Abstract
Defects of the gap junction protein connexin 40 (Cx40) in renin-secreting cells (RSCs) of the kidney lead to a shift of the localization of RSCs from the media layer of afferent arterioles to the periglomerular interstitium. The dislocation of RSCs goes in parallel with elevated plasma renin levels, impaired pressure control of renin secretion, and hypertension. The reasons for the extravascular shift of RSCs and the blunted pressure regulation of renin secretion caused by the absence of Cx40 are still unclear. We have therefore addressed the question if Cx40 is essential for the metaplastic transformation of preglomerular vascular smooth muscle cells (SMCs) into RSCs and if Cx40 is essential for the pressure control of renin secretion from RSCs located in the media layer of afferent arterioles. For our study, we used mice lacking the angiotensin II type 1A (AT1A) receptors, which display a prominent and reversible salt-sensitive metaplastic transformation of SMCs into RSCs. This mouse line was crossed with Cx40-deficient mice to obtain AT1A and Cx40 double deleted mice. The kidneys of AT1A −/−Cx40−/− mice kept on normal salt (0.3 %) displayed RSCs both in the inner media layer of preglomerular vessels and in the periglomerular interstitium. In contrast to hypotensive AT1A −/− (mean bp syst 112 mmHg) and hypertensive Cx40−/− (mean bp syst 160 mmHg) mice AT1A −/−Cx40−/− mice were normotensive(mean bp syst 130 mmHg). Pressure regulation of renin secretion from isolated kidneys was normal in AT1A −/− mice, but was absent in AT1A −/−Cx40−/− mice alike in Cx40−/− mice. Low-salt diet (0.02 %) increased RSC numbers in the media layer, whilst high-salt diet (4 %) caused disappearance of RSCs in the media layer but not in the periglomerular interstitium. Blood pressure was clearly salt sensitive both in AT1A −/− and in AT1A −/−Cx40−/− mice but was shifted to higher pressure values in the latter genotype. Our data indicate that Cx40 is not a requirement for intramural vascular localization of RSCs nor for reversible metaplastic transformation of SMCs into RSCs. Therefore, the ectopic localization of RSCs in Cx40−/− kidneys is more likely due to a disturbed intercellular communication rather than being the result of chronic overactivation of the renin-angiotensin-aldosterone system or hypertension. Moreover, our findings suggest that Cx40 is a requirement for the pressure control of renin secretion irrespective of the localization of RSCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
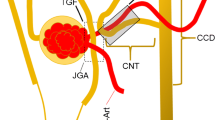
Renin-secreting cells (RSCs) of the kidneys are typically located in the terminal portions of afferent arterioles at juxtaglomerular position, and they regulate renin secretion in response to blood pressure, adrenergic neurotransmitters, and a variety of hormones and autacoids [14]. They display a strong expression of the gap junction protein connexin 40 (Cx40) [15, 16]. In states of renin cell recruitment as it occurs in chronic threats of volume and of blood pressure homeostasis, additional smooth muscle cells (SMCs) of preglomerular arterioles transform into RSCs. This metaplastic transformation of SMCs is associated with an induction of Cx40 expression and downregulation of connexin 45 [13]. Cx40-gap junctions couple RSCs among each other and their neighbors, such as endothelial, mesangial, and SMCs [28]. Loss of function defects of Cx40 in RSCs leads to a translocation of RSCs from the media layer of afferent arterioles into the periglomerular interstitium [17] and an enhancement of renin secretion due to interruption of the negative pressure control leading to hypertension [3, 12, 30]. The reasons for this particular relevance of Cx40 for the localization and function of RSCs are yet unknown.
The disappearance of RSCs from the smooth muscle cell layer may reflect an essential requirement of Cx40 for RSCs to integrate into the vessel wall. It may also be secondarily caused by the persistent hypertension and/or chronically increased levels of angiotensin II in states of defective Cx40. The missing pressure control of renin secretion in the absence of Cx40, leading to renin hypersecretion and hypertension, may simply result from the inability of extramural cells to sense the intravascular pressure.
We were therefore interested to see if preglomerular SMCs can transform into RSCs and exist in the media layer in the absence of Cx40. If so, we further aimed to find out if the cells located in the media layer of preglomerular vessels but lacking Cx40 show a normal or an altered secretory response to the perfusion pressure.
To address these questions, we aimed to examine mice lacking angiotensin II type 1A (AT1A −/−) receptor [22] with intact or with deleted Cx40 (Cx40−/−). There were several reasons to use AT1A −/− mice for this study. Firstly, they show a prominent vascular recruitment of RSCs, which can be triggered by low-salt intake [21]. Secondly, they have an ineffective renin-angiotensin-aldosterone system (RAAS), which should counteract effects of renin hypersecretion on the RAAS seen in Cx40-defective mice [21, 28, 29]. Thirdly, AT1A −/−Cx40−/− mice are expected to have lower blood pressure than Cx40-deficient mice, if the hypertension induced by Cx40 deletion is causally mediated by activation of the RAAS.
Materials and methods
Animals
AT1A and Cx40 double knockout (AT1A −/−Cx40−/−) mice were generated by crossing Cx40-deficient (Cx40−/−) mice of C57BL/6 genetic background which are originally generated by Kirchhoff et al. [10] and obtained from K. Willecke (Institute of Genetics, University of Bonn, Germany) and angiotensin II-AT1A receptor-deficient (AT1A −/−) mice of 129/Sv background, provided by T. M. Coffman [8]. Wild-type (wt) mice were obtained from the F2 generations of AT1A -/-Cx40-/- mice and C57BL/6-129/Sv breedings. For all experiments, female 16- to 24-weeks-old mice were used. Genotyping was performed by PCR on DNA isolated from tail biopsies using the following primers: Cx40-1 5′-gggagatgagcaggccgacttccggtgcg-3′; Cx40-2 5′-gtagggtgccctggacaatcttccc-3′; Cx40-3 5′-ggatcggccattgaacaagatggattgcac-3′; Cx40-4 5′-ctgatgctcttcgtccagatcatcctgatcg-3′. Primers 1 and 2 amplify a 494-bp fragment from the Cx40 knockout allele. Primers 3 and 4 amplify a 314-bp fragment from the Cx40 wt allele. AT1A-1 5′-tgagaacaccaatctcactg-3′; AT1A-2 5′-ttcgtagacaggcttgag-3′; AT1A-3 5′-ccttctatcgccttcttgacg-3′ (wild-type band, 483 bp; mutant band, 520 bp). All animal experiments were performed according to the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the local authorities. For changes in oral salt intake, a group of six female mice received a low-salt diet (0.02 % w/w NaCl; Ssniff Spezialdiäten, Soest, Germany) or a high-salt diet (4 % w/w NaCl) for 10 days, while a control group (n = 10) obtained a standard rodent chow (0.3 % w/w NaCl).
Blood pressure measurements
Measurements of the systolic arterial pressure were performed noninvasively by tail cuff manometry (TSE Systems, Germany). Therefore, the blood pressure of conscious mice was measured in a 37 °C warm box at the same time of the day. Before the first blood pressure determination, the animals were habituated to the experiment procedure by placing them into the holding device on 5–7 subsequent days for 15 min per day. On 10 sequential days, 5 measures per day were analyzed. The mean value per day and mouse was used for calculation.
Determination of renin mRNA expression by real-time PCR
Animals were anesthetized by i.p. injection of ketamine (80 mg/kg body weight; bela-pharm, Germany) and xylazine (12 mg/kg body weight; Serumwerk, Germany). After ligation of the left renal artery, the kidney was removed, frozen in liquid N2, and stored for mRNA analysis. Total RNA was isolated from frozen kidneys as described by Chomczynski and Sacchi [2] and quantified by a photometer. The cDNA was synthesized by MMLV reverse transcriptase (Superscript; Invitrogen). For quantification of renin mRNA expression, real-time PCR was performed using a LightCycler 480 Instrument (Roche Diagnostics Corp.) and the LightCycler SYBR Green I Master kit (Roche Diagnostics Corp.) and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) as a control. For amplification of mouse renin and GAPDH cDNAs, the following primers were used: renin-1 5′-atgaagggggtgtctgtggggtc-3′; renin-2 5′-atgcggggagggtgggcacctg-3′; GAPDH-1 5′-atgccatcactgccacccagaag-3′; GAPDH-2 5′-acttggcaggtttctccaggcgg-3′. The primers used to analyze the Cx37, Cx40, Cx43, and Cx45 mRNA expression were previously described [15].
Immunohistochemistry and 3D reconstruction
For immunohistochemistry and 3D reconstruction, the right kidney was perfused with 40 ml of 3 % paraformaldehyde solution in phosphate buffered saline (pH 7, 4) at a constant perfusion pressure of 120 mmHg through the abdominal aorta. After dehydration and embedding in paraffin, 5-μm-thick serial slices were stained for renin and α-SMA. The deparaffinized kidney sections were blocked with 10 % horse serum, 1 % BSA in PBS, incubated with anti-renin (1:400, generated by Davids Biotechnologie, Germany) and anti-α-SMA (1:600, Abcam, Cambridge) antibodies overnight at 4 °C, followed by incubation with fluorescent secondary antibodies. Slices were mounted with DakoCytomation Glycergel mounting medium. The digitalization of the antibody-stained serial sections (40–60) was performed using an AxioCam MR3 camera mounted on an Axiovert 200M microscope with fluorescence filters (TRITC, filter set 43; Cy2, filter set 38; Zeiss, Germany). The resulting image sequence was converted to an image stack with constant picture size with the graphics software ImageJ (Wayne Rasband; NIH, Bethesda, MD). The equalized data were imported into Amira 5.6 software (FEI Visualization Group, Berlin, Germany) for subsequent generation of aligned grayscale stacks of renin and α-SMA. After correct scaling and alignment, renin and α-SMA were labeled and assigned to different defined materials. Finally, the surfaces were computed from the material data, resulting in a 3D model of α-SMA and renin. All shown surfaces base upon these segments.
Volume calculations
Renin-immunoreactive volume per glomerulus was calculated by Amira 5.6. from 3D kidney reconstructions of three animals per experimental group containing seven to ten glomeruli each. Data is expressed in cubic micrometers.
Isolated perfused mouse kidney
The isolated perfused mouse kidney model has been described in detail elsewhere [7]. Briefly, the kidneys were perfused ex situ with a modified Krebs-Henseleit solution [25] supplemented with 6 g/100 ml bovine serum albumin and human red blood cells (10 % hematocrit) at a constant pressure of 90 mmHg. Using an electronic feedback control, perfusion pressure could be changed stepwise in a pressure range between 40 and 140 mmHg to assess the pressure control of renin secretion. Chemicals to be tested for their effects on renin secretion were prepared as stock solutions and infused into the arterial limb of the system. For the determination of renin secretion rates (RSR), three samples of the venous effluent were taken every 2 min. Renin activity in the venous effluent was measured by radioimmunoassay (RENCTK; DiaSorin, Germany) as described [5, 7]. RSR is denoted as perfusate flow (ml/gorgan weight × min−1) multiplied by renin activity (ngANG I/ml × h−1) of the perfusate.
Aldosterone and renin measurements in plasma samples
Blood samples from mice were taken by facial vein puncture and collected in EDTA-coated capillaries. Plasma was separated by centrifugation in a hematocrit centrifuge and stored at −20 °C until measurements. A specific ELISA from IBL (Hamburg, Germany) was used to determine the concentration of aldosterone in appropriate dilutions of plasma. For determination of plasma renin concentration, plasma samples were incubated for 1.5 h at 37 °C with plasma from bilaterally nephrectomized male rats as renin substrate. The generated angiotensin I (ng/ml × h−1) was determined by radioimmunoassay (RENCTK; DiaSorin, Germany).
Statistical analysis
All values are presented as mean ± SE. Differences between experimental groups were calculated by analysis of variance (ANOVA) and Bonferroni’s adjustment for multiple comparisons. P values less than 0.05 were considered statistically significant unless otherwise specified. Prism 5.0 software (GraphPad, San Diego, CA) was used for all calculations.
Results
Basic characterization of mice
Basic data of the four genotypes of mice used in this study are summarized in Table 1. Kidney weights were not different between the genotypes. Whilst heart weights were increased in Cx40-deficient mice, heart weights were normal in AT1A −/−Cx40−/− mice. Plasma renin concentration was increased in Cx40−/− mice and even more in AT1A −/− mice. The plasma renin concentration of AT1A −/−Cx40−/− mice was between those of Cx40−/− and AT1A −/− mice. Plasma aldosterone concentration was increased in Cx40−/− mice only among the four genotypes under investigation. Renal connexin 40 mRNA was increased in AT1A −/− mice (Table 2). Renal connexin 37, 43, and 45 mRNA levels were not different between the four genotypes under investigation (Table 2).
Intrarenal localization of RSCs in AT1A −/−Cx40−/− mice on a normal salt diet
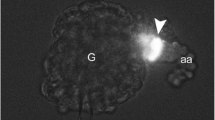
In wild-type mice kept on a normal salt diet, RSCs were restricted to the classical juxtaglomerular position, where RSCs continued the media layer of afferent arterioles into the glomeruli (Fig. 1a). Virtually every glomerulus had a few cubic-shaped RSCs at its vascular pole (Fig. 2a). In Cx40-deficient kidneys, RSCs showed a more variable distribution pattern with regard to localization and numbers (Fig. 1b). RSCs were localized outside the arteriolar vessel wall and showed a more irregular circumference. Some of the cells extended into the peritubular/periglomerular interstitium. Virtually all RSCs were associated with glomeruli, however, with interglomerular differences in the number of RSCs per glomerulus (Fig. 2b). The kidneys from AT1A −/− mice showed an increased number of RSCs, which were almost exclusively localized in the vascular walls (Fig. 1c). RSCs were found over the whole length of afferent arterioles, sometimes also in the walls of interlobular arteries (Fig. 2c). In the kidneys of AT1A −/−Cx40−/− mice, a mixed distribution pattern of RSCs was found. It was an assembly of RSCs which were localized inside the vessel wall in the media layer of afferent arterioles as in AT1A −/− mice and cells of a more irregular shape which were situated outside the vessel wall, similar to the findings in Cx40−/− kidneys (Fig. 1d). Under normal salt diet, RSCs were localized ectopically as well as in correct intramural position. In AT1A −/−Cx40−/− kidneys, RSCs were more restricted to the juxta/periglomerular areas and did not spread over the whole length of afferent arterioles such as those in AT1A −/− kidneys (Fig. 2d).
Representative immunohistochemical stainings of renin (green) and α-smooth muscle actin (α-SMA, red) in kidneys under normal salt conditions of wild-type (wt) (a), Cx40−/− (b), AT1A −/− (c), and AT1A −/−Cx40−/− (d) mice. All figures show afferent arterioles (aa), RSCs, glomeruli (G), and tubules (not marked). In wt kidneys, RSCs continue the media layer (α-SMA positive) of afferent arterioles at the glomerular vascular pole (a, arrows). In Cx40−/− kidneys, RSCs are located outside the media layer of afferent arterioles in the periglomerular area (b, arrowheads). In AT1A −/− kidneys, RSCs are located in the media layer of afferent arterioles (c, arrows). Yellow color indicates overlay of renin and α-SMA immunoreactivity. In AT1A −/−Cx40-/- kidneys, RSCs are located both within the media layer of afferent arterioles (d, arrows) and outside in the periglomerular interstitium (d, arrowheads). Scale bar = 50 μm
3D reconstructions of renin-immunoreactive areas (dark gray) and α-smooth muscle actin (α-SMA, light gray) in kidneys under normal salt conditions of wild-type (wt) (a), Cx40−/− (b), AT1a −/− (c), and AT1A −/−Cx40−/− (d) mice. 3D reconstructions show interlobular arteries (ia), afferent arterioles (aa), glomeruli (G), and efferent arterioles (ea). The pictures indicate the classic distribution pattern with RSCs conferred to the juxtaglomerular apparatus in wt mice (a, arrow) and dislocation of RSCs to the periglomerular interstitium in Cx40−/− mice (b, arrowhead). AT1A −/− mice displayed a marked increase in the number of RSCs in juxtaglomerular areas and along afferent arterioles and interlobular arteries (c, arrows), whereas AT1A −/−Cx40−/− mice showed RSCs along afferent arterioles (d, arrow) and in the periglomerular interstitium (d, arrowhead). Scale bar = 50 μm
The quantitative impression of renin expression derived from the 3D reconstructions (Fig. 2) was corroborated by calculations of renin-immunoreactive volumes from the 3D reconstructions. Those calculations revealed 5-fold and 3-fold increases of renin-immunoreactive volumes in AT1A −/− and AT1A −/−Cx40−/− mice, respectively (Fig. 3a), whilst the renin-immunoreactive volume in Cx40−/− mice was not significantly changed. Renin mRNA abundance was doubled in Cx40−/− mice and was increased 6- and 3-fold in AT1A −/− and AT1A −/−Cx40−/− mice, respectively (Fig. 3b). Plasma renin concentrations paralleled the changes of renin mRNA (Table 1).
a Renin-immunoreactive volume per glomerulus of wild-type (wt), Cx40−/−, AT1A −/−, and AT1A −/−Cx40−/− mice under normal salt conditions calculated from 3D reconstructions (7 to 10 glomeruli analyzed from 3 kidneys per group). b Renin mRNA abundance in the kidneys of Cx40−/−(n = 7), AT1A −/− (n = 7), and AT1A −/−Cx40−/− (n = 10) mice under normal salt conditions compared to wild-type (wt; n = 10) mice. c Systolic blood pressure of wild-type (wt), Cx40−/−, AT1A −/−, and AT1A −/−Cx40−/− mice (5 animals per group). All data are mean ± SE. *P < 0.05 vs wt control, #P < 0.05 (ANOVA) between the indicated groups
Recruitment of RSCs in AT1A −/−Cx40−/− mice by variation of oral salt intake
Next, we determined if in the absence of Cx40, mural cells of preglomerular vessels can undergo reversible metaplastic transformation into RSCs and vice versa. For this aim, AT1A −/− and AT1A −/−Cx40−/− mice were fed low- (0.02 %) and high- (4 %) salt diets for 10 days, and renin cell distribution and renin mRNA abundance were analyzed thereafter. In AT1A −/− kidneys, low-salt diet further increased and high-salt diet markedly reduced the number of preglomerular mural cells expressing cells (Figs. 4a, 5a, and 6a, c). During low-salt diet, mural RSCs almost completely covered the entire afferent arterioles and in part also interlobular arteries. During high-salt diet, RSCs were more restricted to the walls of terminal parts of afferent arterioles. In AT1A −/−Cx40−/− kidneys, low-salt diet also further increased and high-salt diet reduced the number of RSCs (Figs. 4b–d, 5b, and 6b, d). The increase of the number of RSCs during low-salt diet resulted from a clear recruitment of renin expression in the vessel walls of the afferent arterioles on the one hand (Figs. 4c and 6b), which, however, was less prominent than in the AT1A −/− kidneys (Figs. 4a and 6a). In AT1A −/−Cx40−/− mice kept on high-salt diet, mural RSCs had disappeared and only ectopic periglomerular RSCs remained visible (Figs. 5b and 6d). The quantitative impression of renin expression derived from the 3D reconstructions (Fig. 6) was corroborated by calculations of renin-immunoreactive volumes from the 3D reconstructions (Fig. 7a). Those calculations revealed 6- and 4-fold difference increases of renin-immunoreactive volumes between high- and low-salt intake in AT1A −/− and AT1A −/−Cx40−/− mice, respectively (Fig. 7a). Renin mRNA levels mirrored the salt-dependent changes of renin-immunoreactive volumes in the two genotypes (Fig. 7b).
Representative immunohistochemical stainings of renin (green) and α-smooth muscle actin (α-SMA, red) in kidneys of AT1A −/− (a) and AT1A −/−Cx40−/− (b–d) mice kept on low-salt diet for 10 days. In AT1A −/− kidneys, there is a further increase of RSCs in the media layer of preglomerular vessels (arrows). In AT1A −/−Cx40−/− kidneys, there was also an increase of RSCs in the media layer of preglomerular vessels (arrows) and also an increase of ectopically located RSCs (arrowheads). Scale bar = 50 μm
Representative immunohistochemical stainings of renin (green) and α-smooth muscle actin (α-SMA, red) in kidneys of AT1A −/− (a) and AT1A −/−Cx40−/− (b) mice kept on high-salt diet for 10 days. In AT1A −/− kidneys, there is a reduction of RSCs in the media layer of preglomerular vessels (arrows) but no ectopic localization of RSCs. In AT1A −/−Cx40−/− kidneys, RSCs in the media layer almost disappeared and mainly ectopically located RSCs remained visible (arrowheads). Scale bar = 50 μm
3D reconstructions of renin-immunoreactive areas (dark gray) and α-smooth muscle actin (α-SMA, light gray) in kidneys of AT1A −/− (a, c) and AT1A −/−Cx40−/− (b, d) mice, kept on low- (a, b) and high- (c, d) salt diets, respectively. 3D reconstructions show interlobular arteries (ia), afferent arterioles (aa), glomeruli (G) and efferent arterioles (ea). The pictures indicate an increased number of RSCs along preglomrerular vessels in AT1A −/− mice on low-salt diet (a, arrows). Also in AT1A −/−Cx40−/− mice kept on low-salt diet, the number of RSCs in the walls of afferent arterioles increased (b, arrow). In AT1A −/− mice kept on high-salt diet, the number of RSCs in the walls of preglomerular vessels was clearly reduced (c). In AT1A −/−Cx40−/− mice on high-salt diet, RSCs were not found anymore along the vessel walls of afferent arterioles. Scale bar = 50 μm
a Renin-immunoreactive volume per glomerulus of AT1A −/− and AT1A −/−Cx40−/− mice under low- and high-salt intakes calculated from 3D reconstructions. Seven to ten glomeruli were analyzed from three kidneys per group. b Renin mRNA abundance in the kidneys of AT1A −/− (n = 6) and AT1A −/−Cx40−/− (n = 6) mice. c Systolic blood pressure of AT1A −/− and AT1A −/−Cx40−/− mice kept on low-salt or on high-salt diet (five animals per group). All values are mean ± SE. *P < 0.05 (ANOVA) between the low- and high-salt group
Again, it turned out that overall renin expression at any level during normal and low-salt intake was lower in kidneys of AT1A −/−Cx40−/− mice than in kidneys of AT1a −/− mice (Figs. 6 and 7a). The difference in renin mRNA between the two genotypes decreased with increasing salt intake (Fig. 7b).
Blood pressure in AT1A −/−Cx40−/− mice
Hypertension in Cx40-defective mice is hypothesized to be triggered by RAAS activity [12]. To estimate the contribution of ANGII-AT 1A receptor-mediated effects for hypertension in Cx40-deficient mice, we measured blood pressure in wt, Cx40−/−, AT1A −/−, and AT1A −/−Cx40−/− mice on standard chow (Fig. 3c). Mean systolic blood pressure of AT1A −/− mice on normal salt diet was on average 12 mmHg lower than in wild-type controls. The mean systolic blood pressure of AT1A −/−Cx40−/− mice on normal salt diet was on average 30 mmHg lower than that of Cx40−/− controls, but was still higher by 18 mmHg compared to AT1A −/− mice. In both genotypes, low-salt diet further reduced blood pressure by 20–30 mmHg, with pressure values remaining higher in AT1A −/−Cx40−/− compared to AT1A −/− mice (Fig. 7c). Conversely, switching salt diet from normal to high increased systolic blood pressure by about 10 mmHg in both genotypes. Again, blood pressure values in AT1A −/−Cx40−/− mice remained higher than those in AT1A −/− controls (Fig. 7c) during high-salt intake.
In vitro control of renin secretion from AT1A −/−Cx40−/− kidneys
The considerable amount of mural RSCs found in AT1A −/−Cx40−/− kidneys raised the question if those cells secrete renin in a pressure-controlled fashion unlike RSCs of Cx40−/− kidneys, in which the pressure control of renin secretion is blunted [29]. Measuring perfusion pressure-dependent secretion of renin from isolated kidneys revealed that the typical inverse relationship between renin secretion and perfusion pressure was maintained in AT1A −/− kidneys, but was completely absent in AT1A −/−Cx40−/− kidneys, alike in Cx40−/− kidneys (Fig. 8a). The pressure control of renin secretion involves calcium by a yet unknown mechanism. Calcium per se exerts an usual effect on renin secretion in the way that lowering of the calcium concentration strongly enhances renin secretion [4]. This special effect of low extracellular calcium on renin secretion was conserved in AT1A −/− kidneys, but was absent in AT1A −/−Cx40−/− kidneys similar to Cx40−/− kidneys (Fig. 8b) [30].
a Perfusion pressure-related renin secretion rates in isolated perfused kidneys of AT1A −/− and AT1A −/−Cx40−/− mice. Kidneys were perfused with pressures ranging from 40 to 140 mmHg in the presence of the β-adrenergic agonist isoproterenol (3nM). Renin secretion rates are normalized to those measured at 90 mmHg. Data are mean ± SE of five kidneys each. For comparison, also schematic curves for wild-type (wt) kidneys and Cx40−/− kidneys have been included in the figure. Those curves were adapted from previous publications [13, 20, 30]. b Effects of isoproterenol (3nM) and of reduction of the extracellular calcium concentration by adding the calcium chelator EGTA (3.1 mM) to the perfusate on renin secretion from the kidneys of AT1A −/− and AT1A −/−Cx40−/− mice. Kidneys were perfused at a constant pressure of 90 mmHg. Data are mean ± SE of five kidneys each. *P < 0.05 (ANOVA) between the indicated groups
Discussion
A main finding of the present study is that in the adult kidney RSCs can exist in the inner media layer of afferent arterioles in the absence of Cx40 and that SMCs of the afferent arteriole can transform reversibly into RSCs in the absence of Cx40. This finding is relevant since SMCs switch their connexin expression from Cx45 to Cx40 during metaplastic transformation into RSCs [13] and since RSCs have been observed to be ectopically located in the periglomerular interstitium if Cx40 function in RSCs is impaired [17, 19, 29]. Apparently, Cx40 in RSCs and their precursors are not essentially required for induction and maintenance of RSCs in the preglomerular vasculature. We speculate therefore that the disappearance of RSCs in the preglomerular vessels and their ectopic appearance in the renocortical interstitium as typically seen in adult mice with functional defects of Cx40 in RSCs are distinct processes. Since recruitment and existence of RSCs in the walls of preglomerular vessels are considered to be dependent on the intrarenal blood pressure [1, 6, 21], in the way that low pressure favors and high pressure suppresses mural renin expression, the long-lasting hypertension found in all animal models with defective Cx40 function may have prevented mural renin expression by short-term maneuvers of blood pressure lowering. In contrast to Cx40−/− mice, AT1A −/−Cx40−/− mice are normotensive that may allow mural renin expression. The functional consequence of the lower blood pressure in AT1A −/−Cx40−/− mice compared with hypertensive Cx40−/− mice is also reflected by prevention of cardiac hypertrophy seen in Cx40−/− mice (Table 1). Actually, renin expression and blood pressure in AT1A −/−Cx40−/− mice are salt sensitive alike in AT1A −/− mice [21] with the difference that blood pressure values are shifted to higher and renin expression to lower levels. The higher blood pressure values in AT1A −/−Cx40−/− mice therefore could explain the lower mural renin expression, which completely ceases when blood pressure values go beyond 140 mmHg.
Nonetheless, also in normotensive and in hypotensive AT1A −/−Cx40−/− mice, a substantial part of RSCs were located outside the preglomerular vessels as well known from Cx40-defective mice [17, 19, 29]. The appearance of RSCs in the interstitium is therefore unlikely to result from hypertension or chronically RAAS overactivation since biologic RAAS activity should be low in AT1A −/−Cx40−/− mice. Ectopic renin expression both in AT1A −/−Cx40−/− mice and in Cx40−/− mice shows a greater heterogeneity than the juxtaglomerular and vascular renin expression seen in wild-type or in AT1A −/− mice. It will be a task for future research to define the origin and the development of the cells that are located in the interstitium and that express renin if Cx40 is lacking in the cells. The localization of the ectopic RSCs would support the speculation that they derive from extraglomerular mesangial cells which strongly express Cx40 [15, 31] and which are susceptible for renin gene induction under stress conditions [26].
The second main finding of this study was that the pressure control of renin secretion from the kidneys is lacking if Cx40 is defective, irrespective of the intrarenal localization of RSCs. Thus, in AT1A −/−Cx40−/− kidneys, in which RSCs were located both within the vessel wall as well as in the periglomerular interstitium, the pressure control of renin secretion was completely absent as in Cx40−/− kidneys, whilst it was preserved in AT1A −/− kidneys. Apparently, Cx40 function in RSCs is essential for the control of secretion by the perfusion pressure. This conclusion is in accordance with the observation that the nonselective gap junction inhibitor 18αGA impairs pressure control of renin secretion [30] and that peptidic gap junction blockers acutely increase renin secretion from isolated perfused normal adult kidneys [27]. It is known that the pressure control of renin secretion depends on extracellular calcium, in the way that lowering of the extracellular calcium concentration typically stimulates renin secretion and at the same time blunts the pressure control [23]. In line, also the stimulatory effect of low extracellular calcium on renin secretion was blunted in AT1A −/−Cx40−/− kidneys as in Cx40−/− kidneys [30], whilst it was preserved in AT1A −/− kidneys. Altogether, it appears as if Cx40 is required for the physiological control of renin secretion, irrespective of the localization of the RSCs.
Loss of baroreceptor control of renin secretion is considered as a reason for the characteristic hypertension developing in mice with defective Cx40 function [29]. This conclusion is supported by the observation that hypertension is absent if both Cx40- and AT1A-receptors are lacking. On the other hand, introducing the Cx40 deletion into AT1A-deficient mice clearly increased blood pressure from hypo- to normotension. One may argue that this residual blood pressure-increasing effect may result from an incomplete inhibition of RAAS activity, eventually mediated by ANGII-AT1B receptors. However, also experiments with pharmacological RAAS blockers revealed that angiotensin I converting enzyme inhibitors reduced blood pressure in Cx40−/− mice to normotensive values but did not completely abolish the blood pressure difference between wild-types and Cx40-deficient mice [3, 11, 12, 30]. In line, transgenic reintroduction of Cx40 in RSCs of mice with a general Cx40 knockout attenuated but did not abolish hypertension [18]. We considered the possibility that aldosterone could contribute to the residual elevation of blood pressure. Our data in fact confirm that aldosterone is elevated in Cx40-deficient mice, but they also show that the increase of plasma aldosterone is absent in AT1A −/−Cx40−/− kidneys (Table 1). Therefore, the possibility has to be considered that apart from activation of the renin-angiotensin system also additional mechanisms contribute to hypertension in states of Cx40 deficiency. Since selective deletion of Cx40 in the endothelium has no influence on blood pressure [9], at least an endothelial contribution to hypertension in states of Cx40 deficiency appears less likely in this context. Similarly, changes of the renal expression pattern of other vascular connexins appear unlikely to explain the residual increase of blood pressure because we, like others [24], found no difference in Cx37, Cx43, and Cx45 expression levels in Cx40−/− and in AT1A −/−Cx40−/− kidneys.
References
Cantin M, Araujo-Nascimento MD, Benchimol S, Desormeaux Y (1977) Metaplasia of smooth muscle cells into juxtaglomerular cells in the juxtaglomerular apparatus, arteries, and arterioles of the ischemic (endocrine) kidney. An ultrastructural-cytochemical and autoradiographic study. Am J Pathol 87(3):581–602
Chomczynski P, Sacchi N (1987) Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem 162(1):156–159. doi:10.1006/abio.1987.9999
de Wit C, Roos F, Bolz SS, Pohl U (2003) Lack of vascular connexin 40 is associated with hypertension and irregular arteriolar vasomotion. Physiol Genomics 13(2):169–177. doi:10.1152/physiolgenomics.00169.2002
Fray JS (1977) Stimulation of renin release in perfused kidney by low calcium and high magnesium. Am J Physiol 232(4):F377–F382
Gerl M, Kurt B, Kurtz A, Wagner C (2014) Connexin 43 is not essential for the control of renin synthesis and secretion. Pflugers Arch 466(5):1003–1009. doi:10.1007/s00424-013-1349-2
Gomez RA, Chevalier RL, Everett AD, Elwood JP, Peach MJ, Lynch KR, Carey RM (1990) Recruitment of renin gene-expressing cells in adult rat kidneys. Am J Physiol 259(4 Pt 2):F660–F665
Hautmann M, Friis UG, Desch M, Todorov V, Castrop H, Segerer F, Otto C, Schutz G, Schweda F (2007) Pituitary adenylate cyclase-activating polypeptide stimulates renin secretion via activation of PAC1 receptors. J Am Soc Nephrol 18(4):1150–1156. doi:10.1681/ASN.2006060633
Ito M, Oliverio MI, Mannon PJ, Best CF, Maeda N, Smithies O, Coffman TM (1995) Regulation of blood pressure by the type 1A angiotensin II receptor gene. Proc Natl Acad Sci U S A 92(8):3521–3525
Jobs A, Schmidt K, Schmidt VJ, Lubkemeier I, van Veen TA, Kurtz A, Willecke K, de Wit C. Defective Cx40 maintains Cx37 expression but intact Cx40 is crucial for conducted dilations irrespective of hypertension. Hypertension 60(6):1422–1429. doi:10.1161/HYPERTENSIONAHA.112.201194
Kirchhoff S, Nelles E, Hagendorff A, Kruger O, Traub O, Willecke K (1998) Reduced cardiac conduction velocity and predisposition to arrhythmias in connexin40-deficient mice. Curr Biol 8(5):299–302
Krattinger N, Alonso F, Capponi A, Mazzolai L, Nicod P, Meda P, Haefliger JA (2009) Increased expression of renal cyclooxygenase-2 and neuronal nitric oxide synthase in hypertensive Cx40-deficient mice. J Vasc Res 46(3):188–198. doi:10.1159/000156704
Krattinger N, Capponi A, Mazzolai L, Aubert JF, Caille D, Nicod P, Waeber G, Meda P, Haefliger JA (2007) Connexin40 regulates renin production and blood pressure. Kidney Int 72(7):814–822. doi:10.1038/sj.ki.5002423
Kurt B, Kurtz L, Sequeira-Lopez ML, Gomez RA, Willecke K, Wagner C, Kurtz A (2011) Reciprocal expression of connexin 40 and 45 during phenotypical changes in renin-secreting cells. Am J Physiol Renal Physiol 300(3):F743–F748. doi:10.1152/ajprenal.00647.2010
Kurtz A (2011) Renin release: sites, mechanisms, and control. Annu Rev Physiol 73:377–399. doi:10.1146/annurev-physiol-012110-142238
Kurtz L, Janssen-Bienhold U, Kurtz A, Wagner C (2009) Connexin expression in renin-producing cells. J Am Soc Nephrol 20(3):506–512. doi:10.1681/ASN.2008030252
Kurtz L, Madsen K, Kurt B, Jensen BL, Walter S, Banas B, Wagner C, Kurtz A (2010) High-level connexin expression in the human juxtaglomerular apparatus. Nephron Physiol 116(1):p1–p8. doi:10.1159/000315658
Kurtz L, Schweda F, de Wit C, Kriz W, Witzgall R, Warth R, Sauter A, Kurtz A, Wagner C (2007) Lack of connexin 40 causes displacement of renin-producing cells from afferent arterioles to the extraglomerular mesangium. J Am Soc Nephrol 18(4):1103–1111. doi:10.1681/ASN.2006090953
Le Gal L, Alonso F, Wagner C, Germain S, Nardelli Haefliger D, Meda P, Haefliger JA. Restoration of connexin 40 (cx40) in Renin-producing cells reduces the hypertension of cx40 null mice. Hypertension 63(6):1198–1204. doi:10.1161/HYPERTENSIONAHA.113.02976
Lubkemeier I, Machura K, Kurtz L, Neubauer B, Dobrowolski R, Schweda F, Wagner C, Willecke K, Kurtz A (2011) The connexin 40 A96S mutation causes renin-dependent hypertension. J Am Soc Nephrol 22(6):1031–1040. doi:10.1681/ASN.2010101047
Machura K, Iankilevitch E, Neubauer B, Theuring F, Kurtz A (2013) The aldo-keto reductase AKR1B7 coexpresses with renin without influencing renin production and secretion. Am J Physiol Renal Physiol 304(5):F578–F584. doi:10.1152/ajprenal.00617.2012
Machura K, Neubauer B, Steppan D, Kettl R, Gross A, Kurtz A (2012) Role of blood pressure in mediating the influence of salt intake on renin expression in the kidney. Am J Physiol Renal Physiol 302(10):F1278–F1285. doi:10.1152/ajprenal.00688.2011
Oliverio MI, Madsen K, Best CF, Ito M, Maeda N, Smithies O, Coffman TM (1998) Renal growth and development in mice lacking AT1A receptors for angiotensin II. Am J Physiol 274(1 Pt 2):F43–F50
Scholz H, Hamann M, Gotz KH, Kurtz A (1994) Role of calcium ions in the pressure control of renin secretion from the kidneys. Pflugers Arch 428(2):173–178
Schweda F, Kurtz L, de Wit C, Janssen-Bienhold U, Kurtz A, Wagner C (2009) Substitution of connexin40 with connexin45 prevents hyperreninemia and attenuates hypertension. Kidney Int 75(5):482–489. doi:10.1038/ki.2008.637
Schweda F, Wagner C, Kramer BK, Schnermann J, Kurtz A (2003) Preserved macula densa-dependent renin secretion in A1 adenosine receptor knockout mice. Am J Physiol Renal Physiol 284(4):F770–F777. doi:10.1152/ajprenal.00280.2002
Sequeira Lopez ML, Pentz ES, Nomasa T, Smithies O, Gomez RA (2004) Renin cells are precursors for multiple cell types that switch to the renin phenotype when homeostasis is threatened. Dev Cell 6(5):719–728
Shiraishi M, Aramaki Y, Seto M, Imoto H, Nishikawa Y, Kanzaki N, Okamoto M, Sawada H, Nishimura O, Baba M, Fujino M (2000) Discovery of novel, potent, and selective small-molecule CCR5 antagonists as anti-HIV-1 agents: synthesis and biological evaluation of anilide derivatives with a quaternary ammonium moiety. J Med Chem 43(10):2049–2063
Wagner C (2008) Function of connexins in the renal circulation. Kidney Int 73(5):547–555. doi:10.1038/sj.ki.5002720
Wagner C, Jobs A, Schweda F, Kurtz L, Kurt B, Lopez ML, Gomez RA, van Veen TA, de Wit C, Kurtz A (2010) Selective deletion of Connexin 40 in renin-producing cells impairs renal baroreceptor function and is associated with arterial hypertension. Kidney Int 78(8):762–768. doi:10.1038/ki.2010.257
Wagner C, de Wit C, Kurtz L, Grunberger C, Kurtz A, Schweda F (2007) Connexin 40 is essential for the pressure control of renin synthesis and secretion. Circ Res 100(4):556–563. doi:10.1161/01.RES.0000258856.19922.45
Zhang J, Hill CE (2005) Differential connexin expression in preglomerular and postglomerular vasculature: accentuation during diabetes. Kidney Int 68(3):1171–1185. doi:10.1111/j.1523-1755.2005.00509.x
Acknowledgments
This work was financially supported by the German Research Foundation/Collaborative Research Center SFB 699 and by the German Research Foundation/Grant WA-2137/2-2. The excellent technical assistance provided by Gerda Treuner, Marcela Loza Hilares, Robert Götz, and Anna M’Bangui is gratefully acknowledged. We also thank K. Willecke (Institute for Genetics, University of Bonn, Germany) for providing the Cx40-deficient mouse and T.M. Coffman (Duke University, Durham, North Carolina, USA) for the AT1A-deficient mouse.
Conflict of interest
The authors declared no competing interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Machura, K., Neubauer, B., Müller, H. et al. Connexin 40 is dispensable for vascular renin cell recruitment but is indispensable for vascular baroreceptor control of renin secretion. Pflugers Arch - Eur J Physiol 467, 1825–1834 (2015). https://doi.org/10.1007/s00424-014-1615-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-014-1615-y