Abstract
Breast cancer is known for its propensity to recur decades after treatment. The biology behind the phenomenon of tumor dormancy is still poorly understood. Bmi-1, c-myc, and Snail are transcription factors that have prognostic roles in several malignancies. In order to reveal whether any of these markers has impact on late relapses, we used immunohistochemistry to study the expression of Bmi-1, c-myc, Snail, and estrogen receptor in 73 primary breast cancers and in their metastatic relapses detected within 2 years, or 5 or 10 years after primary surgery. The expression of Bmi-1 was higher in the metastases than in their corresponding primary tumors in both early and late relapses. The highest expression of Bmi-1 was seen in the very late relapsing tumors (first tumor relapse after 10 years). Previously, Bmi-1 has been reported to function as a marker of tumor stem cells in breast cancer. Our results indicate that metastases, when compared to primary tumors, arise from tumor cells that have retained stem cell properties. We also analyzed the relationship between the expression of these markers and clinical parameters. A significant association between the expression of Bmi-1 and estrogen receptor was found. Nuclear expression of c-myc in primary tumors correlated with an increased risk for axillary lymph node metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
B cell-specific Moloney murine leukemia virus integration site 1 (Bmi-1), which was first identified by retroviral insertional mutagenesis and as a collaborating oncogene by retroviral insertional mutagenesis in Eμ-myc transgenic mice [1, 2], was assessed. Bmi-1 belongs to the mammalian polycomb group proteins which form multimeric complexes that regulate gene activity at the chromatin level [3]. Bmi-1 contributes to cell cycle regulation by acting as a transcriptional repressor of the INK4a/ARF (=human p19ARF) locus [4]. Kim et al. [5] demonstrated overexpression of Bmi-1 transcripts and protein in breast cancer and found high expression to correlate with axillary lymph node metastases. They suggested that cell cycle deregulation by Bmi-1 might play a role in the progression of breast cancer and lymph node metastasis. Al-Hajj et al. described the existence of a cancer stem cell population in human breast cancers [6]. These cancer stem cells displayed increased expression of Bmi-1 [7]. Overexpression of Bmi-1 correlates with a poor prognosis in non-keratinizing type of nasopharyngeal carcinoma and hepatocellular carcinoma [8, 9] as well as in neural tumors, such as oligodendrogliomas and medulloblastomas [10, 11]. A correlation has also been reported with higher tumor stage in non-small cell lung cancer [12]. In squamous cell carcinoma of the tongue, the absence of Bmi-1 protein in the tumor cells was associated with a higher risk of recurrence [13].
Bishop and co-workers discovered c-myc in the late 1970s [14, 15]. C-myc is a DNA-binding, nuclear transcription factor involved in the regulation of the cell cycle [16], programmed cell death, and tumorigenesis [17, 18]. C-myc was first detected in Burkitt’s lymphoma, but has later been connected with many other cancers, including breast and colon cancer, neuroblastoma, osteosarcoma, and melanoma [19]. Given the plethora of biological roles played by MYC gene products and the lack of reliable antibodies needed for immunohistochemical analysis, the clinical relevance of the overexpression of c-myc protein in breast cancer is not well known [20, 21]. On the other hand, MYC gene amplification has been associated with high histological grade, the presence of lymph node metastasis, a lack of progesterone receptor, and poor survival in breast cancer [21, 22]. Bmi-1 influences c-myc activity and vice versa, and both these oncogenes are able to immortalize certain cells [23–25].
Snail is a zinc-finger transcription factor essential for epithelial-mesenchymal transition (EMT). It downregulates the expression of cell adhesion and basement membrane proteins, most importantly cadherins [26]. Snail increases migration and invasion in various physiological and pathological conditions [26–28]. The involvement of Snail in tumor progression is supported by the expression of Snail in carcinoma cell lines having invasive and metastatic properties [27, 29, 30] in dedifferentiated breast cancer and hepatocellular carcinoma [31, 32]. Snail is required for tumor growth and lymph node metastasis of heterotransplanted human breast carcinoma MDA-MB-231 cells [33].
According to previous investigations, Bmi-1, c-myc, and Snail are stem cell-related proteins. On this basis, we investigated their association to late relapse of breast cancer by analyzing the expression of these proteins in both early and late relapsing tumors.
Materials and methods
Patients and tumors
Paraffin-embedded tissue blocks were obtained from 73 primary breast cancers and their metastatic lesions from the archives of the Department of Pathology, Helsinki University Hospital, as described previously [34]. Patients, from whom histological samples were available from both the primary tumor and metastases, were included in the study. The patients had undergone breast cancer surgery in 1974–2006. The cases were divided into three groups: Group 1 (n = 19), tumors with metastatic recurrence within 2 years after primary surgery; Group 2 (n = 33), tumors with metastatic recurrence in 5–10 years; and Group 3 (n = 21), tumors with metastatic recurrence after more than 10 years (range, >10–23). The histological tumor type and grade were assigned according to the criteria of Elston and Ellis [35]. The clinicopathological characteristics of the patients and their cancers are summarized in Table 1. The Ethics Committee of the Helsinki University Central Hospital approved the study protocol.
Immunohistochemistry
Four-micrometer-thick sections were deparaffinized in xylene and rehydrated through a graded alcohol series. The slides for Bmi-1, c-myc, and Snail immunolabeling were then pretreated in a PT module (LabVision UK Ltd, UK) in Tris–HCl buffer (pH 8.5) for 20 min at 98°C and with 0.3% Dako REAL Peroxidase-Blocking Solution for 5 min to block endogenous peroxidase. Immunostaining was done by incubating each antibody for 1 hour, followed by 30-min incubation with Dako REAL EnVision/HRP secondary antibodies. The antibody clones, their dilutions, and the manufacturers are presented in Table 2. Bound antibodies were finally visualized by Dako REAL DAB + Chromogen reaction for 10 min. The slides were washed between each step with PBS 0.04%–Tween20. For ER, PR, Ki67, and HER2, antigen retrieval was done by microwaving in 10 mM citric acid monohydrate for 1 × 5 min at 900 W and for 3 × 5 min at 600 W. Endogenous peroxidase activity was blocked by treatment with 0.5% H2O2. The slides were incubated overnight in a refrigerator at +4°C with appropriate dilutions of the primary antibodies. The same procedure was used for negative controls, except that the incubation overnight took place in PBS diluent without antibody. The reaction was visualized by the Elite ABC Kit (Vectastain, Vector Laboratories, Burlingame, CA, USA) for ER and Ki67. PR and HER2 staining was performed using the Envision kit (Dako, Copenhagen, Denmark). The result was quantified as the proportion of positively stained tumor cells (range, 0–100%) for Bmi-1, c-myc, Snail, ER, PR, and Ki67. In Bmi-1, Snail, ER, PR, and Ki67, the staining was nuclear. Both nuclear and cytoplasmic stainings of c-myc were evaluated. The invasive front (frontal) and central areas of the tumors were scored separately for Snail. The immunohistochemistry (IHC) of HER2 expression was scored based on the intensity and percentage of positive cells, giving a score of 0 to 3+ [36]. Tumors giving a score of 2+ or 3+ were recorded positive. The 2+ and 3+ IHC HER2 positive cases were validated by chromogenic in situ hybridization (data not shown). We evaluated the entire tumor area in one representative section from the primary tumor and metastasis. The results were scored independently by two experienced pathologists (KJ and JH). When there was a discrepancy between evaluations, a consensus was made.
Statistical methods
All statistical analyses were performed using SPSS 13.0 for Windows (SPSS Inc., Chicago, IL, USA). The differences between the staining of primary tumors and their corresponding metastases were analyzed by the paired samples t test. Kruskal–Wallis and Mann–Whitney U tests were used for comparing the groups. For analyzing the relationship between protein expression of Bmi-1, c-myc, ER, Snail and the clinical parameters and also for compairing the Bmi-1, c-myc, and Snail with PR, HER2, and Ki67 expression, the categorical Pearson’s Chi-square test was used. As a cutoff point for positivity for Bmi-1 [5], c-myc [37, 38], ER, and PR, the frequency of 10% positive tumor cells was used. For Snail, the tumors were divided into high- and low-expressing groups, using 80% proportion of positively stained cells as a cutoff point [13]. Tumors were considered Ki67 positive, if ≥14% of the tumor cells showed positive nuclei [39]. Probability values of p < 0.05 were considered statistically significant, except in the Mann–Whitney U test, where p < 0.0167 (= < 0.05/3) was used.
Results
Bmi-1
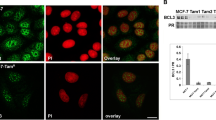
The expression of Bmi-1 in the groups is shown in Table 3. The metastases in groups 1 and 3 showed significantly more Bmi-1 (Fig. 1a, b) positivity than their corresponding primary tumors (p = 0.004 in group 1 and p = 0.019 in group 3, Table 3). The mean expression of Bmi-1 in the primary tumors did not differ between the three groups. In the metastases, there was significantly more Bmi-1 positivity in group 3 than in group 2 (p = 0.007; Table 4; Kruskal–Wallis test and p = 0.003; Table 5; Mann–Whitney U test).
Nuclear c-myc
The nuclear expression of c-myc in the tumor groups is shown in Table 3. In group 2, there was significantly more nuclear c-myc positivity in the metastases than in the corresponding primary tumors (p = 0.013; Table 3). There were no statistical differences in the nuclear expression of c-myc between the three groups (Table 4).
Cytoplasmic c-myc
The cytoplasmic expression of c-myc in the groups is shown in Table 3. There was significantly more expression of cytoplasmic c-myc (Fig. 1c and d) in the metastases of group 2 than in the corresponding primary tumors (p = 0.033; Table 3). The expression of cytoplasmic c-myc did not differ significantly between the three groups (Table 4).
Snail
Sometimes there was greater expression of Snail in frontal than in central areas of the tumor (Fig. 1e, f). Frontal and central Snail expression in the groups is shown in Table 3. The expression did not differ significantly between the primary tumors and their metastases in any of the three groups (Table 3). There was no statistical difference in Snail expression between the three groups (Table 4).
The relationship between Bmi-1, c-myc, Snail, ER protein, and clinical parameters
The significant results are shown in Table 6. For the analysis, the tumors were divided into positive and negative groups for Bmi-1, c-myc, and ER. For Snail, the tumors were divided into groups with high expression (≥80%) and low expression (<80%). These relations were evaluated in all primary tumors as one group (n = 73) and in all metastases as another group (n = 73). We also compared the protein expression of the primary tumors with axillary lymph node status. Comparisons were also made between tumor size, histological grade, type of tumor, and age of the patients (data not shown), but no positive correlation was seen.
Forty-eight (65%) of the primary cancers and 62 (84%) of their metastases were Bmi-1-positive. Bmi-1 positivity was associated with ER positivity in both the primary tumors and the metastases (p = 0.012 in primary tumors and p = 0.005 in metastases; Table 6). Bmi-1 positivity was associated significantly with high frontal and central Snail expression in the metastases (frontal Snail, p = 0.0001, central Snail, p = 0.009; Table 6). Bmi-1 expression was not associated with any of the analyzed clinical parameters.
There were 15 (20%) nuclear c-myc-positive tumors among the primary cancers and 19 (26%) in their corresponding metastases. Nuclear c-myc expression was not associated with the expression of the other proteins. Nuclear c-myc positivity of primary tumors was significantly associated with axillary node positivity of the patients (p = 0.021; Table 6).
Positivity for cytoplasmic c-myc was seen in 27 (37%) of the primary tumors and in 29 (39%) of the corresponding metastases. No association with clinical parameters was obtained. Cytoplasmic c-myc was associated with high frontal and central Snail in primary tumors (p = 0.002 and p = 0.011, respectively; Table 6).
Sixty (81%) of the primary tumors and 67 (91%) of their metastases expressed high frontal Snail. However, high frontal Snail expression (Fig.1) was not associated with any clinical parameters. High frontal Snail expression was associated significantly with Bmi-1 positivity in the metastases (p = 0.0001; Table 6), as mentioned above.
A high expression of central Snail was seen in 52 (70%) of the primary tumors and in 60 (81%) of the metastases. High central expression of Snail was not associated with any clinical parameters. High central Snail was associated with Bmi-1 in metastases (p = 0.009; Table 6), as mentioned above.
The relationship between Bmi-1, c-myc, Snail and PR, HER2 and Ki67
In primary tumors, there was a significant association between nuclear c-myc positivity and HER2 positivity (p = 0.017; Table 6). In metastases, there was no correlation between the expression of these antigens.
In conclusion, the expression of Bmi-1 was highest in metastases of the late (>10 years) relapsing tumor group. In all tumor groups, metastases expressed more Bmi-1 than did the primary tumors. Bmi-1 positivity correlated with ER positivity in both primary tumors and metastases. Nuclear expression of c-myc in the primary tumors was associated with a positive lymph node status of the patients. There was a tendency of higher, both nuclear and cytoplasmic, c-myc expression in the metastases of the late relapsing tumors than in their primary counterparts. In primary tumors, nuclear c-myc positivity correlated with HER2 positivity.
Discussion
In this study, we describe the expression of polycomb protein and oncogene Bmi-1, proto-oncogene c-myc, and transcription factor Snail in a series of 73 primary breast cancers and their corresponding metastases, from which 19 were early relapsing tumors and 54 late relapsing cancers (33 after 5 years and 21 after 10 years). Immunoexpression levels are compared between the primary tumors and their metastases, as well as between early and late relapsing tumors, and also with clinical parameters, in order to analyze their putative role in breast cancer progression.
A higher level of Bmi-1 expression has been reported during progression from in situ ductal breast carcinoma to invasive carcinoma linking Bmi-1 expression to malignant behavior [40]. In our study, we found metastases of breast cancer to express more Bmi-1 than the corresponding primary tumors. On the other hand, no such difference in Bmi-1 expression was detected in a melanoma study [41]. However, these tumors differ quite much since breast cancer is epithelial in origin whereas melanoma originates from melanocytes. We also found the highest level of Bmi-1 expression in the metastases of the very late relapsing tumors, suggesting that Bmi-1 is a marker of tumor cell dormancy [42].
The prognostic correlation studies of Bmi-1expression in breast cancer are contradictory, and association with both a poor as well as a favorable prognosis has been suggested [43]. We did not find Bmi-1 expression to correlate with lymph node metastasis or time of relapse. In our study, however, Bmi-1 positivity correlated significantly with ER expression both in the primary tumors and the metastases. Contrary to our findings, Feng et al. found a positive correlation between lymph node status and Bmi-1 expression, but no association between Bmi-1 and ER [43]. The differences between these results may be explained by the scoring method of positive cells. Feng et al. analyzed four randomly selected fields, while we evaluated the whole tumor area. In line with our results, Choi et al. [44] showed a favorable prognostic impact of Bmi-1 expression in breast cancer, but only in ER-positive patients, by evaluating the whole tumor area, the same way as we did.
Pavelic et al. [37] found heterogeneity in c-myc expression within individual tumors and substantial differences in the level of expression among different tumors. Andrechek et al. used a mouse model to study mammary carcinogenesis and found substantial heterogeneity in Myc-induced tumors, in terms of different gene expression and histological phenotypes [45]. We also found a different expression of c-myc between tumors, while we found a tendency of higher expression of both nuclear and cytoplasmic c-myc in the metastases of the late relapsing tumors than in their primary counterparts, suggesting that c-myc may be connected to tumor dormancy as well.
The significance of the different subcellular sites of c-myc staining, either nuclear, cytoplasmic or both, has not yet been clarified [37]. We speculate that active c-myc is located in the nucleus, where the transcription factors can operate. In our study, nuclear c-myc expression correlated significantly with axillary lymph node positivity. In agreement with our results, Rodriguez-Pinilla et al. found MYC amplification to be an independent predictor of lymph node metastasis [20]. On the contrary, some breast cancer studies have not found any correlation between c-myc expression and axillary lymph node status [46, 47]. The controversy may be due to the differences in the scoring methods. Locker et al. [48] did not find a correlation between axillary lymph node metastases and c-myc in their flow cytometric assay, but they reported that high levels of c-myc expression were found frequently in well-differentiated tumors.
No significant variability in Snail expression levels neither in the primary tumors nor in their metastases and no correlation to clinical parameters were found in our material. Contrary to our results, however, Snail expression has been shown to correlate inversely with the differentiation grade of breast tumors [31]. Come et al. analyzed the levels of Snail, Slug, and E-cadherin RNA expression and protein localization in large numbers of transformed cell lines and breast carcinomas, and they suggested that there is a link between Snail, Slug, and lymph node metastasis in mammary carcinomas. They detected a positive correlation between Snail expression and lymph node invasion by PCR [49]. We were unable to corroborate this association by immunohistochemistry. Instead, we found an association between high Snail expression and Bmi-1 in the metastases. This finding could be explained by a link between Snail and Bmi-1 function via E-cadherin. Bmi-1 expression has been shown to downregulate tumor suppressors, such as p16INK4a p14ARF, and cell adhesion molecules, such as E-cadherin [50]. Snail is essential for the EMT by downregulating the expression of cell adhesion and basement membrane proteins, most importantly cadherins [26].
In conclusion, we found higher Bmi-1 expression in breast cancer metastases than in primary tumors. The highest Bmi-1 expression was seen in the very late metastazing tumor group. These results suggest that small populations of Bmi-1-positive cells in the primary tumor survive long dormancy after primary therapy and retain their capacity for late relapsing. Our results also show an association of nuclear c-myc expression in primary tumors with axillary lymph node positivity, indicating nuclear c-myc expression to correlate with an increased risk for axillary lymph node metastasis.
References
van Lohuizen M, Verbeek S, Scheijen B, Wientjens E, van der Gulden H, Berns A (1991) Identification of cooperating oncogenes in Eμ-myc transgenic mice by provirus tagging. Cell 65(5):737–752
Haupt Y, Alexander WS, Barri G, Klinken SP, Adams JM (1991) Novel zinc finger gene implicated as myc collaborator by retrovirally accelerated lymphomagenesis in Eμ-myc transgenic mice. Cell 65(5):753–763
Satijn DP, Hamer KM, den Blaauwen J, Otte AP (2001) The polycomb group protein EED interacts with YY1 and both proteins induce neural tissue in Xenopus embryos. Mol Cell Biol 21(4):1360–1369
Jacobs JJ, Scheijen B, Voncken JW, Kieboom K, Berns A, van Lohuizen M (1999) Bmi-1 collaborates with c-Myc in tumorigenesis by inhibiting c-Myc-induced apoptosis via INK4a/ARF. Genes Dev 13(20):2678–2690
Kim JH, Yoon SY, Jeong SH, Kim SY, Moon SK, Joo JH, Lee Y, Choe IS, Kim JW (2004) Overexpression of Bmi-1 oncoprotein correlates with axillary lymph node metastases in invasive ductal breast cancer. Breast 13(5):383–388
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF (2006) Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A 100(7):3983–3988
Liu S, Dontu G, Mantle ID, Patel S, Ahn NS, Jackson KW, Suri P, Wicha MS (2006) Hedgehog signalling and Bmi-1 regulate self-renewal of normal and malignant human mammary stem cells. Cancer Res 66(12):6063–6071
Song LB, Zeng MS, Liao WT, Zhang L, Mo HY, Liu WL, Shao JY, Wu QL, Li MZ, Xia YF, Fu LW, Huang WL, Dimri GP, Band V, Zeng YX (2006) Bmi-1 is a novel molecular marker of nasopharyngeal carcinoma progression and immortalizes primary human nasopharyngeal epithelial cells. Cancer Res 66(12):6225–6232
Wang H, Pan K, Zhang HK, Weng DS, Zhou J, Li JJ, Huang W, Song HF, Chen MS, Xia J (2008) Increased polycomb-group oncogene Bmi-1 expression correlates with poor prognosis in hepatocellular carcinoma. J Cancer Res Clin Oncol 134(5):535–541
Häyry V, Tynninen O, Haapasalo HK, Wölfer J, Paulus W, Hasselblatt M, Sariola H, Paetau A, Sarna S, Niemelä M, Wartiovaara K, Nupponen NN (2008) Stem cell protein Bmi-1 is an independent marker for poor prognosis in oligodendroglial tumors. Neuropathol Appl Neurobiol 34(5):555–563
Leung C, Lingbeek M, Shakhova O, Liu J, Tanger E, Saremaslani P, van Lohuizen M, Marino S (2004) Bmi1 is essential for cerebellar development and is overexpressed in human medulloblastomas. Nature 428(6980):337–341
Vrzalikova K, Skarda J, Ehrmann J, Murray PG, Fridman E, Kopolovic J, Knizetova P, Hajduch M, Klein J, Kolek V, Radova L, Kolar Z (2008) Prognostic value of Bmi-1 oncoprotein in NSCLC patients: a tissue microarray study. J Cancer Res Clin Oncol 134(9):1037–1042
Häyry V, Mäkinen LK, Atula T, Sariola H, Mäkitie A, Leivo I, Keski-Säntti H, Lundin J, Haglund C, Hagström J (2010) Bmi-1 expression predicts prognosis in squamous cell carcinoma of the tongue. Br J Cancer 102(5):892–897
Bishop JM (1982) Retroviruses and cancer genes. Adv Cancer Res 37:1–32
Vennstrom B, Sheiness D, Zabielski J, Bishop JM (1982) Isolation and characterization of c-myc, a cellular homolog of the oncogene (v-myc) of avian myelocytomatosis virus strain 29. J Virol 42(3):773–779
Rabbits PH, Watson JV, Lamond A, Forster A, Stinson MA, Evan G, Fischer W, Atherton E, Sheppard R, Rabbitts TH (1985) Metabolism of c-myc gene products: c-myc mRNA and protein expression in the cell cycle. EMBO J 4(8):2009–2015
Harrington EA, Bennett MR, Fanidi A, Evan GI (1994) c-Myc-induced apoptosis in fibroblasts is inhibited by specific cytokines. EMBO J 13(14):3286–3295
Amundadottir LT, Johnson MD, Merlino G, Smith GH, Dickson RB (1995) Synergistic interaction of transforming growth factor alfa and c-myc in mouse mammary and salivary gland tumorigenesis. Cell Growth Differ 6(6):737–748
Pelengaris S, Khan M, Evan G (2002) c-MYC: more than just a matter of life and death. Nat Rev Cancer 2(10):764–776
Rodriguez-Pinilla SM, Jones RL, Lambros MB, Arriola E, Savage K, James M, Pinder SE, Reis-Filho JS (2007) MYC amplification in breast cancer: a chromogenic in situ hybridisation study. J Clin Pathol 60(9):1017–1023
Liao DJ, Dickson RB (2000) c-Myc in breast cancer. Endocr Relat Cancer 7(3):143–164
Deming SL, Nass SJ, Dickson RB, Trock BJ (2000) C-myc amplification in breast cancer: a meta-analysis of its occurrence and prognostic relevance. Br J Cancer 83(12):1688–1695
van Lohuizen M, Frasch M, Wientjens E, Berns A (1991) Sequence similarity between the mammalian bmi-1 proto-oncogene and Drosophila regulatory genes Psc and Su(z)2. Nature 353(6342):353–355
Haupt Y, Bath ML, Harris AW, Adams JM (1993) Bmi-1 transgene induces lymphomas and collaborates with myc in tumorigenesis. Oncogene 8(11):3161–3164
Levy LS, Lobelle-Rich PA, Overbaugh J (1993) Flvi-2, a target of retroviral insertional mutagenesis in feline thymic lymphosarcomas, encodes bmi-1. Oncogene 8(7):1833–1838
Batlle E, Sancho E, Francí C, Domínguez D, Monfar M, Baulida J, García De Herreros A (2000) The transcription factor Snail is a repressor of E-cadherin gene expression in epithelial tumor cells. Nat Cell Biol 2(2):84–89
Cano A, Pérez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, Portillo F, Nieto MA (2000) The transcription factor Snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol 2(2):76–83
Peinado H, Olmeda D, Cano A (2007) Snail, Zeb and bHLH factors in tumor progression: an alliance against the epithelial phenotype? Nat Rev Cancer 7(6):415–428
Cheng CW, Wu PE, Yu JC, Huang CS, Yue CT, Wu CW, Shen CY (2001) Mechanisms of inactivation of E-cadherin in breast carcinoma: modification of the two-hit hypothesis of tumor suppressor gene. Oncogene 20(29):3814–3823
Poser I, Domínguez D, de Herreros AG, Varnai A, Buettner R, Bosserhoff AK (2001) Loss of E-cadherin expression in melanoma cells involves up-regulation of the transcriptional repressor Snail. J Biol Chem 276(27):24661–24666
Blanco MJ, Moreno-Bueno G, Sarrio D, Locascio A, Cano A, Palacios J, Nieto MA (2002) Correlation of Snail expression with histological grade and lymph node status in breast carcinomas. Oncogene 21(20):3241–3246
Sugimachi K, Tanaka S, Kameyama T, Taguchi K, Aishima S, Shimada M, Sugimachi K, Tsuneyoshi M (2003) Transcriptional repressor Snail and progression of human hepatocellular carcinoma. Clin Cancer Res 9(7):2657–2664
Olmeda D, Moreno-Bueno G, Flores JM, Fabra A, Portillo F, Cano A (2007) SNAI1 is required for tumor growth and lymph node metastasis of human breast carcinoma MDA-MB-231 cells. Cancer Res 67(24):11721–11731
Joensuu K, Heikkilä P, Andersson LC (2008) Tumor dormancy: elevated expression of stanniocalcins in late relapsing breast cancer. Cancer Lett 265(1):76–83
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19(5):403–410
Wolff AC, Hammond ME, Schwarts JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal grwth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 131(1):18–43
Pavelic ZP, Pavelic K, Carter CP, Pavelic L (1992) Heterogeneity of c-myc expression in histologically similar infiltrating ductal carcinomas of the breast. J Cancer Res Clin Oncol 118(1):16–22
Pertschuk LP, Tobin EH, Tanapat P et al (1980) Histochemical analyses of steroid hormone receptors in breast and prostatic carcinoma. J Histochem Cytochem 28(8):799–810
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS, Perou CM, Ellis MJ, Nielsen TO (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101(10):736–750
Raaphorst FM, Meijer CJ, Fieret E, Blokzijl T, Mommers E, Buerger H, Packeisen J, Sewalt RA, Otte AP, van Diest PJ (2003) Poorly differentiated breast carcinoma is associated with increased expression of the human polycomb group EZH2 gene. Neoplasia 5(6):481–488
Mihic-Probst D, Kuster A, Kilgus S, Bode-Lesniewska B, Ingold-Heppner B, Leung C, Storz M, Seifert B, Marino S, Schraml P, Dummer R, Moch H (2007) Consistent expression of the stem cell renewal factor BMI-1 in primary and metastatic melanoma. Int J Cancer 121(8):1764–1770
Aguirre-Ghiso JA (2007) Models, mechanisms and clinical evidence for cancer dormancy. Nat Rev Cancer 7(11):834–846
Feng Y, Song LB, Guo BH, Liao WT, Li MZ, Liu WL, Zeng MS, Zhang L (2007) Expression and significance of Bmi-1 in breast cancer. Chin J of Cancer 26(2):154–157
Choi YJ, Choi YL, Cho EY, Shin YK, Sung KW, Hwang YK, Lee SJ, Kong G, Lee JE, Kim JS, Kim JH, Yang JH, Nam SJ (2009) Expression of Bmi-1 protein in tumor tissues is associated with favourable prognosis in breast cancer patients. Breast Cancer Res Treat 113(1):83–93
Andrechek ER, Cardiff RD, Chang JT, Gatza ML, Acharya CR, Potti A, Nevins JR (2009) Genetic heterogeneity of Myc-induced mammary tumors reflecting diverse phenotypes including metastatic potential. Proc Natl Acad Sci U S A 106(38):6387–16392
Spandidos DA, Yiagnisis M, Papadimitriou K, Field JK (1989) Ras, c-myc and c-erB-2 oncoproteins in human breast cancer. Anticancer Res 9(5):1385–1393
Pavelic ZP, Pavelic L, Lower EE, Gapany M, Gapany S, Barker EA, Preisler HD (1992) c-myc, c-erB-2, and Ki-67 expression in normal breast tissue and in invasive and non-invasive breast carcinoma. Cancer Res 52(9):2597–2602
Locker AP, Dowle CS, Ellis IO, Elston CW, Blamey RW, Sikora K, Evan G, Robins RA (1989) c-myc oncogene product expression and prognosis in operable breast cancer. Br J Cancer 60(5):669–672
Côme C, Magnino F, Bibeau F, De Santa BP, Becker KF, Theillet C, Savagner P (2006) Snail and slug play distinct roles during breast carcinoma progression. Clin Cancer Res 12(18):5395–5402
Song LB, Li J, Liao WT, Feng Y, Yu CP, Hu LJ, Kong QL, Xu LH, Zhang X, Liu WL, Li MZ, Zhang L, Kang TB, Fu LW, Huang WL, Xia YF, Tsao SW, Li M, Band V, Band H, Shi QH, Zeng YX, Zeng MS (2009) The polycomb group protein Bmi-1 represses the tumor suppressor PTEN and induces epithelial-mesenchymal transition in human nasopharyngeal epithelial cells. J Clin Invest 119(12):3626–3636
Acknowledgments
We thank Eija Heiliö, Päivi Peltokangas, and Tuire Koski for excellent technical assistance, Antti Nevanlinna for assistance with the statistics, and Doctor Aaron S. Mansfield for proofreading this manuscript. This work was supported by the Helsinki University Central Hospital Research Foundation, the Finnish Cancer Foundation, The Sigrid Juselius Foundation, and the Finnish Breast Cancer Group.
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Joensuu, K., Hagström, J., Leidenius, M. et al. Bmi-1, c-myc, and Snail expression in primary breast cancers and their metastases—elevated Bmi-1 expression in late breast cancer relapses. Virchows Arch 459, 31–39 (2011). https://doi.org/10.1007/s00428-011-1096-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-011-1096-8