Abstract
For the past century, autopsy techniques in clinical pathology have not changed significantly, while autopsy rates are declining. Modern imaging techniques offer interesting prospects of supportive post-mortem diagnostic investigation. In a prospective study of 29 autopsy cases, complimentary virtual autopsy using unenhanced post-mortem computed tomography (pmCT) was performed. We analysed in a prospective cohort study 29 unenhanced pmCT scans, generated prior to autopsy. Clinical information regarding clinical history and circumstances of death were provided. The objective of the study was to find consistency and/or discrepancy between virtual autopsy and conventional autopsy findings regarding cause of death and death-related diagnoses, reconstruction of the pathogenetic mechanisms involved, side diagnoses and CPR (cardiopulmonary resuscitation)- or death-related post-mortem changes. Accuracy of pmCT for cause of death was 68 % and the positive predictive value (PPV) was 75 %. Regarding the pathogenetic mechanisms, accuracy of pmCT was 21 % and PPV was 29 %. The combined diagnostic yield of autopsy and pmCT was 133 % compared to autopsy only. Modern imaging techniques give an opportunity for post-mortem diagnostics to complete but not yet replace traditional autopsy. We could show that in two out of three cases, the cause of death found by pmCT matched the diagnosis from classical autopsy. While both disciplines, pathology and radiology, will profit from the mutual exchange of data, it seems a realistic aim to strive for virtual autopsy possibly further supported by biopsies and contrast-enhanced pmCT as an alternative to the classical clinical autopsy. A combination of both methods enhances diagnostic quality and completeness of the autopsy report.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autopsy is an essential tool for student and pathology resident teaching. At the same time, it is a valuable performance measure for any hospital [1]. Autopsy can be of great importance regarding economic and legal consequences for hospitals and clinicians [2]. In the long term, decline in autopsy rates must lead to a lack of accuracy of mortality statistics, on which the financial support of specific research areas are based. In Europe, autopsy rates have been declining [3–6]. In the USA, Australia and Asia, trends are the same [7–9]. Influential factors include request rates by clinicians, laws determining legal autopsy consent, and consent rates [10].
Autopsy methods used by departments of pathology all over the world have not changed much during the past century. Basically, pathologists rely on macroscopic organ morphology and microscopic examination. As diagnostic methods have changed and improved significantly in the field of radiologic imaging, our aim was to find out whether medical autopsy pathology benefits from modern diagnostic imaging.
In forensic medicine, post-mortem imaging has a long tradition. New imaging techniques, such as spiral multislice computed tomography (CT) and magnetic resonance imaging (MRI), offer excellent utilities for post-mortem examination. Forensic research groups in Europe, the UK, USA, Australia and Asia attend to the concept of post-mortem imaging [11–15].
In medical autopsy pathology, post-mortem imaging has not yet been used to an extent comparable to forensic pathology. Our goal was to investigate the potential of unenhanced post-mortem CT (pmCT) imaging for virtual autopsy. Native CT autopsy imaging in comparison to full autopsy, to our knowledge, has only rarely been used in non-forensic settings [16]. Often, MRI is used in combination with pmCT [17–19]. MRI is more time consuming and more expensive than CT, and the availability of MRI scanners is limited. Therefore, a systematic evaluation of the feasibility and accuracy of finding the cause of death with native pmCT in comparison to the results of conventional autopsy was conducted.
The objectives for virtual autopsy were to provide the examiner with sufficient material to report on the following topics:
-
1.
Cause of death
-
2.
Death-related diagnoses
-
3.
Reconstruction of pathogenetic mechanisms involved
-
4.
Unspecific findings (post-mortem changes, changes related to CPR)
-
5.
Side diagnoses
Materials and methods
This study was conducted at a German university hospital. The study was approved by the local ethics committee.
We included in this prospective study 29 randomly selected cases of deceased persons delivered to the Department of Pathology for conventional autopsy. Sex ratio was f/m = 10:19. Mean age at death was 59 years, ranging from 0 months to 91 years. The cases comprised 17 deaths on a standard hospital ward, eight deaths in an intensive care unit, two deaths in the emergency room, one intrauterine death and one death at home. The manner of death was due to natural cause in all cases.
We used the combination of imaging and classical autopsy prospectively whenever feasible, i.e. availability of CT for consented classical autopsies.
Virtual autopsy
Before conventional autopsy, at a mean time of 50 h (±40 h) after death, the body was wrapped (arms attached laterally) in an artefact-free body bag in the supine position, placed in the CT gantry, and scanned from head to toe with a 64 dual-source CT scanner (SOMATOM Definition, Siemens, Forchheim, Germany) with 64 × 0.6 mm collimation, a tube voltage of 120 kV and an effective tube current-time product of 160 mAseff. From raw data, axial images with 5- and 1-mm slice thickness and a recon increment of 4 or 0.7 mm were reconstructed using medium smooth (B30f) and sharp (B60f) convolution kernels. Including positioning of the body on the scanner, the duration of the average pmCT scan was 10 min. After reconstruction of the raw data, the reconstructed images were transferred to a Picture Archiving and Communication System (iSite Radiology, Philips Medical Systems, the Netherlands). The CT scanner was used out of working hours (before 0730 or after 1800 hours).
Afterwards, the pictures were evaluated by two experienced general radiologists with no previous experience of post-mortem imaging. The clinical information given by the autopsy request form was provided to radiologists before image interpretation. The radiologists reported their findings in a standard form, including the neurocranium, thorax, abdomen and extremities.
Conventional autopsy
The autopsy was performed in a standardized form (accredited Department of Pathology, IS0/IEC 17020) by experienced pathologists at a mean time of 62 h (±45 h) after death. All three body cavities (neurocranium, thorax and abdomen) were opened except in two cases. In one case, only cardiac autopsy was consented. In one case of systemic echinococcosis, classical clinical autopsy was omitted due to infection hazard. Following complete autopsy, the autopsy findings were demonstrated to the clinicians requesting the autopsy. The clinical picture was correlated with findings at autopsy.
Statistical analysis
Statistical analysis was conducted using Microsoft® Office Excel 2003 (Microsoft Corporation, Redmond, WA, USA). All cases in which pmCT and autopsy were performed were included in the statistical analysis (n = 28).
Results
The results are structured according to the report about the Swiss Virtopsy® project published in 2003 [20]. The results of pmCT and conventional autopsy were compared with regard to the detection of
-
1.
Cause of death
-
2.
Death-related diagnoses
-
3.
Reconstruction of pathogenetic mechanisms involved
-
4.
Unspecific findings (post-mortem changes, changes related to CPR)
-
5.
Side diagnoses
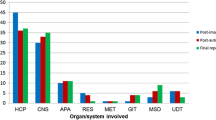
The cause of death was distributed as shown in Table 1, with predominance of diseases of the circulatory system, infectious diseases and diseases of the respiratory system. Summing up the total number of diagnoses found at autopsy in combination with pmCT, 33 % additional diagnoses were found using pmCT (190 at autopsy, 124 with both methods and 103 with pmCT only). Including CPR-related and post-mortem changes, the combined diagnostic yield was 48 % higher than without pmCT (190 at autopsy only, 128 at both autopsy and pmCT, 154 additional diagnoses with pmCT). The distribution in the diagnostic groups is shown in Table 2 and visualized in Fig. 1.
-
1.
Cause of death
The cause of death was assigned to a specific site or pathology, e.g. cardiac failure, cardiorespiratory failure, acute respiratory failure, multi-organ failure or haemorrhage, whenever possible. In one case of intrauterine death, no cause of death could be proved by either method.
In 19 of 28 cases, the cause of death diagnosis after pmCT matched the diagnosis after conventional autopsy (Table 3).
Table 3 Cross-tabulation cause of death in pmCT vs. classical autopsy -
2.
Death-related diagnoses
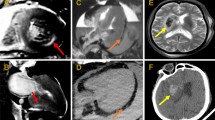
Five-percent more death-relevant diagnoses were found in the combination of classical autopsy and pmCT (122 at autopsy, plus six with pmCT). In a case of multiple myeloma with multiple osteoblastic and osteolytic lesions, the lesions were found with pmCT as well as after macroscopic examination in classical autopsy (Fig. 2).
Fig. 2 a Subarachnoid and intraventricular haemorrhage, visible as hyperdense fluid with pmCT (arrow); b macroscopic view of skull base with haemorrhage; c macroscopic view of brain slice with subarachnoid and intraventricular haemorrhage (arrow, ventricle); d abdominal pmCT with intraabdominal haemorrhage, visible as hyperdense fluid with pmCT (arrow); e Macroscopic view of haematoperitoneum (top, liver; middle right, transverse colon and omentum; down, colon descendens); f hemorrhagic metastasis of chorion carcinoma in liver (arrow, chorion carcinoma cells); g three-dimensional reconstruction of spine and ribs with multiple osteolyses (arrows); h macroscopic view of vertebral bodies with osteolyses (arrows); i microscopic view of plasmocytoma cells in bone marrow
With pmCT, atherosclerosis of cerebral arteries was found in one of five cases with cerebral atherosclerosis in classical autopsy. In one case of fatal subarachnoidal haemorrhage, the haemorrhage was visible with pmCT (Fig. 2). In one case of meningoencephalitis and circumscript subarachnoidal haemorrhage, the haemorrhage was not visible with pmCT. Brain lesions, such as Alzheimer's disease, in two cases and a small haemorrhage were missed with pmCT.
Generalised atherosclerosis with calcification was found in 13 cases with equal results of pmCT and classical autopsy. Coronary sclerosis was identified with pmCT in 16 of 19 cases at classical autopsy. In six cases, in which coronary sclerosis was associated with myocardial infarction and cardiac failure, the cardiac cause of death was diagnosed correctly with regard to characteristic changes of the organs on a balance of probabilities. There were no false-positive findings of coronary sclerosis with pmCT. One basilary artery aneurysm was missed with pmCT, as well as one out of three other aneurysms.
In our patient cohort, thromboses were missed with unenhanced pmCT images in one case of an in-stent thrombosis and two cases of bypass thrombosis.
In our study, out of 12 cases of cardiac failure in clinical autopsy, ten cases were diagnosed correctly by use of pmCT. There were no false-positive findings for cardiac failure. Although myocardial lesions (infarction, myocarditis) were not visible with pmCT, cardiac failure was diagnosed correctly from death-associated diagnoses, such as coronary atherosclerosis, organ congestion and pleural effusions. Myocardial hypertrophy was reported at autopsy in 19 cases, but only in ten cases with pmCT. One left ventricular aneurysm was missed with pmCT.
Ground glass attenuation was diagnosed with pmCT in 12 cases. The pathomorphologic findings in those cases in classical autopsy were acute pulmonary congestion in nine cases, pulmonary oedema in three cases, hyaline membranes and pneumonia in one case, severe bacteremia in one case and bone marrow embolisation in one case. Seven out of nine cases of pulmonary emphysema were missed with pmCT. Mixed dust pneumoconiosis was found with pmCT due to calcified lesions in two cases (100 %).
There were one false-positive, one true-positive and two false-negative diagnoses of pneumonia in pmCT. Pleural effusions were found with pmCT in 19 cases, compared to 18 cases at autopsy. A small pneumothorax was found with pmCT in three cases, which had been missed at autopsy.
Fluid with a density of more than 50 HU in one of the body cavities or preformed spaces (ventricles, pericardium) was found in eight cases with pmCT. The finding correlated with the autopsy finding of haemorrhage in all cases (intraabdominal haemorrhage in five cases, pericardial tamponade in two cases, intraventricular haemorrhage in one case) (Fig. 2). Diffuse haemorrhage, as present in one case, was not visible with pmCT.
-
3.
Reconstruction of the pathogenetic mechanism
The reconstruction of the pathogenetic mechanism using pmCT was correct in 5 of 28 cases, i.e. three cases of intraabdominal haemorrhage, one case of intracranial haemorrhage and one case of pulmonary embolism (Table 4). In one case (intrauterine death), the cause of death and the pathogenetic mechanism remained unclear after both pmCT and classical autopsy. In most cases, the site of death could be assigned to the lung or the heart correctly with pmCT, but the exact cause of organ failure remained unclear. At traditional autopsy, the cause of organ failure could be defined precisely by means of histologic examination and assessment of characteristic macroscopic tissue changes, such as yellow necrosis of myocardial tissue with hemorrhagic margin in case of myocardial infarction. Differing results in the reconstruction of the pathogenetic mechanism were found in a case of severe bacterial infection of the lungs and in cases of cardiac failure due to myocarditis or myocardial infarction with or without pericardial tamponade, as well as chronic ischaemic cardiomyopathy or chronic heart transplant vasculopathy. One case of dilated cardiomyopathy was missed with pmCT, and death was assigned to myocardial hypertrophy. In one case of respiratory distress, the pulmonary oedema was found, but atelectasis had been missed with pmCT, and therefore, the pathogenetic mechanism remained unclear. In one case of COPD, heart failure was correctly found as the cause of death, but the pathogenetic mechanism with right heart failure due to COPD was not reconstructed correctly. In three cases of haemorrhage, haematoperitoneum was found with pmCT, but the exact localisation of the bleeding site was missed. In one case of diffuse bleeding, the haemorrhage was missed with pmCT. Two cases of bronchopneumonia and one case of meningoencephalitis were missed with pmCT. In one case of sepsis after chemotherapy, death was attributed to cardiopulmonary insufficiency, while at autopsy, multi-organ failure was believed to be the cause of death. In one case of respiratory failure, the radiologists suspected air embolism to be the cause of death; therefore, the reconstruction of the pathogenetic mechanism differed from the autopsy result as well.
Table 4 Cross-tabulation Pathogenetic mechanism in pmCT vs. classical autopsy -
4.
Unspecific findings
After the combination of pmCT with classical autopsy, more than ten times more unspecific death-related and CPR-related diagnoses were documented (4 at classical autopsy, 51 additional with pmCT). Cardiopulmonary resuscitation and putrefaction may cause artefacts on pmCT images. Rib fractures are usually examined during classical autopsy but were missed on macroscopic examination in two cases. One case of multiple rib fractures was missed with pmCT. One sternum fracture was found with both methods; one was missed at autopsy.
Gas in the cardiovascular system was found in ten cases with pmCT, associated with CPR before death in seven cases. Aerobilia was described in eight cases with pmCT, as well as six cases of subcutaneous emphysema. None of these findings were documented at clinical autopsy.
-
5.
Side diagnoses
After a combination of side diagnoses found at classical autopsy and additional diagnoses found with pmCT, 35 % additional diagnoses were found (202 at classical autopsy, 70 additional diagnoses with pmCT). With pmCT, hernias were seen in five cases. Traditional autopsy revealed no hernia. Muscle atrophy was found in three cases with pmCT, compared to five cases at autopsy.
Neoplastic lesions were reported by the radiologists; missed at autopsy were one lipoma and two cartilaginous exostoses. On the other hand, at autopsy, one rectum carcinoma, one colon carcinoma, one renal cell carcinoma, one prostate carcinoma, one transitional cell carcinoma and ten cases of low-grade intraepithelial neoplasia of the colon, as well as one pulmonary metastasis of a squamous cell carcinoma, were reported, which were missed with pmCT. Radiologists reported one false-positive “tumour” in the pleural cavity, which at autopsy proved to be coagulated blood.
Calcified lesions, such as cholecystolithiasis, were visible with pmCT in three of five cases at autopsy. Prostate enlargement was diagnosed in two cases with pmCT, compared to three cases at autopsy. Two cases of mixed dust pneumoconiosis were diagnosed with pmCT, in agreement with autopsy findings.
Organ size and configuration as well as hypodense lesions, such as cysts, could be assessed with pmCT. Myocardial hypertrophy was diagnosed with pmCT in 10 of 18 cases at autopsy. Goitre was found with pmCT in one of four cases in conformity with autopsy. Hepatosplenomegaly was found with pmCT in three of four cases at autopsy. Fatty liver was found in one case in agreement with autopsy, as well as liver or kidney cysts in five cases.
Fluid accumulations (anasarca, ascites) were diagnosed in seven cases with pmCT, compared to six cases at autopsy. One small pneumothorax was found with pmCT, which was not visible at autopsy. Thirteen skeletal degenerations and four cases of arthroses, one of herniated vertebral disc, one of a bone cyst and one cartilaginous exostosis, were missed at autopsy.
See complete results online as supplementary material in Supplementary Table 1 (items 1–4) and Supplementary Table 2 (item 5).
Discussion
The basic methods of clinical autopsy technique including macroscopic and microscopic examination have not changed much since Virchow's time. We discuss whether radiologic imaging is capable of providing valid information for diagnosing the cause of death with certainty and reliability and if pmCT adds value to the classical autopsy. Finally, a short outlook on future perspectives is given.
The diagnosis of the cause of death after pmCT matched the diagnosis after autopsy in two out of three of our cases (Table 3). The discrepancy rate of 1/3 is similar to the discrepancy rate of 30 % reported by Roberts et al. [21] and the major discrepancy rate of 12.5–40 % (depending on type of pathology) by Wichmann et al. [16]. Weustink et al. [17] report a discrepancy rate of 23 % with minimal invasive autopsy, consisting of pmCT, MRI and biopsy. The positive predictive value (PPV) of 75 % (Table 3) is obviously not representative for the wide range of diagnoses found. The PPV would ideally be calculated per diagnosis, which would require a much larger sample size.
Other publications on post-mortem imaging report difficulties in finding artery occlusions, myocardial infarctions and pulmonary lesions [22, 23].
The results show that coronary thromboses and in-stent thromboses and myocardial infarction were not found with pmCT in any case. Nevertheless, in all cases of coronary or in-stent thrombosis with myocardial infarction, a cardiac cause of death was diagnosed correctly with pmCT by deduction from associated diagnoses (congestion, coronary atherosclerosis, pleural effusion). Therefore, although the pathogenetic mechanism could not be reconstructed in full detail by the radiologist, the cause of death was diagnosed correctly. The lung is subject to post-mortem sedimentation of blood, which causes density shifts (internal livores) and makes the differentiation between pneumonia and pulmonary oedema difficult. In our study, there was only one false-positive finding of pneumonia. Still, it is difficult to correlate pathologic findings of the lung and the radiologic finding of ground glass attenuation, which not only may partly correlate with pulmonary pathologies but may partly also be caused by internal livores of the lung [24].
In contrast to artery occlusions, myocardial infarctions and pulmonary lesions, haemorrhage and haematoma can be differentiated from other liquids due to their high attenuation in pmCT (unclotted blood, 30–45 HU; clotted blood, .45–70 HU [25]). In our study, in cases of fatal haemorrhage, the intracavital bleeding was recognized equally well with pmCT and macroscopic examination. Organ sizes and configurations as well as cysts could be assessed with pmCT (myocardial hypertrophy, goitre, hepatosplenomegaly, fatty liver, liver and kidney cysts). There was a discrepancy in diagnosis of myocardial hypertrophy between radiologists and pathologists (19 at classical autopsy, 10 with pmCT). This discrepancy might be due to the poor contrast between myocardium and left ventricular lumen in unenhanced pmCT, which makes the differentiation between myocardial hypertrophy and left ventricular dilation difficult for the radiologist. Moreover, post-mortal contraction of the ventricles limits the appraisal of the imaging findings. These shortcomings caused the misinterpretation in the cause of death due to dilated cardiomyopathy, in which the myocardial hypertrophy was reported from pmCT, but dilation of the left ventricle was missed.
While dilation of heart cavities can be easily detected in vivo using contrast-enhanced CT in pmCT, the assessment of cardiac myopathy can be hindered by collapse of the heart cavities and lack of clear delineation of the myocardium due to the missing contrast agent. This is a possible explanation for the discrepancy between autopsy and pmCT findings.
A complete autopsy includes external examination for the documentation of sure signs of death (rigour mortis, livores, putrefaction, injuries not compatible with life) and other external findings. Livores and putrefaction are visible with pmCT as internal livores and intravascular gas [24]. Nevertheless, rigour mortis or punction marks cannot be assessed with pmCT. Therefore, the external examination cannot be completely replaced by imaging methods.
Information on organ colour, not only characteristic for myocardial infarction, but also other characteristic colour changes such as icterus, antracosis or colour of ascites, pleural or pericardial effusion, bile, stomach and intestinal content and “nutmeg liver” (sign of chronic passive congestion of the liver) are not visible.
The results show that the reconstruction of the pathogenetic mechanism is still challenging (Table 4). In the study, the attempt of the radiologists to reconstruct the pathogenetic mechanism was dismissed when it was not identical with the pathogenetic mechanism reconstructed by the pathologists. Probably, in some constellations, there is more than one valid interpretation of findings. Therefore, the discrepancies may be due to different focuses on the pathologies found. The presentation of the autopsy findings to the clinical colleagues requesting autopsy and the interdisciplinary discussion of case progression and autopsy findings imply an important, possibly decisive, advantage to the pathologists. Thus, an interdisciplinary discussion of pmCT findings with autopsy findings and clinical progression of every case would be desirable for the most valid diagnosis of cause of death.
There are special areas in which pmCT may even prove superior to classical autopsy: The results show that pmCT is an excellent tool for assessment and documentation of calcified and bone lesions. Histological assessment of calcified tissue is extremely time consuming, as it is necessary to decalcify tissues prior to sectioning. Furthermore, the comparison of imaging autopsy findings with findings of intravital clinical examinations, such as coronary angiography, is very simple and readily accessible for clinicians. The extremities and the joints are examined only on very rare occasions, in order not to mutilate the body. Pathologies of the musculoskeletal system, especially of the viscerocranium and the extremities, are therefore easily missed by conventional autopsy. Fractures can be missed with both methods when there is no dislocation or haemorrhage [16, 25]; therefore, a combination of both methods gives most valid results. In cases of metallic implants, beam hardening artefacts occur on pmCT images, impairing assessment of underlying structures.
Vessels and organs are opened for macroscopic examination at autopsy. Therefore, air accumulations, such as subcutaneous emphysema, intravascular or intrapericardiac air and aerobilia, are more efficiently visualized and documented with pmCT than at macroscopic examination.
The same applies to small pleural effusions and small pneumothoraces, which were seen on radiological images, but not found at clinical autopsy. With the opening of the body cavities, pressure is released; thus, lesions depending on intracavital pressure such as hiatal or inguinal hernia become invisible at macroscopic examination but are easily recognized with pmCT. The presence of catheters and tracheal tubes can be documented three-dimensionally with pmCT, as well as the site of catheter tip or tracheal tube.
Unlike at conventional autopsy, the data generated with pmCT stay stored and are readily accessible afterwards for repeated examination. Compared to CT images from living patients, with pmCT, we do not have to deal with motion artefacts or limitation of dose of radiation. In contrast to notes or pictures taken at autopsy, the images acquired with pmCT are a three-dimensional snapshot not limited by the point of view or knowledge of the individual generating them.
In the future, a method to overcome diagnostic difficulties resulting from lack of inspiration and dependent density may be post-mortem ventilation [26]. With the use of contrast enhancement, post-mortem imaging of the cardiovascular system might become equal, if not superior, to macroscopic examination, as a bleeding site might be found by extravasation of the contrast agent. In cases of haemorrhage from an unknown site, pmCT angiography could help to find an extravasation site at macroscopic examination and support macroscopic findings. The diagnostic problems concerning myocardial hypertrophy with pmCT could be overcome with contrast filling of the heart cavities. Also, the above-mentioned assessment of in-stent stenosis, in-stent thrombosis, coronary artery occlusion and aneurysms might become possible. Still, signs of intravitality of the lesions would yet need confirmation by macroscopic and histologic analysis, in order to exclude artificial extravasation or post-mortem blood clots.
Conclusion
It is amazing how much we already see on unenhanced post-mortem CT images. Concluding from our observations, unenhanced virtual autopsy represents a valuable tool for documentation of pathologic findings such as calcified lesions of the cardiovascular system, bone fractures, lesions of the musculoskeletal system, air accumulations and herniations. Therefore, pmCT complements traditional autopsy techniques. The combination of both methods enhances the diagnostic quality and completeness of the autopsy report. Furthermore, imaging data can be acquired and stored in a less observer-dependent manner to be re-evaluated ad libitum. In addition to traditional autopsy findings, visualization of pathomorphologic findings by post-mortem imaging is likely to be appreciated by clinicians and students. The acceptance of virtual autopsy as a complementary method to traditional autopsy by clinicians needs to be further evaluated.
We believe that many limitations of pmCT will be overcome in the future with the help of post-mortem angiography and CT-guided biopsy from areas of special interest. Furthermore, by interdisciplinary discussion of the results, pathologists and radiologists will get an opportunity to correlate their diagnoses with clinical findings and experience a learning curve interpreting post-mortem imaging and reconstructing the underlying pathogenetic mechanism. In order to avoid systematic errors and to define the limitations of pmCT accurately, traditional autopsy should always be performed as a gold standard. As an instrument of clinical quality control, resident training in pathology and student teaching, traditional autopsy is still unsurpassed.
References
Horowitz RE, Naritoku WY (2007) The autopsy as a performance measure and teaching tool. Hum Pathol 38:688–695
Krukemeyer MG, Driesch C, Dankof A, Krenn V, Hansen D, Dietel M (2007) Necessity of increasing autopsy frequency following the introduction of DRGs. Pathologe 28:294–298
Brinkmann B, Du CA, Vennemann B (2002) Recent data for frequency of autopsy in Germany. Dtsch Med Wochenschr 127:791–795
Chariot P, Witt K, Pautot V, Porcher R, Thomas G, Zafrani ES, Lemaire F (2000) Declining autopsy rate in a French hospital: physician's attitudes to the autopsy and use of autopsy material in research publications. Arch Pathol Lab Med 124:739–745
Lindstrom P, Janzon L, Sternby NH (1997) Declining autopsy rate in Sweden: a study of causes and consequences in Malmo, Sweden. J Intern Med 242:157–165
Start RD, McCulloch TA, Benbow EW, Lauder I, Underwood JC (1993) Clinical necropsy rates during the 1980s: the continued decline. J Pathol 171:63–66
Harrington DE, Sayre EA (2010) Managed care and measuring medical outcomes: did the rise of HMOs contribute to the fall in the autopsy rate? Soc Sci Med 70:191–198
Anon. (2004) The decline of the hospital autopsy: a safety and quality issue for healthcare in Australia. Med J Aust 180:281–285
Ishiko T (1989) Decline of autopsy rates in Japan and the significance of autopsy in gastric carcinoma. Gan To Kagaku Ryoho 16:1920–1924
Burton JL, Underwood J (2007) Clinical, educational, and epidemiological value of autopsy. Lancet 369:1471–1480
Persson A, Jackowski C, Engstrom E, Zachrisson H (2008) Advances of dual source, dual-energy imaging in postmortem CT. Eur J Radiol 68:446–455
Rutty GN (2007) Are autopsies necessary? The role of computed tomography as a possible alternative to invasive autopsies. Rechtsmedizin 17:21–28
Woodward PJ, Sohaey R, Harris DP, Jackson GM, Klatt EC, Alexander AL, Kennedy A (1997) Postmortem fetal MR imaging: comparison with findings at autopsy. AJR Am J Roentgenol 168:41–46
O'Donnell C, Woodford N (2008) Post-mortem radiology—a new sub-speciality? Clin Radiol 63:1189–1194
Shiotani S, Kohno M, Ohashi N, Yamazaki K, Nakayama H, Ito Y, Kaga K, Ebashi T, Itai Y (2002) Hyperattenuating aortic wall on postmortem computed tomography (PMCT). Radiat Med 20:201–206
Wichmann D, Obbelode F, Vogel H, Hoepker WW, Nierhaus A, Braune S, Sauter G, Pueschel K, Kluge S (2012) Virtual autopsy as an alternative to traditional medical autopsy in the intensive care unit: a prospective cohort study. Ann Intern Med 156:123–130
Weustink AC, Hunink MG, van Dijke CF, Renken NS, Krestin GP, Oosterhuis JW (2009) Minimally invasive autopsy: an alternative to conventional autopsy? Radiology 250:897–904
Stawicki SP, Gracias VH, Schrag SP, Martin ND, Dean AJ, Hoey BA (2008) The dead continue to teach the living: examining the role of computed tomography and magnetic resonance imaging in the setting of postmortem examinations. J Surg Educ 65:200–205
Ikeda G, Yamamoto R, Suzuki M, Ishikawa H, Kikuchi K, Shiotani S (2007) Postmortem computed tomography and magnetic resonance imaging in a case of terminal-stage small cell lung cancer: an experience of autopsy imaging in tumor-related death. Radiat Med 25:84–87
Thali MJ, Yen K, Schweitzer W, Vock P, Boesch C, Ozdoba C, Schroth G, Ith M, Sonnenschein M, Doernhoefer T, Scheurer E, Plattner T, Dirnhofer R (2003) Virtopsy, a new imaging horizon in forensic pathology: virtual autopsy by postmortem multislice computed tomography (MSCT) and magnetic resonance imaging (MRI)—a feasibility study. J Forensic Sci 48:386–403
Roberts IS, Benamore RE, Benbow EW, Lee SH, Harris JN, Jackson A, Mallett S, Patankar T, Peebles C, Roobottom C, Traill ZC (2012) Post-mortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet 379:136–142
Jackowski C, Schweitzer W, Thali M, Yen K, Aghayev E, Sonnenschein M, Vock P, Dirnhofer R (2005) Virtopsy: postmortem imaging of the human heart in situ using MSCT and MRI. Forensic Sci Int 149:11–23
Pflederer T, Marwan M, Schepis T, Ropers D, Seltmann M, Muschiol G, Daniel WG, Achenbach S (2010) Characterization of culprit lesions in acute coronary syndromes using coronary dual-source CT angiography. Atherosclerosis 211:437–444
Shiotani S, Kohno M, Ohashi N, Yamazaki K, Nakayama H, Watanabe K, Oyake Y, Itai Y (2004) Non-traumatic postmortem computed tomographic (PMCT) findings of the lung. Forensic Sci Int 139:39–48
Lubner M, Menias C, Rucker C, Bhalla S, Peterson CM, Wang L, Gratz B (2007) Blood in the belly: CT findings of hemoperitoneum. Radiographics 27:109–125
Germerott T, Preiss US, Ebert LC, Ruder TD, Ross S, Flach PM, Ampanozi G, Filograna L, Thali MJ (2010) A new approach in virtopsy: postmortem ventilation in multislice computed tomography. Leg Med (Tokyo) 12:276–279
Acknowledgments
The authors would like to thank Bernd Sellhaus, Marc Britz and Wim Haas.
Disclosures
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
Results of pmCT vs. classical autopsy (items 1–4) per case (DOC 169 kb)
Supplementary Table 2
Side diagnoses of classical autopsy vs. pmCT (item 5) (DOC 78 kb)
Rights and permissions
About this article
Cite this article
Westphal, S.E., Apitzsch, J., Penzkofer, T. et al. Virtual CT autopsy in clinical pathology: feasibility in clinical autopsies. Virchows Arch 461, 211–219 (2012). https://doi.org/10.1007/s00428-012-1257-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-012-1257-4