Abstract
The purposes of this study are to evaluate the adequacy of pathologic lymph node (LN) staging in radical cystectomy specimens from patients with urothelial carcinoma of the bladder and to analyze the frequency of LN metastases among different anatomic regions. All radical cystectomies performed for primary urothelial bladder cancer over a 5-year period (January 2007–September 2012) at a single institution were reviewed. Particular attention was paid to the total number of LNs examined, the number and location of LNs with metastases (positive LNs), and the presence or absence of extranodal tumor extension and/or lymphovascular invasion in the cystectomy specimen. Results and data were analyzed with Origin 6.0 and Microsoft Office Excel 2007 software. A total of 248 radical cystectomies with 8,432 LNs were reviewed. A total of 60 (24 %) cases, with 274 positive LNs out of the 1,982 total (13.8 %), were identified with a male to female ratio of 6.5:1 (52 male, 8 female patients). The average number of LNs examined in each case was 33.0 ± 20.9 (range 5–112). The average number of positive LNs identified in each case was 4.5 ± 4.8 (range 1–26). Among all of the LNs, the hypogastric/obturator (internal iliac) LNs were the most commonly submitted (35.2 %) and also yielded the highest number of positive LNs (46.0 %). On average, for cases staged pN1 and pN2, there was one positive LN per 17.8 and 8.9 LNs examined from the primary drainage LNs, respectively. For pN3 cases, one out of 4.4 secondary drainage LNs was found to be positive. Similarly, one out of 4.0 distant LNs was found to be positive in cases with pM1 staging. Our study suggests that, on average, 23 LNs (including 18 primary drainage LNs and five secondary drainage LNs) should be submitted for optimal pN staging. For adequate pM1 staging, an average of four distal LNs should be evaluated. In total, an average of 27 LNs (23 for pN staging and 4 for pM staging) should be examined in radical cystectomy specimens. We also propose to stratify the number of positive LNs according to the drainage area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presence of lymph node (LN) metastases is critical for tumor staging and prediction of disease recurrence after radical cystectomy in patients with urothelial carcinoma of the bladder. The extent of pelvic lymphadenectomy during radical cystectomy has been shown to affect the accuracy of TNM staging as well as disease prognosis [1, 2]. In the literature, the nomenclature of LN dissection has been variable and is defined differently by urologists. Dangle et al. divided LN dissection into four groups categorized as follows: (1) limited lymphadenectomy (LLN, removal of the external iliac and obturator lymph nodes); (2) standard lymphadenectomy (SLN, i.e., LLN plus removal of the internal iliac lymph nodes); (3) extended lymphadenectomy (ELN, i.e., SLN plus removal of the common iliac and presacral lymph nodes) (Fig. 1a); and (4) super-extended lymphadenectomy (SELN, i.e., ELN plus removal of any additional lymph nodes above the aortic bifurcation) [3] (Fig. 1b). Dhar et al. demonstrated that the average number of LN removed during ELN is significantly higher than LLN (22 vs. 12) [3, 4]. Dangle et al. further reported that ELN identified all node-positive cases and correctly assigned the pN stage [5]. Besides the anatomical extent of dissection, the total lymph node count is also influenced by the manner of LN submission, i.e., as separate packets or en bloc. According to a report by Bochner et al., submitting LNs in separate anatomic packets increased the total LN count from 21 to 40 when compared to en bloc submission within the same template [6].
The concept of lymph node density (LND) was first introduced in 2003 [7, 8]. It is defined as the number of tumor-positive LNs divided by the total number of LNs examined. LND, as well as extra nodal extension (ENE), are strong predictors of a clinical outcome in patients with a node-positive bladder cancer treated by cystectomy. LND has been a valuable tool for stratifying node-positive patients into different risk groups based on expected survival [9]. It has also been postulated that the current tumor, nodes, metastasis (TNM) classification could be improved by the inclusion of these additional parameters (LND and ENE), which, in turn, would allow a better prognostic classification of a node-positive bladder cancer after radical cystectomy [10, 11].
A meticulous lymphadenectomy not only provides the most accurate staging information but may also be therapeutic for some patients with a low-volume nodal involvement [12–14].
In contrast to cancers of other organ systems (such as colorectal carcinoma, gastric, or breast cancer), there is no consensus regarding the requirement for the minimum number of LNs submitted for pathologic evaluation. Proposals for the required minimum number of LNs examined, and considered optimal for accurate pN staging and improved outcome, vary widely and range from 10 to 27 LNs [5, 15]. One multi-center study showed that the removal of 25 LNs resulted in a 75 % probability of finding one or several that were positive, while 45 LNs were needed to achieve a 90 % probability [16]. The most recent study, in which 12 international academic centers participated, showed that the probability of missing one positive LN is 13 % if 25 LNs are examined [17]. One study indicated that no minimum number of LNs is sufficient for optimizing bladder cancer outcomes when a limited or extended pelvic LN dissection is performed during radical cystectomy. Instead, the probability of survival continues to rise as the number of LNs removed increases [18]. Similarly, by using a cadaveric model, Davies et al. demonstrated the limited utility of LN count as a surrogate for the extent of dissection and illustrated the challenges associated with implementing a surgical standard for minimum LN counts [19]. Thus far, there have been no publications detailing requirements for the minimum number of LNs to be removed from different mapping areas in order to achieve accurate staging. According to the 7th edition of the AJCC Cancer Staging Manual, pN1and pN2 should be assigned when positive LNs are only confined to the primary drainage areas, which include hypogastric, obturator, internal/external iliac, perivesical pelvic, sacral, and presacral LNs. To warrant the assignment of the pN3 stage, metastasis should be found in secondary drainage LNs, i.e., common iliac LNs. LNs above the aortic bifurcation (including periaortic and paracaval LNs) are retroperitoneal LNs and are therefore categorized as distant LNs. Cases with any positive distant LNs should be staged as pM1 [20]. Our aim was to evaluate the effectiveness of the submission of LNs from different drainage areas for accurate pN staging. We also sought to address the issue of what should be considered the standard for adequate pathologic LN staging in bladder carcinoma.
Material and methods
A retrospective cohort study was performed on patients with urothelial carcinoma of the urinary bladder who underwent radical cystectomy or cystoprostatectomy at our institution from January 2007 to September 2012. The study was approved by the Institutional Review Board for the Protection of Human Subjects. Clinical and pathologic information was reviewed for all of these patients. Cases with pelvic LNs submitted in separate packets were included in the study. Packet LNs from different drainage areas and levels were collected in different containers by urologists during the cystectomy procedure, including periaortic, paracaval, common iliac, external iliac, obturator/hypogastric, presacral, presciatic, and Cloquet’s LN etc. All LN packets were carefully examined for the presence of LNs. All palpated LNs were submitted in their entirety. The remaining fibroadipose tissue was also either entirely or representatively submitted for microscopic LN examination. Cases with LNs collected “en bloc” were excluded. Tumors were staged (pTNM staging) according to the 7th edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual [20]. Regional LNs used for pN staging included primary and secondary drainage LNs as defined by the AJCC. Thus, primary drainage LNs include hypogastric/obturator, external iliac, perivesical , sacral, and presacral LNs. Urologists in our institution also submit LNs of Cloquet in packets which are included as primary drainage LNs. Secondary drainage LNs include common iliac LNs. LNs taken from above the aortic bifurcation, including periaortic LNs and paracaval LNs, are lower retroperitoneal LNs and should be considered distant LNs. The total number of LNs and the number of positive LNs were recorded, as well as their size and location, extranodal extension, lymph node density, the presence or absence of lymphovascular invasion within the primary tumor, pT stage, and tumor size. Categorical covariates were assessed using the one-way ANOVA and chi-square test of proportions. A p value <0.05 was set for statistical significance. All data was examined using Origin 6.0 (OriginLab Corporation, Northampton, MA), and composite graphs were constructed using Origin 6.0 and Microsoft Office Excel 2007 (Microsoft Corporate Office Headquarters, Redmond, WA).
Results
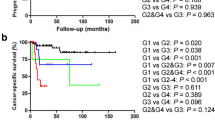
A total of 248 radical cystectomies, yielding 8,432 LNs, which were performed between January 2007 and September 2012, were identified in our electronic medical record system. Positive LNs were recovered in 62 cases. There were 210 cases with urothelial carcinoma (UC) not otherwise specified (NOS), 27 cases with variants (UC with squamous, micropapillary, glandular, mucinous, or sarcomatoid differentiation), and 11 cases with non-urothelial primary malignancies. Overall, LN metastases were detected in 45/210 cases of UC NOS (21.4 %) and among 17/38 cases of non-UC NOS (44.7 %). Two cases, where LNs were submitted en bloc, were excluded from subsequent studies. Among a total of 60 cases included in this study, there were 1,982 LNs of which 274 (13.8 %) were positive for metastases. Among these patients, there were 52 males and eight females, resulting in a male to female ratio of 6.5:1. The average age of patients with positive LNs was 68.2 years old (range 24 to 86 years), which was similar to patients without LN metastases who were, on average, 67.2 years old (range 30 to 88 years). The average number of LNs examined in each case was 33.0 ± 20.9 (range 5–112) with sizes ranging from 0.2 to 5.2 cm. We further stratified the number of LNs submitted for examination according to the pN and pM stages. The results showed that, in general, patients with a higher pN/pM stage correlated with a higher number of LNs examined (Fig. 2). Thus, in cases with stages pN3 and pM1, more extensive LN dissection procedures (i.e., ELN, SELN) were necessary to evaluate secondary drainage and distal LNs. The average number of positive LNs identified in each case was 4.5 ± 4.8 (range 1–26). The smallest positive LN was 0.3 cm, while the largest was 5.0 cm.
Among all LNs, the most commonly submitted were hypogastric/obturator (35.2 %), common iliac (19.9 %), and external iliac (19.6 %). Among all positive LNs identified, the highest percentage derived from hypogastric/obturator (46.0 %), followed by external iliac (20.8 %) and common iliac (20.1 %) (Fig. 3). The yield of positive LNs from each drainage area was also analyzed. For primary drainage LNs, 119/684 (17.4 %) hypogastric/obturator LNs, 57/394 (14.5 %) external iliac LNs, 12/125 (9.6 %) presiatic LNs, 2/49 (4.1 %) presacral LNs, and 1/101 (1.0 %) Cloquet LNs were positive. Among secondary drainage LNs, i.e., common iliac LNs, 55/389 (14.1 %) were positive. For distant LNs, 17/95 (17.9 %) periaortic LNs and 6/118 (5.1 %) paracaval LNs were positive.
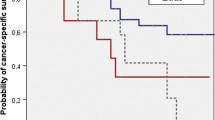
Lymph node density (LND) was analyzed according to pN and pM stages (Fig. 4). The pN1 stage cases had a lower LND compared to those with those with a higher stage (5.61 % in pN1 and 11.21 % in pN2 compared to 22.85 % in pN3, p = 0.003 and 0.035, respectively). Based on the LND, the average number of examined LN corresponding to a yield of one positive LN can be calculated as 1/LND. Thus, on average, for one positive LN in pN1, 17.8 primary drainage LNs were examined, while the corresponding value for pN2 was 8.9. The current (7th) edition of the AJCC Cancer Staging Manual states that pN1 and pN2 represent one, and more than one, positive LN in the primary drainage LNs, respectively. Thus, to identify two or more positive primary drainage LNs among pN2 cases, 8.9 × 2 (i.e., 17.8) LNs from this area should be examined. Our study suggests that, on average, 18 primary drainage LNs should be submitted for pN1 and pN2 staging (18 LNs for pN1, 9 × 2 LNs for pN2). Among pN3 cases, on average, one positive LN was found per 4.4 submitted common iliac LNs. Thus, on average, five common iliac LNs were required for pN3 staging. In our study, an average of 23 LNs, including 18 primary drainage LNs and five secondary drainage (common iliac) LNs, were required for optimal pN staging. Among distant LNs (periaortic, paracaval LNs) staged as M1, one positive LN was found per four examined. Thus, in our study group, on average, 27 LNs were required for the adequate staging of radical cystectomy specimens, including 23 LNs for pN staging and an additional four LNs for pM staging (Fig. 5). The LND was also higher in cases classified as pM1 stage when compared to pM0 (25.03 vs. 15.21 %, respectively, p < 0.001) (Fig. 4).
Among 60 cases with positive LNs, in seven (11.6 %) cases, metastases were found in secondary drainage LNs, with primary drainage LNs being negative; in two (1.7 %) cases, metastases were found in primary drainage and distal LNs, but skipped secondary drainage LNs.
Regarding the relationship between LN dissection and pT staging, 58 cases with positive LNs were staged as follows: pT4 (18), pT3 (30), pT2 (6), pT1 (3), and pTis (1). Two cases were staged as pT0 because there was no residual tumor in the cystectomy specimens (Table 1). Tumors with higher pT stages also showed a higher LN density (14 % for both pT4 and pT3) compared to cases with low pT stages (8 % for pT2 and 6 % for pT1) (p = 0.013 and 0.009, respectively; Table 1). Interestingly, both pT0 and pTis group cases showed a higher LN positive rate (18 and 25 %, respectively). The significance of the data is limited due to the small sample size (one Tis. and two T0). The results show that the pT3 and pT4 groups also had more cases with a higher percentage of pN2 and pN3 staging. However, there was no clear correlation between pT and pM staging (Table 1).
The relationship between lymphovascular invasion and LN positivity was also investigated. Among cases with positive LNs, 56.5 % had evidence of lymphovascular invasion; this is in contrast to 15.5 % (p < 0.001) lymphovascular invasion in cases with negative lymph nodes (Fig. 6).
We further studied the relationship between ENE and pT, including both pN and pM staging. Our data showed that, overall, 57 % (34/60) of cases with positive LN had ENE. Among these, 79.41 % of cases with a high pT stage (pT3 and pT4) had ENE. However, there was no significant difference with regard to high pT staging between the ENE positive and negative groups (79.41 vs. 80.77 %, p = 0.896). Positive ENE did not correlate with either high pN (N3) staging (with ENE = 35.29 % vs. without ENE = 46.15 %, p = 0.395) or distant LN metastasis (M1) (with ENE = 14.71 % vs. without ENE = 11.54 %, p = 0.712) (Table 2).
Discussion
The presence of LN metastases at the time of diagnosis of invasive bladder cancer is not uncommon. In a large cohort of 1,054 patients with urothelial carcinoma of the bladder, treated at a single institution, LN metastases were identified in 246 patients (23 %), most of whom had extravesical tumor extension [21]. An analysis of 4,252 patients, treated at multiple centers, similarly reported that 943 patients (22 %) had LN metastases at radical cystectomy [22]. In a study reported by Dangle et al., 30 % of cases had a positive LN(s) [3]. Our study showed that overall 25 % (62/248) of patients who underwent radical cystectomy for urinary bladder malignancy had a positive LN(s), which is comparable to the above published data. However, the rate of LN positivity was higher among patients with UC variants/non-urothelial malignancy than among patients with UC NOS. Thus, LN metastases were seen in 21.4 % (45/210 cases) of patients with UC NOS in contrast to 44.7 % (17/38 cases) of patients with UC variants/non-urothelial malignancies. However, the small numbers of cases of individual variants precluded a more detailed correlation.
Leadbetter originally described the lymphatic drainage of the bladder from visceral LNs in the bladder wall to the common iliac LNs [23]. Subsequently, Leissner et al. grouped the LNs into three levels: level I —LNs below the common iliac artery; level II—LNs adjacent to the common iliac artery and presacral LNs; level III—LNs above the aortic bifurcation [1]. Currently, LNs are grouped into primary drainage LNs (internal iliac/hypogastric, presiatic, presacral, and external iliac/obturator LNs), secondary drainage LNs (i.e., common iliac LNs), and distant LNs (LNs above the aortic bifurcation). Interestingly, a recent study found that the number of positive LNs (one or two or more) was significantly associated with an increased risk of cancer-specific death, whereas LN location was not an independent predictor of outcome (pN3 compared to pN1 and pN2) [24]. We argue that reporting not only the number of positive LNs but also their location is essential for accurate pN/pM staging.
According to our data, the most common positive regional LNs were within the hypogastric/obturator (17.4 %), external iliac (14.5 %), and common iliac LNs (14.1 %). For distant LNs, 17.9 % of periaortic LNs were positive. These findings are similar to the data published by Leissner, which showed that the obturator lymph nodes were the most common site of metastases (26 %) followed by external iliac (16 %) and obturator/hypogastric (13.2 %), common iliac (19 %), and lymph nodes above the aortic bifurcation (17 %) [1]. Abol-Enein et al., in the same year, presented a similar mapping study of 200 patients that included 48 patients (24 %) with nodal metastases. A total of 388 positive nodes were removed, and the anatomic distribution of metastases, as well as the conclusions arrived at by the authors, were similar to those of the Leissner study [25].
“Lymph node skipping” is defined as LN positivity that is clearly identified in higher levels (secondary drainage or distal) LN(s) without a lower level (primary drainage) involvement. It could be explained by a direct drainage to the common iliac region [26]. Vazina reported 1 of 43 (2.3 %) cases with skipping [26], while Dorin et al. found 7 out of 84 (8.3 %) cases with skip metastasis [27]. In our study, among 60 cases with positive LNs, in 7 (11.6 %) cases, metastases were found in secondary drainage LNs, with primary drainage LNs being negative; in 2 (1.7 %) cases, metastases were found in primary drainage and distal LNs, but skipped secondary drainage LNs.
Among patients who underwent radical cystectomy for bladder cancer, accurate LN staging (pN) and/or LND have been shown to correlate with the prognosis and the incidence of disease recurrence, with LND in particular being a better prognostic factor than the total count of positive LN [28–30]. Stein et al. analyzed 244 patients with a node-positive disease and reported that a LND of less than 20 % was associated with a better recurrence-free survival (5- and 10-year recurrence-free survivals of 44 and 43 %, respectively) when compared with a lymph node density of greater than 20 % (5- and 10-year recurrence-free survivals of 17 %) [8]. Kassouf’s multi-variate analysis of LND demonstrated that an LND >20 %, but not the pN stage or the total number of LN involved by a tumor, was predictive of a decreased disease-specific survival. Therefore, the authors concluded that, in patients with a LN-positive disease after radical cystectomy, LND is superior to pN nodal status in predicting disease-specific survival [31]. In our study, the pM1 group had the highest LND (29.3 %), while the pN3 group closely followed with an LND of 28.5 %. By comparison, the cases that had only primary drainage LN metastases had a lower LND (16.0 %). These results indicate that LND is positively correlated with pN and pM staging. It can be used as an indicator for assessing a patient’s prognosis.
Both studies from Herr et al [7]. and Stein et al [8]. indicated that positive LN with ENE is also a strong predictor of a clinical outcome in bladder cancer patients treated by cystectomy. We studied the relationship between ENE and pathologic staging. However, our data did not show a strong positive association between ENE and high pT (T3, T4), pN (N3), or distant LN metastasis (M1).
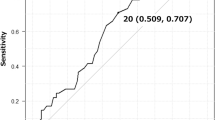
Unlike the situation in colorectal, mammary, and gastric carcinomas, to date, there is no widely accepted recommendation for a “standard LN submission” for radical cystectomy. Several factors, including limited data, complicated LN mapping, and the lack of a sentinel LN, have contributed to this situation. Nevertheless, several attempts have been made to establish such a standard. To this end, Leissner et al. reported that it was necessary to remove 16 LNs at radical cystectomy in order to detect nodal metastases and that this was also associated with improved disease-free and cancer-specific survival [32]. Similarly, Herr et al., based on a retrospective study of 322 patients, confirmed an improved survival for patients with and without nodal metastases when a minimum of nine LNs were removed at radical cystectomy [33]. A study involving 1,698 patients suggested that the removal of 10–14 LNs, regardless of primary tumor stage, resulted in improved oncologic outcomes [15]. Both Herr and Wright also reported that the removal of more than 10 LNs was associated with an improved survival [14, 30]. Capitanio et al. used ROC analyses to explore the relationship between the number of removed and examined LNs and the probability of finding one or more metastatic LN in a pool of 731 patients. The findings suggested that the maximum increase in the probability of finding positive LNs occurred when 15–30 LNs were removed (from 10 to 80 %, respectively). They concluded that removing 25 LNs might represent the lowest threshold for the extent of lymphadenectomy at radical cystectomy [16]. Dangle et al. found that identifying at least 23 to 27 lymph nodes on final pathological evaluation provides a high level of confidence (80 and 90 %, respectively) in the correct staging of a case as node-positive or node-negative [5]. In the latest multi-institution study, which involved 4,335 patients, Shariat et al. tried to achieve adequate staging by computing the nodal staging score (NSS). This score aims to calculate the “true negative pN”, i.e., the probability that a pathologically LN-negative patient is indeed free of nodal disease. Overall, the probability of missing a positive node decreases with the increasing number of nodes examined (52 % if three nodes are examined, 26 % if 10 are examined, and 13 % if 25 are examined). The study also found that the probability of encountering a positive node increased proportionally with advancing pathologic T stage and the presence of lymphovascular invasion (LVI). However, all published data to date have only addressed the issue of the total number of LN that should be examined, without considering their location. Based on our data, we conclude that an average of 23 LNs, including 18 primary drainage LNs and five secondary drainage (common iliac) LNs, should be submitted for optimal pN staging. In addition, four distant LNs should be submitted for pM staging. Thus, overall, a total of 27 LNs is the required minimum for accurate pN and pM staging in radical cystectomy cases.
Although ELN and SELN are necessary for accurate pN and pM staging, it is controversial and undetermined whether ELN is more effective than SLN during surgery. Currently, the Southwest Oncology Group (SWOG) is conducting a prospective phase III surgical trial to evaluate the benefit of a standard vs. extended pelvic lymphadenectomy, performed at the time of radical cystectomy, for muscle-invasive urothelial cancer (ClinicalTrials.gov Identifier: NCT01224665).
Our studies also show that detection of LVI is associated with a higher rate of LN metastases (Fig. 6). In our practice, we routinely comment on LVI whether “not identified, present, or undeterminate” according to the College of American Pathologists (CAP) recommendations for the examination of specimens from patients with carcinoma of the urinary bladder [34]. We also frequently use IHC (stain for CD31 and/or CD34) to detect the presence of lymphatics involved by cancer as recommend by CAP.
Our study is limited by its retrospective design, as well as a number of other factors. These include the following: (1) the lymphadenectomies were not standardized; (2) the extent of LN dissection from each case was dependent on the patient’s clinical stage; (3) other factors such as BMI, previous radiation, previous chemotherapy, etc.; and (4) the patient’s/surgeon’s preferences. Thus, the number of LNs examined is not an exact surrogate for the extent of LN dissection. Thus, there are several factors affecting the true LN count; these include the level of expertise of the surgeon, the person performing the gross examination, and the pathologist performing the microscopic examination. Although this study was conducted at a single institution, with only minor variation in the experience of pathologists and surgeons as compared to a multi-center study, the relative small sample size remains a significant limitation.
Conclusion
Based on our data, we conclude that an average of 23 regional LNs, including 18 from the primary drainage area plus five from the secondary drainage area should be submitted for optimal pN staging. Additionally, on average, four distal LNs should be examined for pM staging. Overall, a total of 27 LNs is ideal for accurate pLN and pM staging in radical cystectomy cases. To the best of our knowledge, this is the first time that the number of LNs was stratified according to their drainage area.
References
Leissner J, Ghoneim MA, Abol-Enein H et al (2004) Extended radical lymphadenectomy in patients with urothelial bladder cancer: results of a prospective multicenter study. J Urol 171(1):139–144
Abaza R, Dangle PP, Gong MC, Bahnson RR, Pohar KS (2012) Quality of lymphadenectomy is equivalent with robotic and open cystectomy using an extended template. J Urol 187(4):1200–1204
Dangle PP, Bahnson RR, Pohar KS (2009) How close are we to establishing standards of lymphadenectomy for invasive bladder cancer? Ther Adv Urol 1(3):167–174
Dhar NB, Klein EA, Reuther AM, Thalmann GN, Madersbacher S, Studer UE (2008) Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. J Urol 179(3):873–878, discussion 878
Dangle PP, Gong MC, Bahnson RR, Pohar KS (2010) How do commonly performed lymphadenectomy templates influence bladder cancer nodal stage? J Urol 183(2):499–503
Bochner BH, Herr HW, Reuter VE (2001) Impact of separate versus en bloc pelvic lymph node dissection on the number of lymph nodes retrieved in cystectomy specimens. J Urol 166(6):2295–2296
Herr HW (2003) Superiority of ratio based lymph node staging for bladder cancer. J Urol 169(3):943–945
Stein JP, Cai J, Groshen S, Skinner DG (2003) Risk factors for patients with pelvic lymph node metastases following radical cystectomy with en bloc pelvic lymphadenectomy: concept of lymph node density. J Urol 170(1):35–41
Lee EK, Herr HW, Dickstein RJ et al (2012) Lymph node density for patient counselling about prognosis and for designing clinical trials of adjuvant therapies after radical cystectomy. BJU Int 110(11 Pt B):E590–E595
Masson-Lecomte A, Vordos D, Hoznek A et al (2013) External validation of extranodal extension and lymph node density as predictors of survival in node-positive bladder cancer after radical cystectomy. Ann Surg Oncol 20(4):1389–1394
Quek ML, Flanigan RC (2009) The role of lymph node density in bladder cancer prognostication. World J Urol 27(1):27–32
Herr HW (2010) Extent of pelvic lymph node dissection during radical cystectomy: where and why! Eur Urol 57(2):212–213
Karl A, Carroll PR, Gschwend JE et al (2009) The impact of lymphadenectomy and lymph node metastasis on the outcomes of radical cystectomy for bladder cancer. Eur Urol 55(4):826–835
Herr HW, Faulkner JR, Grossman HB et al (2004) Surgical factors influence bladder cancer outcomes: a cooperative group report. J Clin Oncol 22(14):2781–2789
Konety BR, Joslyn SA, O’Donnell MA (2003) Extent of pelvic lymphadenectomy and its impact on outcome in patients diagnosed with bladder cancer: analysis of data from the Surveillance, Epidemiology and End Results Program data base. J Urol 169(3):946–950
Capitanio U, Suardi N, Shariat SF et al (2009) Assessing the minimum number of lymph nodes needed at radical cystectomy in patients with bladder cancer. BJU Int 103(10):1359–1362
Shariat SF, Rink M, Ehdaie B et al (2013) Pathologic nodal staging score for bladder cancer: a decision tool for adjuvant therapy after radical cystectomy. Eur Urol 63(2):371–378
Koppie TM, Vickers AJ, Vora K, Dalbagni G, Bochner BH (2006) Standardization of pelvic lymphadenectomy performed at radical cystectomy: can we establish a minimum number of lymph nodes that should be removed? Cancer 107(10):2368–2374
Davies JD, Simons CM, Ruhotina N, Barocas DA, Clark PE, Morgan TM (2013) Anatomic basis for lymph node counts as measure of lymph node dissection extent: a cadaveric study. Urology 81(2):358–363
Edge SBBD, Compton CC, Fritz AG, Greene FL, Trotti A (2010) AJCC Cancer Staging Manual 7th Edition, 7th edn. Springer, Chicago
Stein JP, Lieskovsky G, Cote R et al (2001) Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol 19(3):666–675
Bruins HM, Stein JP (2008) Risk factors and clinical outcomes of patients with node-positive muscle-invasive bladder cancer. Expert Rev Anticancer Ther 8(7):1091–1101
Leadbetter WF, Cooper JF (1950) Regional gland dissection for carcinoma of the bladder; a technique for one-stage cystectomy, gland dissection, and bilateral uretero-enterostomy. J Urol 63(2):242–260
Tarin TV, Power NE, Ehdaie B et al (2012) Lymph node-positive bladder cancer treated with radical cystectomy and lymphadenectomy: effect of the level of node positivity. Eur Urol 61(5):1025–1030
Abol-Enein H, El-Baz M, Abd El-Hameed MA, Abdel-Latif M, Ghoneim MA (2004) Lymph node involvement in patients with bladder cancer treated with radical cystectomy: a patho-anatomical study—a single center experience. J Urol 172(5 Pt 1):1818–1821
Vazina A, Dugi D, Shariat SF, Evans J, Link R, Lerner SP (2004) Stage specific lymph node metastasis mapping in radical cystectomy specimens. J Urol 171(5):1830–1834
Dorin RP, Daneshmand S, Eisenberg MS et al (2011) Lymph node dissection technique is more important than lymph node count in identifying nodal metastases in radical cystectomy patients: a comparative mapping study. Eur Urol 60(5):946–952
Kassouf W, Svatek RS, Shariat SF et al (2013) Critical analysis and validation of lymph node density as prognostic variable in urothelial carcinoma of bladder. Urol Oncol 31(4):480–486
May M, Herrmann E, Bolenz C et al (2011) Lymph node density affects cancer-specific survival in patients with lymph node-positive urothelial bladder cancer following radical cystectomy. Eur Urol 59(5):712–718
Wright JL, Lin DW, Porter MP (2008) The association between extent of lymphadenectomy and survival among patients with lymph node metastases undergoing radical cystectomy. Cancer 112(11):2401–2408
Kassouf W, Agarwal PK, Herr HW et al (2008) Lymph node density is superior to TNM nodal status in predicting disease-specific survival after radical cystectomy for bladder cancer: analysis of pooled data from MDACC and MSKCC. J Clin Oncol 26(1):121–126
Leissner J, Hohenfellner R, Thuroff JW, Wolf HK (2000) Lymphadenectomy in patients with transitional cell carcinoma of the urinary bladder; significance for staging and prognosis. BJU Int 85(7):817–823
Herr HW, Bochner BH, Dalbagni G, Donat SM, Reuter VE, Bajorin DF (2002) Impact of the number of lymph nodes retrieved on outcome in patients with muscle invasive bladder cancer. J Urol 167(3):1295–1298
CAP Cancer Protocols and Checklists: Protocol for the examination of specimens from patients with carcinoma of the urinary bladder. College of American Pathologists 2013. http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2013/UrinaryBladder_13protocol_3210.pdf. Accessed Oct. 2013.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, L., Mudaliar, K., Mehta, V. et al. Seeking a standard for adequate pathologic lymph node staging in primary bladder carcinoma. Virchows Arch 464, 595–602 (2014). https://doi.org/10.1007/s00428-014-1575-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-014-1575-9