The titer of anti-β2 GP1 at ≥15 U/ml was considered positive, ≤10 U/ml was considered as negative result. The titer of anti-β2 GP1 between 10 and 15 U/ml was regarded as an equivocal result and considered as negative results in our study.
Serum anti-CMV antibodies
The presence of immunoglobulin G (IgG) and immunoglobulin M (IgM) antibodies against CMV were determined using a microparticle enzyme immunoassay (MEIA) approach. Positive and negative control tests were included following the manufacturer’s instructions (Abbott Laboratories, Abbott Park, IL, USA). The titer of IgG antibody against CMV at ≥15 U/ml was considered positive, indicating exposure to CMV infection, including past or current CMV infections. The titer of anti-CMV IgG antibody at ≤10 U/ml was considered negative. The titer of anti-CMV IgG between 10 and 15 U/ml was regarded as an equivocal result and considered negative in our study.
The titer of serum CMV IgM indexes at 0.5 or greater was regarded as positive. All serum samples giving CMV IgM indexes ≥0.5 were treated with the rheumatoid factor (RF) neutralization reagent and retested according to the manufacturer’s instructions (Abbott Laboratories, Abbott Park, IL, USA). Equivocal results (anti-CMV IgM index of 0.500–0.599) were regarded as negative. Positive anti-CMV IgM indicates a recent infection, including primary infection, reactivation or re-infection of CMV.
Rheumatoid factor neutralization
The RF neutralization method was applied to avoid false-positive results for anti-CMV IgM following the manufacturer’s instructions (Abbott Laboratories, Abbott Park, IL, USA). All serum samples with positive for anti-CMV IgM were tested. Following neutralization, anti-CMV IgM index of ≥0.6 was considered positive. Equivocal results (after RF neutralization anti-CMV IgM index of 0.500–0.599) were considered negative or a false-positive result for anti-CMV IgM.
Viral replication
In patients who showed IgM reactivity to CMV, viral DNA was detected by real-time polymerase chain reaction (real-time PCR, Roche LightCycler System) in order to establish the presence or absence of systemic viral replication. Real-time PCR for CMV-DNA was carried out in serum samples with primers located within the glycoprotein B genome region.
SLE Disease Activity Index
SLE Disease Activity Index (SLEDAI) scoring: disease activity was scored according to SLEDAI-2K [9].
Statistical analysis
The Student’s t test was applied to examine the mean difference of SLEDAI scores among different SLE subgroups. The Chi-square test was utilized to test for significant differences between categorical variables. Fisher’s exact test was applied to assess the difference in frequency for categorical variables with a limited numbers of samples. A value of P ≤ 0.05 was regarded as a statistically significant difference.
The first study compared the prevalence rate of anti-CMV IgG and IgM between patients with positive and negative anti-β2 GP1. The second study compared the prevalence rate of anti-CMV IgG and IgM between patients with SLE and CVA. Finally, this study compared clinical characteristics and disease activity (determined by SLEDAI score) in cases of positive anti-CMV IgM and IgG patients in SLE patients.
Results
Before and after RF neutralization for anti-CMV IgM
Before RF neutralization, 16 serum samples were positive for anti-CMV IgM. Among these 16 samples, 12 samples were from the SLE group and 4 were from the CVA group. After RF neutralization, 3 samples in each group were false-positive for anti-CMV IgM, leaving 9 true-positive anti-CMV IgM samples in the SLE group and 1 true-positive anti-CMV IgM sample in the CVA group.
CMV infection and anti-β2 GP1
Anti-β2 GP1 and CMV infection in SLE group
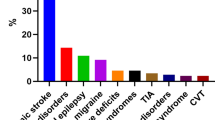
The prevalence of positive anti-CMV IgG in SLE group was 97.7% (85/87). The prevalence of positive anti-CMV IgM in SLE group was 10.34% (9/87). No statistic difference existed for presence of anti-CMV IgG (P = 0.119) or IgM (P = 0.243) between the positive anti-β2 GP1 and negative anti-β2 GP1 in SLE groups (Figs. 1, 2).
The anti-CMV IgG titer distributions of four subgroups are shown. Similar distribution patterns between positive and negative anti-β2 glycoprotein 1 (anti-β2 GP1) groups. The anti-CMV IgG titer distributions of SLE group and CVA group are shown separately; comparing left two columns to right two columns. All except three patients in the SLE group were positive for anti-CMV IgG
The anti-CMV IgM titer distributions (post rheumatoid factor neutralization) of four subgroups are shown. False-positive of anti-CMV IgM was confirmed by rheumatoid factor neutralization. SLE patients with negative anti-β2 glycoprotein 1 (anti-β2 GP1) have higher positive anti-CMV. IgM titers indicates no correlation between CMV infection/activation and anti-β2 GP1 formation. The anti-CMV IgM titer distributions (post rheumatoid factor neutralization) of SLE group and CVA group are shown; comparing left two columns to right two columns
Anti-β2 GP1 and CMV infection in CVA group
The prevalence of positive anti-CMV IgG in the CVA group was 100% (97/97). The prevalence of positive anti-CMV IgM was 1.03% (1/97). All patients including those positive and negative for anti-β2 GP1 were positive for anti-CMV IgG (Fig. 1). No statistical difference existed for positive anti-CMV IgM between the positive anti-β2 GP1 and negative anti-β2 GP1 in the CVA group (Fisher’s exact test, P = 0.186) (Fig. 2).
Comparison of CMV infection between CVA and SLE groups
The prevalence of positive anti-CMV IgM in SLE group is significantly higher than in the CVA group (10.34 vs. 1.03%, P < 0.001) (Fig. 2). The prevalence of anti-CMV IgG was not statistically different between the CVA and SLE groups (100 vs. 96.55%, P = 0.067) (Fig. 1).
In anti-CMV IgM(+) patients (n = 10, 9 SLE patients and 1 CVA patient), testing for viral replication in serum samples showed negative.
Clinical characteristics of SLE patients with positive anti-CMV IgM and IgG
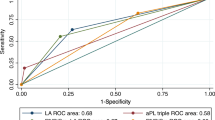
The clinical manifestation of all SLE patients was reviewed. Additionally, we compared SLEDAI scores for anti-CMV IgM(+)/IgG(+) patients, and anti-CMV IgM(-)/IgG(+) patients. The disease activity indicated by SLEDAI score is significantly higher in patients positive for both anti-CMV IgM and IgG than in patients negative for anti-CMV IgM but positive anti-CMV IgG (Fig. 3). The clinical symptoms of nine anti-CMV IgM(+)/IgG(+) SLE patients are shown in Table 2.
Discussion
Initially, we tried to study whether CMV infection was related to anti-β2 GP1 formation or not. However, there was no association found in neither SLE group nor CVA group. Although, it looks that both SLE and CVA patients without anti-β2 GP1 autoantibodies showed higher anti-CMV IgG and IgM values than those with anti-β2 GP1 autoantibodies, there was no statistic significance (P > 0.1). To our surprise, we found the association between CMV and SLE.
The role of CMV upon SLE has been discussed before. Previously, several sporadic cases of CMV colitis, retinitis or hemophagocytosis syndrome have been described in SLE patients. Moreover, it has been reported that CMV infection might trigger the onset of SLE, a systemic autoimmune disease [10, 11]. Therefore, it suggested that CMV-related autoimmune response is an important issue to be studied. However, whether CMV reactivation can cause disease flare of SLE has not been studied thoroughly.
In this study, incidentally, a higher prevalence of anti-CMV IgM in the SLE group compared to the CVA group was noted (10.34 vs. 1.03%, P < 0.001). To our surprise, the disease activity defined by SLEDAI scores differed significantly between those SLE patients with and without anti-CMV IgM (11.44 ± 6.77 vs. 3.87 ± 3.36, P = 0.012) (Fig. 3).
Very impressively, all IgM-positive SLE samples (9/9) were carrying highest levels of anti-CMV IgG (all ≧ 250 U/ml). High CMV IgG values in those cases presenting positive IgM test results and the absence of positive CMV PCRs might support reactivation and are more inconsistent with primary CMV infection. As CMV is an intracellular pathogen and it may establish latency in humans, it can reactivate in patients with suppressed immune system [12]. All nine cases with CMV reactivation are under treatment with steroid or other immunosuppressives, which may contribute toward the reactivation of CMV as described by Yoda et al. [13].
Previously, it has been described that CMV infection might trigger the onset of SLE or exacerbation of pre-existing SLE [10, 11]; however the evidence is not strong enough. In 2002, Stratta and Colla have described a SLE patient with frequent disease flare, with unknown trigger factors. This patient developed lupus nephritis, hemolytic uremic syndrome with thrombotic microangiopathy and life threatening infections for 3 years until CMV replication was confirmed and treated with ganciclovir. Thereafter, the clinical and biochemical conditions of the patient improved and remained stable after the two prolonged courses of ganciclovir [14]. It supports that CMV reactivation might play a role in some SLE patients with disease flare.
Although the timely association between CMV reactivation and SLE flare-up is still unclear, several possibilities have been proposed. The first possibility is that SLE itself can result in CMV reactivation. However, there is no evidence to support this to date. The second possibility is that there may be some other unknown etiologies that trigger both CMV reactivation and SLE disease flare simultaneously. A few articles discussed the immune pathogenesis of reactivation of CMV in immunocompromised patients [15, 16]; gender seems not to affect the prevalence of seropositivity, rather an older age was associated with CMV seropositivity in one study [17]. The evidence of the second possibility is still not clear. The third possibility is that CMV reactivation may cause increased production of autoantibodies with subsequent disease flare up. The last hypothesis seems to be the most promising, because CMV infection has an association with SLE [18], exacerbates SLE [19], and also has been found to be able to induce the expression of autoantigen, Ro/SS-A on keratinocyte and calreticulin in fibroblast [20, 21]. Furthermore, it is considered that the immunosupression due to the use of steroid or cytotoxics in SLE patients might contribute toward the reactivation of CMV in some cases with particular susceptibility [22–25] and vice-versa [26], which might result in a vicious cycle to worsen SLE. To block the vicious cycle, identifying high risk patients, screening CMV seropositivity, and doing baseline CMV PCR/antigen assay were recommended by Yoon et al. [25].
Limitation of this preliminary study is that this is a retrospective case-controlled study with a limited number of samples. However, a strong association between anti-CMV IgM and SLE disease activity implies that seroconversion of anti-CMV IgM might not be a mere non-specific reaction [27], but could be a sign of disease flare in some SLE patients. Seropositivity of anti-CMV IgM could be an additional marker of SLE progress and this is worth further investigation.
References
Ruiz-Irastorza G, Khamashta MA, Castellino G, Hughes GR (2001) Systemic lupus erythematosus. Lancet 357:1027–1032
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, Derksen RH, DE Groot PG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A, Vlachoyiannopoulos PG, Krilis SA (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306
Gharavi AE, Pierangeli SS, Harris EN (2003) Viral origin of antiphospholipid antibodies: endothelial cell activation and thrombus enhancement by CMV peptide-induced APL antibodies. Immunobiology 207:37–42
Blank M, Shoenfeld Y (2004) Beta-2-glycoprotein-I, infections, antiphospholipid syndrome and therapeutic considerations. Clin Immunol 112:190–199
Blank M, Asherson RA, Cervera R, Shoenfeld Y (2004) Antiphospholipid syndrome infectious origin. J Clin Immunol 24:12–23
Bakimer R, Blank M, Kosashvilli D, Ichikawa K, Khamashta MA, Hughes GR, Koike T, Shoenfeld Y (1995) Antiphospholipid syndrome and the idiotypic network. Lupus 4:204–208
Ngou J, Graafland H, Segondy M (1992) Antibodies against polypeptides of purified Epstein-Barr virus in sera from patients with connective tissue diseases. J Autoimmun 5:243–249
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Gladman DD, Ibanez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29:288–291
Nawata M, Seta N, Yamada M, Sekigawa I, Lida N, Hashimoto H (2001) Possible triggering effect of cytomegalovirus infection on systemic lupus erythematosus. Scand J Rheumatol 30:360–362
Sekigawa I, Nawata M, Seta N, Yamada M, Iida N, Hashimoto H (2002) Cytomegalovirus infection in patients with systemic lupus erythematosus. Clin Exp Rheumatol 20:559–564
Bruggeman CA (1993) Cytomegalovirus and latency: an overview. Virchows Arch B Cell Pathol Incl Mol Pathol 64:325–333
Yoda Y, Hanaoka R, Ide H, Isozaki T, Matsunawa M, Yajima N, Shiozawa F, Miwa Y, Negishi M, Kasama T (2006) Clinical evaluation of patients with inflammatory connective tissue diseases complicated by cytomegalovirus antigenemia. Mod Rheumatol 16:137–142
Stratta P, Colla L, Santi S, Grill A, Besso L, Godio L, Davico-Bonino L, Mazzucco G, Ghisetti V, Barbui A, Canavese C (2002) IgM antibodies against cytomegalovirus in SLE nephritis: viral infection or aspecific autoantibody? J Nephrol 15:88–92
Tardy JC, Bosshard S, Aymard M (1985) [Immunologic markers of the risk of cytomegalovirus infection among immunosuppressed patients]. Rev Epidemiol Sante Publique 33:297–303
Temcharoen S, Hirsch P, Theamboonlers A, Likitnukul S, Seksarn P, Poovorawan Y (1999) Cytomegalovirus infection in immunocompromised children in Thailand. Asian Pac J Allergy Immunol 17:295–299
Stratta P, Canavese C, Ciccone G, Santi S, Quaglia M, Ghisetti V, Marchiaro G, Barbui A, Fop F, Cavallo R, Piccoli G (1999) Correlation between cytomegalovirus infection and Raynaud’s phenomenon in lupus nephritis. Nephron 82:145–154
Hrycek A, Kusmierz D, Mazurek U, Wilczok T (2005) Human cytomegalovirus in patients with systemic lupus erythematosus. Autoimmunity 38:487–491
Hayashi T, Lee S, Ogasawara H, Sekigawa I, Iida N, Tomino Y, Hashimoto H, Hirose S (1998) Exacerbation of systemic lupus erythematosus related to cytomegalovirus infection. Lupus 7:561–564
Zhu J, Newkirk MM (1994) Viral induction of the human autoantigen calreticulin. Clin Invest Med 17:196–205
Zhu J (1995) Cytomegalovirus infection induces expression of 60 KD/Ro antigen on human keratinocytes. Lupus 4:396–406
Ikura Y, Matsuo T, Ogami M, Yamazaki S, Okamura M, Yoshikawa J, Ueda M (2000) Cytomegalovirus associated pancreatitis in a patient with systemic lupus erythematosus. J Rheumatol 27:2715–2717
Vilaichone K, Mahachai V, Eiam-Ong S, Kullavanuaya P, Wisedopas N, Bhattarakosol P (2001) Necrotizing ileitis caused by cytomegalovirus in patient with systemic lupus erythematosus: case report. J Med Assoc Thai 84 (Suppl. 1):S469–S473
Sakamoto O, Ando M, Yoshimatsu S, Kohrogi H, Suga M, Ando M (2002) Systemic lupus erythematosus complicated by cytomegalovirus-induced hemophagocytic syndrome and colitis. Intern Med 41:151–155
Yoon KH, Fong KY, Tambyah PA (2002) Fatal cytomegalovirus infection in two patients with systemic lupus erythematosus undergoing intensive immunosuppressive therapy: role for cytomegalovirus vigilance and prophylaxis? J Clin Rheumatol 8:217–222
Scholz M, Doerr HW, Cinatl J (2003) Human cytomegalovirus retinitis: pathogenicity, immune evasion and persistence. Trends Microbiol 11:171–178
Akagi S, Ichikawa H, Suzuki J, Makino H (2004) Systemic lupus erythematosus associated with cytomegalovirus infection. Scand J Rheumatol 33:58–59
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Su, B.YJ., Su, CY., Yu, SF. et al. Incidental discovery of high systemic lupus erythematosus disease activity associated with cytomegalovirus viral activity. Med Microbiol Immunol 196, 165–170 (2007). https://doi.org/10.1007/s00430-007-0040-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-007-0040-7