Abstract
The immune microenvironment plays a pivotal role in cancer development and progression. Therefore, we studied the status of immune cells in esophageal adenocarcinoma (EAC) and adjacent Barrett’s esophagus (BE) and their association with the clinical course of patients. We included 87 patients with EAC who underwent surgical resection or endoscopic submucosal dissection. CD3, CD8, Foxp3, p53, and Ki-67 were immunolocalized in EAC and adjacent BE (N = 87) and BE without EAC (N = 13). BE adjacent to EAC exhibited higher CD3+ lamina propria lymphocyte (LPL) numbers than BE without EAC. Abundant Foxp3+ LPLs in BE were associated with dysplasia and increased Ki-67 labeling index (LI) in BE glandular cells and tended to link to aberrant p53 expression. Abundant CD8+ LPLs in adjacent BE were associated with worse prognosis of EAC patients (P = 0.019). Results of our present study firstly revealed the potential influence of the tissue immune microenvironment of BE adjacent to EAC on cancer development and eventual clinical outcome of EAC patients. T cell infiltration could play pivotal roles in facilitating the dysplasia–adenocarcinoma sequence in BE. The number of Foxp3+ T cells is increased at the early stage of carcinogenesis and could help identify patients harboring dysplastic and highly proliferating cells. CD8+ T cells could reflect unfavorable inflammatory response in adjacent tissue microenvironment and help predict worse prognosis of EAC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Barrett’s esophagus (BE) is characterized by the presence of columnar mucosa in the esophagus and is considered a complication of gastroesophageal reflux disease (GERD) and the precursor of esophageal adenocarcinoma (EAC) [1,2,3]. Recently, the incidence of EAC markedly increased worldwide, especially in developed countries, possibly because of increase in obesity and decrease in Helicobacter pylori infection [4,5,6].
The tumor immune microenvironment including immune cells plays a pivotal role in both cancer development and progression [7]. Regulatory T cells, an immunosuppressive subset of CD4+ T cells characterized by the expression of the master transcription factor forkhead box protein P3 (Foxp3), suppress anticancer immunity, hindering protective immunosurveillance of neoplasia and promoting tumor development and progression [8]. The amounts of Foxp3 mRNA has been reported to be significantly higher in BE than in squamous epithelium [9]. Furthermore, the number of Foxp3+ T cells was reported to be high in BE [10]. However, it remains unclear whether Foxp3+ T cells are associated with Barrett’s carcinogenesis or not [10].
Cytotoxic CD8+ T cells release various effector proteins, including interferon-gamma, perforin, granzyme A, granzyme B, and Fas ligands, and induce apoptosis of target cells. CD8+ T cell infiltration is usually protective as part of the host anti-tumor immune response in many malignancies; however, it can contribute to the aggravation of chronic inflammation, supporting tumor development [11]. The secreted factors in esophagitis tissue have also been reported to enhance CD8+ T cell infiltration [12, 13]. Therefore, CD8+ T cells could be the indicator of inflammatory response in BE adjacent to EAC and could be associated with EAC development and further progression. However, its prognostic impact on patients with EAC has remained unknown. Therefore, in this study, we compared lymphocyte infiltration between BE with EAC and BE without EAC in order to explore the impact of BE microenvironment on cancer development. We also examined the impact of lymphocyte infiltration in EAC and adjacent BE on the survival of patients with EAC.
Materials and methods
Cases
We included 87 patients with EAC who underwent surgical resection or endoscopic submucosal dissection (ESD) at the following hospitals in Japan: Tohoku University Hospital, Hachinohe City Hospital, Nihonkai General Hospital, Hiraka General Hospital, Iwate Prefectural Central Hospital, Osaki Citizen Hospital, Japanese Red Cross Ishinomaki Hospital, and Sendai City Medical Center. Furthermore, BE adjacent to EAC was compared with BE without EAC (N = 13). All these patients were previously untreated.
In this study, BE was defined according to the British Society of Gastroenterology guidelines as a columnar-lined esophagus which is ≥ 1 cm above the esophagogastric junction (EGJ) [2]. The patients in whom BE was not histologically identified adjacent to adenocarcinoma were excluded from this study to exclude carcinoma of the gastric cardia. Overall survival was defined as follows: from the time of the initial pathological diagnosis to the time of death or last census.
Surgically resected specimens
In all surgical specimens examined, the resected tissues were stained with iodine solution to confirm unstained areas and photographed immediately after the surgery. Subsequently, these macroscopic photographs were reviewed to identify EGJ, length of BE, and Siewert type [14]. EGJ was tentatively defined as the point at which the luminal caliber changes and where the tubular esophagus is connected to the vestibule lumen of the stomach [1, 2]. The presence of circular BE extending longitudinally for ≥ 3 cm was defined as long-segment BE (LSBE). Others were defined as short-segment BE (SSBE) [1, 2]. We confirmed BE length histologically by checking whether the columnar epithelium was present in the esophagus based on the presence of at least one of the following conditions: esophageal gland ducts or proper esophageal glands; squamous islands; and a double-layer muscularis mucosae [1, 2].
Endoscopically resected specimens
The length of BE and Siewert type were determined by retrieving the endoscopic reports. In addition, the histopathological diagnoses of BE-related EAC and BE length were also confirmed by reviewing the tissue slides.
The selected portions of BE tissue adjacent to EAC
Figure 1 illustrates the selected sections of EAC-containing tissues and adjacent BE tissues. The selected portions of nonmalignant adjacent BE tissues had at least 3 mm of distance from the tumor cells, in line with previous studies involving patients with prostate cancer [15, 16].
Representation of the anatomy of the tissue sections containing esophageal adenocarcinoma (EAC) and adjacent Barrett’s esophagus (BE) tissues and the methodology of the study. a Gross specimen. b Low magnification of BE. Stromal area was selected (dashed line) and then lamina propria lymphocytes (LPLs) were quantified in × 400 microscopic field. c Low magnification of EAC. Tumor-infiltrating lymphocytes (TILs) were evaluated within the borders of the invasive tumor. The intratumoral and stromal compartments were selected (dashed line) and then quantified in × 400 microscopic field
Immunohistochemistry
Supplemental Table 1 summarizes the details of the primary antibodies, antigen retrieval methods, and buffers used in this study. The tissue specimens fixed in 10% formalin and embedded in paraffin were sectioned at a thickness of 3 μm. In the immunohistochemical study of Foxp3, antigen retrieval was performed by autoclaving the slides (Tomy SX-500 High-Pressure Steam Sterilizer, Tomy Seiko Co., Ltd., Tokyo, Japan) in citrate buffer (pH 6.0) and heating them at 121 °C for 5 min. The slides were then incubated for 30 min at room temperature in a blocking solution containing 1% mouse serum (Nichirei Bioscience, Tokyo, Japan). The dilutions of the primary antibodies employed were 1:200, and antibodies were incubated at 4 °C overnight. A secondary antibody reaction was performed by using a biotinylated anti-mouse antibody (Nichirei Bioscience) for 30 min at room temperature. Peroxidase-conjugated streptavidin (Nichirei Bioscience) was subsequently used for 30 min at room temperature. The antigen–antibody complex was visualized using 3,3′-diaminobenzidine and counterstained with hematoxylin. Moreover, Dako Autostainer Link 48 and EnVision FLEX+ Kit (Dako) were used for immunohistochemical studies of CD3, CD8, and Ki-67, whereas a VENTANA BenchMark ULTRA and the VENTANA OptiView DAB Universal Kit (Ventana Medical Systems, Inc., CA, USA) were used to study p53 immunohistochemistry.
All immunostained slides were independently evaluated by two authors (YG and FF) without prior knowledge of any clinicopathological variables of the patients. The lamina propria lymphocytes (LPLs) of BE were quantified and intraepithelial lymphocytes were excluded (Fig. 1b) [17]. Tumor-infiltrating lymphocytes (TILs) were evaluated within the borders of the invasive tumor. The intratumoral and stromal compartments were selected under light microscopy (Fig. 1c) [18]. The immunopositive lymphocytes were enumerated in × 400 microscopic fields [17,18,19]. Three different fields were analyzed per slide, and the mean number was adopted as a final result [17, 20]. The LPL densities in BE were tentatively classified as high or low group based on their median number of infiltrated lymphocytes [21,22,23,24] (Fig. 2a–c).
Representative illustrations of immunohistochemistry. a–c Lamina propria lymphocytes (LPLs). a High CD3+ LPLs. b High CD8+ LPLs. c High Foxp3+ LPLs. d–f p53. d Distinct nuclear immunoreactivity of p53. e Complete loss of p53 expression. A relatively weak immuno-positivity was detected in the basal region of a few crypts, but nuclear p53 immunoreactivity was not detected in the majority of crypts harboring enlarged nuclei. f p53 normal. g High Ki-67 LI. h High CD8+ TILs
The immunoreactivity of p53 was considered aberrant when at least one BE gland had distinctive nuclear immunoreactivity or a complete loss of immunoreactivity [25,26,27] (Fig. 2d–f). Ki-67 nuclear immunoreactivity was evaluated in 1000 epithelial cells, and a percentage of positive cells of > 20% was tentatively determined as high Ki-67 LI in this study [28, 29] (Fig. 2g).
As LPLs, the TIL densities in EAC were tentatively classified as high or low group based on their median number of infiltrated lymphocytes [21,22,23,24] (Fig. 2h).
Dysplasia
According to the 2019 World Health Organization classification, BE was tentatively classified as with or without low-grade dysplasia and high-grade dysplasia (Supplemental Fig. 1) [30].
Statistical analysis
All the statistical analyses were performed using JMP Pro version 13 with Kruskal–Wallis test, Student’s t test, Cochran–Armitage trend test, and Fisher’s exact test. In addition, the Kaplan–Meier test was employed to estimate the survival curves. P values of < 0.05 were considered statistically significant in this study.
Results
Relationship between LPL status and presence of EAC
Clinicopathological features of the patients with or without EAC are summarized in Table 1. BE patients with EAC had a larger number of hiatus hernia (P < 0.001), reflux esophagitis (P = 0.004), higher body mass index (P = 0.015), LSBEs (P = 0.002), dysplasia (P = 0.007), and aberrant p53 expression (P < 0.001) than those of patients without EAC. The Ki-67 LI was significantly higher in cases with EAC than in those without EAC (P < 0.001). BE cases harboring EAC had significantly higher CD3+ LPL numbers than those without EAC (P = 0.008), but no other significant differences were detected in other subsets of LPLs. No significant differences were observed in CD3+ LPL number according to the degree of dysplasia and in CD8+ LPL number according to presence of dysplasia and concomitant EAC (Fig. 3a, b). However, among the cases with EAC, Foxp3+ LPL counts were significantly higher in cases with low-grade dysplasia than in those without dysplasia (P = 0.005) (Fig. 3c). Foxp3+ LPL counts were also significantly higher in patients with high-grade dysplasia than in those with low-grade dysplasia (P = 0.005) (Fig. 3c).
a–c The lamina propria lymphocyte (LPL) counts according to the presence of dysplasia and adjacent EAC. a CD3+ LPLs counts. Among the cases without dysplasia, CD3+ LPL counts were significantly higher in cases of BE with EAC than those without EAC (P = 0.021). b CD8+ LPL counts. No significant difference was observed among four groups. c Foxp3+ LPL counts. Among the cases without dysplasia, there were no significant differences in Foxp3+ LPLs count. Among the cases with EAC, Foxp3+ LPL counts were significantly higher in cases with low-grade dysplasia than in those without dysplasia (P = 0.005). Foxp3+ LPL counts were also significantly higher in cases with high-grade dysplasia than in those low-grade dysplasia (P = 0.005). Among the cases without EAC, BE dysplasia was observed in only one case; therefore, statistical analysis was not performed with this group. *P < 0.05, **P < 0.01
LPLs in BE adjacent to EAC and their correlation with clinicopathological factors and clinical outcome of patients
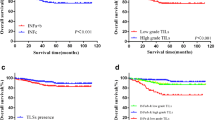
The correlations between LPL counts and clinicopathological characteristics of patients with EAC examined in this study are summarized in supplemental Table 2. High CD3+ LPL counts were significantly associated with the absence of intestinal metaplasia (P = 0.025). High CD8+ LPL counts were significantly associated with lymph node metastasis (P = 0.025) and advanced TNM stage (P = 0.011). High Foxp3+ LPL counts were significantly associated with high Ki-67 LI (P = 0.023) in BE glandular cells. Although this difference was insignificant, high Foxp3+ LPL counts tended to be linked to increased aberrant p53 expression (P = 0.055). There were no significant differences in other factors. Consequently, 25% of patients died of EAC, whereas 2% of patients died due to other causes at the time of last census. In the Kaplan–Meier analysis, patients with high number of CD8+ LPLs in BE adjacent to EAC had significantly worse overall survival than those with low number of CD8+ LPLs (P = 0.019; Fig. 4b), but no significant associations were detected in other subsets of LPLs (Fig. 4a, c). Among the surgically resected cases, high number of CD8+ LPLs group also exhibited worse overall survival (P = 0.028).
Kaplan–Meier curves according to the lamina propria lymphocyte (LPL) and tumor-infiltrating lymphocyte (TIL) status. a CD3+ LPL status. b CD8+ LPL status. c Foxp3+ LPL status. b The high CD8+ LPL counts were significantly associated with worse prognosis (P = 0.019). d CD3+ TIL status. e CD8+ TIL status. f Foxp3+ TIL status. e The high CD8+ TIL counts were significantly associated with better prognosis (P = 0.010). *P < 0.05
TILs in EAC and their correlation with clinicopathological factors and clinical outcomes of the patients
The TIL counts had no significant correlation with the clinicopathological parameters such as Siewert type, tumor depth, lymph node metastasis, and TNM stages of the patients examined. Kaplan–Meier analysis results revealed that the patients harboring more CD8+ TILs in the EAC had a significantly better overall survival than those with fewer CD8+ TILs (P = 0.010; Fig. 4e), but no significant associations were detected in other subsets of TILs examined in this study (Fig. 4d, f).
Discussion
The CD3+ LPL density was significantly higher in BE adjacent to EAC. This result indicated that the T cell infiltration played pivotal roles in facilitating the dysplasia–adenocarcinoma sequence in BE. However, no significant increase was observed on T cell subset analysis of CD8 and Foxp3 possibly due to limited size of the control group (N = 13). Other T cell subsets were not analyzed in this study. Therefore, further detailed T cell profile analysis is warranted to evaluate the impact of BE tissue microenvironment on EAC development.
Foxp3+ LPLs in BE were significantly associated with low- and high-grade dysplasia and increased Ki-67 LI of the glandular epithelium of BE, and tended to link to aberrant p53 protein expression, all of which were the characteristic features of neoplastic progression in BE [2, 25, 31]. These results indicated that the number of Foxp3+ T cells could increase at the early stage of carcinogenesis. Foxp3+ T cells can suppress anti-tumor immunity, thereby hindering immunosurveillance against cancer development [8]. For instance, in uterine cervical epithelium, the environment of Foxp3+ T cell–induced immunoregulatory local tissues played pivotal roles in the multistep carcinogenesis (dysplasia–carcinoma in situ–invasive cancer) [8, 32, 33]. According to a previous study, cervical intraepithelial neoplasia can recruit Foxp3 T cells through the expression of indoleamine 2 and 3-dioxygenase, and the Foxp3+ T cell infiltration was marked in microinvasive cancer cells [32]. Also, in colitis-associated cancer, Foxp3+ T cells may suppress anti-tumor immunity at early stages during cancer development by inhibiting CD4+ and CD8+ T cell activity [34]. In addition, Foxp3 T cells are also reported to play a pivotal role in BE development; however, the clinical impact of Foxp3+ T cells on EAC development has remained unknown [9, 10]. This is the first study demonstrating that the number of Foxp3+ T cells could increase at the early stage of carcinogenesis, dysplasia and increased Ki-67 LI. It is possible that dysplastic and proliferating BE cells have already acquired the ability to recruit Foxp3 T cells and hamper anti-tumor immune response.
In the present study, CD8+ LPLs in adjacent BE were associated with lymph node metastasis and significantly shorter overall survival of the patients, whereas a high density of CD8+ TILs was significantly associated with better prognosis of the patients. These results indicated that CD8+ LPLs represented unfavorable chronic inflammation around the EAC, and subsequently, poor clinical outcomes. Conversely, CD8+ TILs could represent effective anti-tumor immune responses in hosts. The roles of CD8+ T cells in inflammation-associated cancer have remained debatable [11]. For instance, in colitis-associated cancer, CD8+ T cells have been reported to reduce tumor growth via cancer immunosurveillance; however, they also contribute to inflammation, promoting tumor growth [11]. Therefore, the definitive roles of cytotoxic CD8+ T cells under the influence of GERD could be complicated. Previous EAC studies demonstrated that abundant CD8+ TILs were associated with better prognosis [35, 36], but no significant differences were reported in other studies [37, 38]. In addition, the prognostic impact varied with areas of evaluation; high intratumoral CD3/CD8/Foxp3 infiltrations were significantly associated with better prognosis; however, peritumoral lymphocytes had no significant difference, although their mechanisms remained unknown [35]. In the present study, the difference detected between LPL and TIL results could be explained by the methodology used for evaluating lymphocyte infiltration; however, further investigations are required for clarification.
More than 20% of EAC patients treated with endoscopic resection develop metachronous EAC in residual BE within 2 years of resection [39]. Endoscopic ablation is, therefore, recommended to prevent metachronous cancer following ESD. However, it is also true that a relatively high stricture rate and recurrence rate have been reported in the literature in these patients [2]. Therefore, risk stratification of the patients after ESD is at present required in clinical practice. When the Foxp3+ T cells are abundant in the EAC-adjacent areas of the resected specimen, endoscopic ablation or careful surveillance may be recommended because residual BE is highly likely to harbor dysplastic and proliferating cells. In addition, especially in surgically resected cases, when abundant CD8+ T cells are detected in BE adjacent to EAC, repeated (PET-) CT scans might be recommended after treatment because these patients could be more likely to harbor lymph node metastases and experience adverse clinical outcomes. In endoscopically resected cases, abundant CD8+ T cells can be one of the indications of additional surgery because these patients are more likely to harbor lymph node metastases that were not detected at the time of endoscopic resection.
One of the limitations of the present study is the relatively small number of control cases and high-grade dysplasia cases, which may have increased the margin of error.
The results of our present studies revealed the potential influence of the tissue immune microenvironment of BE adjacent to EAC on cancer development and eventual clinical outcome of EAC patients. High T cell density could be associated with EAC development. Foxp3+ T cells possibly increase in number at the early stage of carcinogenesis, and CD8+ T cells in adjacent tissue of EAC could reflect unfavorable inflammatory response and worse prognosis.
Abbreviations
- BE:
-
Barrett’s esophagus
- EAC:
-
esophageal adenocarcinoma
- EGJ:
-
esophagogastric junction
- ESD:
-
endoscopic submucosal dissection
- LPL:
-
lamina propria lymphocyte
- LSBE:
-
long-segment BE
- SSBE:
-
short-segment BE
- TIL:
-
tumor-infiltrating lymphocyte
References
(2017) Japanese classification of esophageal cancer, 11th edition: part I. Esophagus 14:1–36
Fitzgerald RC, di Pietro M, Ragunath K, Ang Y, Kang JY, Watson P, Trudgill N, Patel P, Kaye PV, Sanders S, O'Donovan M, Bird-Lieberman E, Bhandari P, Jankowski JA, Attwood S, Parsons SL, Loft D, Lagergren J, Moayyedi P, Lyratzopoulos G, de Caestecker J, British Society of Gastroenterology (2014) British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut 63:7–42
Spechler SJ, Souza RF (2014) Barrett’s esophagus. N Engl J Med 371:836–845
Coleman HG, Xie SH, Lagergren J (2018) The epidemiology of esophageal adenocarcinoma. Gastroenterology 154:390–405
Ueda Y, Osada H, Osugi H (2007) Thoracic and cardiovascular surgery in Japan during 2005. Annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 55:377–399
Masuda M, Endo S, Natsugoe S et al (2015) Thoracic and cardiovascular surgery in Japan during. Gen Thorac Cardiovasc Surg:2018
Curtius K, Wright NA, Graham TA (2017) An evolutionary perspective on field cancerization. Nat Rev Cancer 18:19
Togashi Y, Shitara K, Nishikawa H (2019) Regulatory T cells in cancer immunosuppression - implications for anticancer therapy. Nat Rev Clin Oncol 16:356–371
Lind A, Siersema PD, Kusters JG, Konijn T, Mebius RE, Koenderman L (2018) The microenvironment in Barrett’s esophagus tissue is characterized by high FOXP3 and RALDH2 levels. Front Immunol 9:1375
Rubinkiewicz M, Migaczewski M, Hankus J et al (2016) Foxp3+ lymphocyte count in Barrett’s esophagus tissue is higher than in inflamed esophageal tissue. Folia Med Cracov 3:51–59
Waldner MJ, Neurath MF (2009) Colitis-associated cancer: the role of T cells in tumor development. Semin Immunopathol 31:249–256
Kavanagh ME, Conroy MJ, Clarke NE, Gilmartin NT, O'Sullivan KE, Feighery R, MacCarthy F, O'Toole D, Ravi N, Reynolds JV, O'Sullivan J, Lysaght J (2016) Impact of the inflammatory microenvironment on T-cell phenotype in the progression from reflux oesophagitis to Barrett oesophagus and oesophageal adenocarcinoma. Cancer Lett 370:117–124
Tantibhaedhyangkul U, Tatevian N, Gilger MA et al (2009) Increased esophageal regulatory T cells and eosinophil characteristics in children with eosinophilic esophagitis and gastroesophageal reflux disease. Ann Clin Lab Sci 39(2):99–107
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg 85:1457–1459
Magi-Galluzzi C, Maddala T, Falzarano SM, Cherbavaz DB, Zhang N, Knezevic D, Febbo PG, Lee M, Lawrence HJ, Klein EA (2016) Gene expression in normal-appearing tissue adjacent to prostate cancers are predictive of clinical outcome: evidence for a biologically meaningful field effect. Oncotarget 7:33855–33865
Richiardi L, Fiano V, Grasso C, Zugna D, Delsedime L, Gillio-Tos A, Merletti F (2013) Methylation of APC and GSTP1 in non-neoplastic tissue adjacent to prostate tumour and mortality from prostate cancer. PLoS One 8:e68162
Moons LM, Kusters JG, Bultman E et al (2005) Barrett’s oesophagus is characterized by a predominantly humoral inflammatory response. J Pathol 207:269–276
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an international TILs working group 2014. Ann Oncol 26:259–271
Hwang WT, Adams SF, Tahirovic E, Hagemann IS, Coukos G (2012) Prognostic significance of tumor-infiltrating T cells in ovarian cancer: a meta-analysis. Gynecol Oncol 124:192–198
Konno-Kumagai T, Fujishima F, Nakamura Y, Nakano T, Nagai T, Kamei T, Sasano H (2019) Programmed death-1 ligands and tumor infiltrating T lymphocytes in primary and lymph node metastasis of esophageal cancer patients. Dis Esophagus 32
Salama P, Phillips M, Grieu F, Morris M, Zeps N, Joseph D, Platell C, Iacopetta B (2009) Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 27:186–192
Chiba T, Ohtani H, Mizoi T, Naito Y, Sato E, Nagura H, Ohuchi A, Ohuchi K, Shiiba K, Kurokawa Y, Satomi S (2004) Intraepithelial CD8+ T-cell-count becomes a prognostic factor after a longer follow-up period in human colorectal carcinoma: possible association with suppression of micrometastasis. Br J Cancer 91:1711–1717
Frey DM, Droeser RA, Viehl CT, Zlobec I, Lugli A, Zingg U, Oertli D, Kettelhack C, Terracciano L, Tornillo L (2010) High frequency of tumor-infiltrating FOXP3(+) regulatory T cells predicts improved survival in mismatch repair-proficient colorectal cancer patients. Int J Cancer 126:2635–2643
Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, Ohtani H (1998) CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res 58:3491–3494
Kastelein F, Biermann K, Steyerberg EW, Verheij J, Kalisvaart M, Looijenga LHJ, Stoop HA, Walter L, Kuipers EJ, Spaander MCW, Bruno MJ, on behalf of the ProBar-study group (2013) Aberrant p53 protein expression is associated with an increased risk of neoplastic progression in patients with Barrett’s oesophagus. Gut 62:1676–1683
Kaye PV, Ilyas M, Soomro I, Haider SA, Atwal G, Menon S, Gill S, Richards C, Harrison R, West K, Ragunath K (2016) Dysplasia in Barrett’s oesophagus: p53 immunostaining is more reproducible than haematoxylin and eosin diagnosis and improves overall reliability, while grading is poorly reproducible. Histopathology 69:431–440
van Olphen S, Biermann K, Spaander MC et al (2015) SOX2 as a novel marker to predict neoplastic progression in Barrett's esophagus. Am J Gastroenterol 110:1420–1428
Sikkema M, Kerkhof M, Steyerberg EW, Kusters JG, van Strien PMH, Looman CWN, van Dekken H, Siersema PD, Kuipers EJ (2009) Aneuploidy and overexpression of Ki67 and p53 as markers for neoplastic progression in Barrett’s esophagus: a case-control study. Am J Gastroenterol 104:2673–2680
Altaf K, Xiong JJ, la Iglesia D et al (2017) Meta-analysis of biomarkers predicting risk of malignant progression in Barrett's oesophagus. Br J Surg 104:493–502
Odze RD. WHO classification of tumours, 5th edition, Volume 1: Digestive System Tumours 2019:32–5
Hong MK, Laskin WB, Herman BE, Johnston MH, Vargo JJ, Steinberg SM, Allegra CJ, Johnston PG (1995) Expansion of the Ki-67 proliferative compartment correlates with degree of dysplasia in Barrett’s esophagus. Cancer 75:423–429
Nakamura T, Shima T, Saeki A et al (2007) Expression of indoleamine 2, 3-dioxygenase and the recruitment of Foxp3-expressing regulatory T cells in the development and progression of uterine cervical cancer. Cancer Sci 98:874–881
Luo Q, Zhang S, Wei H, Pang X, Zhang H (2015) Roles of Foxp3 in the occurrence and development of cervical cancer. Int J Clin Exp Pathol 8:8717–8730
Olguín JE, Medina-Andrade I, Molina E, Vázquez A, Pacheco-Fernández T, Saavedra R, Pérez-Plasencia C, Chirino YI, Vaca-Paniagua F, Arias-Romero LE, Gutierrez-Cirlos EB, León-Cabrera SA, Rodriguez-Sosa M, Terrazas LI (2018) Early and partial reduction in CD4+Foxp3+ regulatory T cells during colitis-associated colon cancer induces CD4+ and CD8+ T cell activation inhibiting tumorigenesis. J Cancer 9:239–249
Stein AV, Dislich B, Blank A, Guldener L, Kröll D, Seiler CA, Langer R (2017 Jan) High intratumoural but not peritumoural inflammatory host response is associated with better prognosis in primary resected oesophageal adenocarcinomas. Pathology 49(1):30–37
Noble F, Mellows T, McCormick Matthews LH et al (2016) Tumour infiltrating lymphocytes correlate with improved survival in patients with oesophageal adenocarcinoma. Cancer Immunol Immunother 65(6):651–662
Hynes CF, Kwon DH, Vadlamudi C, Lofthus A, Iwamoto A, Chahine JJ, Desale S, Margolis M, Kallakury BV, Watson TJ, Haddad NG, Marshall MB (2018) Programmed death ligand 1: a step toward Immunoscore for esophageal cancer. Ann Thorac Surg 106(4):1002–1007
Zingg U, Montani M, Frey DM, Dirnhofer S, Esterman AJ, Went P, Oertli D (2010) Tumour-infiltrating lymphocytes and survival in patients with adenocarcinoma of the oesophagus. Eur J Surg Oncol 36(7):670–677
Pech O, Behrens A, May A, Nachbar L, Gossner L, Rabenstein T, Manner H, Guenter E, Huijsmans J, Vieth M, Stolte M, Ell C (2008) Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett's oesophagus. Gut 57:1200–1206
Acknowledgments
We would like to acknowledge Ms. Yayoi Aoyama and Ms. Yasuko Furukawa for technical support.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Yusuke Gokon, Fumiyoshi Fujishima, Hirotaka Ishida, Taku Yamagata, Takashi Sawai, Miwa Uzuki, Hirofumi Ichikawa, Yuko Itakura, Kazutomi Takahashi, Nobuhisa Yajima, Motohisa Hagiwara, Akiko Nishida, Yohei Ozawa, Tsutomu Sakuma, Rikiya Kanba, Kazuhiro Sakamoto, Masashi Zuguchi, and Masahiro Saito. The first draft of the manuscript was written by Yusuke Gokon and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study protocol was approved by the ethics committee or institutional review board of each participating institution (Accession number of Tohoku University Hospital 2017–1-325). Informed consent was obtained for experimentation with human subjects.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gokon, Y., Fujishima, F., Taniyama, Y. et al. Immune microenvironment in Barrett’s esophagus adjacent to esophageal adenocarcinoma: possible influence of adjacent mucosa on cancer development and progression. Virchows Arch 477, 825–834 (2020). https://doi.org/10.1007/s00428-020-02854-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-020-02854-0