Abstract
The understanding of regeneration in salivary glands as a finely tuned balance of cellular proliferation, differentiation and apoptosis has been limited by the difficulty of identifying proliferating cells. This has been overcome in the present investigation by double immunohistochemical labelling for the proliferation-associated antigen Ki67 and for different cell-type-specific antigens applied to 8 specimens of normal parotids and 16 specimens of chronic parotid sialadenitis with particular reference to acini and intercalated ducts. In comparison with low baseline rates of proliferation in normal parotids, proliferative indices were significantly increased in chronic sialadenitis in mature acinar cells, intercalated ductal cells and myoepithelial cells without evidence of proliferation by an additional population of cells. In accordance with findings in glands of experimental animals, the present data do not support the previously postulated concept of regeneration of acini and intercalated ducts by a hypothetical population of uncommitted ductal stem cells. The demonstration of a profound capacity for intrinsic glandular regeneration from differentiated cells represents a biological basis for the good results obtained from conservative therapy of chronic sialadenitis and offers hope for novel therapies designed to reconstitute impaired salivary flow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic sialadenitis is a common cause of removal of salivary glands, although, recently, interest in conservative procedures has increased due to their excellent results and the morbidity associated with surgery, especially parotidectomy [1, 20]. Preliminary animal studies with gene transfer or transplantation of stem cells are being undertaken with the aim of improving salivary flow rates in severely atrophic glands [3]. However, the understanding of the glandular regeneration that is important for the development of these therapies is limited.
Regeneration of the salivary glands has, for a long time, been predominantly attributed to a putative population of uncommitted stem cells believed to be situated in the ducts [2]. However, investigations on experimental animals have failed to support this concept, and a growing body of evidence indicates the importance of a proliferative capacity of differentiated cells in diverse segments of the salivary duct [7, 8, 10, 29]. The major obstacle for an analysis of the proliferative capacity has been the difficulty of accurately identifying types of proliferating cells in the complex cellular composition of the salivary glands, which is aggravated in sialadenitis by an additional intimate admixture of intensely proliferating inflammatory and stromal cells (Fig. 3a).
The implementation of double immunohistochemical labelling for the proliferation-associated antigen Ki67 and for different cell-type-specific antigens has greatly improved the accurate localisation and quantification of proliferating cells. This technique recently enabled us to demonstrate a quantitatively diverse, but generally low, baseline proliferation in all five types of parenchymal cells of the normal human salivary gland [18]. These findings indicate that acinar cells, intercalated ductal cells and myoepithelial cells regenerate independently, without cellular transition and without the participation of an additional population of cells, while the renewal of luminal columnar cells in striated and excretory ducts is maintained by proliferation and differentiation of basal cells. In conditions of chronic damage, these basal cells manifest an additional capacity for a pluridirectional morphogenetic differentiation into several types of reactive ductal metaplasias [18, 24]. However, despite this prominent role of basal cells in the striated and excretory ducts, there is no evidence for an active participation of basal cells in the cellular regeneration of the acini and intercalated ducts.
Investigations on the effects of chronic noxious stimuli on the acini and intercalated ducts have shown a limited reaction pattern that is largely confined to atrophy of the acini [11, 12, 13, 15, 21, 23, 25, 26, 27, 28, 29]. The role of cellular proliferation and apoptosis in parenchymal atrophy in chronic sialadenitis is not understood, and it is not clear to what extent cellular regeneration can compensate for the loss of cells in the atrophic glands. The aim of the present investigation is, therefore, to examine proliferation and apoptosis in chronic parotid sialadenitis to provide a biological basis for modern therapies and is focused on the alterations in the acini and intercalated ducts to complement the previous investigation, in which the striated and excretory ducts were examined [18].
Materials and methods
Materials
Surgical specimens (n=24) from human parotids were retrieved from the archives of the Institute of Pathology, Ludwig-Maximilians-University, Munich. They had been fixed in buffered formaldehyde (4%; pH 7), embedded in paraffin wax and cut into 4-µm serial sections. Normal parenchyma lacking inflammation was obtained from 8 of the specimens that had been resected for small Warthin tumours or pleomorphic adenomas (male 5; female 3; ages 36–51 years). Of the specimens, 16 had been diagnosed as chronic sialadenitis with or without sialolithiasis (male 9; female 7; ages 28–58 years) and did not include cases of benign lymphoepithelial lesion.
Methods
The degree of inflammation and parenchymal atrophy in these cases ranged from minor to severe and often demonstrated a variable focal distribution. The 16 cases of chronic sialadenitis were divided into a subgroup of 10 cases with minor acinar atrophy, which varied from mild to moderate and was often focal, and a subgroup of 6 cases with predominantly severe acinar atrophy. An accurate enumeration of cellular proliferation and apoptosis could not be accomplished in the latter subgroup because so few acinar cells were preserved. Previous data on the cellular proliferation of the normal parotids [18] served as a basis for the present investigation.
Quantification of proliferation
The protocols of double immunohistochemical labelling for Ki67–CK7 (labelling intercalated ductal cells) and Ki67–CK18 (labelling acinar cells) are as follows. Deparaffinised slides were subjected to microwave pretreatment (750 Watt) with target retrieval solution (TRS 6; pH 6; 30 min). Endogenous peroxidase was blocked with peroxidase solution (7.5%). An aviditin-biotin peroxidase complex method was applied (ABC-kit; Vector). The slides were incubated with normal horse serum for 20 min. After avidin-biotin blocking, the slides were incubated (room temperature; 60 min) for either monoclonal anti-CK7 (1:500 dilution) or anti-CK18 (1:450 dilution). Biotinylated universal antibody was applied as secondary antibody followed by avidin-biotin complex (Elite; 30 min each). Diaminobenzidine+ (Dako; 3 min) was used as chromogen. For staining with Ki67, the alkaline phosphatase–antialkaline phosphatase (APAAP)-method was used (APAAP-ChemMate; Dako). The monoclonal anti-Ki67 (1:50 dilution) was applied at room temperature for 60 min. Visualisation of the bound anti-Ki67 was obtained with a secondary antibody of mouse immunoglobulin followed by APAAP-immunocomplex (30 min each). Fast red (Sigma) was used as the chromogen (10 min) and Vector haematoxylin (Gill’s formula) as the counterstain. For double staining with Ki67 and α-actin (labelling myoepithelial cells), the same procedure was used as outlined above with the following exceptions: a labelled streptavidin biotin kit was applied (LSAB-Kit, Dako) and anti-α-actin was used in a dilution of 1:400. Table 1 summarises the protocols.
The labelling-index was determined by calculating the percentage of Ki67-positive nuclei within a total of 400 acinar cells, intercalated ductal cells and myoepithelial cells, each identified according to cytological criteria and the immunohistochemical staining pattern (Fig. 4) [5, 16, 17, 18, 22]. The mean percentage of cellular proliferation and the standard error of the mean were calculated. For comparison of normal glands with inflamed glands, statistical analysis of the primary data of the three different types of cells was undertaken, using the χ2 test.
Quantification of apoptosis
Caspase-mediated cleavage of cytoplasmic intermediate filaments is an early event in apoptosis of epithelial cells. The immunohistochemical detection of a specific caspase-cleavage site in CK18 filaments as a neo-epitope (M30) can be applied to formalin-fixed material for the detection of apoptosis in certain types of epithelial cells [9, 19]. Although M30 does not detect apoptosis in myoepithelial cells, due to the absence of CK18 filaments, it is associated with a better morphological result than when other markers of apoptosis are used, and the type of parenchymal cell that is labelled by M30 can be identified morphologically without confusion with the numerous inflammatory and stromal cells in sialadenitis, in which apoptosis is also not detected due to the lack of CK18 filaments. Cytological criteria for apoptosis (especially nuclear condensation and fragmentation) were used as a control for positive M30 labelling. Double labelling for M30 and cell-type specific markers analogous to Ki67 could not be established.
Due to the relatively small number of apoptoses demonstrated by M30, they were counted in 20 microscopical fields (0.25 mm2 with a 10× eyepiece and 20× objective) separately for acinar cells and intercalated ductal cells. The mean number of cellular apoptoses and the standard error of the mean were calculated.
Results
The striated and excretory ducts contain columnar cells and were easily distinguished from the intercalated ducts, which are smaller and contain cuboidal or flattened lining cells, in normal and moderately atrophic glands. The columnar structure was often maintained in very atrophic glands, but sometimes all the intralobular ducts were very atrophic and lacked columnar cells, although there was a difference in size that enabled the smaller ducts to be interpreted as intercalated ducts.
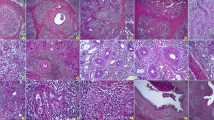
Double immunohistochemical labelling accurately demonstrated proliferation in the different types of cells of the salivary parenchyma, even with a background of intensely proliferating inflammatory and stromal cells in sialadenitis. The proliferation indices in chronic sialadenitis were increased about twofold in acinar cells, fourfold in intercalated ductal cells and more than tenfold in myoepithelial cells (Fig. 2a, b, c, Fig. 3b, c; Table 2). In the statistical analysis, the proliferation indices were significantly higher in the sialadenitis subgroups, with minor atrophy and severe atrophy compared with normal glands for intercalated ductal cells (both P<0.001) and myoepithelial cells (P<0.02 and P<0.01, respectively). The proliferation indices for intercalated ductal cells and myoepithelial cells were slightly higher in the sialadenitis subgroup with severe atrophy than in the subgroup with minor atrophy, although this was not statistically significant. In contrast to an absence of apoptoses in normal parotids (Fig. 1d), small numbers of apoptoses were seen in acinar and intercalated ductal cells in chronic sialadenitis (Fig. 2d, Fig. 3d; Table 3).
Cellular proliferation and apoptosis in acini and intercalated ducts illustrated in representative cases of normal parotid. Original magnification: ×160. Double immunohistochemical labelling applied to normal parotids demonstrates proliferation in a CK18-positive acinar cell (a), a CK7-positive intercalated ductal cell (b) and an α-actin-positive myoepithelial cell (c). Apoptoses are absent (d; M30)
Cellular proliferation and apoptosis in acini and intercalated ducts illustrated in representative cases of chronic sialadenitis with minor atrophy. Original magnification: ×160. In chronic sialadenitis with minor atrophy, cellular proliferation is markedly increased. Applying double labelling, increased proliferation can be attributed to CK18-positive acinar cells (a; arrows), CK7-positive intercalated ductal cells (b; arrow; remnants of CK7-negative acinar cells are indicated by arrowheads) and myoepithelial cells (c; arrows). One apoptosis is seen and is attributable to an acinar cell (d; M30)
Cellular proliferation and apoptosis in acini and intercalated ducts illustrated in representative cases of chronic sialadenitis with severe atrophy. Original magnification: ×160. In chronic sialadenitis with severe atrophy, a illustrates that an accurate demonstration of proliferation is difficult when staining for Ki67 alone, owing to the complex cellular composition. Double labelling demonstrates the increased proliferation in intercalated ductal cells (b; arrows) and myoepithelial cells (c; arrows), while recognisable acinar cells are absent. The apoptosis demonstrated by M30 (d) is attributable to an intercalated ductal cell
Discussion
A precise identification and quantification of proliferating cells facilitated by double immunohistochemical labelling has recently enabled us to establish a low, yet quantitatively diverse, proliferative capacity in the five types of differentiated parenchymal cells of the human salivary gland that maintain the gland in a steady state [18]. The significant increase of proliferation demonstrated in the present investigation in mature acinar cells, intercalated ductal cells and myoepithelial cells in chronic sialadenitis is consistent with several experimental animal investigations, which indicate a proliferative capacity in differentiated glandular cells [7, 8, 10, 11, 29]. Previous investigations on proliferation in salivary glands have mainly been performed on the animal model of experimental ductal obstruction, followed by removal of obstruction [7, 8, 10, 25, 27, 29] and are of value in helping our understanding of chronic sialadenitis in which ductal obstruction, which is often intermittent, is one of the noxious stimuli [14].
Burgess et al. [7, 8] used a similar immunohistochemical technique to that of the present investigation in rodent glands and found that an increased proliferation predominantly of myoepithelial cells during ductal ligation was followed by an increased proliferation predominantly of acinar cells after removal of the ligation. Thus, the increased proliferation of both of these types of cells in sialadenitis found in the present investigation possibly represents a reaction to intermittent obstruction, in which there is increased proliferation of myoepithelial cells during obstruction in an attempt to overcome the obstruction followed by proliferation of the acini during relief from the obstruction, when the environment is more conducive to secretory activity.
In addition to increased proliferation, the present investigation demonstrates an increased rate of apoptosis (Fig. 1d, Fig. 2d, Fig. 3d) in acinar and intercalated ductal cells in chronic sialadenitis compared with normal glands, in which apoptosis was not demonstrated. This does not mean that there is no apoptosis of these cells in normal glands, for there is a rapid phagocytic removal of apoptotic cells, which restricts the immunohistochemical demonstration of apoptosis to a much shorter time [19] than the demonstration of cellular proliferation by an antibody to Ki67, which appears to last for about one to several days [6]. Therefore, in contrast to Ki67-based demonstration of proliferation, which includes events that occur during one or more days before removal of the glands, only a relatively small fraction of the apoptoses that occur during this time will be demonstrable. Nevertheless, the presence of M30 labelling indicates that there is an increase in apoptosis in sialadenitis. However, the immunohistological detection of the dynamic processes of cellular proliferation and apoptosis that last for very different lengths of time does not allow a direct quantitative comparison between the proliferation and apoptotic indices. Possibly, the cell loss in chronic sialadenitis is partly compensated by increased cellular proliferation of differentiated cells, which is compatible with partial glandular recovery after removal of experimental ductal ligation [25]. The rates of apoptosis in chronic sialadenitis are much lower than the high rates reported by Walker et al. [29] and Scott et al. [25] in ductal ligation, and this is possibly due to adaptation to a chronic damaging process and to an obstruction that is intermittent and partial in sialadenitis.
Despite the capacity for intrinsic cellular proliferation, chronic sialadenitis eventually leads to progressive glandular atrophy, characterised by a loss of acinar cells with preservation of the intercalated ducts and myoepithelial cells (Fig. 4) [11, 12, 13, 14, 15, 21, 23, 25, 26, 28]. A gradual transformation of acinar cells during severe glandular damage into a less differentiated type of cell, similar to the intercalated ductal cells, has long been postulated. Convincing support for this kind of dedifferentiation of acinar cells is derived from ultrastructural studies [12, 13, 15, 21, 23, 27, 28, 29] and from the gradual gain of CK7 expression, which is seen in atrophic salivary parenchyma of man [18]. This gradual dedifferentiation, together with the increased apoptotic loss of acinar cells, is likely to contribute to the predominant atrophy of acini, which occurs in spite of increased acinar proliferation [25, 29].
The synthesis of data from animal models [7, 8, 10, 25, 29], our previous investigation on reactive metaplasia in human glands [18] and the present investigation of sialadenitis supports the following principles for glandular regeneration: (1) The physiological regeneration of the acini and intercalated ducts is based on a low baseline proliferation of mature acinar cells, intercalated ductal cells and myoepithelial cells with a capacity for greatly increased proliferation in the presence of noxious stimuli. (2) The basal cells harbour an important role in the central duct segment as reserve cells for the physiological regeneration of luminal columnar cells and for a pluridirectional differentiation into several types of reactive epithelial metaplasia. This function of basal cells, however, obviously is restricted to the striated and excretory ducts. (3) There is a lack of support for the previously prevailing postulate of a predominant role for putative uncommitted stem cells in parenchymal regeneration.
Although the basic principles of cellular proliferation are likely to be universal [4, 6, 18], the complex mechanisms of physiological cellular regeneration, reactive metaplasias and, presumably, also pluriform tumorigenesis of salivary glands are likely to be a consequence of their unique and complex cellular composition. With regard to clinical implications, the low baseline and profound inducible capacity for intrinsic glandular regeneration represents a biological basis for the good functional results from conservative therapies of chronic sialadenitis [1, 3, 20]. This offers hope for novel therapeutic strategies designed to restore impaired salivary function.
References
Antoniades D, Harrison JD, Epivatianos A, Papanayotou P (2004) Treatment of chronic sialadenitis by intraductal penicillin or saline. J Oral Maxillofac Surg (in press)
Batsakis JG, Regezi JA, Luna MA, El-Naggar A (1989) Histogenesis of salivary gland neoplasms: a postulate with prognostic implications. J Laryngol Otol 103: 939–944
Baum B (2000) Prospects for re-engineering salivary glands. Adv Dent Res 14:84–88
Bonkoff H, Remberger K (1998) Morphogenetic concepts of normal and abnormal growth in the human prostate. Virchows Arch 433:195–202
Born IA, Schwechheimer K, Maier H, Otto HF (1987) Cytokeratin expression in normal salivary glands and in cystadenolymphomas demonstrated by monoclonal antibodies against selective cytokeratin polypeptides. Virchows Arch 411:583–589
Brown DC, Gatter KC (1990) Monoclonal antibody Ki-67: its use in histopathology. Histopathology 17:489–503
Burgess KL, Dardick I (1998) Cell population changes during atrophy and regeneration of rat parotid gland. Oral Surg Med Oral Pathol Oral Radiol Endod 85:699–706
Burgess KL, Dardick I, Cummings MM, Burford-Mason AP, Bassett R, Brown DH (1996) Myoepithelial cells actively proliferate during atrophy of rat parotid gland. Oral Surg Oral Med Oral Pathol 82:674–680
Caulin C, Salvesen GS, Oshima RG (1997) Caspase cleavage of keratin 18 and reorganization of intermediate filaments during epithelial cell apoptosis. J Cell Biol 138:1379–1393
Dardick I, Byard RW, Carnegie A (1990) A review of the proliferative capacity of major salivary glands and the relationship to current concepts of neoplasia in salivary glands. Oral Surg Oral Med Oral Pathol 69:53–67
Donath K, Hirsch-Hoffmann HU, Seifert G (1973) Zur Pathogenese der Parotisatrophie nach experimenteller Gangunterbindung. Ultrastrukturelle Befunde am Drüsenparenchym der Rattenparotis. Virchows Arch 359:31–48
Emmelin N, Garrett JR, Ohlin P (1974) Secretory activity and the myoepithelial cells of salivary glands after duct ligation in cats. Arch Oral Biol 19:275–283
Harrison JD, Badir MS (1998) Chronic submandibular sialadenitis: ultrastructure and phosphatase histochemistry. Ultrastruct Pathol 22:431–437
Harrison JD, Epivatianos A, Bhatia SN (1997) Role of microliths in the aetiology of chronic submandibular sialadenitis: a clinicopathological investigation of 154 cases. Histopathology 31:237–251
Harrison JD, Fouad HMA, Garrett JR (2000) The effects of ductal obstruction on the acinar cell of the parotid of cat. Arch Oral Biol 45:945–949
Ihrler S, Zietz C, Riederer A, Diebold J, Löhrs U (1996) HIV-related parotid lymphoepithelial cysts. Immunohistochemistry and 3-D reconstruction of surgical and autopsy material with special reference to formal pathogenesis. Virchows Arch 429:139–147
Ihrler S, Zietz C, Sendelhofert A, Riederer A, Löhrs U (1999) Lymphoepithelial duct lesions in Sjögren-type sialadenitis. Virchows Arch 434:315–323
Ihrler S, Zietz C, Sendelhofert A, Lang S, Blasenbreu-Vogt S, Löhrs U (2002) A morphogenetic concept of salivary duct regeneration and metaplasia. Virchows Arch 440:519–526
Leers MPG, Kölgen W, Björklund V, Bergman T, Tribbick G, Persson B, Björklund P, Ramaekers S, Björklund B, Nap M, Jörnvall H, Schutte B (1999) Immunocytochemical detection and mapping of a cytokeratin 18 neo-epitope exposed during early apoptosis. J Pathol 187:567–572
Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W (2001) Specificity of parotid sialendoscopy. Laryngoscope 111:264–271
Matthews TW, Dardick I (1988) Morphological alterations of salivary gland parenchyma in chronic sialadenitis. J Otolaryngol 17:385–394
Moll R (1988) Differenzierungsprogramme des Epithels und ihre Änderungen. Verh Dtsch Ges Pathol 72:102–114
Palmer RM, Eveson JW (1987) Chronic sialadenitis. An immunohistochemical study in humans. Virchows Arch 412:73–78
Pammer J, Horvat R, Weninger W, Ulrich W (1995) Expression of bcl-2 in salivary glands and salivary gland adenomas. A contribution to the reserve cell theory. Pathol Res Pract 191:35–41
Scott J, Liu P, Smith PM (1999) Morphological and functional characteristics of acinar atrophy and recovery in the duct-ligated parotid gland of the rat. J Dent Res 78:1711–1719
Seifert G, Donath K (1977) Zur Pathogenese des Küttner-Tumors der Submandibularis. Analyse von 349 Fällen mit chronischer Sialadenitis der Submandibularis. HNO 25:81–92
Tamarin A (1971) Submaxillary gland recovery from obstruction. II. Electron microscopic alterations of acinar cells. J Ultrastruct Res 34:288–302
Tandler B (1977) Ultrastructure of chronically inflamed human submandibular glands. Arch Pathol Lab Med 101:425–431
Walker NI, Gobé GC (1987) Cell death and cell proliferation during atrophy of the rat parotid gland induced by duct obstruction. J Pathol 153:333–344
Acknowledgements
This study was supported by a grant from the “Friedrich-Baur-Stiftung” (Grant no. 0016/2003). The assistance of Mrs. Diane Raabe in reviewing the manuscript is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ihrler, S., Blasenbreu-Vogt, S., Sendelhofert, A. et al. Regeneration in chronic sialadenitis: an analysis of proliferation and apoptosis based on double immunohistochemical labelling. Virchows Arch 444, 356–361 (2004). https://doi.org/10.1007/s00428-003-0964-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-003-0964-2