Abstract
Little is known about CD117 prevalence and clinicopathological implications in pulmonary large-cell neuroendocrine carcinoma. We studied CD117 immunoreactivity in surgical specimens from 39 large-cell neuroendocrine carcinomas of stages I–III and 27 limited-disease small-cell carcinomas, 56 typical and atypical carcinoids of the lung, and 10 neuroendocrine tumorlets, including the membrane and cytoplasmic immunostaining patterns. Membrane CD117 immunoreactivity in 5% or more tumor cells was documented in 30 (77%) large-cell neuroendocrine carcinomas and 18 (67%) small-cell carcinomas and 4 (7%) carcinoids, whereas cytoplasmic labeling was seen in 17 (44%) large-cell neuroendocrine carcinomas, 19 (70%) small-cell carcinomas, and 3 (5%) carcinoids. None of the neuroendocrine cells of the normal bronchial epithelium and of 10 tumorlets showed any CD117 immunoreactivity. Cytoplasmic immunostaining was more prevalent in small-cell carcinomas, whereas membrane labeling did not differ between the two types of high-grade carcinomas. Downregulation of CD117 by neoadjuvant chemotherapy was seen in large-cell neuroendocrine carcinomas but not small-cell carcinomas. Multiple linear regression analysis demonstrated a marginal association between cytoplasmic CD117 immunoreactivity and regional lymph node metastasis in small-cell carcinomas but not large-cell neuroendocrine carcinomas. There was no association between CD117 immunoreactivity and survival in either small-cell carcinoma or large-cell neuroendocrine carcinoma patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
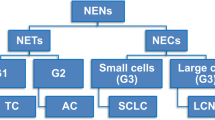
Approximately one-fourth to one-third of lung neoplasms are neuroendocrine tumors. These are classified along a continuum from low-grade tumors to intermediate-grade tumors with longer life expectancy (e.g., typical and atypical carcinoids) to very aggressive neoplasms with dismal prognosis (e.g., small-cell carcinomas and large-cell neuroendocrine carcinomas) [5, 30, 31]. Large-cell neuroendocrine carcinomas share most of the epidemiological and clinical features of small-cell lung carcinomas, including the highest association with a male prevalence, the highest incidence of regional lymph node and distant metastases at the time of the diagnosis, and the shortest survival; however, they reportedly differ in both morphological and genetic characteristics [9, 11, 28, 32, 33]. In particular, recent molecular data support the view that large-cell neuroendocrine carcinomas are much more akin to non-neuroendocrine large-cell carcinomas than to small-cell carcinomas or the other types of pulmonary neuroendocrine tumors [32], and therefore they have been included in the most recent World Health Organization classification of lung cancer.
Cell receptors with tyrosine kinase activity are important regulators of cell proliferation, differentiation, and survival and are thought to play a central role in the development and progression of several human malignancies, including lung cancer [19]. The proto-oncogene c-Kit, mapping to the chromosome 4q11-q12, encodes for a 145- to 160-kDa type 3 transmembrane tyrosine kinase receptor (CD117) that may undergo activation upon binding to its specific ligand [4, 35, 36] or through somatic intragenic mutations [13]. In neuroendocrine tumors of the lung CD117 immunoreactivity is commonly reported in small-cell carcinoma cell lines and in excised primary tumors, and some studies have reported it to be associated with adverse prognosis [14, 16, 20, 22, 29, 34]. Very few data, however, are available on the prevalence and clinicopathological implications of CD117 immunoreactivity in large-cell neuroendocrine carcinomas of the lung, with only two reports published in the English literature, to our knowledge [2, 8].
The aim of the present study was to compare the prevalence of CD117 immunoreactivity in (a) 39 stage I-III surgically resected large-cell neuroendocrine carcinomas of the lung and (b) 27 radically operated limited-disease small-cell carcinomas and 56 stage I-III typical and atypical carcinoids. We also investigated any change in CD117 immunoreactivity following neoadjuvant chemotherapy and its prognostic implications.
Materials and methods
Patients
The study included 122 consecutive patients who underwent radical resection at the participating institutions between 1987 and 2002. The population consisted of 79 men and 43 women with stage I–III neuroendocrine tumors [21]: 34 typical carcinoids, 22 atypical carcinoids, 39 large-cell neuroendocrine carcinomas, 27 small-cell carcinomas. All paraffin blocks were retrieved in each case, and the original hematoxylin and eosin-stained sections were reviewed. The diagnosis and the typing of tumors followed the 1999 WHO classification of lung and pleural tumors and adopted previously refined immunohistochemical criteria (immunoreactivity for synaptophysin, chromogranin A, and a variety of respiratory tract related hormones including gastrin-related peptide, calcitonin, adrenocorticotropic hormone, serotonin, and α-subunit of human chorionic gonadotropin) [24]. To ensure accurate staging all tumors had been removed by radical surgery, including an extensive mediastinal lymph node dissection (median: nine excised lymph nodes per patient). Two sections from each regional lymph node were examined histologically as previously reported [24].
Table 1 presents clinicopathological characteristics of the 122 neuroendocrine patients. All patients with small-cell carcinoma patients had limited disease according to the Veterans Administration Lung Cancer Study Group classification [15] (i.e., tumors restricted to one hemithorax without bulky regional metastases to hilar, ipsilateral, or contralateral mediastinal lymph nodes, or to supraclavicolar lymph nodes, or without ipsilateral pleural effusion). Among the patients undergoing neoadjuvant combination chemotherapy by the protocol of cyclophosphamide, doxorubicin, vincristine, and etoposide, including 5 with large-cell neuroendocrine carcinomas and 12 with small-cell carcinomas, there was a prevalence of more advanced-stage disease than among untreated patients (P=0.002). Detailed information on the cigarette smoking history was unavailable at the time of the present study, but most patients with high-grade tumors were known to be heavy smokers, consuming at least 20 cigarettes per day.
Immunohistochemistry
Formalin-fixed and paraffin-embedded tissue samples obtained at surgery were investigated. Tumors up to 2 cm in size were entirely embedded and immunostained; at least two representative tissue blocks were investigated in larger neoplasms. Ten samples of normal bronchial tree taken at different levels from patients with nonmalignant lung diseases, and ten samples of pulmonary neuroendocrine tumorlets and nonneoplastic peritumoral tissue from the study patients were used as control groups. Scattered neuroendocrine cells of the bronchial epithelium and tumorlets were identified with after chromogranin A immunostaining as previously described [23].
After blocking endogenous peroxidase activity with 5% hydrogen peroxide for 12 min, the tissue sections were reacted with the primary antibody to CD117 (a polyclonal antiserum raised against the C-terminal region of the human p145 KDa c-kit gene product encompassing the 963–976 amino acid residues; Dako-Cytomation, Glostrup, Denmark) for 30 min at room temperature using an automatic immunostainer (Autostainer, Dako) with no retrieval antigen procedure at the dilution of 10 µg/ml and then incubated with a high-sensitivity detection kit (Dako EnVision Plus-HRP) according to the manufacturer’s instructions. Peroxidase activity was then developed with 3–3′diaminobenzidine-copper sulfate (Sigma, St. Louis, Mo., USA) to obtain a bright brown-black end product. The specificity of all immunoreactions was double-checked by replacing the primary antibody by a nonrelated isotypic mouse immunoglobulin at a comparable dilution a nonrelated or by normal serum alone [7]. Appropriate internal positive controls of tumor-infiltrating mast cells were also checked in all reactions. The proliferative fraction was evaluated by Ki-67 immunostaining as previously reported [23].
Scoring method
Immunostaining reactions were evaluated without knowledge of the patient’s identity or clinical outcome. The proportion of immunoreactive tumor cells (labeling index) was assessed by scanning at least 1,000 neoplastic cells in representative fields of immunostaining. The CD117 immunostaining pattern was recorded as either predominantly membranous, if staining was primarily confined to the tumor cell membrane, or predominantly cytoplasmic, if a granular dotting reaction was identified in the cytoplasm of tumor cells with uneven membrane reinforcement. Tumors were considered negative for CD117 if staining was either completely absent or observed in only 5% or fewer of the neoplastic cells.
Statistical analysis
The significance of differences was evaluated using the χ2 or Fisher’s exact test. The medians of continuous data (e.g., age, tumor size) were compared by the Mann-Whitney or the Kruskal-Wallis test. To identify factors associated with the occurrence of regional lymph node metastases (yes/no) multiple logistic regression models included variables that emerged as significant in univariate regression analyses. Logistic regression results are expressed as odds ratios (OR) and corresponding 95% confidence intervals (CI). The overall and disease-free survival of patients classified in accordance with CD117 immunoreactivity were calculated by the Kaplan-Maier method and compared by the log-rank test. Cox’s proportional regression models of survival data were calculated including patient age and gender, tumor stage, Ki-67 labeling index, neoadjuvant chemotherapy, and three different cutoff thresholds (5%, 10%, and 30%) for cytoplasmic and membrane CD117 immunostaining. Hazard ratios (HR) and 95% CI were calculated. All analyses used SAS (SAS Institute, Cary, N.C., USA). All P values reported here are two-tailed.
Results
CD117 immunoreactivity is lacking in normal and hyperplastic neuroendocrine cells of the lung
The scattered neuroendocrine cells and the neuroepithelial bodies of the normal respiratory mucosa, highlighted by chromogranin A immunostaining on adjacent sections, were consistently nonreactive for CD117, both in the nonneoplastic peritumoral lung tissue of the patients under investigation and in the bronchial tree taken at different levels from patients with nonmalignant lung diseases. Likewise, the hyperplastic neuroendocrine cells of tumorlets were always devoid of any CD117 immunoreactivity. Mast cells in the tumor tissue and the stroma of all examined samples were the only cells consistently and strongly immunoreactive for this marker.
CD117 immunoreactivity was correlated with high-grade neuroendocrine carcinomas and lymph node metastases
Overall the CD117 membrane labeling of 5% or more tumor cells was observed in 52 (43%) neuroendocrine tumors, and prominent cytoplasmic decoration in 39 (32%). Membrane immunoreactivity was documented in 30 (77%) large-cell neuroendocrine carcinomas, 18 (67%) small-cell carcinomas, and 4 (7%) carcinoids, whereas cytoplasmic labeling was seen in 17 (44%) large-cell neuroendocrine carcinomas, 19 (70%) small-cell carcinomas, and 3 (5%) carcinoids (P<0.001). Figure 1 shows representative features of membrane and cytoplasmic immunostaining in both large-cell neuroendocrine carcinomas and small-cell carcinomas.
CD117 immunoreactivity in high-grade neuroendocrine carcinomas of the lung. A membrane and cytoplasmic decoration is present in a case of large-cell neuroendocrine carcinoma with peripheral palisading of tumor cells (arrowheads) and focal necrosis (asterisk; A), whereas a predominantly cytoplasmic accumulation of immunostaining product is found in a case of small-cell carcinoma (B). Stromal mast cells are strongly decorated for CD117 and act as an internal positive control (B, arrows). All immunoperoxidase staining was performed with diaminobenzidine-copper sulfate, and counterstained with hematoxylin; ×250
Cytoplasmic immunostaining was more common in small-cell carcinomas than large-cell neuroendocrine carcinomas (median 5% vs. 0%, respectively; P=0.014), whereas membrane labeling did not differ between the various histotypes (median 0% in carcinoids, 10% in large-cell neuroendocrine carcinomas, 30% in small-cell carcinomas). Therefore a trend for membrane-positive/cytoplasm-negative tumors was seen in large-cell neuroendocrine carcinomas (80%) compared with small-cell carcinomas (20%), whereas the membrane-negative/cytoplasm-positive tumors were more likely to be small-cell carcinomas (63%) than large-cell neuroendocrine carcinomas (37%; P=0.096). In large-cell neuroendocrine carcinomas downregulation of CD117 membrane immunoreactivity was seen following neoadjuvant chemotherapy (Table 2), while in small-cell carcinomas only the patient’s age was associated with increased membrane labeling of tumor cells (Table 2).
Overall, regional lymph node metastases were identified in 34 (52%) high-grade carcinoma patients (Table 1). Factors associated with the occurrence of regional lymph node metastases were female gender (P=0.059) and the presence of adjuvant chemotherapy (P=0.019) in small-cell but not large-cell neuroendocrine carcinomas; no significant correlations were found with age, tumor size, or proliferative activity. Multiple linear regression analysis for regional lymph node involvement revealed only neoadjuvant chemotherapy (HR=25.3, CI=1.3–501.3, P=0.034) and, marginally, CD117 cytoplasmic immunoreactivity (HR=10.9, CI=0.7–181.0, P=0.093) in the model based on a cutoff of 5% or more immunoreactive tumor cells was correlated independently with the occurrence of regional lymph node metastases in small-cell carcinomas but not large-cell neuroendocrine carcinoma.
CD117 immunoreactivity and survival in high-grade neuroendocrine carcinomas
In the present series either disease-free or overall survival was similar for large-cell neuroendocrine carcinoma and small-cell carcinoma (Fig. 2). Using the cutoff level of 5% immunoreactive cells, in small-cell carcinoma but not large-cell neuroendocrine carcinomas there was a trend for predominantly cytoplasm, not membrane-immunoreactive, tumors to take a more aggressive course, with shorter time to progression and overall survival (Fig. 3) Similar results were obtained the cutoff thresholds of 10% and 30%, with a trend for more aggressive clinical course in small-cell carcinoma only (data not shown). Multivariate Cox’s analysis identified only neoadjuvant therapy (HR=3.9, CI=1.1–14.7, P=0.038) in large-cell neuroendocrine carcinoma and tumor stage (HR=19.9, CI=1.6–248.1, P=0.021) in small-cell carcinoma as independent predictor of shorter overall survival, and Ki-67 labeling index (HR=1.1, CI=1.0–1.1, P=0.048) in large-cell neuroendocrine carcinoma and tumor stage (HR=19.8, CI=1.7–234.2, P=0.018) in small-cell carcinoma as independent indicator of reduced disease-free survival in the model of based on a cutoff of 5% or more immunoreactive tumor cells for CD117.
Disease-free (A) and overall (B) survival curves according to histological typing of 56 high-grade neuroenodocrine tumors of the lung (36 large-cell and 20 small-cell neuroendocrine carcinomas), for which complete follow-up information was available at the time of the study. No significant differences in survival were seen between the two histologies. Brackets Number of patients for each survival curve
Overall survival curve according to histological typing and 5% cutoff threshold of predominantly cytoplasmic immunoreactivity for CD117. In small-cell carcinomas but not large-cell neuroendocrine carcinomas there was a trend for cytoplasm—but not membrane—immunoreactive tumors to take a more aggressive course and entail a shorter life expectancy. Brackets Number of patients for each survival curve
Discussion
This study identified a subset of pulmonary high-grade neuroendocrine carcinomas that consistently exhibit either membranous or cytoplasmic CD117 immunoreactivity. Membrane immunostaining is downregulated in large-cell neuroendocrine carcinoma patients treated with neoadjuvant chemotherapy, whereas there is a trend for predominantly cytoplasmic decoration to be associated with regional lymph node metastasis in small-cell carcinomas. Although CD117 is not an independent predictor of survival in either large-cell neuroendocrine carcinoma or small-cell carcinomas of the lung, a predominantly cytoplasmic pattern of immunostaining is marginally associated with shorter disease-free and overall survival in patients with limited-disease small-cell carcinoma.
The high prevalence of CD117 immunoreactivity in pulmonary high-grade neuroendocrine tumors (as opposed to the lack of staining in normal and hyperplastic neuroendocrine cells of the lower respiratory tract and to the occasional immunoreactivity in low- to intermediate-grade neuroendocrine tumors) emphasizes the possible involvement of this molecule in the development of most large-cell neuroendocrine carcinoma and small-cell carcinomas. The mechanisms responsible for CD117 overexpression/activation in high-grade neuroendocrine tumors of the lung are largely unknown, although the possibility of an autocrine growth loop has been suggested for small-cell carcinoma cell lines [12]. The actual prevalence of small-cell carcinomas coexpressing CD117 and its cognate ligand and/or bearing activating gene mutations, however, is unknown, but this has not thus far been fully assessed [12].
The prevalence of CD117 immunoreactivity in high-grade neuroendocrine tumors of the lung that we observed (77% in large-cell neuroendocrine carcinoma, 70% in small-cell carcinomas) is higher than previously reported in (from 39% [8] to 55% [2] in cell lines or tumor specimens of large-cell carcinomas and 25–70% in small-cell carcinomas [12]). We believe that this may be explained at least in part by the different selection crietria for assessing immunoreactivity. Standardized criteria for evaluating CD117 immunoreactivity in tumors other then gastrointestinal stromal tumors are lacking [6]. We used a cutoff threshold of 5% immunostained tumor cells for evaluating immunoreactivity, in contrast to the 10% threshold used by Araki et al. [2] and the 50% threshold used by Casali et al. [8] for large-cell neuroendocrine carcinomas to ensure inclusion of all cases with valuable immunoreactivity. We excluded from the analysis all positive tumors showing less than 5% immunoreactive cells because these findings are less reproducibile and may be biologically negligible. Variable cutoff levels have previously been used to assess immunoreactivity in small-cell carcinomas, with threshold values ranging from 10% to 50% [17, 20, 26, 27]. In our series, cytoplasmic CD117 immunoreactivity in even 5% or more tumor cells was marginally correlated with the occurrence of regional lymph node metastases in small-cell carcinomas but not in large-cell neuroeendocrine carcinomas. This suggests that CD117 expression plays different roles in the progression of the various types of high-grade pulmonary neuroendocrine carcinomas, and that it may be biologically relevant to the clinical behavior of small-cell lung carcinomas.
Moreover, we report for the first time that neoadjuvant therapy is effective in downregulating membrane CD117 labeling even in large-cell neuroendocrine carcinoma, as recently reported for small-cell carcinoma of the lung [27]. The possible downregulation of CD117 induced by chemotherapy may be relevant in the selection of candidate patients for second-line treatments targeting CD117. The lack of CD117 downregulation following induction chemotherapy among small-cell carcinoma patients of the present series may be due to the inclusion of patients showing only very limited disease and amenable to complete surgical resection. However, there was a trend for patients not undergoing chemotherapy to show more immunoreactive tumor cells in the membrane (Table 2).
This study examined both membrane and cytoplasmic CD117 immunoreactivity, at variance with previous investigations, although the biological implications of the cytoplasmic accumulation of CD117 are currently unknown. A cytoplasmic labeling for this molecule, however, has been reported by others in several tumor types, including small-cell carcinomas [17, 20, 27], large-cell neuroendocrine carcinomas [8], non-small-cell carcinomas of the lung [3, 25], colorectal neuroendocrine carcinoma [1], and gastrointestinal stromal tumors [10]. Moreover, definite paranuclear, dotlike, cytoplasmic immunoreactivity for CD117 is also common in gastrointestinal tumor cells [10], and a definite nuclear immunolocalization was reported [18] in both normal and neoplastic medullary cells of the adrenal gland, suggesting that CD117 differs in compartmentalization between the various normal and neoplastic cells.
The prognostic implications of CD117 immunoreactivity in pulmonary neuroendocrine carcinomas are still under debate. Using a 5% cutoff for immunoreactivity we found no effect of CD117 on survival of patients with large-cell neuroendocrine carcinomas, thus confirming previous data using a 10% cutoff [2]. Other authors reported a reduction in both overall survival and time to progression in 33 large-cell neuroendocrine carcinomas by increasing the threshold level up to 50% immunoreactive tumor cells [8]. In the our study, however, increasing the cutoff levels (up to 30% of CD117 immunoreactive tumor cells) was ineffective in reaching any prognostic value for CD117 in large-cell carcinomas, although a marginal influence on overall survival and time to progression was found in limited-disease small-cell carcinoma patients. In multivariate analysis only neoadjuvant therapy and Ki-67 labeling index for large-cell neuroendocrine carcinomas and tumor stage in small-cell carcinomas emerged as significant risk factors for death and time to progression. These findings again emphasize that CD117 is relevant to the development of high-grade neuroendocrine tumors of the lung and probably is an early event considering the high prevalence of immunoreactivity within these tumors, but that it is less important as a prognosticator of prognosis.
In conclusion, we observed CD117 immunoreactivity in most high-grade neuroendocrine carcinomas, with differential expression of predominantly cytoplasmic labeling in small-cell carcinomas and chemotherapy-related downregulation of membrane staining in large-cell neuroendocrine carcinomas. Its effect on prognosis is marginal.
References
Akintola-Ogunremi O, Pfeifer JD, Tan BR, Yan Y, Zhu X, Hart J, Goldblum JR, Burgart L, Lauwers GY, Montgomery E, Lewin D, Washington K, Bronner M, Xiao SY, Greenson JK, Lamps L, Lazenby A, Wang HL (2003) Analysis of protein expression and gene mutation of c-kit in colorectal neuroendocrine carcinomas. Am J Surg Pathol 27:1551–1558
Araki K, Ishii G, Yokose T, Nagai K, Funai K, Kodama K, Nishiwaki Y, Ochiai A (2003) Frequent overexpression of the c-kit protein in large cell neuroendocrine carcinoma of the lung. Lung Cancer 40:173–180
Arber DA, Tamayo R, Weiss LM (1998) Paraffin section detection of the c-kit gene product (CD117) in human tissues: value in the diagnosis of mast cell disorders. Hum Pathol 29:498–504
Ashman LK (1999) The biology of stem cell factor and its receptor C-kit. Int J Biochem Cell Biol 31:1037–1051
Axiotis CA (2002) The neuroendocrine lung. In: Li Volsi V, Asa SL (eds) Endocrine pathology. Churchill Livingstone, Edinburgh, pp 261–296
Berman J, O’Leary TJ (2001) Gastrointestinal stromal tumor workshop. Hum Pathol 49:786–798
Burry RW (2000) Specificity controls for immunocytochemical methods. J Histochem Cytochem 48:163–166
Casali C, Stefani A, Rossi G, Migaldi M, Bettelli S, Parise A, Morandi U (2004) The prognostic role of c-kit protein expression in resected large cell neuroendocrine carcinoma of the lung. Ann Thorac Surg 77:247–252
Debelenko LV, Swalwell JI, Kelley MJ, Brambilla E, Manickam P, Baibakov G, Agarwal SK, Spiegel AM, Marx SJ, Chandrasekharappa SC, Collins FS, Travis WD, Emmert-Buck MR (2000) MEN1 gene mutation analysis of high-grade neuroendocrine lung carcinoma. Genes Chromosomes Cancer 28:58–65
Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP, Shmookler B, Sobin LH, Weiss SW (2002) Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 33:459–465
Haruki N, Yatabe Y, Travis WD, Nomoto S, Osada H, Nakamura S, Nakao A, Fujii Y, Takahashi T (2000) Characterization of high-grade neuroendocrine tumors of the lung in relation to menin mutations. Jpn J Cancer Res 91:317–323
Heinrich MC (2003) Is KIT an important therapeutic target in small cell lung cancer? Clin Cancer Res 9:5825–5828
Heinrich MC, Rubin BP, Longley BJ, Fletcher JA (2002) Biology and genetic aspoects of gastrointestinal stromal tumors: KIT activation and cytogenetic alterations. Hum Pathol 33:486–495
Hida T, Ueda R, Sekido Y, Hibi K, Matsuda R, Ariyoshi Y, Sugiura T, Takahashi T, Takahashi T (1994) Ectopic expression of c-kit in small-cell lung cancer. Int J Cancer Suppl 8:108–109
Hyde L, Yee J, Wilson R (1965) Cell type and the natural history of lung cancer. JAMA 193:52–54
Krystal GW, Hines SJ, Organ CP (1996) Autocrine growth of small cell lung cancer mediated by coexpression of c-kit and stem cell factor. Cancer Res 56:370–376
Lonardo F, Pass HI, Lucas DR (2003) Immunohistochemistry frequently detects c-Kit expression in pulmonary small cell carcinoma and may help select clinical subsets for a novel form of chemotherapy. Appl Immunohistochem Mol Morphol 11:51–55
Matsuda R, Takahashi T, Nakamura S, Sekido Y, Nishida K, Seto M, Seito T, Sugiura T, Ariyoshi Y, Takahashi T, Ueda R (1993) Expression of the c-kit protein in human solid tumors and in corresponding fetal and adult normal tissues. Am J Pathol 142:339–346
Maulik G, Kijima T, Salgia R (2003) Role of receptor tyrosine kinases in lung cancer. Methods Mol Med 74:113–125
Micke P, Basrai M, Faldum A, Bittinger F, Ronnstrand L, Blaukat A, Beeh KM, Oesch F, Fischer B, Buhl R, Hengstler JG (2003) Characterization of c-kit expression in small cell lung cancer: prognostic and therapeutic implications. Clin Cancer Res 9:188–194
Mountain CF (1997) Revisions in the international system for staging for lung cancer. Chest 111:1710–1717
Naeem M, Dahiya M, Clark JI, Creech SD, Alkan S (2002) Analysis of c-kit protein expression in small-cell lung carcinoma and its implication for prognosis. Hum Pathol 33:1182–1187
Pelosi G, Pasini F, Olsen Stenholm C, Pastorino U, Maisonneuve P, Sonzogni A, Maffini F, Pruneri G, Fraggetta F, Cavallon A, Roz E, Iannucci A, Bresaola E, Viale G (2002) p63 immunoreactivity in lung cancer: yet another player in the development of squamous cell carcinomas? J Pathol 198:100–109
Pelosi G, Pasini F, Fraggetta F, Pastorino U, Iannucci A, Maisonneuve P, Arrigoni G, De Manzoni G, Bresaola E, Viale G (2003) Independent value of fascin immunoreactivity for predicting lymph node metastases in typical and atypical pulmonary carcinoids. Lung Cancer 42:203–213
Pelosi G, Barisella M, Pasini F, Leon ME, Veronesi G, Spaggiari L, Fraggetta F, Iannucci A, Masullo M, Sonzogni A, Maffini F, Viale G (2004) CD117 immunoreactivity in stage I adenocarcinoma and squamous cell carcinoma of the lung: relevance to prognosis in a subset of adenocarcinoma patients. Mod Pathol 17:711–721
Potti A, Moazzam N, Ramar K, Hanekom DS, Kargas S, Koch M (2003) CD117 (c-Kit) overexpression in patients with extensive-stage small-cell lung carcinoma. Ann Oncol 14:894–897
Rossi G, Cavazza A, Marchioni A, Milgaldi M, Bavieri M, Facciolongo N, Petruzzelli S, Longo L, Tamberi S, Crino L (2003) KIT expression in small cell carcinomas of the lung: effects of chemotherapy. Mod Pathol 16:1041–1047
Sampietro G, Tomasic G, Collini P, Biganzoli E, Boracchi P, Bidoli P, Pilotti S (2000) Gene product immunophenotyping of neuroendocrine lung tumors. No linking evidence between carcinoids and small-cell lung carcinomas suggested by multivariate statistical analysis. Appl Immunohistochem Mol Morphol 8:49–56
Sekido Y, Obata Y, Ueda R, Hida T, Suyama M, Shimokata K, Ariyoshi Y, Takahashi T (1991) Preferential expression of c-kit protooncogene transcripts in small cell lung cancer. Cancer Res 51:2416–2419
Travis WD, Gal AA, Colby TV, Klimstra DS, Falk R, Koss MN (1998) Reproducibility of neuroendocrine lung tumor classification. Hum Pathol 29:272–279
Travis WD, Rush W, Flieder DB, Falk R, Fleming MV, Gal AA, Koss MN (1998) Survival analysis of 200 pulmonary neuroendocrine tumors with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. Am J Surg Pathol 22:934–944
Ullmann R, Petzmann S, Sharma A, Cagle PT, Popper HH (2001) Chromosomal aberrations in a series of large-cell neuroendocrine carcinomas: unexpected divergence from small-cell carcinoma of the lung. Hum Pathol 32:1059–1063
Ullmann R, Petzmann S, Klemen H, Fraire AE, Hasleton P, Popper HH (2002) The position of pulmonary carcinoids within the spectrum of neuroendocrine tumors of the lung and other tissues. Genes Chromosomes Cancer 34:78–85
Wang WL, Healy ME, Sattler M, Verma S, Lin J, Maulik G, Stiles CD, Griffin JD, Johnson BE, Salgia R (2000) Growth inhibition and modulation of kinase pathways of small cell lung cancer cell lines by the novel tyrosine kinase inhibitor STI 571. Oncogene 19:3521–3528
Witte O (1990) Steel locus defines new multipotent growth factor. Cell 63:5–6
Yarden Y, Kuang WJ, Yang-Feng T, Coussens L, Munemitsu S, Dull JT, Chen E, Schlessinger J, Francke U, Ullrich A (1987) Human proto-oncogene c-kit: a new cell surface receptor tyrosine kinase for an undefinited ligand. EMBO J 6:3341–3351
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pelosi, G., Masullo, M., Leon, M.E. et al. CD117 immunoreactivity in high-grade neuroendocrine tumors of the lung: a comparative study of 39 large-cell neuroendocrine carcinomas and 27 surgically resected small-cell carcinomas. Virchows Arch 445, 449–455 (2004). https://doi.org/10.1007/s00428-004-1106-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-004-1106-1