Abstract
There is paucity of literature on liver histological spectrum of acute-on-chronic liver failure (ACLF). The aims of this study are to (a) to characterize the liver histological features in ACLF, (b) to correlate histological parameters with prognosis, and (c) to investigate whether etiology influences prognosis. We retrospectively studied liver biopsies of patients with ACLF. The histological findings were correlated with the clinical outcome. Fifty cases (median age, 39 years [10–69 years]; M/F, 3:1) were included. Etiology of acute insult was viral or alcohol in majority of the cases. Twenty-five patients survived (good outcome, 50%) and 25 died (poor outcome, 50%). On a univariate analysis, the outcome correlated with fibrosis, ballooning, eosinophilic degeneration, ductular proliferation, pericellular fibrosis, Mallory’s hyaline, foci of confluent necrosis and/or bridging necrosis (CN/BN), cholestasis, apoptosis (present), and parenchyma left. However, on a multivariate analysis, only fibrosis, ballooning, ductular proliferation, apoptosis, and parenchyma left were found to be independently associated with outcome. Two distinct patterns of liver histology were observed: pattern I, observed in cases with poor outcome, showing marked ductular proliferation, coarse inspissated ductular bile plugs, eosinophilic degeneration of hepatocytes, foci of CN/BN, higher apoptosis, pericellular fibrosis, Mallory’s hyaline, and higher stage of fibrosis. Pattern II is seen in cases with good outcome, show prominent hepatocyte ballooning with lesser parenchymal involvement by fibrosis and necrosis. Histological features of liver biopsy are: extent of fibrosis, ballooning, ductular proliferation, apoptosis, and lesser degree of parenchymal replacement by fibrosis or necrosis which correlates with the outcome in patients with ACLF. Two distinct patterns of liver histology are seen which help in prognostication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver failure can develop either as acute liver failure in the absence of any preexisting liver disease, as chronic decompensation of an end-stage liver disease (ESLD), or as an acute deterioration of known or unknown chronic liver disease—the acute-on-chronic liver failure (ACLF). ACLF constitutes an illness where two insults to the liver are operating simultaneously: one acute and other chronic.
There is limited data on the entity of ACLF. The Asian Pacific Association for the Study of the Liver (APASL) has defined ACLF as acute hepatic insult manifesting as jaundice and coagulopathy, complicated within 4 weeks by ascites, and/or encephalopathy in a patient with previously diagnosed or undiagnosed chronic liver disease [1]. Presentation, course, and outcome of these patients are different from patients of acute liver failure (ALF) and from ESLD. ACLF is potentially reversible, more so with the emergence of newer liver support strategies, hence it has become necessary to distinguish these entities.
Early and accurate diagnosis and prognosis of patients with ACLF is of critical importance for optimum management. There is paucity of literature highlighting the liver histological spectrum of ACLF. The role of liver biopsy as an outcome predictor in ACLF is not clear and has not been highlighted so far. We undertook this study with the following aims: (a) to characterize the liver histological features in ACLF, (b) to investigate whether histological parameters can determine the prognosis and differentiate end-stage fibrotic liver disease from ACLF, and (c) to investigate whether etiology influences histology–prognosis relationship.
Patients and methods
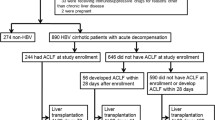
Patients
A retrospective study was conducted in which we evaluated liver biopsies of 50 patients with clinical diagnosis of ACLF that were received in the department of pathology. These cases were included in the study based on the APASL criteria of ACLF [1] and availability of an adequate liver biopsy (≥1 cm in length). Patients with HCC or portal vein thrombosis or cardiovascular comorbidities were excluded from the study.
Methods
Demographic, clinical findings, and outcome were recorded from the hospital medical records. The main clinical outcome measures were survival (good outcome) versus death (poor outcome).
Histology
Formalin-fixed paraffin-embedded transjugular liver biopsies were retrospectively reviewed by three histopathologists (AR, PS, RG) blinded to individual patient’s etiological details, clinical findings, and to the eventual outcome. Almost perfect concordance was found amongst them for most of the parameters and minor discrepancies encountered were resolved by reviewing the cases together on multilateral microscope. Serial sections of liver biopsies stained with hematoxylin and eosin (H&E), Masson’s Trichrome, and Shikata’s orcein were examined in all the cases. Reticulin stain for reticulin fibers and Fouchet’s stain for bile were also done in most of the cases.
The degree of hepatic inflammation and fibrosis were graded using Ishak’s score [2]. Histological activity index (HAI) ≥6 and fibrosis score ≥3 were considered significant for the present study.
Following histological features were also assessed and semiquantitatively graded for each of the 50 biopsies of ACLF patients available for analysis: hepatocyte ballooning, eosinophilic degeneration of hepatocytes, rosette formation by hepatocytes, pericellular fibrosis, ductular proliferation, cholangiolitis, apoptosis, and Mallory’s hyaline. Hepatocytes were said to be undergoing eosinophilic degeneration when the cytoplasm showed hypereosinophilia. These histological features were visually estimated on a scale of 0 to 3 (0, absent; 1, occasional to mild; 2, moderate; 3, marked). A score of 2–3 was considered positive for analysis.
Cholestasis is a common feature of acute hepatocellular injury. Ductular cholestasis is a more advanced form of cholestasis, and usually develops in a background of cellular and canalicular cholestasis. It is often seen in systemic conditions, extensive hepatocellular necrosis, and chronic liver disease in terminal stages. Cholestasis was defined as type 1 when fine granular intrahepatocytic and canalicular bile was seen; type 2 when in addition to type 1, coarse inspissated canalicular and few ductular bile plugs were seen; and type 3 when in addition to type 2, prominent ductular bile plugs along with the cellular cholestasis was seen. Type 2 and 3 were taken together for correlation.
For parenchyma left (percentage) a cutoff of 50% was considered significant (fraction of total surface area of the biopsy that is not occupied by parenchymal necrosis or fibrosis). Fatty change involving ≥30% of the liver biopsy parenchyma was considered significant for the present study.
Foci of confluent necrosis and/or bridging necrosis (CN/BN) were visualized on H&E-stained sections and confirmed by orcein and reticulin stain. Bridging necrosis is confluent necrosis that bridges terminal hepatic venules to portal tracts. When hepatocytes are damaged and undergo necrosis, the reticulin fibers surrounding them collapse in the empty space left behind. Reticulin crowding is seen in areas of focal hepatocyte loss and reticulin collapse in large areas of necrosis. Orcein stains elastic fibers and helps distinguish areas of bridging necrosis from bridging fibrosis and in assessment of periportal fibrosis in severely inflamed portal areas. Foci CN/BN were visually estimated on a scale of 0 to 3 (0, absent; 1, occasional to mild; 2, moderate; 3, marked). A score of 2–3 was considered significant.
All the histological parameters were correlated with the outcome. Presence of histological features was also compared amongst the major etiological groups—group I, acute viral hepatitis (AVH) superimposed on chronic liver disease (CLD) of any etiology; group II, reactivation of chronic hepatitis B (CHB); and group III, alcoholic hepatitis on underlying chronic alcoholic liver disease (ALD).
Statistical analysis
All results were expressed as mean (±SD), median (range), or number (%). Comparisons between the two groups (good outcome versus poor outcome) were carried out by Student’s t test for parametric data, Mann–Whitney U test for nonparametric data, and Fischer’s exact test for categorical data. Differences were considered significant at p value of <0.05. Statistical analyses were performed with the SPSS 15.0 statistical package (SPSS Inc., Chicago, IL).
Results
Demographic characteristics
A total of 50 cases were included in this study. The median age of the patients was 39 years (range, 10–69 years). There were 36 males and 14 females (M/F ratio, 2.6:1).
Etiology of acute insult and chronic liver disease
Chronic liver disease was due to hepatitis B virus (n = 32) and alcohol (n = 10) in most of the cases. Possible etiology of acute decompensation was viral (n = 37) or alcoholic (n = 7) in majority of the cases. Major etiologic groups were reactivation of chronic hepatitis B (n = 20), acute alcoholic hepatitis superimposed on alcoholic liver disease (n = 7), and acute hepatitis of any etiology superimposed on chronic liver disease of different etiology (n = 23) (Table 1).
Outcome of patients
An equal number of patients had good (n = 25, 50%) and poor (n = 25, 50%) outcome. All deaths occurred during the same admission. The median time (from hospital admission) to death was 15 days (range, 2 to 102).
Demographic and biochemical characteristics in patients with good and poor outcome
The median age was similar in patients with good and poor outcome. Mean serum bilirubin and albumin levels were 22.0 ± 9.5 mg/dl and 3.0 ± 0.7 g/dl, respectively. Serum bilirubin levels (mean ± SD) for the groups with good and poor outcome were 19.7 ± 8.8 and 24.1 ± 9.8 mg/dl, respectively (p < 0.05). Serum albumin levels (mean ± SD) for the groups with good and poor outcome were 3.3 ± 0.8 and 2.7 ± 0.6 g/dl, respectively (p < 0.05).
Histological characteristics of ACLF
Mean core tissue length of liver biopsy specimens was 1.2 cm. All cases showed features of acute and chronic hepatitis in variable combinations. Features of acute injury such as ballooning degeneration of hepatocytes, cellular, and/or ductular cholestasis, ductular proliferation with variable degree of parenchymal necrosis/collapse along with the features of chronic liver disease as periportal fibrous extensions, bridging fibrosis or cirrhosis, pericellular fibrosis and interface activity, were seen in all the biopsies.
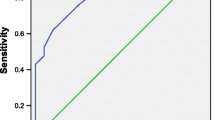
Correlation of liver histology with outcome in ACLF
Table 2 summarizes histological characteristics in both the outcome groups. On a univariate analysis, the following factors were found to be associated with poor outcome: fibrosis (stage, ≥3); ballooning inversely correlates with poor outcome (score, 2–3); eosinophilic degeneration (score, 2–3); ductular proliferation (score, 2–3); pericellular fibrosis (score, 2–3); Mallory’s hyaline (score, 2–3); foci of CN/BN (score, 2–3); cholestasis (types, 2–3); apoptosis (present); and parenchyma left (> 50%) inversely correlates with poor outcome. However, on a multivariate analysis (Table 3) fibrosis, ductular proliferation, and apoptosis independately correlate with poor outcome; whereas ballooning and parenchyma left correlate inversely with poor outcome.
Correlation of histological characteristics amongst the major etiologic groups
Based on etiology, the patients were categorized into the following three groups: group I, AVH superimposed on CLD of any etiology (n = 23); group II, reactivation of CHB (n = 20); and group III, alcoholic hepatitis on underlying chronic ALD (n = 7). The presence of all the histological parameters were assessed in the three major etiologic groups to confirm that such histologic patterns and their prognostic value were not related to any specific etiology. Most of the 14 histological parameters did not show any association with the etiologic groups, except that Mallory’s hyaline and pericellular fibrosis which were significantly more common in group III than group I or II. Similarly, HAI was more marked in group I than III (Table 4).
Histological patterns
Two distinct patterns of liver histology were observed. Pattern I was observed in cases with poor outcome, and biopsy showed marked ductular proliferation, coarse inspissated ductular bile plugs, eosinophilic degeneration of hepatocytes, foci of confluent necrosis/bridging necrosis, higher apoptosis, pericellular fibrosis, Mallory’s hyaline, and higher stage of fibrosis. Pattern II was seen in cases with good outcome, show prominent hepatocyte ballooning with lesser parenchymal involvement by fibrosis and necrosis (Figs. 1 and 2).
Discussion
This is a study of the liver histology of 50 cases of ACLF, first to the best of our knowledge, in which 14 liver histological features and their role as outcome predictor were studied. Liver histology revealed features of acute injury and chronic liver diseases with/without necrosis, in varying combinations and variable degrees of severity. Two distinct histological patterns were observed. Eosinophilic degeneration of hepatocytes, ductular cholestasis, advanced fibrosis, ductular proliferation, increased apoptosis, foci of confluent necrosis/bridging necrosis, pericellular fibrosis, and Mallory’s hyaline emerged as predictors of poor outcome, whereas ballooning degeneration of hepatocytes and lesser degree of parenchymal involvement by fibrosis or necrosis were indicators of good outcome, on a univariate analysis. The multivariate analysis showed fibrosis, ductular proliferation, and apoptosis to be independently associated with poor outcome and ballooning degeneration and parenchymal (left) with good outcome in patients with ACLF. These features were also compared amongst the main etiological groups (AVH superimposed on CHB, HBV reactivation, and exacerbation of ALD). Of the 14 histological features, pericellular fibrosis and Mallory’s hyaline showed etiologic association and were significantly more commonly seen in the alcoholic group. HAI was more marked in group I than III. These findings need validation by studies in larger disease groups.
ACLF is a serious condition with varied acute and chronic underlying etiologies and high mortality. This term was first used in 1995 to describe a condition where two insults to the liver are operating simultaneously, an acute event occurring on an underlying chronic liver disease [3]. However, this entity of acute-on-chronic liver failure still remains poorly defined.
With the emergence of newer liver support strategies and encouraging results reported in patients with ACLF, it has become essential to define this entity, its pathophysiology, and the prognosis determinants [4].
The APASL’s definition of ACLF is “Acute hepatic insult manifesting as jaundice and coagulopathy, complicated within 4 weeks by ascites and/or encephalopathy in a patient with previously diagnosed or undiagnosed chronic liver disease” [1].
Whether the prognosis of the patient depends on the degree of acute insult or chronic insult or the combination of the two is still not well defined. It is essential to separate ACLF from ALF and CLD as presentation, course, and outcome differ from them.
There is scarcity of histological data on ACLF. The role of liver biopsy in diagnosing underlying chronic liver disease and its prognostic significance are not clear and have not been studied so far.
In the present study, liver biopsies in all the cases revealed features of both acute and chronic hepatitis with variable severity. Liver histology comprised of hepatocyte ballooning and eosinophilic degeneration of hepatocytes, rosette formation by hepatocytes, apoptosis (councilman bodies), fatty change, cholestasis (hepatocyte, canalicular, bile ductular, and ducts), lobular inflammation, portal inflammation, Mallory’s hyaline, percentage of parenchyma left (not involved by necrosis/fibrosis), foci of CN/BN with portal/periportal fibrosis, ductular proliferation, pericellular fibrosis, and cholangiolitis [5, 6].
Previous studies in patients with liver failure have shown that liver biopsy can be very helpful particularly in prognostication by determining the extent of necrosis, liver damage, and fibrosis. It can help in differentiating acute liver failure from acute-on-chronic liver failure by confirming chronic liver disease [7–10].
Liver biopsy can also provide clues to the underlying etiology if the diagnosis remains elusive after extensive initial evaluation as is recommended in AASLD position paper on acute liver failure which states that liver biopsy may be appropriate to attempt to identify a specific etiology that might influence treatment strategy—malignant infiltration, autoimmune hepatitis, certain viral infections, Wilson disease, drug-induced injury [11].
Although terminology used in various studies differ, the importance of liver histology in predicting outcome is well emphasized particularly of parenchymal necrosis, fibrosis, ductular cholestasis, and hepatocyte changes. These findings are similar to our study in which all these parameters were studied in a large group of ACLF patients.
Distinct histological patterns identified in our patients have not been previously reported in literature; however, some of the individual parameters were found to be quite convincing and consistent with the observations of other studies in a small number of patients [8].
Boyer and Klatskin [7], in their study of 170 patients, had emphasized the importance of liver biopsy in assessing prognosis during the acute phase of viral hepatitis by assessing presence of bridging necrosis (subacute hepatic necrosis). One hundred eighteen of their patients who had a benign clinical course revealed only spotty necrosis in liver biopsy, whereas in 50 patients (subacute hepatic necrosis group), outcome was poor (19% died and 37% developed cirrhosis), and their diagnosis in most of the cases depended on liver biopsy.
Nayak et al. [8], in their study of 42 patients of subacute hepatic failure, reported presence of bridging necrosis, ductular cholestasis, and nonreactive/eosinophilic change in hepatocytes to be more common in fatal group. Nonreactive change in hepatocytes appeared to be directly related to mortality in subacute hepatic failure. Twenty-two out of 23 patients in the group with poor outcome and one out of 19 in patients with good outcome showed nonreactive change in liver biopsy. Ductular cholestasis alone or along with cellular cholestasis was much more common in fatal cases (19/21 vs 8/19, respectively). Bridging necrosis was also more common in the fatal group, and it was more extensive and wide, 22/23 (96%) vs 14/19 (74%), respectively.
Tandon et al. [12] have shown, in their study of 33 patients of subacute hepatic failure, submassive and bridging necrosis as the main liver histological findings.
We also found similar correlation of histology with prognosis in our study. Eosinophilic degeneration of hepatocytes (<0.001), ductular cholestasis (<0.001), advanced fibrosis (<0.001), ductular proliferation (<0.001), foci of confluent necrosis/bridging necrosis (0.002), apoptosis (0.001), pericellular fibrosis (<0.001), Mallory’s hyaline (0.022) emerged as predictors of poor outcome, whereas ballooning degeneration of hepatocytes (<0.001) and lesser degree of parenchymal replacement by fibrosis or necrosis (<0.001) were indicators of good outcome on univariate analysis. Multivariate analysis showed fibrosis, ductular proliferation, and apoptosis to be independently associated with poor outcome and ballooning degeneration and parenchyma left with good outcome in patients with ACLF. Scotto et al. have also shown that early liver biopsy during acute liver failure allows a good estimation of remaining functional hepatocyte volume and prognosis [13].
None of the previous studies have discussed the influence of etiology on the role of histological features as outcome predictors. In our study, we have assessed all the features in three main etiologic groups, and pericellular fibrosis and Mallory’s hyaline were significantly more common in the alcoholic group. HAI was more marked in group I than III.
Liver biopsy provides useful prognostic information by determining the extent of necrosis, liver damage, and fibrosis. Two distinct patterns of liver histology are seen in ACLF, and a classification based on histopathology can help in management and prognostication. Extensive necrosis, advanced fibrosis, ductular cholestasis, and proliferation, pericellular fibrosis, increased apoptosis along with eosinophilic degeneration of hepatocytes were predictors of poor outcome in ACLF. The impact of the histological parameters and of the etiology on prognosis needs validation by studies on larger groups of patients, postmortem biopsies, and explant data. Biopsy in ACLF should be need-based/individualized.
References
Sarin SK, Kumar A, Almeida J et al (2009) Acute on chronic liver failure (ACLF): consensus recommendations of the Asia Pacific Association for the Study of the Liver (APASL). Hepatol Int 3:269–282
Ishak K, Baptista A, Bianchi L et al (1995) Histological grading and staging of chronic hepatitis. J Hepatol 22:696–699
Ohnishi H, Sugihara J, Moriwaki H, Muto Y (1995) Acute-on-chronic liver failure. Ryoikibetsu Shokogun Shirizu 7:217–219
Bauer M, Winning J, Kortgen A (2005) Liver failure. Curr Opin Anaesthesiol 18:111–116
Suriawinata AA, Thung SN (2006) Acute and chronic hepatitis. Semin Diagn Pathol 23:132–148
Burt AD, Portmann BC, Ferrell LD (2007) MacSween’s pathology of the liver, 5th edn. Churchill Livingstone, Edinburgh
Boyer JL, Klatskin G (1970) Pattern of necrosis in acute viral hepatitis. Prognostic value of bridging (subacute hepatic necrosis). N Engl J Med 283:1063–1071
Nayak NC, Dutta Gupta S, Tandon A, Dasarathy S, Acharya SK (1993) Pathology of sub-acute hepatic failure. Indian J Gastroenterol 12(suppl 3):11–14
Liu Q, Liu Z, Wang Q, Wang Q, Shi X, Dao W (2007) Characteristics of acute and sub-acute liver failure in China: nomination, classification and interval. J Gastroenterol Hepatol 22:2101–2106
Donaldson BW, Gopinath R, Wanless IR et al (1993) The role of transjugular liver biopsy in fulminant liver failure: relation to other prognostic indicators. Hepatology 18:1370–1376
Polson J, Lee WM (2005) AASLD position paper: the management of acute liver failure. Hepatology 41:1179–1197
Tandon BN, Joshi YK, Krishnamurthy L, Tandon HD (1982) Subacute hepatic failure: is it a distinct entity? J Clin Gastroenterol 4:343–346
Scoto J, Opolon P, Itipvi J, Vergoz D, Thomas M, Caroli J (1973) Liver biopsy and prognosis in acute liver failure. Gut 14:927–933
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rastogi, A., Kumar, A., Sakhuja, P. et al. Liver histology as predictor of outcome in patients with acute-on-chronic liver failure (ACLF). Virchows Arch 459, 121–127 (2011). https://doi.org/10.1007/s00428-011-1115-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-011-1115-9