Abstract
In addition to clinical and biological factors, further valuable prognostic information in neuroblastoma (Schwannian stroma-poor) (NB) patients is provided by the histopathologic analysis and the application of the International Neuroblastoma Pathology Classification (INPC) system. The objective of this study was to assess the prognostic impact of the INPC classification in a series of NB (Schwannian stroma-poor) and its relation with other prognostic factors. One hundred eighty-two cases of NB were collected from the files of the Spanish Neuroblastoma Registry. Slides were reviewed, and NB cases were grouped into favorable and unfavorable categories according to INPC criteria, taking into account morphological features (mitosis–karyorrhexis index, histological subtype) and patient’s age at diagnosis. Other pathological [presence of calcifications, tissular components, and number of mitotic cells per 10 high-power field (HPF)], immunohistochemical (P-glycoprotein and Ki-67 protein expression) and genetic (MYCN amplification and chromosome 1p deletion) features were also studied. Statistical analyses of overall survival with Kaplan–Meier curves and a multivariate study using Cox regression were performed (40.3% of NBs were considered favorable and 59.7% unfavorable). Unfavorable NB showed a mean survival time of 57 months compared with 89 months in favorable cases. Advanced stage, more than ten mitoses per 10 HPF, Ki-67 expression in more than 30% of tumor cells, MYCN oncogene amplification and chromosome 1p deletion were observed more frequently in unfavorable NB. The Cox regression analysis demonstrated that clinical stage (International Neuroblastoma Staging System stage 4) and histological subtype (undifferentiated NB) were the most important factors that influence the overall survival (p<0.001). INPC classification results are major prognostic indicators in NB and should be considered in the therapeutic stratification of NB patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Classically, neuroblastoma (NB) (Schwannian stroma-poor) prognosis is based on two clinical parameters: patient’s age at diagnosis and tumor stage [7]. Several established molecular prognostic parameters, such as DNA content (ploidy) [39], MYCN oncogene amplification [45], allelic loss in the short arm of chromosome 1 (1p) [15], and gain of genetic material in chromosome 17 [4, 10], have been progressively introduced as further prognostic indicators. Telomerase activity is being analyzed as a strong new prognostic molecular parameter in NB [42, 43].
Valuable prognostic information is also provided by the histopathologic analyses. Shimada et al. [49] proposed a classification system for neuroblastic tumors based on the proportion of Schwannian stroma, with a prognostic categorization in favorable or unfavorable subgroups, combining morphological features with the patient’s age at diagnosis. Subsequently, Joshi et al. [31, 32] proposed a different age-linked prognostic categorization of NB into two risk groups supported by a new histological grading system, which was later modified [34]. Finally, the system of Shimada et al. [49] was adapted by the International Neuroblastoma Pathology Committee to elaborate on the International Neuroblastoma Pathology Classification (INPC) [47, 48], which standardized a terminology and morphological criteria to classify neuroblastic tumors with prognostic significance.
The immunohistochemical procedures allow the consideration of additional features with actual prognostic value in NB such as P-glycoprotein (the product of the multidrug resistance gene, MDR-1) [13] and the overexpression of the neural growth factor receptor-associated protein Trk-A [5]. The determination of cell proliferation markers such as Ki-67 protein also provides prognostic information on these tumors [44].
In this paper, we review the morphological features of 182 NBs (Schwannian stroma-poor) collected from the files of the Spanish Neuroblastoma Registry, applying the INPC criteria, with the aim of assessing the prognostic impact of this classification and its relation with other clinical, morphological, and biological prognostic factors.
Materials and methods
In this study, 209 NBs (Schwannian stroma-poor) with pathologically valuable material were retrieved from the files of the Spanish Neuroblastoma Registry. The cases were collected between January 1992 and December 1999 from the 26 hospitals enrolled in the Spanish Cooperative Neuroblastoma Study N-II-92 [12]. Each case was diagnosed and staged in accordance with the International Neuroblastoma Staging System (INSS) [6, 7]. Samples of fresh and frozen tumor tissue from the primary tumor or a metastatic site (if it was not available for the primary tumor) were submitted to this reference laboratory. Tumor specimens taken after chemotherapy were excluded from the study. Clinical data from each patient were collected, including sex, date of birth, age at diagnosis, tumor location, INSS stage, clinical follow-up, and final outcome (data available for 182 patients). The cutoff date for the study was June 2000.
Histopathologic analysis
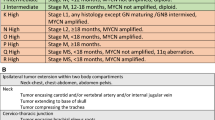
Standard procedures were used to prepare hematoxylin-eosin (H&E) sections after paraffin embedding of tumor tissue fixed in 10% buffered formaldehyde. All slides in each tumor were examined by two of the authors with no knowledge of either clinical or genetic abnormalities, and the histological diagnosis based on INPC recommendations [47] was established. The mitosis–karyorrhexis index (MKI) was determined in each tumor according to INPC criteria. Patient’s age was taken into account to classify each case into a prognostic subset, favorable or unfavorable, following INPC prognostic categorization [48] (Table 1). Other morphological features considered were the diverse parameter of tissular components found in the slides: percentage of viable tumor cells, percentage of Schwannian stroma, percentage of necrotic tissue (including hemorrhagic and calcified areas) and percentage of other elements (including inflammatory cells, normal tissue, and non-Schwannian stroma), the presence of tumor calcifications, and the number of mitotic cells per 10 HPF.
Immunohistochemical expression of Ki-67 protein (MIB-1; Immunotech; 1:50) was analyzed in all cases following the streptavidin–biotin peroxidase method (LSAB, DAKO) [22]. Antigen retrieval was obtained with microwave heating in a solution of citrate buffer (pH 6). The same technique was performed to assess P-glycoprotein expression using the monoclonal antibody JSB-1 (Centocor; 1:50).
Genetic studies
MYCN oncogene amplification was determined in all cases by means of Southern blot analysis of total DNA extracted from frozen tumor samples and fluorescence in situ hybridization (FISH) analysis with a DNA probe [N-myc (2p24) red/Alphasatellite 2 Dual-Color, Q-Biogene/mpbio]. To study chromosome 1 status, FISH analysis was performed on tumor touch imprints in 72 NBs using a chromosome 1 centromeric (1p36 Midi Satellite Probe; green, Q-Biogene/mpbio) and subtelomeric [Chr.1 Classical Satellite (1qh), red, Q-Biogene/mpbio] probe by means of standardized methods [2]. The number of signals was counted in 100 tumor cell nuclei.
Statistical analysis
All clinical, morphological, and biological data obtained for each case were filed in a computerized database. A descriptive analysis was performed for each variable included, and associations among these variables were analyzed using the appropriate statistical method (χ 2, Mann–Whitney test, and Kruskal–Wallis test). The Kaplan–Meier method was used to estimate survival rates, and multivariate study using Cox regression procedure was performed. p values ≤0.05 were regarded as statistically significant.
Results
Analysis of clinical, biological, and morphological features and their influence on patient’s outcome and survival
The clinical, morphological, and biological features of tumors with known follow-up data are listed in Table 2, which also includes the results for their final outcome, p value for bivariate analysis, and statistical test used. Information on the clinical course of 182 patients was available: 135 (74.2%) were alive at the last follow-up, whereas 47 (25.8%) had died of the disease or as a complication of the treatment. Mean observation time was 33.54 months. The 3-year estimated survival rate was 72.9%, with a mean survival rate of 73 months.
The mean age at the moment of diagnosis was 20.5 months. Patients younger than 18 months presented a better outcome and a more prolonged survival (87 months) than older ones. The intermediate age group (1.5–5 years) had the worst survival (44 months), and 51.9% of the patients were dead. Mean age at diagnosis in patients who remained alive was 17 months, nearly half of the patients who died (31.3 months).
Tumors presented in all stages. The number of deaths increased significantly with higher stages. With a mean survival rate of 35 months, 59.3% of INSS stage 4 patients were dead. Behavior of INSS stage 4s NBs was similar to INSS stage 1 tumors (Fig. 1).
MYCN amplification was observed in 29 NBs (16.7%) and was significantly associated with a worse outcome (58.6% were dead) and shorter survival (40 months) than patients without amplification of the gene (17.2% were dead; mean survival, 79 months). By FISH analysis, 27.3% of the NBs studied showed loss of genetic material in the short arm of chromosome 1, a feature that was also related with patient outcome and survival: 44.4% of the patients with this alteration died, with a mean survival rate of 32 months, in contrast to patients without 1p deletion, who for the most part remained alive (87.5%) (mean survival rate, 74 months). All 12 tumors with MYCN amplification in which chromosome 1 was analyzed showed loss of genetic material. INSS stage data were available in 11 of them: 8 (72.7%) were stage 4 tumors, and 3 (27.3%) were stage 3. All but one (91.7%) showed a high MKI. Clinical follow-up information was available in nine of them, and seven (77.8%) were dead.
The immunohistochemical expression of P-glycoprotein was found in 10.3% of 156 NBs analyzed. The percentage of dead patients in the group with P-glycoprotein expression (31.3%) was higher than in the negative group (25.7%), but differences were not statistically significant.
Morphological features
According to the INPC diagnostic criteria, 111 (61%) tumors were diagnosed as poorly differentiated NB (PD-NB), 35 (19.2%) as undifferentiated NB (U-NB), and 12 (6.6%) as differentiating NB (D-NB). The remaining 24 (13.2%) cases were tumors with a definitive generic diagnosis of NB, but in which the subtype was impossible to determine because of the paucity of tumor cells or the degree of artifact. These last cases fit into the not otherwise specified (NOS-NB) category. A sample of each subtype is showed on (Fig. 2).
Nearly two-thirds (62.9%) of U-NBs with clinical follow-up had a fatal outcome, with a mean survival rate of 33 months, significantly shorter than in the other subtypes (58–81 months). The best outcome was for D-NB, with only one (8.3%) dead patient. Behavior of tumors regarded as “NOS” was similar to PD-NB, with less than 20% of dead patients (18% in PD-NB, 16.7% in NOS-NB) and a mean survival rate of 80 months (Fig. 3).
Necrosis was significantly related to a higher proportion of dead patients (15.4% in tumors with necrosis vs 8% in tumors without this feature). Inversely, the presence of Schwann cells was associated with a better outcome. A high MKI, more than 6 mitoses per 10 HPF, or Ki-67 expression in more than 30% of tumor cells were features that determined a significant rise in the proportion of dead patients, with a concomitant drop in the mean survival time. We found no differences in outcome between patients whose tumors showed a low or intermediate MKI, most of them (87.9% with low MKI, 85.3% with intermediate MKI) remaining alive at last follow-up.
Multivariate analysis
Tumor stage and histological subtype of NB were the factors having a highly significant influence on survival rate. Moreover, INSS stage 4 and undifferentiated subtype of NB were the features with a more negative effect over hazard rate compared with the remaining stages and histological subtypes. Results of the Cox regression procedure are resumed in Table 3.
Relations between histological subtype of NB and other clinical, morphological, and biological parameters
Poorly differentiated NB and NOS-NB were diagnosed frequently in the first 18 months of life (70%). In contrast, 60% of D-NBs and 63.2% of U-NBs were diagnosed in children older than 1.5 years.
Nearly two thirds of the U-NBs (63.2%) presented as disseminated (INSS stage 4) tumors, whereas PD-NBs and D-NBs were usually localized (INSS stages 1 and 2). Most INSS stage 4s tumors were PD-NBs (66.7%).
The presence of Schwann cells was only significant in D-NB, reaching a mean proportion of 10.3% in this subtype. On the contrary, necrosis was rare in these tumors (2.3%), but reached a mean proportion of 18.2% in slides from U-NB. Tumor calcifications were related to the degree of differentiation of NB, being detected in 60% of D-NBs but in only 18.4% of U-NBs. The proliferative activity offered marked differences among the NB subtypes, being significantly higher in U-NB compared with the remaining categories. With detail, 72.7% of U-NBs showed a high MKI, more than 10 mitoses were found in 62.5% of them, and Ki-67 nuclear labeling reached a mean percentage of 47.6%. In contrast, D-NBs showed a low MKI (86.7%), less than 5 mitoses (93.3%), and a mean percentage of Ki-67 nuclear labeling of 11.8%.
MYCN oncogene amplification and 1p deletion were found significantly more frequently among U-NB than in remaining subtypes: 45.9% of these tumors showed MYCN amplification, but this feature was found in 16% of NOS-NBs, 9% of PD-NBs, and none in D-NB. 1p deletion was present in seven (70%) of 10 U-NBs, but in only 20–22% in the remaining categories. We could not find any significant differences on P-glycoprotein expression with regard to the histological subtype of NB.
Analysis of the prognostic INPC categorization
Following the INPC criteria, we established the favorable or unfavorable category in 162 patients with available follow-up data. Of the 162 patients, 39.5% of them fitted into the favorable group, whereas the remaining 60.5% were considered as unfavorable. We found an evident association between the prognostic group and outcome: most patients (93.8%) in the favorable group remained alive at last follow-up (Fig. 4), and their mean survival rate (89 months) was significantly higher than those in the unfavorable group (57 months) (Fig. 5). The INPC prognostic system offered a high sensitivity (90.9%), with most of the dead patients located in the unfavorable group (40 of 44 dead patients). However, specificity of this prognostic scheme was low (50.8%) because in this series, half of the patients regarded as unfavorable remained alive at last follow-up.
The tumor stage was significantly related to INPC prognosis. Progression in stage implied a higher proportion of unfavorable cases, which reached 89.3% in INSS stage 4 tumors. Results for INSS stage 4s tumors were similar to those of INSS stage 1 tumors, with two thirds of the cases categorized as favorable (65.2% in stage 1; 68.4% in stage 4s).
Regarding the histological composition of the samples, only the proportion of Schwann cells was significantly higher among favorable tumors. The proportion of favorable cases was higher among tumors in which calcifications were found (48.3% vs 36.5% of INPC favorable tumors in the group without calcifications), but differences were not significant.
Tumors with less than five mitoses per 10 HPF were mainly classified as favorable (70.9%), whereas nearly all tumors (98.2%) with more than ten mitoses per 10 HPF belonged to the unfavorable group. The Ki-67 nuclear expression reached a mean value of 40% in unfavorable cases, significantly higher than the mean expression found in favorable tumors (15.8%). In fact, most cases (96.5%) with Ki-67 nuclear expression in more than 30% of tumor cells fell into the unfavorable group.
The presence of MYCN gene amplification or 1p deletion was significantly related to INPC prognosis. Nearly all tumors with MYCN gene amplification were in the unfavorable group (93.1%), the same as for NB showing 1p deletion (84.2% of tumors classified as unfavorable).
Discussion
It has been assumed that NB follows a maturative sequence characterized by a progressive differentiation of tumor cells together with the development of stroma composed mainly of Schwann cells [30, 46]. First attempts to establish a classification of these tumors considered cell differentiation as the main morphological parameter with prognostic value [3, 28, 40]. Tumor cell differentiation and development of Schwannian stroma were the basis for the classification system and age-linked prognostic categorization proposed by Shimada et al. [49], whose prognostic value was confirmed in subsequent reports [14, 33]. This model was adapted and modified by the International Neuroblastoma Pathology Committee to establish a standard terminology and morphological criteria for the diagnosis of NB, offering a reproducible classification system (the INPC system) that has prognostic value and biological relevance [47, 48].
In this article, we have reviewed 182 NBs (Schwannian stroma-poor) collected from the files of the Spanish Neuroblastoma Registry focusing on pathological features. The INPC diagnostic and prognostic system was applied with the aim of assessing the true prognostic value of this system in our series and its relation with other prognostic factors.
We found patient outcome to be related with histological subtype of NB in such a way that U-NB had a death rate significantly higher than in the other subtypes, and their mean survival time was cut in half. Using a multivariate analysis (Cox regression), the histological subtype of NB was the second most influential factor on survival, closely following tumor stage. INSS stage 4 and undifferentiated histology were the features with a more negative effect on hazard rate.
Tumor necrosis has been related to a worse prognosis in NB [14]. In this series, the proportion of dead patients was significantly higher among tumors with necrosis, which mainly fit into the undifferentiated or “NOS” category. In contrast, the presence of Schwann cells has been related with a better outcome in NB [47, 48]. We found a better outcome for patients whose tumors contained Schwann cells, but this cell type was practically restricted to D-NB. Tumor calcifications have an uncertain biologic significance in NB, but they have been related to a better prognosis in some reports [14, 32], including the INPC report [47]. In our series, they appeared significantly more frequently in D-NB, but differences in outcome with regard to their presence were not significant.
Joshi et al. [32] proposed a grading system for NB based on mitotic rate and the presence of calcifications, these being the morphological factors found to have more impact on prognosis. In our series, mitotic count was significantly related to patient’s outcome in such a way that more than six mitoses per 10 HPF implied a remarkable rise in death rate, which was 42% in tumors with more than ten mitoses per 10 HPF. We found mitotic rate to be also related to the histological subtype of NB, being especially high in U-NB. Assessment of mitotic rate in NB can be difficult in practice because of the resemblance of mitotic and karyorrhectic cells. For this reason, the MKI was proposed. These data are obtained from the sum of mitotic and karyorrhectic figures out of 5,000 tumor cells [49]. MKI was one of the features that determined the prognosis in the original Shimada system and, after subsequent reports confirmed its prognostic value [31], it has been maintained as a prognostic factor in the INPC system [48]. In our series, high MKI tumors had a death rate close to 50%, whereas most patients with low or medium MKI tumors remained alive at last follow-up and had a significantly higher mean survival rate. Almost all D-NBs showed a low MKI, whereas this index was high in most U-NBs. Ki-67 protein is an excellent marker for assessing the proliferative activity in tissue [9]. We found significant differences in patient outcome and survival with regard to mean nuclear Ki-67 expression, to the effect that death rate increased markedly when expression was 30% or higher, with a concomitant decrease in mean survival time. In previous reports, low Ki-67 protein expression in NB was related to a better prognosis [24, 44]. U-NB showed a high Ki-67 protein expression (mean value near 50%), significantly higher than in PD-NB and in D-NB (lower than 30%).
Recently, some reports have described prominent nucleoli to be a sign of unfavorable tumor biology and MYCN amplification in U-NB and PD-NB [1, 37]. We are reviewing the slides collected in the Spanish Neuroblastoma Registry to evaluate this parameter (manuscript in preparation).
It is well established that NB of any stage diagnosed in infants have a better prognosis than those diagnosed in children at the same stage [17, 19, 25, 29]. In fact, the main NB prognostic categorization schemes based on morphological parameters were age-linked systems [32, 48, 49].
Tumor stage is also an independent prognostic factor in NB: localized tumors have longer survival rates than disseminated ones [17, 19]. In the multivariate analysis, we found that INSS stage 4 was the parameter with a more negative effect on hazard rate. U-NB appeared as disseminated tumors in the majority of patients, similar to those categorized as NOS, whereas localized tumors predominated among PD-NB and D-NB. INSS stage 4s tumors represented 10% of all NB in our series, a similar proportion to that previously reported [18, 29], and for the most part, they fit into the PD-NB category.
MYCN gene amplification correlates with poor prognosis in NB [8, 16, 20, 45, 52]. We confirmed this fact in our series, in that almost 60% of the patients with MYCN-amplified tumors were deceased, and moreover, we also found a clear relation between this alteration and the histological subtype of NB. MYCN gene amplification appeared in half of the U-NB cases. Previous reports described the presence of a typical phenotype in these amplified NB, being for the most part undifferentiated stroma-poor tumors with a high proliferative activity [21, 38, 50, 52].
Only 72 tumors in our series were studied by means of FISH analysis to assess chromosome 1p status, deletion being found in 28% of them. As has been previously reported [11, 15, 20, 27, 35], del 1p was related to a worse outcome and a shorter survival rate. We detected this alteration in 70% of the U-NB.
We have classified NB into favorable or unfavorable groups according to the INPC prognostic system. INPC prognosis was significantly related to patient’s outcome in such a way that most patients in the favorable group remained alive at last follow-up, whereas the proportion of dead patients was high in the unfavorable group. Mean survival rate for favorable patients was significantly higher than that of unfavorable patients. The INPC prognostic system had a high sensitivity in this series (90.9%): most of the dead patients were in the unfavorable group. However, the specificity of this system was low (50.8%) because half of the patients classified as unfavorable remained alive at last follow-up. The prognostic value of the INPC system has been confirmed in several reports [1, 23, 38, 51]. Recently, the Localised Neuroblastoma European Study Group (LNESG) have shown that the INPC prognostic categorization has a significant impact on outcome prediction in INSS stage 2 localized peripheral NB [41].
In addition to factors that determine INPC prognosis (histological type, MKI, and patient’s age at diagnosis), we have found significant associations between the prognostic group and other clinical, morphological, and biological parameters. Progress in the tumor stage is associated with a rise in the proportion of unfavorable cases. Results for INSS stage 4s tumors were similar to those of stage 1 NB and, as is described in the literature, most of them were tumors with favorable features [26, 36]. The rise in mitotic count or in Ki-67 protein labeling index also implied a higher proportion of unfavorable cases. We found MYCN gene amplification and 1p deletion to be significantly more frequent in the unfavorable group. Nearly all tumors with one of these alterations were located in the unfavorable group.
Based upon the present analysis, we can state that, although molecular biology studies have an increasing significance, the histopathologic study is still an important procedure in the study of NB and provides valuable prognostic information. We have confirmed the high sensitivity of the INPC prognostic system, observing that NB in the unfavorable group displays a worse outcome. We have also corroborated the association of clinical, morphological, and biological parameters with their clinical outcome. In this series, NB located in the unfavorable group presented features related to a worse prognosis, INSS stage 4 and undifferentiated histology being the features with a more negative impact on survival.
References
Ambros IM, Hata H, Joshi VV, Roald B, Dehner LP, Tüchler H, Pötschger U, Shimada H (2002) Morphologic features of neuroblastoma (Schwannian stroma-poor tumors) in clinically favorable and unfavorable groups. Cancer 94:1574–1583
Ambros PF, Ambros IM (2001) Pathology and biology guidelines for resectable and unresectable neuroblastic tumors and bone marrow examination guidelines. Med Pediatr Oncol 37:492–504
Beckwith JB, Martin RF (1968) Observations on the histopathology of neuroblastomas. J Pediatr Surg 3:106–110
Brinkschmidt C, Poremba C, Christiansen H, Simon R, Schafer KL, Terpe HJ, Lampert F, Boecker W, Dockhorn-Dworniczak B (1998) Comparative genomic hybridization and telomerase activity analysis identify two biologically different groups of 4s neuroblastomas. Br J Cancer 77:2223–2229
Brodeur GM (1993) TRK-A expression in neuroblastomas: a new prognostic marker with biological and clinical significance (editorial). J Natl Cancer Inst 85:344–345
Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castleberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F, Kaneko M, Kemshead J, Lampert F, Lee R, Look AT, Pearson AD, Philip T, Roald B, Sawada T, Seeger RC, Tsuchida Y, Voute PA (1993) Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol 11:1466–1477
Brodeur GM, Seeger RC, Barrett A, Berthold F, Castleberry RP, D’Angio G, De Bernardi B, Evans AE, Favrot M, Freeman AI, Haase G, Hartmann O, Hayes FA, Helson L, Kemshead J, Lampert F, Ninane J, Ohkawa H, Philip T, Pinkerton CR, Pritchard J, Sawada T, Siegel S, Smith EI, Tsuchida Y, Voute PA (1988) International criteria for diagnosis, staging, and response to treatment in patients with neuroblastoma. J Clin Oncol 6:1874–1881
Brodeur GM, Seeger RC, Schwab M, Varmus HE, Bishop JM (1984) Amplification of N-myc in untreated human neuroblastomas correlates with advanced disease stage. Science 224:1121–1124
Brown DC, Gatter KC (1990) Monoclonal antibody Ki-67: its use in histopathology. Histopathology 17:489–503
Caron H (1995) Allelic loss of chromosome 1 and additional chromosome 17 material are both unfavourable prognostic markers in neuroblastoma. Med Pediatr Oncol 24:215–221
Caron H, Van Sluis P, De Kraker J, Bökkerink J, Egeler M, Laureys G, Slater R, Westerveld A, Voute PA, Versteeg R (1996) Allelic loss of chromosome 1p as a predictor of unfavorable outcome in patients with neuroblastoma. N Engl J Med 334:225–230
Castel V, Garcia-Miguel P, Melero C, Navajas A, Navarro S, Molina J, Badal MD, Ruiz-Jimenez JI (1995) The treatment of advanced neuroblastoma. Results of the Spanish Neuroblastoma Study Group (SNSG) studies. Eur J Cancer 31A:642–645
Chan HS, Haddad G, Thorner PS, DeBoer G, Lin YP, Ondrusek N, Yeger H, Ling V (1991) P-Glycoprotein expression as a predictor of the outcome of therapy for neuroblastoma. N Engl J Med 325:1608–1614
Chatten J, Shimada H, Sather HN, Wong KY, Siegel SE, Hammond GD (1988) Prognostic value of histopathology in advanced neuroblastoma: a report from the Childrens Cancer Study Group. Hum Pathol 19:1187–1198
Christiansen H, Lampert F (1988) Tumour karyotype discriminates between good and bad prognostic outcome in neuroblastoma. Br J Cancer 57:121–126
Christiansen H, Sahin K, Berthold F, Hero B, Terpe H-J, Lampert F (1995) Comparison of DNA aneuploidy, chromosome 1 abnormalities, MYCN amplification and CD44 expression as prognostic factors in neuroblastoma. Eur J Cancer 31A:541–544
Coldman AJ, Fryer CJ, Elwood JM, Sonley MJ (1980) Neuroblastoma: influence of age at diagnosis, stage, tumor site, and sex on prognosis. Cancer 46:1896–1901
Evans AE, Chatten J, D’Angio GJ, Gerson JM, Robinson J, Schnaufer L (1980) A review of 17 IV-S neuroblastoma patients at the children’s hospital of Philadelphia. Cancer 45:833–839
Evans AE, D’Angio GJ, Propert K, Anderson J, Hann HW (1987) Prognostic factors in neuroblastoma. Cancer 59:1853–1859
Fong CT, White PS, Peterson K, Sapienza C, Cavenee WK, Kern SE, Vogelstein B, Cantor AB, Look AT, Brodeur GM (1992) Loss of heterozygosity for chromosomes 1 or 14 defines subsets of advanced neuroblastomas. Cancer Res 52:1780–1785
George RE, Variend S, Cullinane C, Cotterill SJ, McGuckin AG, Ellershaw C, Lunec J, Pearson AD (2001) Relationship between histopathological features, MYCN amplification, and prognosis: a UKCCSG study. United Kingdom Children Cancer Study Group. Med Pediatr Oncol 36:169–176
Giorno R (1984) A comparison of two immunoperoxidase staining methods based on the avidin–biotin interaction. Diagn Immunol 2:161–165
Goto S, Umehara S, Gerbing RB, Stram DO, Brodeur GM, Seeger RC, Lukens JN, Matthay KK, Shimada H (2001) Histopathology (International Neuroblastoma Pathology Classification) and MYCN status in patients with peripheral neuroblastic tumors: a report from the Children’s Cancer Group. Cancer 92:2699–2708
Graham D, Magee H, Kierce B, Ball R, Dervan P, O’Meara A (1995) Evaluation of Ki-67 reactivity in neuroblastoma using paraffin embedded tissue. Pathol Res Pract 191:87–91
Grosfeld JL, Schatzlein M, Ballantine TV, Weetman RM, Baehner RL (1978) Metastatic neuroblastoma: factors influencing survival. J Pediatr Surg 13:59–65
Hachitanda Y, Hata J (1996) Stage IVS neuroblastoma: a clinical, histological, and biological analysis of 45 cases. Hum Pathol 27:1135–1138
Hayashi Y, Kanda N, Inaba T, Hanada R, Nagahara N, Muchi H, Yamamoto K (1989) Cytogenetic findings and prognosis in neuroblastoma with emphasis on marker chromosome 1. Cancer 63:126–132
Hughes M, Marsden HB, Palmer MK (1974) Histologic patterns of neuroblastoma related to prognosis and clinical staging. Cancer 34:1706–1711
Jereb B, Bretsky SS, Vogel R, Helson L (1984) Age and prognosis in neuroblastoma. Review of 112 patients younger than 2 years. Am J Pediatr Hematol Oncol 6:233–243
Joshi VV (2000) Peripheral neuroblastic tumors: pathologic classification based on recommendations of international neuroblastoma pathology committee (modification of Shimada classification). Pediatr Dev Pathol 3:184–199
Joshi VV, Cantor AB, Altshuler G, Larkin EW, Neill JS, Shuster JJ, Holbrook CT, Hayes FA, Castleberry RP (1992) Recommendations for modification of terminology of neuroblastic tumors and prognostic significance of Shimada classification. A clinicopathologic study of 213 cases from the Pediatric Oncology Group. Cancer 69:2183–2196
Joshi VV, Cantor AB, Altshuler G, Larkin EW, Neill JS, Shuster JJ, Holbrook CT, Hayes FA, Nitschke R, Duncan MH, Shochat SJ, Talbert J, Smith EI, Castleberry RP (1992) Age-linked prognostic categorization based on a new histological grading system of neuroblastomas. A clinicopathologic study of 211 cases from the Pediatric Oncology Group. Cancer 69:2197–2211
Joshi VV, Chatten J, Sather HN, Shimada H (1991) Evaluation of the Shimada classification in advanced neuroblastoma with a special reference to the mitosis–karyorrhexis index: a report from the Children’s Cancer Study Group. Mod Pathol 4:139–147
Joshi VV, Rao PV, Cantor AB, Altshuler G, Shuster JJ, Castleberry RP (1996) Modified histologic grading of neuroblastomas by replacement of mitotic rate with mitosis karyorrhexis index. A clinicopathologic study of 223 cases from the Pediatric Oncology Group. Cancer 77:1582–1588
Kaneko Y, Kanda N, Maseki N, Sakurai M, Tsuchida Y, Takeda T, Okabe I, Sakurai M (1987) Different karyotypic patterns in early and advanced stage neuroblastomas. Cancer Res 47:311–318
Katzenstein HM, Bowman LC, Brodeur GM, Thorner PS, Joshi VV, Smith EI, Look AT, Rowe ST, Nash MB, Holbrook T, Alvarado C, Rao PV, Castleberry RP, Cohn SL (1998) Prognostic significance of age, MYCN oncogene amplification, tumor cell ploidy, and histology in 110 infants with stage D (S) neuroblastoma: the Pediatric Oncology Group experience—a Pediatric Oncology Group study. J Clin Oncol 16:2007–2017
Kobayashi C, Monforte-Munoz HL, Gerbing RB, Stram DO, Matthay KK, Lukens JN, Seeger RC, Shimada H (2005) Enlarged and prominent nucleoli may be indicative of MYCN amplification: a study of neuroblastoma (Schwannian stroma-poor), undifferentiated/poorly differentiated subtype with high mitosis–karyorrhexis index. Cancer 103:174–180
Lastowska M, Cullinane C, Variend S, Cotterill S, Bown N, O’Neill S, Mazzocco K, Roberts P, Nicholson J, Ellershaw C, Pearson AD, Jackson MS (2001) Comprehensive genetic and histopathologic study reveals three types of neuroblastoma tumors. J Clin Oncol 19:3080–3090
Look AT, Hayes FA, Nitschke R, McWilliams NB, Green AA (1984) Cellular DNA content as a predictor of response to chemotherapy in infants with unresectable neuroblastoma. N Engl J Med 311:231–235
Makinen J (1972) Microscopic patterns as a guide to prognosis of neuroblastoma in childhood. Cancer 29:1637–1646
Navarro S, Amann G, Beiske K, Cullinane CJ, d’Amore E, Gambini C, Mosseri V, De Bernardi B, Michon J, Peuchmaur M (2006) Prognostic value of International Neuroblastoma Pathology Classification in localized resectable peripheral neuroblastic tumors: a histopathologic study of Localized Neuroblastoma European Study Group 94.01 Trial and Protocol. J Clin Oncol 24:695–699
Poremba C, Scheel C, Hero B, Christiansen H, Schaefer KL, Nakayama J, Berthold F, Juergens H, Boecker W, Dockhorn-Dworniczak B (2000) Telomerase activity and telomerase subunits gene expression patterns in neuroblastoma: a molecular and immunohistochemical study establishing prognostic tools for fresh-frozen and paraffin-embedded tissues. J Clin Oncol 18:2582–2592
Poremba C, Willenbring H, Hero B, Christiansen H, Schafer KL, Brinkschmidt C, Jurgens H, Bocker W, Dockhorn-Dworniczak B (1999) Telomerase activity distinguishes between neuroblastomas with good and poor prognosis. Ann Oncol 10:715–721
Rudolph P, Lappe T, Hero B, Berthold F, Parwaresch R, Harms D, Schmidt D (1997) Prognostic significance of the proliferative activity in neuroblastoma. Am J Pathol 150:133–145
Seeger RC, Brodeur GM, Sather H, Dalton A, Siegel SE, Wong KY, Hammond D (1985) Association of multiple copies of the N-myc oncogene with rapid progression of neuroblastomas. N Engl J Med 313:1111–1116
Shimada H (1992) Neuroblastoma. Pathology and biology. Acta Pathol Jpn 42:229–241
Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B (1999) Terminology and morphologic criteria of neuroblastic tumors. Recommendations by the International Neuroblastoma Pathology Committee. Cancer 86:349–363
Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B, Stram DO, Gerbing RB, Lokens JN, Matthay KK, Castleberry RP (1999) The International Neuroblastoma Pathology Classification (the Shimada system). Cancer 86:364–372
Shimada H, Chatten J, Newton WA, Sachs N, Hamoudi AB, Chiba T, Marsden HB, Misugi K (1984) Histopathologic prognostic factors in neuroblastic tumors: definition of subtypes of ganglioneuroblastoma and an age-linked classification of neuroblastomas. J Natl Cancer Inst 73:405–416
Shimada H, Stram D, Chatten J, Joshi VV, Hachitanda Y, Brodeur G, Lukens J, Matthay K, Seeger R (1995) Identification of subsets of neuroblastomas by combined histopathologic and N-myc analysis. J Natl Cancer Inst 87:1470–1476
Shimada H, Umehara S, Monobe Y, Hachitanda Y, Nakagawara A, Goto S, Gerbing RB, Stram D, Lukens JN, Matthay KK (2001) International neuroblastoma pathology classification for prognostic evaluation of patients with peripheral neuroblastic tumors: a report from the Children’s Cancer Group. Cancer 92:2451–2461
Tsuda T, Obara M, Hirano H, Gotoh S, Kubomura S, Higashi K, Kuroiwa A, Kakagawara A, Nagahara N, Shimizu K (1987) Analysis of N-myc amplification in relation to disease stage and histologic types in human neuroblastomas. Cancer 60:820–826
Acknowledgement
Supported by grant no. G03/089 from Instituto Carlos III, Madrid, Spain.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burgues, O., Navarro, S., Noguera, R. et al. Prognostic value of the International Neuroblastoma Pathology Classification in Neuroblastoma (Schwannian stroma-poor) and comparison with other prognostic factors: a study of 182 cases from the Spanish Neuroblastoma Registry. Virchows Arch 449, 410–420 (2006). https://doi.org/10.1007/s00428-006-0253-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-006-0253-y