Abstract
Chromosome 9 harbors several relevant oncogenes related to hematolymphoid malignancies and one specific region, 9p24, has come into the focus of attention in the last years as it contains recurrently mutant genes of therapeutic interest. The most prominent genes of this locus are programmed death ligands 1 and 2 (PDL1/PDL2), with the amplification of PDL1 being a hallmark of both classical Hodgkin and primary mediastinal B cell lymphoma, and Janus kinase 2 (JAK2), which is point-mutated in myeloproliferative neoplasms and other myeloid malignancies, and rearranged in PCM1-JAK2-positive myeloid/lymphoid neoplasms with eosinophila. Finally, this locus contains the lysine (K)-specific demethylase 4C (KDM4C/JMJD2C), which is also relevant for oncogenesis. Activation of these genes is effectuated, as exemplified, by multiple mechanisms, which is rather unique to oncogenes, since they are usually affected by just one type of mutation, and points towards the central role of these genes in tumor initiation and growth. Amplifications and, less frequently, translocations are the most common findings for PDL1/PDL2 and JAK2 in lymphomas. In this review, we describe the role of genes located on chromosome 9p24 and their derived proteins in diverse subtypes of lymphomas, with a special focus on PDL1 and PDL2, which are becoming a central target of immunotherapy, not only in classical Hodgkin lymphoma but also in various types of solid cancers. We also elucidate the role of the surgical pathologists in this setting — concerning what they can contribute — both diagnostically and predictively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chromosome 9 has a length of 138,394,717 million base pairs, and is the basis for 774 coding genes [1, 2], representing 4.5% of the total amount of human nuclear DNA. It contains several genes related to hematopoietic functions, ranging from AB0 histo-blood group glycosyltransferases, Abelson murine leukemia viral oncogene homolog 1 (ABL1), to genes at the 9p24 locus (Fig. 1). The latter has recently gained a lot of interest, as several genes implicated in hematolymphoid malignancies are located in this region.
Programmed death ligands 1 and 2 (PDL1/PDL2) are the genes of this locus most attention has been paid to at, as they are key targets of immune checkpoint inhibition. They exert their function by inducing T cell anergy and exhaustion [3]. Another gene located here is Janus kinase 2 (JAK2), mostly known in relation to myeloproliferative neoplasms such as polycythemia vera, primary myelofibrosis, and essential thrombocythemia, in which point mutations (the best-known being JAK2 V617F) are even part of the disease definition [4]. Furthermore, fusions of JAK2 and the pericentriolar material 1 (PCM1) gene, mostly leading to myelodysplastic/myeloproliferative neoplasms with eosinophilia and fibrosis, have been described by us and other groups [5, 6] and were considered by the current WHO classification of tumors of hematopoietic and lymphoid tissues as a separate entity in the chapter of myeloid/lymphoid neoplasms with eosinophilia and recurrent gene rearrangements [7]. Moreover, JAK2 aberrations have also been recognized in subsets of lymphomas [8,9,10]. Another gene at 9p24, seeming to play a role in lymphomas, along with other much commonly mutant epigenetic modifiers such as the histone-lysine N-methyltransferase 2D (KMT2D) [11], is the lysine (K)-specific demethylase 4C (KDM4C/JMJD2C) [12].
Immunotherapy of cancer has a long history dating back to early anti-cancer vaccination attempts [13]. It has recently gained a tremendous amount of interest in the wake of the discovery of the PD1/PDL1 checkpoint axis as a new therapeutic option in oncology [14]. By overcoming the suppression of the immune system induced by tumor cells, both locally and systemically, the therapeutic approach of PD1/PDL1 immune checkpoint inhibition improves the possibility of patients’ organisms to fight cancer. However, this goes in hand with prototypic side effects resembling graft versus host like changes or autoimmune disorders due to immune system (hyper) activation [15].
In this review, we will summarize, from a surgical pathologist’s perspective, the different types of genetic alterations of the 9p24 locus and discuss their implications in lymphomas.
Genetic alterations of the 9p24 region
Alterations of 9p24 and the genes situated here can occur in different ways and mainly consist of amplifications and translocations, while single nucleotide (point) mutations as well as insertions and deletions are not of substantial relevance.
Amplifications
Concerning PDL1 and JAK2, amplifications (Fig. 2) are known to occur in classical Hodgkin lymphomas (cHL), mainly the nodular sclerosis subtype, and primary mediastinal B cell lymphomas (PMBCL) [10, 16]. It also has to be kept in mind that especially in PMBCL and cHL, both harboring 9p24 amplifications in approximately a third of instances, usually several genes are affected as the amplicon encompasses about 3.5 Mb of DNA. Indeed, Rui et al. were the first to describe that more than 10 genes involved in lymphomagenesis are amplified by 9p24 gains [17]. They also suggested a considerable additive “cooperative effect” of KMD4C and JAK2 that leads to increased proliferation and survival advantage of neoplastic cells due to the cumulative effect of epigenetic changes and increased JAK2 downstream signaling.
Multiple JAK2-PDL1 locus FISH signals indicating a 9p24 gain in a primary mediastinal B cell lymphoma case, × 1000. Note 3 to 6 fused red and green FISH signals/case with the RP11-3H3 and RP11-2302 (red) and RP11-28A9 and RP11-60G18 (green) bacterial artificial chromosome probes for the 5′ and 3′ regions of JAK2. Analogous results can be achieved by, e.g., commercially available JAK2 break-apart FISH probes
Translocations
Recently, van Roosbroeck et al. have described several translocations of PDL1 and PDL2 [9]. Such translocations occur both in cHL and in T cell lymphomas (Fig. 3) showing a plethora of translocation partners. In cHL, a frequency of 2% for PDL1 translocations was reported, in contrast to 25% of cases showing 9p24 amplifications [16]. PDL1 rearrangements with IGH, PIM1, and TP63 have also been described in diffuse large B cell lymphomas (DLBCL) [18], where they mainly occur in the non-germinal center B cell (non-GCB) subtype.
Rearrangement of the JAK2-PDL1 locus with split red and green FISH signals with the probes mentioned in Fig. 2 in a peripheral T cell lymphoma case, × 1000
Less is known about specific alterations of JAK2 and KDM4C in lymphomas. JAK2-SEC31 homolog A (SEC31A) fusions have been described in cHL [8]; JAK2-ataxin 2 like (ATXN2L) fusions, in CD4-positive cutaneous T cell lymphoma [19]; JAK2-PCM1 fusions, in exceptionally rare cases of T cell acute lymphoblastic leukemia/lymphoma and B cell acute lymphoblastic leukemia [20]; and KMD4C-IGH fusions, in mucosa-associated lymphoid tissue (MALT) lymphomas [21]. In addition, E twenty-six variant 6 (ETV6)-JAK2 fusions are observable in B- and T cell acute lymphoblastic leukemia/lymphoma [5, 22,23,24].
Other genetic alterations of genes at 9p24
Alterations of PDL1 or PDL2 by single nucleotide mutations or insertions/deletions seem not to play a major role in lymphomas. However, Kataoka et al. reported a disruption of PDL1’s 3′-untranslated region (UTR) leading to a marked increase of PDL1 expression, being stabilized by truncation of the 3′-UTR, in cases of adult T cell leukemia/lymphoma as well as DLBCL [25]. An inversion between SWI/SNF-related, matrix-associated, actin-dependent regulator of chromatin, subfamily a, member 2 (SMARCA2), which is also located at 9p24, and PDL1 has been described in testicular DLBCL, in which this alteration removes a part of the 3′-untranslated region of PDL1 and, most likely, increases the respective protein expression [26].
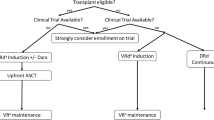
Role of the surgical pathologist
By means of diagnostic surgical pathology techniques, both structural and numeric genetic changes of the 9p24 locus, i.e., rearrangements and amplifications, as well as overexpression of the key players PDL1 or JAK2 and their downstream targets such as phosphorylated (p)-STATs (Fig. 4) can be examined. Although PDL1 expression (Fig. 5) is not as mandatory for clinical trials in lymphomas as in solid tumors such as lung carcinomas [29], knowledge on its status can additionally help in some challenging differential diagnostic instances [28], be prognostically informative [30] or possibly predict sensitivity to PD1/PDL1 immune checkpoint inhibition [31], as illustrated later on.
Overexpression of phosphorylated STAT5 (clone 8-5-2 from Merck; antibody-handling conditions exactly as described in [27]) in a classical Hodgkin lymphoma case, × 360, chromogen diaminobenzidine
Strongly PDL1 (clone E1L3N from Cell Signaling; antibody-handling conditions exactly as described in [28]) positive Hodgkin cell of classical Hodgkin lymphoma, × 400, chromogen diaminobenzidine
The key players on 9p24
In the second part of this review, we summarize the role of the different genes located on 9p24 and their derived proteins in lymphomagenesis. Furthermore, we discuss how these genes’ status can contribute to diagnosis, therapy decision making, and prognosis.
PDL1/PDL2—control of the immune system
PDL1/PDL2 are the best-known genes on 9p24, and their altered expression is a hallmark of immunomodulation used by tumor cells to manipulate host’s immune system to improve chances of the tumor to prevail. PDL1/PDL2’s mechanistic role in lymphoma progression is already well established and used in clinical trials. The prognostic and predictive role of PDL1/PDL2 is still a matter of debate.
Background
PD1 and its ligand PDL1 were discovered in the early and late 1990s, respectively [32, 33]; the genes encoding both PDL1 and PD1’s second ligand, PDL2, the expression of which is more restricted than that of PDL1 [34], are located on chromosome 9p24. PD1 contains an immunoreceptor tyrosine-based switch motif (ITSM) and an immunoreceptor tyrosine-based inhibitory motif (ITIM); ITSM is essential for the transmission of inhibitory signals [35]. After ligation with PDL1 or PDL2, ITSM and ITIM undergo phosphorylation, which consequently leads, through activation of several downstream signaling cascades, to depression of intracellular ZAP70, AKT, ERK, NF-κB and AP1 activity, and net T cell inactivation and impedes T cell proliferation [36]. By means of this the PD1/PDL1 axis is an important checkpoint for controlling T cells, and it can both inhibit effector T cells as well as stimulate immunosuppressive regulatory T cells [3, 37]. Unlike cytotoxic T lymphocyte-associated protein 4 (CTLA4), PD1 and its ligands exert their function in the peripheral tissues and, thus, seem to lead to a primarily local and not to a systemic affection of the immune system [38, 39]. CTLA4 impedes both the cell cycle and several intracellular pathways in T cells; it affects T cells in primary lymphatic organs such as the bone marrow and the thymus. In contrast to PDL1, it does not contain ITIMs [40].
Genetic alterations of PDL1/PDL2 and mechanisms of activation
The genetic mechanisms of PDL1 overexpression have been first discovered in cHL and mainly consist of 9p24 locus amplifications (Fig. 2). Similar alterations have been found in PMBCL [41] and, to a lower extent, in DLBCL [18] as well as in lymphomas of immune-privileged sites such as the central nervous system and the testis [42]. Other less common genetic mechanisms of PDL1 upregulation and activation comprise translocations [9, 18] (Fig. 3) or disruption of the 3′-UTR of PDL1.
PDL1 expression can be regulated by other mechanisms not directly involving aberrations of its gene. It has been shown that PDL1 is inducible by activation of the JAK/STAT pathway [10]. In lymphomas, L265P mutant myeloid differentiation primary response gene 88 (MYD88) can activate JAK2 and PDL1 [43]. In addition, PDL1 expression can be induced by the latent membrane protein 1 (LMP1) of Epstein-Barr virus (EBV) via activation of STAT (particularly STAT3)- and activated protein 1 (AP1)-mediated pathways, which is observable in cHL [44] and extranodal NK/T cell lymphoma of the nasal type [45]. As to be expected, other causes of STAT-activation also enhance PDL1-expression as seen in anaplastic lymphoma kinase (ALK)-positive anaplastic large cell lymphoma (ALCL) [46], or in relation to active cytokine signaling [47], which is commonly observable in, e.g., activated B cell (ABC)-like DLBCL and cHL [48, 49]. Finally, at least in DLBCL, translocations of IGH, PIM1, and TP63 with the PDL1 locus that lead to the latter’s overexpression have been described too [18].
Expression of PDL1/PDL2 and its use in the differential diagnosis of lymphomas
We and other groups have investigated the expression of PDL1 and, to a smaller extent, PDL2 in lymphomas with consistent results regarding most entities [28, 50]. It could be demonstrated that, apart from cHL and nodular lymphocyte predominant Hodgkin lymphoma (NLPHL), up to a third of DLBCL, mainly those of the ABC type [51], and PMBCL express PDL1; in other B cell lymphoma entities, PDL1 is only expressed in a low percentage of cases [28]. PDL1 shows a homogenous staining in lymphomas (Fig. 5), yet in chronic lymphocytic B cell leukemia (CLL), PDL1-expression has been described to be confined to the proliferation centers [52]. PDL1 expression is observed both in the tumor microenvironment (particularly in tumor-infiltrating macrophages; Fig. 6) and in lymphoma cells, which is in contrast to PD1-expression that is primarily seen in T cells of the microenvironment [53, 54]. In T cell- and histiocyte-rich B cell lymphomas (THRBCL), PDL1-expression is seen in both T cells and histiocytes, while the tumor cells themselves are negative for PDL1 as we could demonstrate in double-staining approaches [28]. This is a particularly helpful feature in the difficult differential diagnosis of THRBCL and cHL and NLPHL. The latter two entities show detectable PDL1 expression in the tumor cells in 70 to 50% of cases, respectively, in contrast to THRBCL. Admittedly, result interpretation might be occasionally difficult since all three diseases are characterized by high numbers of PDL1-positive tumor-infiltrating macrophages, an issue that can be elegantly approached by double-stainings for MUM1/PDL1 [35] in case of suspected cHL, for OCT2/PDL1 in NLPHL and BCL6/PDL1 in THRBCL [28] to unequivocally identify respective tumor cells for estimation of PDL1 expression. In T cell lymphomas, PDL1 expression is observable in peripheral T cell lymphoma, ALK-positive ALCL, extranodal NK/T cell lymphoma of the nasal type, cutaneous T cell lymphoma, as well as in adult T cell leukemia/lymphoma [55], which should be taken into differential diagnostic consideration. Expectedly (rev. in [35]), all EBV-associated malignancies with latency types 2 and 3 of virus infection are anticipated to be PDL1 positive.
Multiple PDL1 positive tumor-infiltrating macrophages (TIM) in classical Hodgkin lymphoma intermingled with a few very strongly positive Hodgkin- and Reed-Sternberg cells (HRSC), × 200, chromogen diaminobenzidine. Note that those TIM considerably outnumber the HRSC and, thus, more substantially contribute to the total PDL1-positivity in respective cases
Shi et al. performed the first larger study investigating the expression of PDL2 in lymphomas in 2014 [56]. Using a cutoff of 20% of tumor cells and not considering the staining intensity, similar results were obtained as in a previously published study on the expression of PDL1 [50]. More than two thirds of PMBCL cases were positive for PDL2, while most DLBCL cases did not show PDL2 expression. This finding led to propose PDL2 as a potential discriminatory marker for PMBCL and DLBCL (specificity 97%, sensitivity 72%), which remains to be validated. PDL2-expression substantially correlated with PDL2 copy number gains, which was considerably more pronounced than the rather weak link between expression of PDL1 and PDL1 gene amplifications in lymphomas [28].
PDL1 as a therapeutic target of lymphomas
There are already several finished as well as ongoing, mainly phase 2 trials regarding the PD1/PDL1 immune checkpoint inhibition in B cell lymphomas (reviewed in [57, 58]). Due to the high expression levels of PDL1, cHL was the first lymphoid malignancy in which this type of therapy was applied. The initial seminal study in a cohort of 18 patients with refractory/relapsing cHL showed complete remissions (CR) in 17% and partial remissions (PR) in 70% [59]. Subsequent studies showed similar encouraging results (n = 31, CR 16%, PR 48%/n = 210, CR 22%, PR 47%) [60, 61]. Currently, two antibodies (nivolumab and pembrolizumab) are approved by the American and European agencies for treatment of relapsed and/or refractory cHL [57, 58]. Combinatory/additive approaches of radio- and chemotherapy together with PDL1-centered immunotherapy have been successfully tested in first cohorts too [62]. These approaches base on the hypothesis that the damage induced by radio- and chemotherapy renders tumor cells more “visible” to an immune system (re-)activated by immune checkpoint inhibition [63]. In PMBCL, which shares 9p24 amplifications with cHL, first clinical trials using similar approaches have been reported as well, yet the overall response rates are approximately 40% (heavily pretreated patients, n = 18) [64]. In DLBCL, PDL1-targeted therapy has only been tested in small cohorts or cohorts mixed with other entities such as PMBCL and small B cell lymphomas, and data still remains somewhat inconclusive [65], which can be related to, e.g., the less prominent interactions of PMBCL with its microenvironment compared to cHL. In small B cell lymphomas such as follicular lymphoma (FL), mantle cell lymphoma, and CLL, immunotherapy in general has not been investigated at a larger scale; in relapsed FL, a first study combining PDL1-centered immunotherapy and rituximab has shown promising results (n = 29, CR 52%, PR 14%) [66]. As in cHL, adding PDL1 blockers to conventional therapy regimens has been reported to imply a benefit in comparison to only very limited treatment response if given as a single agent [58]. PDL1 inhibition in lymphomas of immunoprivileged sites may deserve further evaluation too (5 investigated cases) [67].
So far, no drugs specifically targeting PDL2 have been developed [57].
While clinical trials with PD1/PDL1 immune checkpoint inhibition in T cell lymphomas in general have thus far shown limited response rates [65], in extranodal NK/T cell lymphoma of the nasal type, which is known to have an aggressive and mostly fatal course, the situation is different. A small case series (n = 3) has shown that PDL1 is substantially upregulated in this entity due to EBV infection of the tumor cells, and PD1 blockade is very effective in otherwise fatal relapses of this disease [68].
The impact of PDL1 expression on prognosis and therapy response
The prognostic and predictive role of PDL1 expression in lymphomas is still a matter of debate. Due to the lack of large randomized trials as available in solid tumors such as lung carcinomas, most experience is gathered from retrospective studies, which might be difficult to compare, especially when dealing with rarer entities such as PMBCL. This might be not only due to limited case numbers but also due to different antibodies or different evaluation strategies being used. A large study on 1253 DLBCL patients showed negative correlation between PDL1 expression and overall survival [51]. However, Xing et al. could show that PDL1 expression in DLBCL treated with standard R-CHOP treatment is associated with a better overall survival rate, yet not with other important variables such as remission after first therapy, relapse- or progression-free survival [69]. Bledsoe et al. demonstrated that high PDL1 expression and low MUM1 expression is correlated with better outcome than vice versa expression of these two proteins in PMBCL [30]. In our opinion, the “conflicting” results on the prognostic impact of PDL1 expression in lymphomas are on the one hand linked to technical issues related to diagnostic antibodies and to difficulties in distinguishing expression on tumor cells and tumor-microenvironment cells; on the other, probably due to the subentity-specific and patient’s immunologic/immunogenetic-specific context, PDL1’s rather moderate prognostic effect might be highly modified by the specific type of therapy applied (e.g., whether steroids, cereblon-targeted therapy, or other immunomodulatory compounds are given or not).
In a landmark study of cHL, 9p24 alterations were associated with inferior outcome (in conventionally treated patients); on the other hand, 9p24 alterations in general seemed to be an indicator for response to PD1/PDL1 immune checkpoint inhibition [31]. Several smaller cohort studies suggested that best responses with immune checkpoint inhibition (targeting PD1/PDL1) are seen in lymphomas harboring specific 9p24 alterations such as cHL-, PMBCL-, and EBV-associated lymphomas and lymphomas of immunoprivileged sites [67]. In therapy-refractory lymphomas, there seems to be a discrepancy between PDL1 expression and amplification of the PDL1 locus, supporting the hypothesis that other mechanisms, next to gene amplifications, are involved in upregulation of PDL1 expression [70].
Hands-on PDL1 immunohistochemistry
Several antibodies for PDL1 immunohistochemistry are available for routine and research purposes. In lung carcinomas, immunohistochemical evaluation of PDL1-expression both in tumor cells and in the microenvironment is an essential part for treatment decision, and depending on the drug used, several antibody clones and detailed guidelines for their respective evaluation are available [29, 71]. For lymphomas, no such guidelines exist, and results of the PDL1 immunohistochemistry are not part of a treatment decision. However, apart from being useful in some difficult differential diagnoses as detailed above, information on the PDL1 expression quality is regularly asked for by our clinical colleagues particularly in relapsed/refractory instances. In our study on PDL1 expression in lymphomas, we directly compared the performance of two different clones, E1L3N and SP142 [28]. In our hands, both antibodies showed good practicability, with SP142 being less sensitive and considerably more expensive than E1L3N, so the latter clone was used in our lymphoma cohorts. Other clones, which are currently mainly used in PDL1 evaluation of lung carcinomas, such as SP263 und 22C3 [72], show in our hands result very similar to E1L3N when evaluated in lymphomas, so that all these clones might be considered equivalent for the particular circumstances of lymphoma diagnostics. Indeed, the main differences between the assays are rather linked to the antigenic retrieval conditions, to which the tissue sections are exposed as per protocol, than to genuine biological issues.
JAK2—functions beyond mere signal transduction
JAK2 is an important signal transducer and is also involved in activation of histones and is thus directly influencing gene expression. It plays a role in both B cell and T cell lymphomas, and its therapeutic role has not yet been thoroughly explored in lymphomas.
Background
JAK2 is a member of a family of cytoplasmic tyrosine kinases, comprising JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2). JAKs are associated with cytokine receptors, which themselves lack intrinsic tyrosine kinase activity. JAKs activate target genes by phosphorylation of signal transducer and activator of transcription (STAT) factors. JAKs can also activate other signaling cascades such as the mitogen-activated protein (MAP) kinase and the phosphatidylinositide 3 (PI3)-kinase/protein kinase B (also called AKT) pathway. Besides phosphorylating proteins of signal transduction cascades, JAK2 can also be found in the nucleus directly phosphorylating histone H3, which leads to chromatin remodeling (non-canonical JAK signaling) [73].
Genetic alterations of JAK2 and mechanisms of activation
JAK2 point mutations are common in myeloid neoplasms such as the JAK2 V617F mutation in myeloproliferative neoplasms [74] or mutation in exon 12 in polycythemia vera [75]. However, mutations in lymphoid neoplasms have only been found in subsets of acute lymphoblastic leukemia but not in lymphomas [76, 77]. With respect to lymphomas, JAK3, the gene of which is located on chromosome 19, is the primarily mutant JAK family member [78]. The very rare translocations JAK2-SEC31A in cHL [8] and JAK2-PCM1 in B/T cell acute lymphoblastic leukemias [20] have been mentioned before. In the latter, the fusion partner PCM1 supports oligomerization and, thus, activation of JAK2 and increases STAT-, particularly STAT5-mediated signaling [79]. Nevertheless, JAK2 has an important function in lymphomas as being confirmed in JAK2 inhibition experiments in in vitro models [17]. JAK2 is part of the 9p24 amplicon in cHL and PMBCL, which causes its enhanced activity in these entities (Fig. 7) even in the absence of activating mutations [17]. It has been shown that V617F mutant JAK2 can stimulate PDL1 expression in myeloproliferative neoplasms [80], so — provided these findings can be translated to lymphoma cells as well — another direct link between JAK2 and PDL1 has been found.
Overexpression of phosphorylated JAK2 (clone C80C3 from Cell Signaling; 1, antibody-handling conditions exactly as described in [16]) in a primary mediastinal B cell lymphoma case, × 400, chromogen aminoethyl carbazole
It has also become evident that, particularly in lymphomas, alterations of other genes can lead to increased JAK2 activation and, thus, enhanced JAK2-mediated signaling and cell proliferation: inactivating mutations of suppressor-of-cytokine-signaling 1 (SOCS1), a downregulator of JAK2, have been first described in cHL and PMBCL lacking 9p24 amplifications [81]. Later studies of the same group and our own observations show that SOCS1 mutations and 9p24 amplifications are not as mutually exclusive as previously thought, and can also be found in DLBCL and small B cell lymphomas as well as with a “pervasive” high frequency in cHL [27, 82]. In addition, JAK2 can be dephosphorylated and, thus, inactivated by tyrosine-protein phosphatase non-receptor type 1 (PTPN1), which is also mutated in a subset of cHL and PMBCL [83]. Mutations of STAT-genes themselves have been described in small subsets of DLBCL [84], and similar to SOCS1, concurrent mutations including JAK2, SOCS1, and STAT6 have been described in PMBCL [85]. Finally, MYD88, which is rather linked to activation of the NF-κB pathway, also interferes with JAK/STAT signaling, as Ngo et al. demonstrated in cell culture experiments of ABC DLBCL cell lines that MYD88 L265P mutant clones rely on JAK-related activation of STAT3 for NF-κB mediated cell proliferation and survival [86].
In T cell lymphomas, JAK2 may also play a role. In angioimmunoblastic T cell lymphoma, gain of function mutations of JAK2 have been observed in 2/85 cases [87]. JAK2-PCM1 fusions are known to occur in a small subset of T cell acute lymphoblastic leukemia/lymphoma [20]. In addition, Roncero et al. [88] recently described some new JAK2 mutations and fusions in this entity leading to JAK2 upregulation associated with activation of LIM domain only 2 (LMO2), a key molecule in this entity.
Expression of JAK2
A previous large scale study of our group could confirm the high prevalence rate of JAK2 gains in cHL and PMBCL [16]. An analysis of phosphorylated, and, thus, functional p-JAK2, p-STAT3, and p-STAT5 protein expressions showed, as to be expected, that their phosphorylation correlated with JAK2 gains; furthermore, p-STAT3 expression defined a group of non-GCB DLBCL with inferior outcome.
Importantly, with respect to 9p24 gains, besides canonical and non-canonical JAK signaling, JAK2 synergistically enhances PDL1 expression, which has been shown by Green et al. in cell culture experiments [10], and JAK2 inhibition had a direct effect on PDL1 expression in these cells.
The interactions between JAK2 and KDM4C are discussed in the next section of this review.
There are no practical published guidelines on how to qualitatively and quantitatively analyze JAK2 and p-JAK2 expressions; moreover, the p-JAK2 staining is prone to fixation artifacts, and as so far these markers are mainly applied in research settings and not in the diagnostic routine. Yet, in the context of myeloproliferative malignancies, application of p-STAT5 stainings can serve as a diagnostic substitute for pathologic activation of JAK2 signaling and has some routine applications [89, 90]; the relevance of which remains to be determined in lymphomas.
JAK2 as a therapeutic target of lymphomas
One of the first clinical trials using JAK2 inhibition with ruxolitinib in cHL has recently been published (NCT01877005) [91]. The overall response rate was only 9.4% with partial responses only; transient stable disease was achieved in 34% of the 32 enrolled patients. The authors suggest that despite this limited success, ruxolitinib might still be included in combination therapy approaches with other drugs due to its minor toxicity profile.
KMD4C—A key to the epigenome
The 9p24 locus plays a role in epigenetic regulation hosting the KMD4C gene. KMD4C synergistically interacts with other proteins such as JAK2. However, its therapeutic potential still needs further evaluation.
Background
Epigenetic regulation of genes is mainly effectuated by histone methylation or acetylation or by direct methylation of DNA [92]. KMD4C, also known as JMJDC2 and gene amplified in squamous cell carcinoma 1 (GASC1), is a member of the Jumonji family of demethylases and exerts its function by removing methyl groups from the repressive histone mark, trimethylated lysine 9, of histone H3 (H3K9me3), thus, leading to gene activation [93]. It acts contrarily to histone-lysine N-methyltransferase 2D (KMT2D/MLL2), a histone methyltransferase. Importantly, KMT2D is the gene with the highest mutational frequency in DLBCL (20–35% of cases) and FL (up to 80% of cases), with mutations leading to a loss of its function [94].
Genetic alterations of KMD4C and mechanisms of activation
A role for KMD4C in lymphoid malignancies has first been suggested in MALT lymphomas in 2008 [21]. Two years later, a seminal study of Rui et al. revealed the co-amplification of JAK2 and KMD4C, supposed to be a new way to modify the epigenome of lymphomas [17], and JAK2 and KMD4C were titled “partners in crime” by the accompanying editorial [95]. This study revealed a new role for JAK2 to activate histones, as described in the section above, as well as showed the importance of epigenetic regulation in lymphomas. The synergistic functional importance of these two oncogenes has been corroborated by experimental evidence showing that inhibition of JAK2 and KMD4C knockdown lead to cell death, and that JAK2 and KMD4C synergistically upregulate MYC expression in lymphoma cells. Direct interactions between KMD4C and PDL1 have not been described yet.
Epigenetic modifiers as a therapeutic target of lymphomas
Therapeutic epigenetic modification has been already applied to DLBCL and FL [96]. Here, besides the already mentioned KMT2D mutants, key molecularly selected instances might be enhancer of zeste homolog 2 (EZH2) and cAMP-response element-binding binding protein/E1A-associated protein p300 (CREBBP/EP300) mutant cases. First clinical phase 1 and phase 2 studies have been or are currently undertaken utilizing histone deacetylase inhibitors. In vitro studies have produced conflicting equivocal results so far [96]. In cHL and PMBCL, epigenetic-targeted therapy has yet not been studied in clinical trials.
Is there still something else? Less well-studied genes on 9p24 with potential oncogenic importance
What is known about the other genes encoded by the region 9p24? Besides PDL1, PDL2, KMD4C, and JAK2, 6 genes have been shown to be upregulated in lymphomas with 9p24 amplifications [17]:
-
Glycine decarboxylase (GLDC) is involved in the folate mediated one-carbon metabolism, and its upregulation is associated with tumorigenesis, tumor cell growth, and poorer outcome in lung cancer patients [97]. A higher expression of GLDC has been found in lymphoma cell lines harboring TP53 mutations [98], and this was accompanied by changes in glycolysis and glycine/serine metabolism fostering tumor cell growth.
-
RAS-related nuclear protein binding protein 6 (RANBP6) has been initially identified to be a potential oncogene as it was included in the minimal amplification region of 9p24 in PMBCL [17]. In cell culture experiments, knockdown of RANBP6, along with KMD4C and JAK2, had an effect on cell survival by induction of apoptosis in PMBCL and cHL, yet not in DLBCL cell lines [17]. RANBP6 is an 80% homolog of RANBP1 (the latter located at 22q11.21). RANBP1 stimulates the GTPase activity of RAN and is important in the complex process of mitosis [99]. So far, its function and relevance in lymphomas has not been elucidated further.
The remaining identified four genes, C9orf46, KIAA1432, KIAA2026, and UHRF2, have not been yet linked to lymphomagenesis.
Other genes located on 9p24 such as relaxin 1 and 2 (RLN1/RLN2), interleukin 33 (IL33), and excitatory amino-acid transporter 3 (EAAT3) have not been related to lymphomas, yet may play a general role in tumorigenesis (Fig. 1). SMARCA2 (also located at 9p24) as a fusion partner of PDL1 has been mentioned above.
Conclusions
Coming back to the question raised initially regarding the role of the surgical pathologist in this setting, many pathologists including our research group have been involved in and significantly contributed to studies deciphering alterations of the 9p24 locus and their importance for lymphomagenesis. By tools already implemented in routine diagnostic procedures such as FISH and sequencing techniques, amplifications, translocations, and mutations of genes at 9p24 can be actively sought for. Furthermore, protein expression of PDL1, PDL2, and JAK2 as well as downstream targets of JAK2 such as p-STATs can be quantified or at least visualized. Diagnostically, PDL1 and potentially PDL2 can be used in equivocal cases with the differential diagnosis of cHL, PMBCL, and THRBCL. So far and in contrast to solid cancers, PDL1 scoring is not required for current therapeutic trials, and no guidelines exist regarding how to qualitatively and quantitatively analyze PDL1 in lymphomas. This, according to our experience, is a substantial lack and potentially also a restraint which has to be addressed accordingly.
Indeed, although 9p24 locus alterations in lymphomas do not (yet?) contribute significantly to the routine diagnostic work of surgical pathologists, investigation in this field by pathologists has certainly improved our knowledge on lymphomas and empowered clinical studies, as this chromosomal region 9p24 harbors several genes of interest concerning the emerging therapeutic approach of immune checkpoint inhibition therapy, targeted signaling inhibition, and epigenetic modulation. It has become evident that not only PDL1 and PDL2 are of significance in this regard, since other genes of the amplicon, particularly JAK2 and KDM4C also play a distinctive additive role. All these genes and their derived proteins have a broad impact on the manipulation of the immune system as well as on tumor cell growth and survival. Their effects may provide a potential new starting point of chemotherapy-saving treatment approaches aiming at blocking several factors and pathways of this complex.
References
http://www.ensembl.org/Homo_sapiens/Location/Chromosome?chr=9;r=9:1-138394717. Accessed 01/10/2018
Humphray SJ, Oliver K, Hunt AR, Plumb RW, Loveland JE, Howe KL, Andrews TD, Searle S, Hunt SE, Scott CE, Jones MC, Ainscough R, Almeida JP, Ambrose KD, Ashwell RI, Babbage AK, Babbage S et al (2004) DNA sequence and analysis of human chromosome 9. Nature 429(6990):369–374. https://doi.org/10.1038/nature02465
Zhang X, Schwartz JC, Guo X, Bhatia S, Cao E, Lorenz M, Cammer M, Chen L, Zhang ZY, Edidin MA, Nathenson SG, Almo SC (2004) Structural and functional analysis of the costimulatory receptor programmed death-1. Immunity 20(3):337–347
Kota J, Caceres N, Constantinescu SN (2008) Aberrant signal transduction pathways in myeloproliferative neoplasms. Leukemia 22(10):1828–1840. https://doi.org/10.1038/leu.2008.236
Hoeller S, Walz C, Reiter A, Dirnhofer S, Tzankov A (2011) PCM1-JAK2-fusion: a potential treatment target in myelodysplastic-myeloproliferative and other hemato-lymphoid neoplasms. Expert Opin Ther Targets 15(1):53–62. https://doi.org/10.1517/14728222.2011.538683
Heiss S, Erdel M, Gunsilius E, Nachbaur D, Tzankov A (2005) Myelodysplastic/myeloproliferative disease with erythropoietic hyperplasia (erythroid preleukemia) and the unique translocation (8;9)(p23;p24): first description of a case. Hum Pathol 36(10):1148–1151. https://doi.org/10.1016/j.humpath.2005.07.020
Bain BJ, Horny H-P, Arber DA, Tefferi A, Hasserjian RP (2017) Myeloid/lymphoid neoplasms with eosinophilia and rearrrangement of PDGFRA, PDGFRB or FGFR1, or with PCM1-JAK2. In: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC, Lyon
Van Roosbroeck K, Cox L, Tousseyn T, Lahortiga I, Gielen O, Cauwelier B, De Paepe P, Verhoef G, Marynen P, Vandenberghe P, De Wolf-Peeters C, Cools J, Wlodarska I (2011) JAK2 rearrangements, including the novel SEC31A-JAK2 fusion, are recurrent in classical Hodgkin lymphoma. Blood 117(15):4056–4064. https://doi.org/10.1182/blood-2010-06-291310
Van Roosbroeck K, Ferreiro JF, Tousseyn T, van der Krogt JA, Michaux L, Pienkowska-Grela B, Theate I, De Paepe P, Dierickx D, Doyen C, Put N, Cools J, Vandenberghe P, Wlodarska I (2016) Genomic alterations of the JAK2 and PDL loci occur in a broad spectrum of lymphoid malignancies. Genes Chromosomes Cancer 55(5):428–441. https://doi.org/10.1002/gcc.22345
Green MR, Monti S, Rodig SJ, Juszczynski P, Currie T, O'Donnell E, Chapuy B, Takeyama K, Neuberg D, Golub TR, Kutok JL, Shipp MA (2010) Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood 116(17):3268–3277. https://doi.org/10.1182/blood-2010-05-282780
Juskevicius D, Jucker D, Klingbiel D, Mamot C, Dirnhofer S, Tzankov A (2017) Mutations of CREBBP and SOCS1 are independent prognostic factors in diffuse large B cell lymphoma: mutational analysis of the SAKK 38/07 prospective clinical trial cohort. J Hematol Oncol 10(1):70. https://doi.org/10.1186/s13045-017-0438-7
Berry WL, Janknecht R (2013) KDM4/JMJD2 histone demethylases: epigenetic regulators in cancer cells. Cancer Res 73(10):2936–2942. https://doi.org/10.1158/0008-5472.CAN-12-4300
Pardoll D (2015) Cancer and the immune system: basic concepts and targets for intervention. Semin Oncol 42(4):523–538. https://doi.org/10.1053/j.seminoncol.2015.05.003
Lipson EJ, Forde PM, Hammers HJ, Emens LA, Taube JM, Topalian SL (2015) Antagonists of PD-1 and PD-L1 in cancer treatment. Semin Oncol 42(4):587–600. https://doi.org/10.1053/j.seminoncol.2015.05.013
Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, Iyer AK (2017) PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol 8:561. https://doi.org/10.3389/fphar.2017.00561
Meier C, Hoeller S, Bourgau C, Hirschmann P, Schwaller J, Went P, Pileri SA, Reiter A, Dirnhofer S, Tzankov A (2009) Recurrent numerical aberrations of JAK2 and deregulation of the JAK2-STAT cascade in lymphomas. Mod Pathol 22(3):476–487. https://doi.org/10.1038/modpathol.2008.207
Rui L, Emre NC, Kruhlak MJ, Chung HJ, Steidl C, Slack G, Wright GW, Lenz G, Ngo VN, Shaffer AL, Xu W, Zhao H, Yang Y, Lamy L, Davis RE, Xiao W, Powell J, Maloney D, Thomas CJ, Moller P et al (2010) Cooperative epigenetic modulation by cancer amplicon genes. Cancer Cell 18(6):590–605. https://doi.org/10.1016/j.ccr.2010.11.013
Georgiou K, Chen L, Berglund M, Ren W, de Miranda NF, Lisboa S, Fangazio M, Zhu S, Hou Y, Wu K, Fang W, Wang X, Meng B, Zhang L, Zeng Y, Bhagat G, Nordenskjold M, Sundstrom C, Enblad G, Dalla-Favera R, Zhang H, Teixeira MR, Pasqualucci L, Peng R, Pan-Hammarstrom Q (2016) Genetic basis of PD-L1 overexpression in diffuse large B-cell lymphomas. Blood 127(24):3026–3034. https://doi.org/10.1182/blood-2015-12-686550
Panagopoulos I, Gorunova L, Spetalen S, Bassarova A, Beiske K, Micci F, Heim S (2017) Fusion of the genes ataxin 2 like, ATXN2L, and Janus kinase 2, JAK2, in cutaneous CD4 positive T-cell lymphoma. Oncotarget 8(61):103775–103784. https://doi.org/10.18632/oncotarget.21790
Bain BJ, Ahmad S (2014) Should myeloid and lymphoid neoplasms with PCM1-JAK2 and other rearrangements of JAK2 be recognized as specific entities? Br J Haematol 166(6):809–817. https://doi.org/10.1111/bjh.12963
Vinatzer U, Gollinger M, Mullauer L, Raderer M, Chott A, Streubel B (2008) Mucosa-associated lymphoid tissue lymphoma: novel translocations including rearrangements of ODZ2, JMJD2C, and CNN3. Clin Cancer Res 14(20):6426–6431. https://doi.org/10.1158/1078-0432.CCR-08-0702
Adelaide J, Perot C, Gelsi-Boyer V, Pautas C, Murati A, Copie-Bergman C, Imbert M, Chaffanet M, Birnbaum D, Mozziconacci MJ (2006) A t(8;9) translocation with PCM1-JAK2 fusion in a patient with T-cell lymphoma. Leukemia 20(3):536–537. https://doi.org/10.1038/sj.leu.2404104
Roberts KG, Li Y, Payne-Turner D, Harvey RC, Yang YL, Pei D, McCastlain K, Ding L, Lu C, Song G, Ma J, Becksfort J, Rusch M, Chen SC, Easton J, Cheng J, Boggs K, Santiago-Morales N, Iacobucci I, Fulton RS, Wen J, Valentine M, Cheng C, Paugh SW, Devidas M, Chen IM, Reshmi S, Smith A, Hedlund E, Gupta P, Nagahawatte P, Wu G, Chen X, Yergeau D, Vadodaria B, Mulder H, Winick NJ, Larsen EC, Carroll WL, Heerema NA, Carroll AJ, Grayson G, Tasian SK, Moore AS, Keller F, Frei-Jones M, Whitlock JA, Raetz EA, White DL, Hughes TP, Guidry Auvil JM, Smith MA, Marcucci G, Bloomfield CD, Mrózek K, Kohlschmidt J, Stock W, Kornblau SM, Konopleva M, Paietta E, Pui CH, Jeha S, Relling MV, Evans WE, Gerhard DS, Gastier-Foster JM, Mardis E, Wilson RK, Loh ML, Downing JR, Hunger SP, Willman CL, Zhang J, Mullighan CG (2014) Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia. N Engl J Med 371(11):1005–1015. https://doi.org/10.1056/NEJMoa1403088
Reiter A, Walz C, Watmore A, Schoch C, Blau I, Schlegelberger B, Berger U, Telford N, Aruliah S, Yin JA, Vanstraelen D, Barker HF, Taylor PC, O'Driscoll A, Benedetti F, Rudolph C, Kolb HJ, Hochhaus A, Hehlmann R, Chase A, Cross NC (2005) The t(8;9)(p22;p24) is a recurrent abnormality in chronic and acute leukemia that fuses PCM1 to JAK2. Cancer Res 65(7):2662–2667. https://doi.org/10.1158/0008-5472.CAN-04-4263
Kataoka K, Shiraishi Y, Takeda Y, Sakata S, Matsumoto M, Nagano S, Maeda T, Nagata Y, Kitanaka A, Mizuno S, Tanaka H, Chiba K, Ito S, Watatani Y, Kakiuchi N, Suzuki H, Yoshizato T, Yoshida K, Sanada M, Itonaga H, Imaizumi Y, Totoki Y, Munakata W, Nakamura H, Hama N, Shide K, Kubuki Y, Hidaka T, Kameda T, Masuda K, Minato N, Kashiwase K, Izutsu K, Takaori-Kondo A, Miyazaki Y, Takahashi S, Shibata T, Kawamoto H, Akatsuka Y, Shimoda K, Takeuchi K, Seya T, Miyano S, Ogawa S (2016) Aberrant PD-L1 expression through 3'-UTR disruption in multiple cancers. Nature 534(7607):402–406. https://doi.org/10.1038/nature18294
Twa DD, Mottok A, Chan FC, Ben-Neriah S, Woolcock BW, Tan KL, Mungall AJ, McDonald H, Zhao Y, Lim RS, Nelson BH, Milne K, Shah SP, Morin RD, Marra MA, Scott DW, Gascoyne RD, Steidl C (2015) Recurrent genomic rearrangements in primary testicular lymphoma. J Pathol 236(2):136–141. https://doi.org/10.1002/path.4522
Juskevicius D, Jucker D, Dietsche T, Perrina V, Rufle A, Ruiz C, Dirnhofer S, Tzankov A (2018) Novel cell enrichment technique for robust genetic analysis of archival classical Hodgkin lymphoma tissues. Lab Invest. https://doi.org/10.1038/s41374-018-0096-6
Menter T, Bodmer-Haecki A, Dirnhofer S, Tzankov A (2016) Evaluation of the diagnostic and prognostic value of PDL1 expression in Hodgkin and B-cell lymphomas. Hum Pathol 54:17–24. https://doi.org/10.1016/j.humpath.2016.03.005
Scheel AH, Dietel M, Heukamp LC, Johrens K, Kirchner T, Reu S, Ruschoff J, Schildhaus HU, Schirmacher P, Tiemann M, Warth A, Weichert W, Fischer RN, Wolf J, Buettner R (2016) Harmonized PD-L1 immunohistochemistry for pulmonary squamous-cell and adenocarcinomas. Mod Pathol 29(10):1165–1172. https://doi.org/10.1038/modpathol.2016.117
Bledsoe JR, Redd RA, Hasserjian RP, Soumerai JD, Nishino HT, Boyer DF, Ferry JA, Zukerberg LR, Harris NL, Abramson JS, Sohani AR (2016) The immunophenotypic spectrum of primary mediastinal large B-cell lymphoma reveals prognostic biomarkers associated with outcome. Am J Hematol 91(10):E436–E441. https://doi.org/10.1002/ajh.24485
Roemer MG, Advani RH, Ligon AH, Natkunam Y, Redd RA, Homer H, Connelly CF, Sun HH, Daadi SE, Freeman GJ, Armand P, Chapuy B, de Jong D, Hoppe RT, Neuberg DS, Rodig SJ, Shipp MA (2016) PD-L1 and PD-L2 genetic alterations define classical Hodgkin lymphoma and predict outcome. J Clin Oncol 34(23):2690–2697. https://doi.org/10.1200/JCO.2016.66.4482
Ishida Y, Agata Y, Shibahara K, Honjo T (1992) Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J 11(11):3887–3895
Dong H, Zhu G, Tamada K, Chen L (1999) B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med 5(12):1365–1369. https://doi.org/10.1038/70932
Messal N, Serriari NE, Pastor S, Nunes JA, Olive D (2011) PD-L2 is expressed on activated human T cells and regulates their function. Mol Immunol 48(15–16):2214–2219. https://doi.org/10.1016/j.molimm.2011.06.436
Muenst S, Soysal SD, Tzankov A, Hoeller S (2015) The PD-1/PD-L1 pathway: biological background and clinical relevance of an emerging treatment target in immunotherapy. Expert Opin Ther Targets 19(2):201–211. https://doi.org/10.1517/14728222.2014.980235
Menter T, Tzankov A (2018) Mechanisms of immune evasion and immune modulation by lymphoma cells. Front Oncol 8:54. https://doi.org/10.3389/fonc.2018.00054
Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, Kuchroo VK, Sharpe AH (2009) PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med 206(13):3015–3029. https://doi.org/10.1084/jem.20090847
Tivol EA, Borriello F, Schweitzer AN, Lynch WP, Bluestone JA, Sharpe AH (1995) Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity 3(5):541–547
Nishimura H, Okazaki T, Tanaka Y, Nakatani K, Hara M, Matsumori A, Sasayama S, Mizoguchi A, Hiai H, Minato N, Honjo T (2001) Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science 291(5502):319–322. https://doi.org/10.1126/science.291.5502.319
Ok CY, Young KH (2017) Checkpoint inhibitors in hematological malignancies. J Hematol Oncol 10(1):103. https://doi.org/10.1186/s13045-017-0474-3
Twa DD, Chan FC, Ben-Neriah S, Woolcock BW, Mottok A, Tan KL, Slack GW, Gunawardana J, Lim RS, McPherson AW, Kridel R, Telenius A, Scott DW, Savage KJ, Shah SP, Gascoyne RD, Steidl C (2014) Genomic rearrangements involving programmed death ligands are recurrent in primary mediastinal large B-cell lymphoma. Blood 123(13):2062–2065. https://doi.org/10.1182/blood-2013-10-535443
Chapuy B, Roemer MG, Stewart C, Tan Y, Abo RP, Zhang L, Dunford AJ, Meredith DM, Thorner AR, Jordanova ES, Liu G, Feuerhake F, Ducar MD, Illerhaus G, Gusenleitner D, Linden EA, Sun HH, Homer et al (2016) Targetable genetic features of primary testicular and primary central nervous system lymphomas. Blood 127(7):869–881. https://doi.org/10.1182/blood-2015-10-673236
Choi JW, Kim Y, Lee JH, Kim YS (2013) MYD88 expression and L265P mutation in diffuse large B-cell lymphoma. Hum Pathol 44(7):1375–1381. https://doi.org/10.1016/j.humpath.2012.10.026
Green MR, Rodig S, Juszczynski P, Ouyang J, Sinha P, O'Donnell E, Neuberg D, Shipp MA (2012) Constitutive AP-1 activity and EBV infection induce PD-L1 in Hodgkin lymphomas and posttransplant lymphoproliferative disorders: implications for targeted therapy. Clin Cancer Res 18(6):1611–1618. https://doi.org/10.1158/1078-0432.CCR-11-1942
Bi XW, Wang H, Zhang WW, Wang JH, Liu WJ, Xia ZJ, Huang HQ, Jiang WQ, Zhang YJ, Wang L (2016) PD-L1 is upregulated by EBV-driven LMP1 through NF-kappaB pathway and correlates with poor prognosis in natural killer/T-cell lymphoma. J Hematol Oncol 9(1):109. https://doi.org/10.1186/s13045-016-0341-7
Marzec M, Zhang Q, Goradia A, Raghunath PN, Liu X, Paessler M, Wang HY, Wysocka M, Cheng M, Ruggeri BA, Wasik MA (2008) Oncogenic kinase NPM/ALK induces through STAT3 expression of immunosuppressive protein CD274 (PD-L1, B7-H1). Proc Natl Acad Sci U S A 105(52):20852–20857. https://doi.org/10.1073/pnas.0810958105
Chikuma S, Kanamori M, Mise-Omata S, Yoshimura A (2017) Suppressors of cytokine signaling: potential immune checkpoint molecules for cancer immunotherapy. Cancer Sci 108(4):574–580. https://doi.org/10.1111/cas.13194
Gascoyne RD, Rosenwald A, Poppema S, Lenz G (2010) Prognostic biomarkers in malignant lymphomas. Leuk Lymphoma 51(Suppl 1):11–19. https://doi.org/10.3109/10428194.2010.500046
Carbone A, Gloghini A (2013) Relationships between lymphomas linked to hepatitis C virus infection and their microenvironment. World J Gastroenterol 19(44):7874–7879. https://doi.org/10.3748/wjg.v19.i44.7874
Chen BJ, Chapuy B, Ouyang J, Sun HH, Roemer MG, Xu ML, Yu H, Fletcher CD, Freeman GJ, Shipp MA, Rodig SJ (2013) PD-L1 expression is characteristic of a subset of aggressive B-cell lymphomas and virus-associated malignancies. Clin Cancer Res 19(13):3462–3473. https://doi.org/10.1158/1078-0432.CCR-13-0855
Kiyasu J, Miyoshi H, Hirata A, Arakawa F, Ichikawa A, Niino D, Sugita Y, Yufu Y, Choi I, Abe Y, Uike N, Nagafuji K, Okamura T, Akashi K, Takayanagi R, Shiratsuchi M, Ohshima K (2015) Expression of programmed cell death ligand 1 is associated with poor overall survival in patients with diffuse large B-cell lymphoma. Blood 126(19):2193–2201. https://doi.org/10.1182/blood-2015-02-629600
Brusa D, Serra S, Coscia M, Rossi D, D'Arena G, Laurenti L, Jaksic O, Fedele G, Inghirami G, Gaidano G, Malavasi F, Deaglio S (2013) The PD-1/PD-L1 axis contributes to T-cell dysfunction in chronic lymphocytic leukemia. Haematologica 98(6):953–963. https://doi.org/10.3324/haematol.2012.077537
Muenst S, Hoeller S, Willi N, Dirnhofera S, Tzankov A (2010) Diagnostic and prognostic utility of PD-1 in B cell lymphomas. Dis Markers 29(1):47–53. https://doi.org/10.3233/DMA-2010-0725
Muenst S, Hoeller S, Dirnhofer S, Tzankov A (2009) Increased programmed death-1+ tumor-infiltrating lymphocytes in classical Hodgkin lymphoma substantiate reduced overall survival. Hum Pathol 40(12):1715–1722. https://doi.org/10.1016/j.humpath.2009.03.025
Goodman A, Patel SP, Kurzrock R (2017) PD-1-PD-L1 immune-checkpoint blockade in B-cell lymphomas. Nat Rev Clin Oncol 14(4):203–220. https://doi.org/10.1038/nrclinonc.2016.168
Shi M, Roemer MG, Chapuy B, Liao X, Sun H, Pinkus GS, Shipp MA, Freeman GJ, Rodig SJ (2014) Expression of programmed cell death 1 ligand 2 (PD-L2) is a distinguishing feature of primary mediastinal (thymic) large B-cell lymphoma and associated with PDCD1LG2 copy gain. Am J Surg Pathol 38(12):1715–1723. https://doi.org/10.1097/PAS.0000000000000297
Wang Y, Wu L, Tian C, Zhang Y (2018) PD-1-PD-L1 immune-checkpoint blockade in malignant lymphomas. Ann Hematol 97(2):229–237. https://doi.org/10.1007/s00277-017-3176-6
Merryman RW, Armand P, Wright KT, Rodig SJ (2017) Checkpoint blockade in Hodgkin and non-Hodgkin lymphoma. Blood Adv 1(26):2643–2654. https://doi.org/10.1182/bloodadvances.2017012534
Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, Schuster SJ, Millenson MM, Cattry D, Freeman GJ, Rodig SJ, Chapuy B, Ligon AH, Zhu L, Grosso JF, Kim SY, Timmerman JM, Shipp MA, Armand P (2015) PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N Engl J Med 372(4):311–319. https://doi.org/10.1056/NEJMoa1411087
Armand P, Shipp MA, Ribrag V, Michot JM, Zinzani PL, Kuruvilla J, Snyder ES, Ricart AD, Balakumaran A, Rose S, Moskowitz CH (2016) Programmed Death-1 blockade with Pembrolizumab in patients with classical Hodgkin lymphoma after brentuximab vedotin failure. J Clin Oncol 34(31):3733–3739. https://doi.org/10.1200/JCO.2016.67.3467
Chen R, Zinzani PL, Fanale MA, Armand P, Johnson NA, Brice P, Radford J, Ribrag V, Molin D, Vassilakopoulos TP, Tomita A, von Tresckow B, Shipp MA, Zhang Y, Ricart AD, Balakumaran A, Moskowitz CH, Keynote (2017) Phase II study of the efficacy and safety of pembrolizumab for relapsed/refractory classic Hodgkin lymphoma. J Clin Oncol 35(19):2125–2132. https://doi.org/10.1200/JCO.2016.72.1316
Herrera AF, Moskowitz AJ, Bartlett NL, Vose JM, Ramchandren R, Feldman TA, LaCasce AS, Ansell SM, Moskowitz CH, Fenton K, Ogden CA, Taft D, Zhang Q, Kato K, Campbell M, Advani RH (2017) Interim results of brentuximab vedotin in combination with nivolumab in patients with relapsed or refractory Hodgkin lymphoma. Blood 131:1183–1194. https://doi.org/10.1182/blood-2017-10-811224
Bracci L, Schiavoni G, Sistigu A, Belardelli F (2014) Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ 21(1):15–25. https://doi.org/10.1038/cdd.2013.67
Zinzani PL, Ribrag V, Moskowitz CH, Michot JM, Kuruvilla J, Balakumaran A, Zhang Y, Chlosta S, Shipp MA, Armand P (2017) Safety and tolerability of pembrolizumab in patients with relapsed/refractory primary mediastinal large B-cell lymphoma. Blood 130(3):267–270. https://doi.org/10.1182/blood-2016-12-758383
Lesokhin AM, Ansell SM, Armand P, Scott EC, Halwani A, Gutierrez M, Millenson MM, Cohen AD, Schuster SJ, Lebovic D, Dhodapkar M, Avigan D, Chapuy B, Ligon AH, Freeman GJ, Rodig SJ, Cattry D, Zhu L, Grosso JF, Bradley Garelik MB, Shipp MA, Borrello I, Timmerman J (2016) Nivolumab in patients with relapsed or refractory hematologic malignancy: preliminary results of a phase Ib study. J Clin Oncol 34(23):2698–2704. https://doi.org/10.1200/JCO.2015.65.9789
Westin JR, Chu F, Zhang M, Fayad LE, Kwak LW, Fowler N, Romaguera J, Hagemeister F, Fanale M, Samaniego F, Feng L, Baladandayuthapani V, Wang Z, Ma W, Gao Y, Wallace M, Vence LM, Radvanyi L, Muzzafar T, Rotem-Yehudar R, Davis RE, Neelapu SS (2014) Safety and activity of PD1 blockade by pidilizumab in combination with rituximab in patients with relapsed follicular lymphoma: a single group, open-label, phase 2 trial. Lancet Oncol 15(1):69–77. https://doi.org/10.1016/S1470-2045(13)70551-5
Nayak L, Iwamoto FM, LaCasce A, Mukundan S, Roemer MGM, Chapuy B, Armand P, Rodig SJ, Shipp MA (2017) PD-1 blockade with nivolumab in relapsed/refractory primary central nervous system and testicular lymphoma. Blood 129(23):3071–3073. https://doi.org/10.1182/blood-2017-01-764209
Chan TSY, Li J, Loong F, Khong PL, Tse E, Kwong YL (2017) PD1 blockade with low-dose nivolumab in NK/T cell lymphoma failing L-asparaginase: efficacy and safety. Ann Hematol 97:193–196. https://doi.org/10.1007/s00277-017-3127-2
Xing W, Dresser K, Zhang R, Evens AM, Yu H, Woda BA, Chen BJ (2016) PD-L1 expression in EBV-negative diffuse large B-cell lymphoma: clinicopathologic features and prognostic implications. Oncotarget 7(37):59976–59986. https://doi.org/10.18632/oncotarget.11045
Vranic S, Ghosh N, Kimbrough J, Bilalovic N, Bender R, Arguello D, Veloso Y, Dizdarevic A, Gatalica Z (2016) PD-L1 status in refractory lymphomas. PLoS One 11(11):e0166266. https://doi.org/10.1371/journal.pone.0166266
Mino-Kenudson M (2017) Immunohistochemistry for predictive biomarkers in non-small cell lung cancer. Transl Lung Cancer Res 6(5):570–587. https://doi.org/10.21037/tlcr.2017.07.06
Tsao MS, Kerr KM, Kockx M, Beasley MB, Borczuk AC, Botling J, Bubendorf L, Chirieac L, Chen G, Chou TY, Chung JH, Dacic S, Lantuejoul S, Mino-Kenudson M, Moreira AL, Nicholson AG, Noguchi M, Pelosi G, Poleri C, Russell PA, Sauter J, Thunnissen E, Wistuba I, Yu H, Wynes MW, Pintilie M, Yatabe Y, Hirsch FR (2018) PD-L1 immunohistochemistry comparability study in real-life clinical samples: results of blueprint phase 2 project. J Thorac Oncol. https://doi.org/10.1016/j.jtho.2018.05.013
Shi S, Calhoun HC, Xia F, Li J, Le L, Li WX (2006) JAK signaling globally counteracts heterochromatic gene silencing. Nat Genet 38(9):1071–1076. https://doi.org/10.1038/ng1860
Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, Tichelli A, Cazzola M, Skoda RC (2005) A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 352(17):1779–1790. https://doi.org/10.1056/NEJMoa051113
Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, Futreal PA, Erber WN, McMullin MF, Harrison CN, Warren AJ, Gilliland DG, Lodish HF, Green AR (2007) JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 356(5):459–468. https://doi.org/10.1056/NEJMoa065202
Scott LM (2013) Lymphoid malignancies: another face to the Janus kinases. Blood Rev 27(2):63–70. https://doi.org/10.1016/j.blre.2012.12.004
Wu D, Dutra B, Lindeman N, Takahashi H, Takeyama K, Harris NL, Pinkus GS, Longtine J, Shipp M, Kutok JL (2009) No evidence for the JAK2 (V617F) or JAK2 exon 12 mutations in primary mediastinal large B-cell lymphoma. Diagn Mol Pathol 18(3):144–149. https://doi.org/10.1097/PDM.0b013e3181855c7f
Cornejo MG, Kharas MG, Werneck MB, Le Bras S, Moore SA, Ball B, Beylot-Barry M, Rodig SJ, Aster JC, Lee BH, Cantor H, Merlio JP, Gilliland DG, Mercher T (2009) Constitutive JAK3 activation induces lymphoproliferative syndromes in murine bone marrow transplantation models. Blood 113(12):2746–2754. https://doi.org/10.1182/blood-2008-06-164368
Ehrentraut S, Nagel S, Scherr ME, Schneider B, Quentmeier H, Geffers R, Kaufmann M, Meyer C, Prochorec-Sobieszek M, Ketterling RP, Knudson RA, Feldman AL, Kadin ME, Drexler HG, MacLeod RA (2013) T(8;9)(p22;p24)/PCM1-JAK2 activates SOCS2 and SOCS3 via STAT5. PLoS One 8(1):e53767. https://doi.org/10.1371/journal.pone.0053767
Prestipino A, Emhardt AJ, Aumann K, O'Sullivan D, Gorantla SP, Duquesne S, Melchinger W, Braun L, Vuckovic S, Boerries M, Busch H, Halbach S, Pennisi S, Poggio T, Apostolova P, Veratti P, Hettich M et al (2018) Oncogenic JAK2(V617F) causes PD-L1 expression, mediating immune escape in myeloproliferative neoplasms. Sci Transl Med 10(429):eaam7729. https://doi.org/10.1126/scitranslmed.aam7729
Mottok A, Renne C, Willenbrock K, Hansmann ML, Brauninger A (2007) Somatic hypermutation of SOCS1 in lymphocyte-predominant Hodgkin lymphoma is accompanied by high JAK2 expression and activation of STAT6. Blood 110(9):3387–3390. https://doi.org/10.1182/blood-2007-03-082511
Mottok A, Renne C, Seifert M, Oppermann E, Bechstein W, Hansmann ML, Kuppers R, Brauninger A (2009) Inactivating SOCS1 mutations are caused by aberrant somatic hypermutation and restricted to a subset of B-cell lymphoma entities. Blood 114(20):4503–4506. https://doi.org/10.1182/blood-2009-06-225839
Gunawardana J, Chan FC, Telenius A, Woolcock B, Kridel R, Tan KL, Ben-Neriah S, Mottok A, Lim RS, Boyle M, Rogic S, Rimsza LM, Guiter C, Leroy K, Gaulard P, Haioun C, Marra MA, Savage KJ, Connors JM, Shah SP, Gascoyne RD, Steidl C (2014) Recurrent somatic mutations of PTPN1 in primary mediastinal B cell lymphoma and Hodgkin lymphoma. Nat Genet 46(4):329–335. https://doi.org/10.1038/ng.2900
Couronne L, Scourzic L, Pilati C, Della Valle V, Duffourd Y, Solary E, Vainchenker W, Merlio JP, Beylot-Barry M, Damm F, Stern MH, Gaulard P, Lamant L, Delabesse E, Merle-Beral H, Nguyen-Khac F, Fontenay M, Tilly H, Bastard C, Zucman-Rossi J, Bernard OA, Mercher T (2013) STAT3 mutations identified in human hematologic neoplasms induce myeloid malignancies in a mouse bone marrow transplantation model. Haematologica 98(11):1748–1752. https://doi.org/10.3324/haematol.2013.085068
Ritz O, Guiter C, Castellano F, Dorsch K, Melzner J, Jais JP, Dubois G, Gaulard P, Moller P, Leroy K (2009) Recurrent mutations of the STAT6 DNA binding domain in primary mediastinal B-cell lymphoma. Blood 114(6):1236–1242. https://doi.org/10.1182/blood-2009-03-209759
Ngo VN, Young RM, Schmitz R, Jhavar S, Xiao W, Lim KH, Kohlhammer H, Xu W, Yang Y, Zhao H, Shaffer AL, Romesser P, Wright G, Powell J, Rosenwald A, Muller-Hermelink HK, Ott G, Gascoyne RD, Connors JM, Rimsza LM, Campo E, Jaffe ES, Delabie J, Smeland EB, Fisher RI, Braziel RM, Tubbs RR, Cook JR, Weisenburger DD, Chan WC, Staudt LM (2011) Oncogenically active MYD88 mutations in human lymphoma. Nature 470(7332):115–119. https://doi.org/10.1038/nature09671
Odejide O, Weigert O, Lane AA, Toscano D, Lunning MA, Kopp N, Kim S, van Bodegom D, Bolla S, Schatz JH, Teruya-Feldstein J, Hochberg E, Louissaint A, Dorfman D, Stevenson K, Rodig SJ, Piccaluga PP, Jacobsen E, Pileri SA, Harris NL, Ferrero S, Inghirami G, Horwitz SM, Weinstock DM (2014) A targeted mutational landscape of angioimmunoblastic T-cell lymphoma. Blood 123(9):1293–1296. https://doi.org/10.1182/blood-2013-10-531509
Roncero AM, Lopez-Nieva P, Cobos-Fernandez MA, Villa-Morales M, Gonzalez-Sanchez L, Lopez-Lorenzo JL, Llamas P, Ayuso C, Rodriguez-Pinilla SM, Arriba MC, Piris MA, Fernandez-Navarro P, Fernandez AF, Fraga MF, Santos J, Fernandez-Piqueras J (2016) Contribution of JAK2 mutations to T-cell lymphoblastic lymphoma development. Leukemia 30(1):94–103. https://doi.org/10.1038/leu.2015.202
Gerlach MM, Arranto C, Dirnhofer S, Tzankov A (2018) Localized pain-causing JAK2-V617F-positive myeloproliferation with normal peripheral blood values. Ann Hematol. https://doi.org/10.1007/s00277-018-3363-0
Aboudola S, Murugesan G, Szpurka H, Ramsingh G, Zhao X, Prescott N, Tubbs RR, Maciejewski JP, Hsi ED (2007) Bone marrow phospho-STAT5 expression in non-CML chronic myeloproliferative disorders correlates with JAK2 V617F mutation and provides evidence of in vivo JAK2 activation. Am J Surg Pathol 31(2):233–239. https://doi.org/10.1097/01.pas.0000213338.25111.d3
Van den Neste E, Andre M, Gastinne T, Stamatoullas A, Haioun C, Belhabri A, Reman O, Casasnovas O, Guesquieres H, Verhoef G, Claessen MJ, Poirel HA, Copin MC, Dubois R, Vandenberghe P, Stoian IA, Cottereau AS, Bailly S, Knoops L, Morschhauser F (2018) Phase II study of oral JAK1/JAK2 inhibitor ruxolitinib in advanced relapsed/refractory Hodgkin lymphoma. Haematologica 103:840–848. https://doi.org/10.3324/haematol.2017.180554
Allis CD, Jenuwein T (2016) The molecular hallmarks of epigenetic control. Nat Rev Genet 17(8):487–500. https://doi.org/10.1038/nrg.2016.59
Cloos PA, Christensen J, Agger K, Maiolica A, Rappsilber J, Antal T, Hansen KH, Helin K (2006) The putative oncogene GASC1 demethylates tri- and dimethylated lysine 9 on histone H3. Nature 442(7100):307–311. https://doi.org/10.1038/nature04837
Morin RD, Mendez-Lago M, Mungall AJ, Goya R, Mungall KL, Corbett RD, Johnson NA, Severson TM, Chiu R, Field M, Jackman S, Krzywinski M, Scott DW, Trinh DL, Tamura-Wells J, Li S, Firme MR, Rogic S, Griffith M, Chan S, Yakovenko O, Meyer IM, Zhao EY, Smailus D, Moksa M, Chittaranjan S, Rimsza L, Brooks-Wilson A, Spinelli JJ, Ben-Neriah S, Meissner B, Woolcock B, Boyle M, McDonald H, Tam A, Zhao Y, Delaney A, Zeng T, Tse K, Butterfield Y, Birol I, Holt R, Schein J, Horsman DE, Moore R, Jones SJM, Connors JM, Hirst M, Gascoyne RD, Marra MA (2011) Frequent mutation of histone-modifying genes in non-Hodgkin lymphoma. Nature 476(7360):298–303. https://doi.org/10.1038/nature10351
Min DJ, Licht JD (2010) Partners in crime: genes within an amplicon collude to globally deregulate chromatin in lymphoma. Cancer Cell 18(6):539–541. https://doi.org/10.1016/j.ccr.2010.11.032
Kuhnl A, Cunningham D, Chau I (2017) Beyond genomics - targeting the epigenome in diffuse large B-cell lymphoma. Cancer Treat Rev 59:132–137. https://doi.org/10.1016/j.ctrv.2017.07.009
Zhang WC, Shyh-Chang N, Yang H, Rai A, Umashankar S, Ma S, Soh BS, Sun LL, Tai BC, Nga ME, Bhakoo KK, Jayapal SR, Nichane M, Yu Q, Ahmed DA, Tan C, Sing WP, Tam J, Thirugananam A, Noghabi MS, Pang YH, Ang HS, Mitchell W, Robson P, Kaldis P, Soo RA, Swarup S, Lim EH, Lim B (2012) Glycine decarboxylase activity drives non-small cell lung cancer tumor-initiating cells and tumorigenesis. Cell 148(1–2):259–272. https://doi.org/10.1016/j.cell.2011.11.050
Li X, Cui C, Guo Y, Yang G (2015) Glycine decarboxylase expression increased in p53-mutated B cell lymphoma mice. Oncol Res Treat 38(11):586–589. https://doi.org/10.1159/000441595
Zhang MS, Arnaoutov A, Dasso M (2014) RanBP1 governs spindle assembly by defining mitotic ran-GTP production. Dev Cell 31(4):393–404. https://doi.org/10.1016/j.devcel.2014.10.014
Contributions
Both authors conceived and wrote the manuscript. Both authors gave final approval for publication. AT takes full responsibility for the work as a whole, including the study design, access to data, and the decision to submit and publish the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Menter, T., Tzankov, A. Genetic alterations of 9p24 in lymphomas and their impact for cancer (immuno-)therapy. Virchows Arch 474, 497–509 (2019). https://doi.org/10.1007/s00428-018-2438-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-018-2438-6