Abstract
After renal ischemic reperfusion injury, a series of pathological changes, such as impaired intestinal barrier function, intestinal flora, and endotoxin translocation, are caused by intestinal ischemia and hypoxia, which then trigger systemic inflammatory responses and affect the condition and prognosis of the patients. In this study, a rat model of ischemia-reperfusion injury was established by examining changes in renal function, intestinal barrier function, inflammatory index, oxidative stress, and macrophage phenotypes to evaluate the effect of probiotic VSL#3 on renal ischemia-reperfusion injury. The results showed that, after VSL#3 intervention, the levels of BUN, Scr, Cys C, PRO, and NGAL were all significantly decreased compared with the I/R group, while the value of Ccr showed a significant increase. In addition, the concentrations of MPO, IL-1β, TNF-α, IL-6, ED-1, and PCNA were all significantly lower than those in the I/R group, while the levels of endotoxin, DOA, and d-lactic acid were significantly decreased. Furthermore, the proteins associated with intestinal barrier functions, such as ZO-1, Occludin, and Claudin-1, were significantly upregulated compared with the I/R group. Overall, the VSL#3 intervention group was able to maintain the required number of beneficial intestinal flora and to inhibit the proliferation of harmful bacteria. At the same time, the VSL#3 intervention could also prevent the decrease in the levels of CAT, GSH-PX, H2O2, and T-SOD, while downregulating the expression of Keap1 and Nrf2. After the intervention with the VSL#3, the expression levels of CD68 and CD86 proteins were significantly decreased, while the expression levels of CD163 and CD206 proteins were significantly higher. Further experiments confirmed that the expression of iNOS protein was significantly decreased after the VSL#3 intervention, and the expression of Arg-1 and Ym1 proteins was significantly increased. The VSL#3 was able to induce high expressions of p-GSK-3β and p-PTEN proteins, while the use of IL-10 antibody impaired the effect of the VSL#3. In summary, this research confirms that probiotics can alleviate renal dysfunction caused by ischemia and reperfusion by protecting the intestinal barrier function and maintaining the functions of intestinal flora. The pathway screening test of this study suggests that IL-10/GSK3β/PTEN may play an important role in the process of the prototypic VSL#3 inducing M2 transformation of macrophages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a common clinical critical illness, and more eyes should be attracted. The kidney is a highly perfused organ that often suffers from ischemia and reperfusion after shock, heart failure, or kidney transplantation [11]. Therefore, ischemia-reperfusion is one of the most important causes of acute kidney injury. In China, as one of the most common complications of patients with renal diseases, the incidence of AKI is 11.6% and its mortality is 8.8%. In addition, the incidence of AKI in critically ill patients exceeds 30%, while its mortality reaches as high as 50–80% [2]. Furthermore, the renal function in about 35–71% of AKI patients cannot fully recover after the illness [3, 4]. Even among patients whose results of renal function tests have returned to normal, some still develop chronically impaired renal functions and eventually progress to chronic kidney disease (CKD) or end-stage renal disease (ESRD). Previous studies showed that the risk of CKD or ESRD in surviving AKI patients was increased by 8.8-fold and 3.3-fold, respectively [5, 6]. Therefore, the mechanisms underlying post-AKI renal injury and repair have become a hotspot in the field of international kidney research.
After renal ischemic reperfusion injury (IRI), a series of pathological changes, such as impaired intestinal barrier function, intestinal flora, and endotoxin translocation, are caused by intestinal ischemia and hypoxia, which then activate intestinal cytokines, increase intestinal permeability, induce the translocation of intestinal flora and endotoxin, and trigger the systemic inflammatory response syndrome or even multiple organ dysfunction syndrome [7, 8, 10]. It exerts a great influence on the condition and prognosis of patients. Thus, timely and effective improvement of intestinal dysfunctions following renal IRI is of great significance to improve prognosis of the patients.
Severe types of renal IRI may lead to shortened intestinal villi, edema of the intestinal mucosa, and even intestinal necrosis and apoptosis. Studies have confirmed that probiotics can protect post-traumatic mechanical barriers by increasing the height of intestinal villi as well as the thickness and surface area of intestinal mucosa. It has been indicated that TNF-α, IL-1α, and IFN-γ can stimulate the apoptosis of intestinal epithelial cells [9]. In contrast, probiotics can maintain the integrity of intestinal epithelia by activating the anti-apoptotic signaling and blocking the apoptotic signaling pathway of MAPKp38. Wonseok found that probiotic VSL#3 can protect the intestinal epithelial barrier by activating P38 and the pathways of protein kinase signaling, thus increasing the expression of tight junction proteins both in vivo and in vitro [11].
Probiotics are a type of active microorganisms that are beneficial to the host and are often present in the human intestinal tract. Probiotics are known to antagonize harmful bacteria and carry specific enzymes (such as galactosidase) to facilitate the digestion and nutrient absorption in human body. In addition, probiotics produce antibacterial substances to reduce inflammation, to promote the production of secretary IgA (sIgA), to inhibit the secretion of IgE, and to enhance cellular immunity [12,13,14]. Therefore, probiotics help to correct the disorders of intestinal flora, to repair the gastrointestinal mucosal barrier and to increase immunity [15]. However, the study of probiotics is mainly concentrated in diseases of the digestive tract, and their roles and mechanisms in renal IRI remain uncertain. Therefore, in this study, a rat model of renal IRI was used to investigate the relationship between renal IRI and intestinal flora disturbance/intestinal barrier dysfunction. The aim of this study was to clarify the protective effect of probiotics on renal IRI and its possible mechanisms. It is hoped that this study can provide a new strategy for the prevention and treatment of renal IRI in clinical applications and provide a theoretical basis for the application of probiotics in the treatment of renal IRI.
Materials and methods
Preparation of an IRI animal model and experimental grouping
The male Wistar rats weighing 200 g ± 10 g were divided into six groups with six rats in each group. Intraperitoneal injection of 10% chloral hydrate (350 mg/kg) was performed for anesthesia of the rats in a fixed prone position, followed by disinfection and a 1.5-cm longitudinal incision at the paravertebral arch at the lower edge of the bilateral costal arch. In the I/R group and VSL#3 + I/R group, the bilateral renal pedicles were dissociated. The left renal pedicle was clipped by a non-invasive arterial clip. The color change of the left kidney from red to dark red indicated successful ischemic injury. After 45 min, the left renal artery clip was released and the right kidney was immediately removed. The color change of the left kidney was observed, and a change from dark red to red within 5 min indicated successful reperfusion. In the Sham group, the bilateral renal pedicles were dissected only, a piece of saline gauze was used to cover the incision, and the right kidney was removed 45 min later. The VSL#3 + I/R group was continuously instilled with the VSL#3 (0.6 g/kg/day) once a day for 2 weeks before ischemia-reperfusion. The VSL#3 + I/R + IL-10 antibody group was continuously administered with the VSL#3 (0.6 g/kg/day) once a day for 2 weeks before ischemia-reperfusion, and the tail vein was injected with IL-10 antibody (10 mg/kg) at 4 h after the operation. The VSL#3 + I/R + GSK-3β inhibitor group was continuously instilled with the VSL#3 (0.6 g/kg/day) once a day for 2 weeks before ischemia-reperfusion, and GSK-3β inhibitor (LiCL 15 mg/kg) was injected into the tail vein at 2 h after the surgery. The VSL#3 + I/R + PTEN inhibitor group was continuously infused with the VSL#3 (0.6 g/kg/day) once a day for 2 weeks before ischemia-reperfusion, and GSK-3β inhibitor (Bpv 1.6 μmol/kg) was injected into the tail vein at 2 h after the operation. The Sham and I/R groups were given an equal volume of saline for 2 weeks. After successful reperfusion, the surgical incision was sterilized and sutured. The rats were then completely resuscitated and placed back into the cage, where the rats were allowed to eat freely.
Western blot detection of related proteins
Kidney tissues or large intestine tissues were collected and homogenized after centrifugation, and the protein concentration was determined. Then, 50 μg of the protein sample was separated by SDS-electrophoresis and transferred to a PVDF membrane, which was blocked using a 5% skim milk solution at room temperature for 2 h and then incubated with rabbit anti-rat antibodies against ED-1, PCNA (1:400, Rockland, USA), ZO-1, Occludin, Claudin-1, Keap1, and Nrf2 (1:400, Sigma, USA), as well as goat anti-rat antibodies against CD68, CD86, CD163, CD206, iNOS, Arg-1, Ym1, IL-10, GSK-3β, and PTEN (1:200, Santa Cruz, USA), overnight on a 4 °C shaker. After washing, the membrane was incubated for 1 h at room temperature with horseradish peroxidase–labeled secondary antibody (1:2000, Jackson, USA) under shaking. ImageJ was used for coloration, exposure, scanning, and overall analysis.
Detection of biochemical indicators
The blood urea nitrogen (BNN) and serum creatinine (Scr) were measured by an automatic blood biochemical analyzer. The concentrations of Cys C, PRO, and NGAL in the urine of rats from each group were determined by ELISA according to the kit instructions.
Detection of inflammatory factors
The serum levels of MPO, IL-1β, IL-6, and TNF-α in the gastric mucosa of rats were determined by ELISA following the routine procedures.
Detection of intestinal mucosal barrier function
The serum DAO (Shanghai, China) activity was measured by spectrophotometry using an automatic biochemical analyzer (7600, Hitachi, Japan). The level of plasma endotoxin (Shanghai, China) was determined using the automated biochemical analyzer and a chromogenic substrate assay. The level of plasma d-lactic acid (Shanghai, China) was detected by enzyme-linked ultraviolet spectrophotometry following the manufacturer’s instructions.
Intestinal flora distribution
Samples of wet stools were collected from each group, and the distribution of intestinal microflora was determined using live plate counts. The Bifidobacterium and Lactobacillus culture media were first placed in an anaerobic jar and then incubated at 37 °C for 48–72 h. The Enterobacteriaceae and enterococcus culture media were directly placed into a 37 °C constant temperature incubator for 24~48 h of culture.
Statistical analysis
SPSS 19.0 software was used for analysis. Measured data were expressed as mean ± standard deviation. One-way analysis of variance was used for comparison between different groups. P < 0.05 was considered statistically significant.
Results
The probiotic VSL#3 can reduce the damage of renal functions after IRI
The renal function of rats was measured after 24 h of renal ischemia-reperfusion. The levels of BUN, Scr, Cys C, PRO, and NGAL were all significantly increased in the I/R group, but the level of Ccr was significantly decreased. After the VSL#3 intervention, the levels of BUN, Scr, Cys C, PRO, and NGAL all showed a significant decrease compared with their corresponding values in the I/R group, while the level of Ccr showed a significant increase (Fig. 1). These results showed that the pretreatment with the VSL#3 significantly reduced the renal damages caused by ischemia-reperfusion.
The probiotic VSL#3 can reduce inflammatory reaction induced by renal ischemia-reperfusion
The inflammatory index of the rats was measured at 24 h after reperfusion. As shown in Fig. 2, the plasma levels of MPO, IL-1β, TNF-α, and IL-6 were significantly increased in the I/R group. In addition, the levels of ED-1 and PCNA proteins in renal tissues were also increased in the I/R group. After the intervention with the VSL#3, the values of the above indicators dropped significantly. These results indicated that the VSL#3 protected renal functions by regulating the inflammation after IRI.
The probiotic VSL#3 can reduce the inflammatory reaction induced by renal ischemia-reperfusion. Levels of MPO a in renal tissue of the all experimental groups of rats. ***P < 0.001 vs. Sham group; #P < 0.05 vs. IR group. b Western blotting analysis of ED-1 and PCNA protein levels in renal tissue. c–e Levels of IL-1β, TNF-α, and IL-6 in renal tissue of the all experimental groups of rats. **P < 0.01; ***P < 0.001 vs. Sham group; #P < 0.05 vs. IR group
The probiotic VSL#3 can reduce intestinal barrier functions after renal ischemia-reperfusion
The changes in intestinal mucosal barrier functions and bacterial flora were investigated in this study. First, it was observed that the levels of endotoxin, DOA, and d-lactic acid (Fig. 3a–c), indicators of impairment of intestinal barrier functions, were all significantly elevated in the IR group. After the VSL#3 intervention, values of the above indicators significantly decreased compared with their corresponding values in the IR group. Then, the levels of intestinal barrier-associated proteins ZO-1, Occludin, and Claudin-1 (Fig. 3d) were measured. It was found that the protein expression of the above factors was significantly decreased in the IR group but the VSL#3 intervention significantly reversed the effect of IRI. In addition, the intestinal microflora of the feces collected from each group was also analyzed. The results showed that the number of enterococci and enterococci increased in the IR group, while the number of lactobacilli and bifidobacteria decreased significantly in the IR group (Fig. 3e–h). On the contrary, the VSL#3 intervention was able to maintain the number of beneficial bacteria in the gut while inhibiting the growth of harmful bacteria.
The probiotic VSL#3 can reduce intestinal barrier function after renal ischemia-reperfusion. a–c Levels of ET, d-lactate, and DOA in serum of the all the experimental groups of rats. **P < 0.01; ***P < 0.001 vs. Sham group; ##P < 0.01 vs. IR group. d Western blotting analysis of ZO-1, Occludin, and Claudin-1 protein levels in colon tissues. Contents of Enterococcus e, enterobacteria f, Lactobacillus g, and Bifidobacterium h in feces. *P < 0.05 vs. IR group
The probiotic VSL#3 reduces the oxidative stress caused by renal IRI and impairment of intestinal barrier function
Renal ischemia reperfusion and impairment of intestinal barrier function can trigger oxidative stress, which in turn can further impair renal and intestinal barrier functions. In this study, a significant decrease in the levels of CAT, GSH-PX, H2O2, and T-SOD (Fig. 4a–d) was observed in the IR group, but the treatment by the VSL#3 prevented IR-induced reduction. In addition, the expression of oxidative stress-related proteins Keap1 and Nrf2 (Fig. 4e) was detected in this study. The results showed that IR promoted the expression of Keap1 and Nrf2, but the treatment by the VSL#3 significantly decreased the expression of Keap1 and Nrf2.
The probiotic VSL#3 reduces oxidative stress caused by ischemia/reperfusion of the kidney and injury of intestinal barrier function. a–c Levels of ET, d-lactate, and DOA in serum of the all the experimental groups of rats. *P < 0.05; **P < 0.01; ***P < 0.001 vs. Sham group; #P < 0.05; ##P < 0.01 vs. IR group. d Western blotting analysis of Keap1 and Nrf2 protein levels in colon tissues
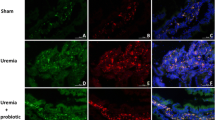
The probiotic VSL#3 promotes the M2 transformation and inhibits the M1 transformation of macrophages after renal ischemia-reperfusion
The surface markers and proteins specific to M1 and M2 types of macrophages were measured in this study. The results showed that the expression of CD68 and CD86 (surface markers of M1 macrophages) was high in the IR group, along with low expressions of CD163 and CD206 (surface markers of M2 macrophages) (Fig. 5a–e). After the VSL#3 intervention, the expression of CD68 and CD86 was significantly decreased, while the expression of CD163 and CD206 was significantly upregulated. Similarly, the expression of iNOS protein was high in the IR group, along with low expressions of Arg-1 and Ym1 (Fig. 5f–i) proteins. After the VSL#3 intervention, the expression of iNOS protein was significantly decreased, while the expression of Arg-1 and Ym1 proteins was increased considerably. The above results suggested that renal IRI promoted the phenotype transformation of macrophages into M1. The previous results obtained from the authors of this study showed that IR induced the M1 transformation of macrophages and the release of pro-inflammatory cytokines IL-6 and TNF-α, consistent with the above observations.
The probiotic VSL#3 promotes macrophage transformation to M2 after renal ischemia-reperfusion and inhibits M1-type transformation. a Western blotting analysis of CD68, CD86, CD163, and CD206 protein levels in renal tissue. b–e Analysis of CD68, CD86, CD163, and CD206 protein expression. Statistical analyses were done with one-way ANOVA. **P < 0.01; ***P < 0.001 vs. IR group. f Western blotting analysis of iNOS, Arg-1, and Ym1 protein levels in renal tissue. g–i Analysis of iNOS, Arg-1, and Ym1 protein expression. Statistical analyses were done with one-way ANOVA. *P < 0.05; **P < 0.01; ***P < 0.001 vs. IR group
The probiotic VSL#3 regulates the phenotypic changes of macrophages via the IL-10/GSK3β/PTEN signaling
Previous studies have demonstrated that the probiotic VSL#3 exerts a protective effect on renal IRI by inducing the transformation of activated macrophages into the M2 phenotype. However, it remains unclear how the VSL#3 alters the phenotypes of macrophages. Others have shown that IL-10 induced the M2 transformation of macrophages in vitro. Therefore, IL-10 antibodies were used here to determine whether the VSL#3 also regulated the transformation of macrophages via IL-10. The results showed that the incubation with an anti-IL10 antibody inhibited the phenotypic changes caused by the VSL#3. In addition, the expression of CD68 and CD86 was increased, while the expression of CD163 and CD206 was decreased after the treatment (Fig. 6c). Similarly, the expression of iNOS was significantly increased, while the expression of Arg-1 and Ym1 (Fig. 6d) was significantly decreased. Therefore, it can be concluded that the VSL#3 was involved in the transformation of macrophages via the function of IL-10.
The probiotic VSL#3 regulates macrophage phenotypic changes through IL-10/GSK3β/PTEN signaling. Western blotting analysis of IL-10 (a); p-GSK3β and p-PTEN (b); CD68, CD86, CD163, and CD206 (c); iNOS, Arg-1, and Ym1 (d); p-GSK3β and p-PTEN (e); p-GSK3β (f); and p-PTEN (g) protein levels in renal tissue
In order to clarify what signaling pathways are utilized by IL-10 to change the phenotypes of macrophages, the GSK-3β/PTEN signaling pathway was investigated here. Western blot results showed that the VSL#3 induced the protein expression of p-GSK-3β and p-PTEN, whose expression was reduced in the presence of an IL-10 antibody (Fig. 6b). These results confirmed that the VSL#3 regulated the phenotypic changes of macrophages via IL-10 and its downstream GSK-3β/PTEN signaling.
The above studies demonstrate that IL-10 increases the expression of p-GSK3β and p-PTEN. To further clarify the relationship between GSK-3β and PTEN, inhibitors of GSK3β and PTEN were used to investigate their functions. The results showed that GSK-3β inhibitors inhibited the expression of p-PTEN, although PTEN inhibitors cannot always induce the expression of p-GSK-3β (Fig. 6e–g). These results suggested that GSK-3β may regulate the phosphorylation of upstream p-PTEN and induce the phenotypic change of macrophages. In summary, it was found in this study that the probiotic VSL#3 induced the M2 transformation of macrophages after renal IRI through the IL-10/GSK3β/PTEN signaling pathway.
Discussion
In this study, a rat model was used to investigate the protective effect of probiotics on renal IRI. Probiotics can reduce renal dysfunctions caused by ischemia and reperfusion, protect the intestinal barrier function, and maintain the intestinal flora. As a result, probiotics can also reduce early-stage inflammatory reactions and oxidative stress, thus preventing the M1 transformation but promoting the M2 transformation of macrophages. This study also showed that the regulatory effect of the probiotic VSL#3 on the macrophage phenotype was exerted through IL-10, and it was further confirmed that the GSK3β/PTEN signaling acted as an important downstream signaling pathway of IL-10. These results showed that probiotics can protect kidney damages caused by ischemia and reperfusion, thus providing powerful experimental evidence for the clinical use of probiotics in the treatment of renal IRI.
It is known that the kidney acts as an important endocrine and excretion organ in the human body by excreting most of metabolites and by maintaining the internal environment of the body [16]. The blood flow in kidney is very rich, accounting for about 1/4 of the cardiac output. Therefore, kidney is particularly vulnerable to ischemia and reperfusion [17, 18]. In solid organ transplantation, IRI has become one of the most important antigenic and non-immune factors affecting graft survival, and the presence of IRI in renal transplantation can induce acute rejection. The apoptosis of renal tubular epithelial cells can also cause delayed graft function (DGF) after renal transplantation, eventually leading to decreased survival of transplanted kidneys [19]. Therefore, it is of great clinical significance to adopt an effective method to alleviate renal IRI, to prevent acute rejection after renal transplantation, and to improve the long-term survival of patients with transplanted kidneys [20, 22, 23]. This study found that renal dysfunctions were detectable after 24-h ischemia-reperfusion since a large amount of pro-inflammatory factors were secreted by damaged tubular cells. Pretreatment with the probiotic VSL#3 resulted in less impairment of renal functions after IRI and subsequently alleviated inflammatory responses, suggesting that probiotics can reduce the degree of renal damages after IRI.
IRI is inevitable in renal transplantation. After renal IRI, the level of inflammatory factors in the patient increases and induces a complex inflammatory response [21, 24]. The outbreak of inflammatory factors and inflammatory mediators leads to secondary inflammatory attacks and damages to the gastrointestinal mucosa, thus aggravating gastrointestinal mucosal dysfunctions [25]. In this case, severe patients even develop sepsis, septic shock, and multiple organ dysfunction (MODS), which can even lead to death [26]. Previous studies have shown that probiotics can effectively improve post-operative nutritional status and inflammation, thus reducing the risk of nosocomial infection and shortening the length of ICU stay.
When the intestinal flora is disturbed, pathogenic bacteria competitively adhere to intestinal epithelial cells and induce their apoptosis, thus disrupting the cytoskeleton, affecting the phosphorylation of tight junction proteins, increasing the permeability of intestinal mucosa, and increasing the level of serum endotoxin [27]. High levels of endotoxin in serum activate monocytes and macrophages in the blood to release a large amount of pro-inflammatory cytokines, which in turn mediate inflammatory reactions and activate the synthesis of NO by iNOS, thus further increasing the permeability of the intestinal mucosa and inflammatory responses. This situation becomes more serious upon intestinal damages by creating a vicious cycle. Therefore, when the permeability of intestinal mucosa increases, the levels of serum endotoxin also increase, which in turn lead to more severe inflammatory reactions and increase the incidence of infections. In this study, it was found that the levels of endotoxin, DOA, and d-lactic acid were all significantly decreased after the VSL#3 intervention. In addition, the levels of intestinal barrier-associated proteins ZO-1, Occludin, and Claudin-1 were significantly increased after the VSL#3 intervention by maintaining the number of beneficial bacteria in the intestine and by inhibiting the growth of harmful bacteria. At the same time, the VSL#3 intervention also prevented the decrease in CAT, GSH-PX, H2O2, and T-SOD, and downregulated the expression of Keap1 and Nrf2. It is suggested that when probiotics are used to treat renal IRI, the response induced by oxidative stress is inhibited, intestinal permeability is improved, and integrity of gastrointestinal mucosa barrier is reconstructed and maintained.
Macrophages are a kind of multifunctional immune cells. In innate immunity, the main function of macrophages is to kill infected pathogenic microorganisms, to engulf necrotic tissue fragments and apoptotic cells, and to participate in the repair of damaged tissues. As classical antigen-presenting cells, macrophages also participate in the initiation of T cell responses [28, 30]. In fact, activated macrophages can secrete a variety of cytokines and play an important role in the regulation of immune responses [29]. The previous results showed that renal IRI impairs the intestinal barrier function and increases the level of inflammatory responses. In this case, a variety of media can induce the M1 differentiation of macrophages. M1 macrophages are known to aggravate renal cell damages and apoptosis by releasing a large amount of inflammatory mediators. In this study, it was found that the intervention with the VSL#3 significantly decreased the expression levels of CD68 and CD86 while significantly upregulating the expression of CD163 and CD206. Further experiments confirmed that the expression of iNOS protein was also significantly decreased by the VSL#3 intervention, while the expression of Arg-1 and Ym1 proteins was significantly increased. The above results suggested that renal IRI induces the M1 transformation of macrophages while inhibiting their M2 transformation. Our previous results showed that renal IR-induced M1 transformation of macrophages also triggered the release of pro-inflammatory cytokines IL-6 and TNF-α, consistent with the above observations.
IL-10 is thought to inhibit the activation of antigen-presenting cells, thereby suppressing excessive inflammatory responses [32]. It has been pointed out that IL-10 plays an important role in the reversal of macrophages by Treg cells. It was also found in this study that the probiotic VSL#3 regulated the transformation of macrophage phenotypes via IL-10. Other studies suggest that PI3K/Akt signaling acts as an important signaling pathway for microglia polarization to M2, whereas GSK3β/PTEN is an upstream of PI3K/Akt [31]. This study also suggested that the probiotic VSL#3 could reverse the downregulation of GSK3β phosphorylation in macrophages, thereby preventing the decrease in PTEN phosphorylation. In summary, the findings of this study indicate that IL-10/GSK3β/PTEN acts as an important signaling pathway involved in the VSL#3-induced M2 transformation of macrophages.
References
Allison SJ (2015) Acute kidney injury: activated protein c protective in iri. Nat Rev Nephrol 11(8):445
Aguilar A (2016) Acute kidney injury: loss of pkc-ɛ protects against iri. Nat Rev Nephrol 12(12):714
Binek M, Kizerwetter-Swida M, Cisek AA, Rzewuska M, Chrobak-Chmiel D, Gierynska M (2016) Mechanisms of maintenance of intestinal homeostasis by autochthonic microbiota and probiotics. Medycyna Weterynaryjna 72(10):611–615
Bron PA, Kleerebezem M, Brummer RJ, Cani PD, Mercenier A, Macdonald TT et al (2017) Can probiotics modulate human disease by impacting intestinal barrier function? Br J Nutr 117(1):93–107
Carney EF (2016) Acute kidney injury: role of platelet activation and nets in renal IRI. Nat Rev Nephrol 12(12):715
Chen K, Xie W, Luo B, Xiao W, Teitelbaum DH, Yang H et al (2016) Intestinal mucosal barrier is injured by bmp2/4 via activation of nf-b signals after ischemic reperfusion. Mediat Inflamm 2014(3):901530
Dai H, Wang M, Patel PN, Kalogeris TJ, Liu Y, Durante W et al (2017) Preconditioning with the bkca channel activator ns-1619 prevents ischemia/reperfusion-induced inflammation and mucosal barrier dysfunction: ros and ho-1. Am J Physiol Heart Circ Physiol 313(5):ajpheart.00620.2016
Ferenbach DA (2010). Role of the macrophage in acute kidney injury. University of Edinburgh, [Thesis]
Fan LH, Ting-Liang FU, Han XL (2017) The function and influence to intestinal barrier in ischemia-reperfusion injury. China Modern Medicine 8(11):348–351
Fan J, Xin J, Shao W (2017) Effects of probiotics combined with olsalazine sodium on intestinal mucosal barrier function and rage,srage in patients with ulcerative colitis. Journal of Guangxi Medical University 14(8):264–267
Han B, Sheng B, Zhang Z, Pu A, Yin J, Yang H (2016) Effect of aryl hydrocarbon receptor activation on intestinal mucosal barrier in mice after acute intestinal ischemia reperfusion injury. J Third Mil Med Univ 22(17):458–462
Jang HD, Noh JY, Shin JH, Lin JJ, Lee SY (2013) Pten regulation by the akt/gsk-3β axis during rankl signaling. Bone 55(1):126–131
Lech M, Gröbmayr R, Mi R, Lorenz G, Hartter I, Mulay SR et al (2014) Macrophage phenotype controls long-term Aki outcomes—kidney regeneration versus atrophy. J Am Soc Nephrol 25(2):292–304
Li X, Pu Y, Qiu Y, Wang W, Yang H, Xiao W (2017) Effect of adenosine 2a receptor on intestinal barrier function in mice with acute reperfusion injury. J Third Mil Med Univ 27(9):382–385
Luo B, Chen K, Feng Q, Xiao W, Ma D, Yang H et al (2018) The interplay of bmp4 and il-7 regulates the apoptosis of intestinal intraepithelial lymphocytes under conditions of ischemia̸reperfusion. Int J Mol Med 41(5):348–352
Meng XM, Tang PMK, Li J, Lan HY (2015) Macrophage phenotype in kidney injury and repair. Kidney Dis 1(2):138–146
Nakamura K, Zhang M, Kageyama S, Ke B, Sosa R, Reed E et al (2017) Myeloid HO-1 regulates M2 macrophage activation in liver ischemia-reperfusion injury (IRI). American Transplant Congress 17:550–550
Pang M, Qingping LU, Zhu L, Xia B, Zhang H (2016) Effects of probiotics to against acute diarrhea and on intestinal mucosal barrier of rats. Chin J Animal Nutr 12(6):274–277
Ren K, Chao J, Ma P, Ren Q, Jia Z, Zhu D (2016) Ginsenoside rd alleviates mouse acute renal ischemia/reperfusion injury by modulating macrophage phenotype. J Ginseng Res 40(2):196–202
Rosero O, Molnár D, Harsányi L, Szijártó A, Onody P, Kovács T et al (2014) Impaired intestinal mucosal barrier upon ischemia-reperfusion: “patching holes in the shield with a simple surgical method”. Biomed Res Int 2014(6):210901
Shu X, Zhang J, Wang Q, Xu Z, Yu T (2016) Glutamine decreases intestinal mucosal injury in a rat model of intestinal ischemia-reperfusion by downregulating hmgb1 and inflammatory cytokine expression. Exp Ther Med 12(3):1367–1372
Singh AP, Singh N, Singh Bedi PM (2016) Estrogen attenuates renal IRI through PPAR-γ agonism in rats. J Surg Res 203(2):324–330
Suguru Y, Jiayong Z, Yancey PG, Yiqin Z, Linton MRF, Sergio F et al (2015) Atherosclerosis following renal injury is ameliorated by pioglitazone and losartan via macrophage phenotype. Atherosclerosis 242(1):56–64
Sun M, Zhang Z, Han X, Zhang X & Anesthesiology DO (2017) Breviscapine pretreatment attenuates ischemia reperfusion induced intestinal mucosal barrier damage via promoting enos/no production. J Pract Med
Thorenz A, Schröder C, Dressler L, Skwirblies F, Chen R, Hüper K et al (2017) Mp236c5ar2 defficiency attenuates renal iri via il-10 dependent mechanisms. Nephrol Dial Transplant 32(suppl_3):512
Tian S, Zhang L, Tang J, Guo X, Dong K, Chen SY (2015) Hmgb1 exacerbates renal tubulointerstitial fibrosis through facilitating m1 macrophage phenotype at the early stage of obstructive injury. Am J Physiol Ren Physiol 308(1):69–75
Tian N-q, Su Y-t, Wang X-z, General Medicine Department, Baoji Central Hospital, & Cardiology Department et al (2018) Clinical effect of probiotics combined with glutamine in the treatment of liver cirrhosis and its effect on intestinal mucosal barrier and liver function. Clinical Research and Practice
Yang W, Nam KS, Ji-hyun J, Lee K-m, Sunhwa O, Shin I (2014) S100a4 negatively regulates β-catenin by inducing the egr-1-pten-akt-gsk3β degradation pathway. Cell Signal 26(10):2096–2106
Zhang Y, Zhang J, Nephropathy DO (2015) Mycophenolate mofetil affects toll-like receptor 4 signaling pathway of monocytes in renal ischemia/reperfusion injury(iri) of mice. Chinese Journal of Clinicians 17(13):363–366
Zhang Y, Zhang J, Nephropathy DO (2015) Mycophenolate mofetil affects toll-like receptor 4 signaling pathway of monocytes in renal ischemia/reperfusion injury (IRI) of mice. Chinese Journal of Clinicians (electronic version) 17(13):363–366
Zhou J, Ping FF, Lv WT, Feng JY, Shang J (2014) Interleukin-18 directly protects cortical neurons by activating pi3k/akt/nf-κb/creb pathways. Cytokine 69(1):29–38
Zhou J, Ping FF, Lv WT, Feng JY, Shang J (2014) Interleukin-18 directly protects cortical neurons by activating pi3k/akt/nf-κb/creb pathways. Cytokine 69(1):29–38
Funding
This work was supported by the scientific and technological project of Shaanxi Province (No. 2016SF-246); the National Nature Science Foundation of China (No. 81670681); and the Major clinical research projects of the First Affiliated Hospital of Xi’an Jiao Tong University (XJTU1AF-CRF-2015-005).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ding, C., Han, F., Xiang, H. et al. Probiotics ameliorate renal ischemia-reperfusion injury by modulating the phenotype of macrophages through the IL-10/GSK-3β/PTEN signaling pathway. Pflugers Arch - Eur J Physiol 471, 573–581 (2019). https://doi.org/10.1007/s00424-018-2213-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-018-2213-1