Abstract
Promoter hypermethylation in precursor lesions of the breast cancer may be biomarkers of cancer risk and targets for cancer chemoprevention. Pi-class glutathione-S-transferases (GSTP1) is inactivated by promoter hypermethylation in invasive breast cancers. However, little is known about epigenetic silencing of GSTP1 gene by promoter hypermethylation in precursor lesions. To determine the significance of GSTP1 promoter hypermethylation in breast carcinogenesis, methylation status of GSTP1 gene was studied by nested methylation-specific polymerase chain reaction, and GSTP1 expression was studied by immunohistochemistry in invasive ductal carcinoma (IDC), ductal carcinoma in situ (DCIS), usual ductal hyperplasia (UDH), and normal breast tissue. GSTP1 promoter hypermethylation was detected in 4/24 (16.7%) of UDH, 18/49 (36.7%) of DCIS, and 14/36 (38.9%) of IDC. No hypermethylation was detected in normal breast tissues. GSTP1 promoter hypermethylation was found to be progressively elevated during breast carcinogenesis (p < 0.01). GSTP1 promoter hypermethylation was associated with loss of GSTP1 expression (p < 0.01 for UDH, p < 0.001 for DCIS and IDC). Our results suggest that GSTP1 promoter hypermethylation is an early event in breast carcinogenesis and appears to functionally silence GSTP1 expression. GSTP1 promoter hypermethylation in the precursor lesions of breast cancer may be used as a target for cancer chemoprevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The currently favored working hypothesis of breast cancer evolves in a linear progression through sequential stages of hyperplastic benign breast lesions with or without cellular atypia, carcinoma in situ, and ultimately, invasive cancer [2, 7]. Molecular studies have shown that numerous genetic alterations found in invasive cancer are also found with increased frequency during progression in this proposed continuum [5, 16, 25]. Inactivation of tumor suppressor genes by promoter hypermethylation has been considered as a potentially important mechanism involved in the development of breast cancer. It is generally assumed that breast cancer develops in a stepwise manner from normal breast epithelium towards cancer by the accumulation of epigenetic alterations [24].
Glutathione-S-transferases (GST) are an enzyme family that can detoxify reactive chemical species by catalyzing their conjugation to reduced glutathione [6]. Among the isoenzymes, the role of pi-class GST (GSTP1) is involved in the metabolism, detoxification, and elimination of potentially genotoxic foreign compounds and, thus, acts to protect cells from DNA damage and cancer initiation [13]. Previous studies have shown that the CpG-rich promoter regions are methylated in several types of human cancers [4, 23, 26]. GSTP1 promoter hypermethylation is also associated with loss of GSTP1 expression, as measured by immunohistochemistry [4, 26]. Previous studies have already investigated the methylation status of GSTP1 in invasive breast cancer [1, 8, 11, 19, 21]. Promoter hypermethylation of GSTP1 is associated with a poor prognosis of breast cancer [1]. However, little is known about epigenetic silencing of GSTP1 gene by promoter hypermethylation in the precursors of breast cancer. Consequently, the significance of alterations in GSTP1 promoter hypermethylation status during multistage carcinogenesis of the breast is not fully understood. Cancer chemoprevention can be defined as the prevention of cancer or treatment of identifiable precursors [22]. If GSTP1 promoter hypermethylation occurs in precursor lesions, then this opens new avenues for cancer chemoprevention based on the inhibition or reversal of epigenetic alterations before the onset of invasive breast cancer. Moreover, the detection of promoter hypermethylation in precursor lesions at risk for progression to invasive cancer paves the way for the use of DNA methylation markers in risk assessment.
To elucidate the role of GSTP1 in breast carcinogenesis, we have investigated the promoter methylation status of GSTP1 in normal breast tissues, usual ductal hyperplasia (UDH), ductal carcinoma in situ (DCIS), and invasive ductal carcinoma (IDC). We have also studied the expression of GSTP1 protein by immunohistochemistry and compared its expression with GSTP1 methylation status.
Materials and method
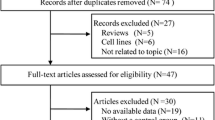
Tissues
A total of 124 breast specimens, representing 15 normal breast tissues, 24 UDH, 49 DCIS, and 36 IDC, not otherwise specified, were selected from the files of the Department of Pathology, Chonnam National University Hospital, Gwangju, South Korea. We only selected stage I IDC to rule out complex genetic alterations relating to metastasis.
Nested methylation-specific PCR
For DNA extraction, one 5-μm tissue section was deparaffinized with xylene. On a mirror-imaged hematoxylin–eosin stained slide, the region of interest was manually scraped off to ensure a specific cell population of more than 80% in the preparation. The scraped tissue extracted in 27 μl TNES (10 mM Tris, pH 8.0, 150 mM NaCl, 2 mM EDTA, 1% SDS) containing 3 μl proteinase K for 4 h at 52°C. The tissue extract was heat inactivated at 99°C for 10 min and clarified by centrifugation at 13,000 rpm for 30 s. Supernatant (13.5 μl) was used directly as a source of DNA for sodium bisulfite treatment. DNA was heated 10 min to 99°C, quick chilled, and incubated with 1.5 μl of 2 mol/l NaOH for 30 min at 42°C. Freshly prepared 3.6 mol/l sodium bisulfite containing 1 mmol/l hydroquinone was mixed with DNA, then overlaid with oil, and incubated at 55°C for 5 h in the dark. The sample was desalted using ion exchange columns (Amersham, Piscataway, NJ, USA). DNA was precipitated with 200-μl absolute alcohol, washed with 70% ethanol, air dried, and resuspended in water (20 μl). Samples were stored at −80°C until use.
To facilitate methylation-specific PCR (MSP) analysis on DNA retrieved from formalin-fixed, paraffin-embedded tissue, the methylation status of GSTP1 was analyzed by a nested, two-step PCR approach, as described previously, with slight modifications [18]. Step 1 of the nested MSP was performed to amplify a 303-bp fragment of the GSTP1 gene with primer sets flanking the CpG-rich promoter region. Hence, these primers did not discriminate between methylated and unmethylated nucleotides after bisulfite treatment. The primer sequences for step 1 were 5′-ATT TGG GAA AGA GGG AAA GGT-3′ as the forward and 5′-ACT AAA AAC TCT AAA CCC CAT C-3′ as the reverse. Reactions were carried out using the following conditions: 95°C for 5 min; then 36 cycles at 95°C for 30 s, 56°C for 30 s, and 72°C for 40 s; and a final extension step at 72°C for 5 min. A negative control for the assay (water only) and unmethylated (human sperm DNA) and methylated controls (MDA-MB-231 cells) were included in step 1 reactions.
PCR products from step 1 reactions were diluted 1:5 in water and subjected to the second step of MSP, which incorporated one set of primers (labeled as unmethylated or methylated) that were designed to recognize bisulfite-induced modifications of unmethylated cytosines. The sense and antisense primers for the methylated GSTP1 sequence were 5′-TTC GGG GTG TAG CGG TCG TC-3′ and 5′-GCC CCA ATA CTA AAT CAC GAC G-3′, respectively. The sense and antisense primers for the unmethylated sequence were 5′-GAT GTT TGG GGT GTA GTG GTT GTT-3′and 5′-CCA CCC CAA TAC TAA ATC ACA ACA-3′, respectively. The PCR amplification protocol for step 2 was as follows: 95°C for 5 min, then denature at 95°C for 30 s, anneal at 60°C for 30 s, extension at 72°C for 40 s for 30 cycles followed by a 5-min final extension. Primer sequences used in the step 2 amplification were previously described [8].
The PCR products were resolved by electrophoresis in a 2% agarose gel, and the ethidium bromide-stained PCR products were imaged with the Eagle Eye II Video System (Stratagene, La Jolla, CA, USA). Any tumor sample that reliably yielded a PCR product in the methylated reaction visible by ethidium bromide staining was considered positive for promoter hypermethylation.
Immunohistochemistry
Immunohistochemical analysis of GSTP1 protein expression in matching tissue sections was performed by applying the avidin–biotin–peroxidase complex method. Sections were deparaffinized and then were placed in a microwave oven with a 2.1% citric acid buffer solution (pH 6.0) for 10 min to retrieve the antigens. After microwave processing, the sections were incubated overnight at 4°C with primary anti-GSTP1 antibody (1:100 dilution, clone GSTpi, Novocastra, Burlingame, CA, USA). The streptavidin–horseradish peroxidase (Research Genetics, Huntsville, AL, USA) detection system was then applied, followed by 30 min of incubation at room temperature. After washing, the tissue sections were developed with a peroxidase substrate solution (3,3-diaminobenzidine tetrahydrochloride). The sections were counterstained with hematoxylin, dehydrated, and mounted. For negative controls, sections were treated similarly with the exception of the primary antibody.
GSTP1 expression was considered to be positive when >10% of cells exhibited cytoplasmic or nuclear staining [12].
Statistical analysis
The χ 2 test was used for group comparison. For the statistical analysis, a two-sided value of p < 0.05 was considered to indicate statistical significance. Data were analyzed using the SPSS software 11.5 for windows.
Results
Frequency of GSTP1 promoter hypermethylation
GSTP1 promoter hypermethylation was detected in 16.7% (4 of 24) of UDH, 36.7% (18 of 49) of DCIS, and 38.9% (14 of 36) of IDC samples. No hypermethylation was detected in normal breast tissues. Representative results of MSP assay are shown in Fig. 1. The frequency of GSTP1 promoter hypermethylation was found to be progressively increased along the continuum from normal breast tissue to IDC (p < 0.01). DCIS and IDC showed statistically higher frequency of GSTP1 promoter methylation compared to normal breast tissues (p < 0.01 and p < 0.01, respectively). Although not statistically significant, the incidence of GSTP1 promoter hypermethylation was higher in high nuclear grade DCIS: 18.2% (2 of 11) for grade 1, 35.3% (6 of 17) for grade 2, and 47.6% (10 of 21) for grade 3.
Representative results of nested methylation-specific PCR analysis for GSTP1 in breast carcinogenesis. Lanes U and M correspond to unmethylated and methylated DNA, respectively. DNA from human sperm (HS) and MDA-MB-231 (231) breast cancer cell line served as negative and positive controls for methylated genes, respectively. Water served as negative control for both unmethylated and methylated genes. N normal breast case; H usual ductal hyperplasia case; D ductal carcinoma in situ case; C invasive ductal carcinoma case
We also determined the association of risk factors, such as age, tumor grade, and estrogen receptor status with GSTP1 promoter hypermethylation in IDC. None of the risk factors showed significant association with promoter hypermethylation of GSTP1 (data not shown).
Immunohistochemical analysis of GSTP1
To determine whether the GSTP1 promoter hypermethylation was correlated with the loss of GSTP1 expression, immunohistochemical staining using an anti-GSTP1 antibody was carried out on all samples that were subjected to methylation analysis in this study. Representative results of GSTP1 immunohistochemistry are shown in Fig. 2. In all of the 15 normal breast tissues, mammary epithelium including myoepithelial cells showed both nuclear and cytoplasmic immunoreactivity for GSTP1. GSTP1 was also detected in non-epithelial cells (e.g., stromal cells and inflammatory cells). Loss of GSTP1 expression (negative) was observed in 8.3% of UDH, 49.0% of DCIS, and 41.7% of IDC. Strong staining was found in non-neoplastic breast tissues of all samples with UDH, DCIS, and IDC. When the GSTP1 expression was compared against the methylation status of GSTP1, GSTP1 expression was more frequently lost in breast tissues with methylation (p < 0.01 for UDH, p < 0.001 for DCIS and IDC; Table 1).
Positive and negative immunohistochemical staining of GSTP1 in normal breast tissue, UDH, DCIS, and IDC. Normal breast tissues show strong, diffuse nuclear and cytoplasmic staining representing a positive expression of GSTP1 (a and b). UDH (c), DCIS (e), and IDC (g) show strong positivity in unmethylated cases. In methylated UDH (d), DCIS (f), and IDC (h), loss of GSTP1 expression is observed. Adjacent non-neoplastic breast tissues show strong GSTP1 expression
Discussion
GSTP1 is known to play a role in detoxification of potential carcinogens [13]. Breast epithelial cells with lack the expression of GSTP1 is supposed to suffer from DNA damage more easily upon exposure to carcinogens. Loss of GSTP1 expression is observed in approximately two thirds of breast cancers, which indicates its potential role in breast carcinogenesis [1]. GSTP1 promoter hypermethylation appears likely to be responsible for absence of GSTP1 expression [4, 26]. Previous studies have described the significance of GSTP1 promoter hypermethylation in invasive breast cancer [1, 8, 11, 19, 21]. To determine when, in the breast carcinogenesis, promoter hypermethylation of the GSTP1 gene begins to play a role, we analyzed the promoter hypermethylation of GSTP1 in invasive breast cancer as well as its precursor lesions. We found out that GSTP1 promoter hypermethylation is an early event in breast carcinogenesis.
The frequency of GSTP1 promoter hypermethylation in IDC (38.9%) was found to be higher than reported previously. The frequency given in other studies of breast cancer varied between 13 and 30% [1, 8, 11, 19, 21]. The higher detection rate in our study might be due to the nested MSP. A PCR-based approach called MSP can detect 1 copy of methylated DNA in 1,000 unmethylated copies of genomic DNA [10]. We used nested MSP. This method is very sensitive and can detect 1 methylated allele in >50,000 unmethylated alleles [18].
Previous studies reported that GSTP1 promoter hypermethylation is associated with loss of GSTP1 protein expression, as measured by immunohistochemistry [1, 4, 26]. In this study, we have demonstrated a significant correlation between the promoter hypermethylation of GSTP1 and the data obtained from immunohistochemical analyses. Promoter hypermethylation of GSTP1 resulted in loss of GSTP1 protein expression in samples with methylation. These data provide evidence that GSTP1 promoter hypermethylation is a major mechanism involved in GSTP1 gene inactivation, resulting in impaired GSTP1 function during breast cancer development. While GSTP1 promoter hypermethylation status correlated well with GSTP1 expression, 21 cases of IDC and its precursors gave discordant data. The inconsistency between GSTP1 promoter hypermethylation and protein expression has been reported previously [1, 4, 8, 26]. Twenty-one cases can be divided into two groups: methylated and positive group (8 cases) and unmethylated and negative group (13 cases). The finding of GSTP1 hypermethylation in the fraction of IDC and its precursors that retained GSTP1 expression could be due to incomplete or low methylation. We used nested MSP. This is a very sensitive method, but it cannot distinguish high from low levels of promoter methylation. Using quantitative methylation analysis, Ogino et al. [17] found that tumors that show low levels of methylation in the gene promoters do not silence protein expression. GSTP1 unmethylated and negative group might be caused by mechanisms other than hypermethylation of GSTP1 promoter region. We concluded that GSTP1 is inactivated not only by promoter hypermethylation but also by other factors or mechanisms.
The potential reversibility of epigenetic states offers exciting opportunities for novel cancer drugs that can reactivate epigenetically silenced tumor suppressor genes. If epigenetic changes occur in precursor lesions of cancer, these changes may be targets for chemoprevention. GSTP1 detoxify carcinogens by conjugating them with glutathione. It is suggested that GSTP1 plays an important role in the prevention of the development of cancer upon exposure to carcinogens [13]. GSTP1 is a good candidate for cancer chemoprevention. To date, almost all of the studies on GSTP1 promoter hypermethylation have been analyzed in invasive breast cancer. To our knowledge, there are no data available about GSTP1 promoter hypermethylation in precursor lesions of breast cancer. In this study, promoter region of GSTP1 gene was methylated in 36.7% of DCIS and in 16.7% of UDH. However, GSTP1 promoter hypermethylation was not detected in normal breast tissues. Although not statistically significant, the incidence of GSTP1 promoter hypermethylation was higher in high nuclear grade DCIS. Loss of GSTP1 expression was observed in 49.0% of DCIS and in 17.7% of UDH. The data of GSTP1 immunohistochemistry in DCIS are consistent with previous report [3]. Promoter hypermethylation and loss of GSTP1 expression in DCIS and UDH provide opportunities for breast cancer prevention strategies including restoration of GSTP1 function via treatment with inhibition of promoter methylation.
Consistent with our results, previous studies reported the detection of promoter hypermethylation for other genes in tissue samples from precursor lesions of breast cancer [9, 14, 15]. The histologic appearance of precursor lesions is similar regardless of whether they progress or stabilize, suggesting that there may be morphologically silent molecular differences that result in progression, regression, or stabilization of these precursor lesions [2]. Promoter hypermethylation in precursor lesions can be used as a cancer risk marker. Promoter hypermethylation of p16, RUNX3, and HPP1 in Barrett’s esophagus or low-grade dysplasia was independently associated with an increased risk of progression of Barrett’s esophagus to high-grade dysplasia or esophageal adenocarcinoma [20]. It is presently unknown whether precursor lesions with GSTP1 promoter hypermethylation harbor an increased risk of malignant transformation. It would be interest to test in retrospective studies whether precursor lesions with and without promoter hypermethylation of GSTP1 may differ for the risk of developing invasive breast cancer.
In conclusion, we have shown that GSTP1 promoter hypermethylation occurred almost exclusively in IDC and its precursor lesions. GSTP1 promoter hypermethylation was found to be progressively elevated along the continuum from normal breast tissue to invasive breast cancer. GSTP1 promoter hypermethylation was associated with loss of GSTP1 expression. Our results suggest that GSTP1 promoter hypermethylation is an early event in breast carcinogenesis and appears to functionally silence GSTP1 expression. GSTP1 promoter hypermethylation in the precursor lesions of breast cancer may be used as a target for cancer chemoprevention and a cancer risk marker.
References
Arai T, Miyoshi Y, Kim SJ, Taguchi T, Tamaki Y, Noguchi S (2006) Association of GSTP1 CpG islands hypermethylation with poor prognosis in human breast cancers. Breast Cancer Res Treat 100:169–176
Arpino G, Laucirica R, Elledge RM (2005) Premalignant and in situ breast disease: biology and clinical implications. Ann Intern Med 43:446–457
Bellamy CO, Harrison DJ (1994) Evaluation of glutathione S-transferase pi in non-invasive ductal carcinoma of breast. Br J Cancer 69:183–185
Chan QK, Khoo US, Chan KY, Ngan HY, Li SS, Chiu PM, Man LS, Ip PP, Xue WC, Cheung AN (2005) Promoter methylation and differential expression of pi-class glutathione S-transferase in endometrial carcinoma. J Mol Diagn 7:8–16
Cho MH, Yoon JH, Jaegal YJ, Choi YD, Lee JS, Lee JH, Nam JH, Choi C, Lee MC, Park CS, Juhng SW, Min KW (2006) Expression of cyclooxygenase-2 in breast carcinogenesis and its relation to HER-2/neu and p53 protein expression in invasive ductal carcinoma. Breast 15:390–398
Coles BF, Kadlubar FF (2003) Detoxification of electrophilic compounds by glutathione S-transferase catalysis: determinants of individual response to chemical carcinogens and chemotherapeutic drugs? Biofactors 17:115–130
Dupont WD, Page DL (1985) Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med 312:146–151
Esteller M, Corn PG, Urena JM, Gabrielson E, Baylin SB, Herman JG (1998) Inactivation of glutathione S-transferase P1 gene by promoter hypermethylation in human neoplasia. Cancer Res 58:4515–4518
Fackler MJ, McVeigh M, Evron E, Garrett E, Mehrotra J, Polyak K, Sukumar S, Argani P (2003) DNA methylation of RASSF1A, HIN-1, RAR-beta, cyclin D2 and twist in in situ and invasive lobular breast carcinoma. Int J Cancer 107:970–975
Herman JG, Graff JR, Myohanen S, Nelkin BD, Baylin SB (1996) Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci USA 93:9821–9826
Hoque MO, Feng Q, Toure P, Dem A, Critchlow CW, Hawes SE, Wood T, Jeronimo C, Rosenbaum E, Stern J, Yu M, Trink B, Kiviat NB, Sidransky D (2006) Detection of aberrant methylation of four genes in plasma DNA for the detection of breast cancer.J Clin Oncol 24:4262–4269
Huang J, Tan PH, Thiyagarajan J, Bay BH (2003) Prognostic significance of glutathione S-transferase-pi in invasive breast cancer. Mod Path 16:558–565
Lee WH, Morton RA, Epstein JI, Brooks JD, Campbell PA, Bova GS, Hsieh WS, Isaacs WB, Nelson WG (1994) Cytidine methylation of regulatory sequences near the pi-class glutathione S-transferase gene accompanies human prostatic carcinogenesis. Proc Natl Acad Sci USA 91:11733–11737
Lehmann U, Langer F, Feist H, Glockner S, Hasemeier B, Kreipe H (2002) Quantitative assessment of promoter hypermethylation during breast cancer development. Am J Pathol 160:605–612
Lo PK, Mehrotra J, D’Costa A, Fackler MJ, Garrett-Mayer E, Argani P, Sukumar S (2006) Epigenetic suppression of secreted frizzled related protein 1 (SFRP1) expression in human breast cancer. Cancer Biol Ther 5:281–286
O’Connell P, Pekkel V, Fuqua SA, Osborne CK, Clark GM, Allred DC (1998) Analysis of loss of heterozygosity in 399 premalignant breast lesions at 15 genetic loci. J Natl Cancer Inst 90:697–703
Ogino S, Kawasaki T, Brahmandam M, Cantor M, Kirkner GJ, Spiegelman D, Makrigiorgos GM, Weisenberger DJ, Laird PW, Loda M, Fuchs CS (2006) Precision and performance characteristics of bisulfite conversion and real-time PCR (MethyLight) for quantitative DNA methylation analysis. J Mol Diagn 8:209–217
Palmisano WA, Divine KK, Saccomanno G, Gilliland FD, Baylin SB, Herman JG, Belinsky SA (2000) Predicting lung cancer by detecting aberrant promoter methylation in sputum. Cancer Res 60:5954–5958
Parrella P, Poeta ML, Gallo AP, Prencipe M, Scintu M, Apicella A, Rossiello R, Liguoro G, Seripa D, Gravina C, Rabitti C, Rinaldi M, Nicol T, Tommasi S, Paradiso A, Schittulli F, Altomare V, Fazio VM (2004) Nonrandom distribution of aberrant promoter methylation of cancer-related genes in sporadic breast tumors. Clin Cancer Res 10:5349–5354
Schulmann K, Sterian A, Berki A, Yin J, Sato F, Xu Y, Olaru A, Wang S, Mori Y, Deacu E, Hamilton J, Kan T, Krasna MJ, Beer DG, Pepe MS, Abraham JM, Feng Z, Schmiegel W, Greenwald BD, Meltzer SJ (2005) Inactivation of p16, RUNX3, and HPP1 occurs early in Barrett’s-associated neoplastic progression and predicts progression risk. Oncogene 24:4138–4148
Shinozaki M, Hoon DS, Giuliano AE, Hansen NM, Wang HJ, Turner R, Taback B (2005) Distinct hypermethylation profile of primary breast cancer is associated with sentinel lymph node metastasis. Clin Cancer Res 11:2156–2162
Steele VE, Kelloff GJ (2005) Development of cancer chemopreventive drugs based on mechanistic approaches. Mutat Res 591:16–23
Tokumaru Y, Harden SV, Sun DI, Yamashita K, Epstein JI, Sidransky D (2004) Optimal use of a panel of methylation markers with GSTP1 hypermethylation in the diagnosis of prostate adenocarcinoma. Clin Cancer Res 10:5518–5522
Widschwendter M, Jones PA (2002) DNA methylation and breast carcinogenesis. Oncogene 21:5462–5482
Yang C, Trent S, Ionescu-Tiba V, Lan L, Shioda T, Sgroi D, Schmidt EV (2006) Identification of cyclin D1- and estrogen-regulated genes contributing to breast carcinogenesis and progression. Cancer Res 66:11649–11658
Zhong S, Tang MW, Yeo W, Liu C, Lo YM, Johnson PJ (2002) Silencing of GSTP1 gene by CpG island DNA hypermethylation in HBV-associated hepatocellular carcinomas. Clin Cancer Res 8:1087–1092
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00428-007-0465-9
Rights and permissions
About this article
Cite this article
Lee, J.S. GSTP1 promoter hypermethylation is an early event in breast carcinogenesis. Virchows Arch 450, 637–642 (2007). https://doi.org/10.1007/s00428-007-0421-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-007-0421-8