Abstract
Renin synthesis and renin secretion at the level of renal juxtaglomerular cells are regulated by neurotransmitters, hormones, paracrine, and mechanical signals. Although morphological evidence has indicated an intense intercellular communication of renin cells via connexins between the cells composing the juxtaglomerlar area, the functional behavior of renin-secreting cells has been considered of that of individual isolated cells for a long time. Findings obtained during recent years shed first light on the functional relevance of connexins for the control of renin secretion and also for the positioning of renin-secreting cells in the kidney. This short review aims to summarize these findings and tries to set them into a functional context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
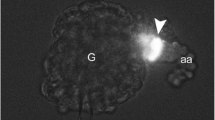
Almost five decades ago, electron microscopical investigations have revealed that intraglomerular cells, extraglomerular mesangial (lacis) cells, renin-producing cells, and cells of the preglomerular vasculature in the kidney are interconnected by a high density of gap junctions [58] (Fig. 1). Gap junctions are composed of connexin proteins which define the biophysical properties of the gap junctions [22]. The human genome encodes for 21 and the mouse genome for 20 different connexin proteins, which show a high degree of interspecies homology [46]. Sexamers of connexins build a channel-like structure termed connexon or hemichannel, which is inserted into the plasma membrane. Connexons of two neighboring cells can dock and thus form a large intercellular channel that allows charge- and size-controlled permeation of larger molecules up to a molecular mass of 1 kDa, depending on the connexin subtype. An emerging discussion has started about the possible function of hemichannels, i.e., connexons that do not form gap junctions but instead enable the release of intracellular signaling molecules into the extracellular space [13, 67]. The functional meaning and relevance of this striking regional accumulation of gap junctions in the (juxta)glomerular areas of the kidney remained unknown for long.
Distribution of gap junctions (cylinders) and connexins in the juxtaglomerular area. Vascular smooth muscle cells and endothelial cells of afferent arterioles are colored in red and yellow, respectively. Granule containing renin-secreting cells are indicated in light green. IGM and EGM indicate intraglomerular and extraglomerular mesangial cells, respectively. Gap junctions connecting the endothelial, vascular smooth muscle cells, and intraglomerular and extraglomerular mesangial cells are illustrated by black cylinders, the coupling of renin-secreting cells is shown by red cylinders
Intrarenal distribution of gap junctions and connexins
The development of specific antibodies against the different connexin proteins has allowed to analyze the gap junction types in the (juxta)glomerular area in more detail. Four different connexin proteins appear to be expressed in the (juxta)glomerular area (Fig. 1). Several groups of investigators agreed upon that connexin 40 is the most abundant connexin protein in this particular area. It is expressed by intra- and extraglomerular mesangial cells (black cylinders, Fig. 1), by renin-secreting juxtaglomerular cells (red cylinders) and by endothelial cells of the preglomerular vasculature including afferent arterioles (black cylinders) [17, 19, 25, 63, 64, 68]. Electron microscopical immunolocalization studies have confirmed that Cx40 contributes to gap junction formation between mesangial cells, between renin-secreting cells, between endothelial cells, and between endothelial and renin-secreting cells [17].
Apart from Cx40, also connexin 37 is found in the (juxta)glomerular area. It is clearly expressed by endothelial cells and to a certain extent also by renin-secreting cells (Fig. 1). Connexin 43 is expressed by endothelial cells, but probably not or only at a low level in renin-secreting cells or mesangial cells (Fig. 1) [20, 53, 63]. Finally, connexin 45 is clearly expressed by preglomerular smooth muscle cells (Fig. 1). Conflicting data exist about the expression of Cx45 in renin-secreting cells and mesangial cells (Fig. 1) While immunolocalization studies did not provide positive results for an extravascular localization of Cx45 [35], studies with Cx45fl/Nestin Cre transgenic mice (eGFP) suggest an expression of Cx45 in renin-secreting and in mesangial cells [21].
Functional relevance of connexin 40
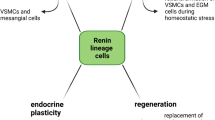
Having defined the connexin composition of the gap junctions in the (juxta)glomerular area (Fig. 1), it was possible to address their potential function in genetically engineered mice. It was found that mice with a global deletion of Cx40 are severely hypertensive [12]. Further analyses revealed that these mice also had high levels of circulating renin [28, 37, 64]. Since the hypertension in Cx40-deficient mice can be corrected by inhibitors of the renin–angiotensin system such as by ACE inhibitors or by angiotensin II-AT1 receptor blockers [12, 50, 64], it is reasonable to assume that hyperreninemia in mice is the cause for hypertension. Normally, renin secretion into the circulation is controlled by the blood pressure in the sense of a negative feedback that allows to activate the renin–angiotensin system in states of subnormal blood pressure and to put a brake on the activation of the system in states of high blood pressure to avoid aggravation of hypertension [8] (Fig. 2).
Perfusion pressure dependency of renin secretion from isolated perfused mouse kidneys from wild-type mice (black curve) and Cx40-deficient (Cx40KO) (red curve) kidneys. The green curve gives data of wild-type kidneys perfused with a solution containing calcium in the micromolar range. Secretion data are normalized to the value obtained with wild-type kidneys at the standard perfusion pressure (90 mmHg)
The control of renin secretion by blood pressure is mediated indirectly by the activity of sympathetic outflow [8] to the kidney and, more directly, at the level of the kidney by the “renal baroreceptor” mechanism [8]. Baroreceptor control of renin release is the typical inverse dependency of renin secretion on perfusion pressure [9]. The functionality of this important local control mechanism is not well understood so far. One may even debate if sensing of pressure changes really occurs in the vascular wall or if effects of pressure on glomerular filtration and therefore on the tubular chloride concentration at the macula densa represent the work mode of the baroreceptor mechanism. However, the characteristic inverse dependency of renin release on perfusion pressure is conserved in nonfiltering kidneys and in kidneys with blocked macula densa salt transport indicating the existence of an independent pressure control. It turned out that the renal baroreceptor mechanism controlling renin secretion was fundamentally altered in kidneys lacking Cx40. The characteristic inverse relationship between renin secretion and renal perfusion pressure was shifted to a linear positive relationship between the two parameters [64, 65] (Fig. 2).
Experiments with unilateral renal artery stenosis performed to test for the renal baroreceptor function in vivo also indicated a markedly reduced sensitivity of renin secretion towards changes of renal perfusion pressure in Cx40-deficient mice [28, 64]. Since Cx40 gap junctions are formed between preglomerular endothelial cells, between endothelial cells and renin-secreting cells, between renin-secreting cells themselves, and between renin-secreting cells and neighboring mesangial cells, cell-specific Cx40 deletions were performed to identify those Cx40 gap junctions that are relevant for the baroreceptor control of renin secretion. It turned out that deletion of Cx40 from preglomerular endothelial cells had no effect on renin secretion nor on blood pressure [65], suggesting that Cx40 gap junctions between endothelial cell and between endothelial cells and renin-secreting cells are less important for the baroreceptor function. Conversely, deletion of Cx40 from renin-secreting cells mimicked the renin phenotype of the global Cx40 knockout [65], suggesting that Cx40 gap junctions between renin-secreting cells and potentially between renin-secreting cells and mesangial cells are fundamental for a normal baroreceptor control of renin secretion. Although it is still a matter of debate, there is increasing acceptance of the concept that connexons that are not linked to connexons of neighboring cells to form functional gap junctions might also gain function as so called hemichannels that allow the release of chemical signaling molecules which act in a paracrine manner [47, 54, 60]. The most promising candidate for such a signaling molecule is ATP that induces calcium mobilization in neighboring cells via binding to purinergic cell surface receptors [52]. In fact, it has been already hypothesized that connexin hemichannels could be important for calcium spreading between preglomerular endothelial cells [60] and between extraglomerular mesangial cells in the context of tubuloglomerular feedback signaling between the macula densa cells and the smooth muscle cells of the afferent arteriole [20, 44, 53].
At present, there is no direct proof of either mechanism, namely Cx40 gap junctional coupling or Cx40 hemichannel function for the pressure control of renin secretion, except that Cx40 in renin-secreting cells is fundamental for this mechanism. Since membrane-inserted Cx40 can also gain scaffold function as indicated by its association with eNOS in endothelial cells [1], it is in principle also possible that the renin phenotype induced by deletion of Cx40 from renin-secreting cells is not due to the loss of Cx40 channel function at all but rather to the disorganization of membrane protein complexes involving Cx40. It was of importance therefore to see that connexin 40 proteins carrying a single amino acid substitution [42], which produces a 90 % reduction of Cx40 gap junction permeability, are normally inserted in the membranes of (juxta)glomerular cells, but produce a very similar renin phenotype as does the deletion of Cx40 protein from renin-secreting cells [42].
To identify possible signals that pass Cx40 gap junctions/hemichannels in renin cells in the context of the baroreceptor mechanism, it was investigated to what extent the function of Cx40 in renin-secreting cells can be compensated by connexin 45 which is typically found in preglomerular smooth muscle cells [21, 29, 35]. The permeability of Cx45 gap junctions/hemichannels differs from that of Cx40 with regard to charge and size. Compared to Cx40 channels, Cx45 channels have a low electrical conductivity (20–40 vs 200 pS) [7, 62] and are less sensitive to transjunctional potentials [5, 6, 23, 43]. Moreover, cAMP strongly increases the conductance and permeability of Cx40 channels [50], but reduces the conductance of Cx45 gap junctions [62]. Replacement of Cx40 by Cx45 (Cx40koCx45ki mice) ameliorates the renin phenotype of Cx40-deficient mice but does not rescue it [50]. Cx40koCx45ki mice are moderately hypertensive and have an altered relationship between renal perfusion pressure and renin secretion similar to Cx40-deficient mice (Fig. 2) [50]. Although the signal relevant for the baroreceptor mechanism passing Cx40 gap junctions/hemichannels has not yet been identified, a board of evidence meanwhile suggests that calcium is a relevant signal. As outlined elsewhere in this “special issue” (doi:10.1007/s00424-012-1107-x), calcium is a strong inhibitory signal for renin secretion. Similar to the myogenic mechanism in vascular smooth muscle cells [3], the cytosolic calcium concentration in renin-secreting cells rises with increasing renal perfusion pressure [38, 49, 51] due to enhanced transmembrane calcium influx [32, 67]. In line, by lowering the concentration of calcium in the extracellular fluid, the inverse relationship between renal perfusion pressure and renin secretion converts into a relationship that was even positively related to perfusion pressure [15, 49] (Fig. 2). The change of the relationship between perfusion pressure and renin secretion induced by lowering of the extracellular calcium concentration is therefore very similar to that produced by deletion of Cx40 [64]. Lowering of the extracellular concentration of calcium not only abrogates the baroreceptor mechanism, but per se also leads to a marked stimulation of renin secretion which is in accordance with the powerful inhibitory action of calcium on renin secretion [26, 33, 61]. This typical and prominent stimulation of renin secretion by lowering of the extracellular concentration of calcium (Fig. 2) is absent or strongly attenuated in kidneys, in which Cx40 is absent, nonfunctional, or replaced by Cx45, i.e., under all conditions, in which the renal baroreceptor mechanism is nonfunctional [50, 64]. An obvious hypothesis combining all of these results is that Cx40 is fundamental for the spreading of calcium among renin-secreting cells. In fact, calcium spreading via gap junction has already been demonstrated to be of importance for coordinated secretion from endocrine cells, such as insulin secreting β cells [45].
Even more speculative, Cx40 hemichannels in renin-secreting cells could serve as mechanosensors, which mediate pressure- or stretch-dependent calcium influx into renin-secreting cells. Alternatively, mechanosensitive ATP release is conceivable [39]. While mechanosensivity of certain connexin hemichannels has already been demonstrated [41], it is unknown if Cx40 hemichannels are mechanosensitive at all.
The results of pharmacological experiments would support the concept that the gap junction rather than a hemichannel function of Cx40 is relevant for the baroreceptor mechanism controlling renin secretion. Thus, the nonselective gap junction blocker 18α-GA (glycyrrhetinic acid) abrogates pressure regulation of renin secretion in a similar fashion as deletion of Cx40 does [64]. In addition, peptides considered to block Cx40 gap junctions stimulate renin secretion from the kidneys [10, 56], compatible with the idea that Cx40 gap junctions mediate an inhibitory (calcium-dependent) effect on renin secretion. In diabetes, renal connexins exhibit an abnormal expression to that effect that Cx40 is also found in the smooth muscle cells and Cx43 is markedly expressed in renin-producing cells, whereas its expression in the endothelium of the efferent arteriole disappears [68]. Interestingly, peptides considered to block Cx37 and Cx40 fail to elicit stimulatory effects on renin secretion in diabetes [57]. Thus, it is likely that this diabetes-induced modified intercellular communication markedly impairs signal transduction through the juxtaglomerular apparatus.
The findings mentioned above aimed to explain a function of Cx40 for the pressure control of renin secretion from cells that are typically located in the tunica media of afferent arterioles at juxtaglomerular position. The embryonic deletion of Cx40 from renin-secreting cells causes an additional effect that might also be relevant for understanding the abnormalities of the renal baroreceptor mechanism in conjunction with defective Cx40 function. Development of renin-producing cells follows the development of the preglomerular arteriolar tree in Cx40-deficient mice [37] and wild-type mice alike [48]. A marked difference between these mouse strains becomes apparent at a developmental stage when renin expression reaches the terminal parts of afferent arterioles. In kidneys in which Cx40 is absent, nonfunctional or replaced by Cx45, renin-expressing cells become ectopically located outside the tunica media of afferent arterioles [37, 50]. Renin cells are found in the periglomerular interstitium, in the glomerular tuft, and in cells covering the Bowman capsule from outside [37, 42, 65]. The number of renin-expressing cells appearing in this ectopic position increases with increasing age of the mice. In parallel, circulating renin concentrations increase, while the defective baroreceptor control of renin secretion is apparent already in young animals. Experimental maneuvers applied to stimulate chronically renin secretion such as severe salt depletion cause a strong increase of the number of ectopic renin expressing also in young mice [34].
It will be of importance for future experiments to investigate if the striking abnormalities in the control of renin secretion and localization of renin expression cells are related to an embryonic Cx40 defect or can be induced also in the adult normally differentiated kidney. The findings described so far were obtained in mice and rats. Immunohistochemistry has revealed that the connexin distribution pattern in the human kidney and in particular in renin-secreting cell is very similar to that of mouse kidneys [36], suggesting comparable modes of gap junctional coupling. Furthermore, the loss of function mutation of Cx40, that leads to hyperreninemia and hypertension in mice, has originally been discovered in a hypertensive man suffering from atrial fibrillation [16]. Since the basic principles of the regulation of renin synthesis and renin secretion between men and rodents appear to be rather concordant, it is not unlikely that Cx40 fulfils a similarly important role in the control of renin secretion in humans as in mice.
Functional relevance of other connexins
Apart from Cx40, also Cx37 is expressed in the juxtaglomerular area, mainly in preglomerular endothelial cells but to some extent also in renin-secreting cells [2, 31, 35]. Mice lacking Cx37 globally have a normal renin system with regard to the regulation of renin secretion and localization of renin-expressing cells [66]. As a consequence, also blood pressure is normal in these animals [14]. These findings would suggest that neither homologous nor heterologous Cx37 containing gap junctions nor Cx37 hemichannels appear to be of major functional relevance for the control of renin secretion. A study with acute application of a putative blocking peptide of Cx37 gap junctions reported a moderate stimulation of renin secretion from isolated rat kidneys [55, 56]. In this experimental setting, the Cx37 blocking peptide also led to marked renal vasoconstriction [55, 56], which might have caused the increase of renin secretion by indirect pathways, such as a fall of perfusion pressure in the juxtaglomerular area.
A potential role of Cx43 for the control of renin secretion was originally assessed in mice, in which Cx43 was globally substituted by Cx32 [18], which is normally not expressed in the juxtaglomerular area [2, 4, 17, 28, 68]. It was found that these mice had lower circulating levels of renin, and more strikingly, they did not increase renin expression and renin secretion in response to unilateral renal artery stenosis [18]. As a consequence, the typical “Goldblatt” hypertension did not develop in these mice, suggesting that Cx43 is highly relevant for the baroreceptor mechanisms controlling renin secretion. Since global Cx43 deletion is embryonically lethal [11, 40, 59], we generated mice with renin cell-specific deletion of Cx43 (renin-Cre Cx43fl/fl mice). These mice were normal with regard to the regulation of renin secretion, renin cells, and blood pressure regulation (Wagner et al. unpublished results), what would be in accordance with a minor or even lacking Cx43 expression in renin-secreting cells [2, 24]. The effect of replacement of Cx43 by Cx32 on renin secretion is therefore probably related to a more indirect effect on renin-secreting cells that might be mediated by endothelial cells, which express Cx43 [17, 19, 25, 68]. In line with this idea, it has been demonstrated that endothelial prostacyclin formation is fundamental for the stimulation of renin secretion by unilateral renal artery stenosis [27]. It is a tempting speculation therefore that endothelial Cx43 could be relevant for the regulation of prostacyclin formation.
Finally, a possible role of connexin 45 for the function of renin-secreting cells should be considered. While there is agreement that Cx45 is expressed by smooth muscle cells of the preglomerular vasculature, controverse data exist about the expression of Cx45 in renin-secreting cells [20, 30, 35, 36, 53]. Immunolocalization studies [50] and staining of LacZ driven by the Cx45 promoter [29] have not provided evidence for an expression of Cx45 in renin-expressing cells. Conversely, it appeared as if the expressions of renin and of Cx45 are mutually exclusive [30]. A study using a more indirect approach, namely the analysis of mice harboring Cre recombinase under the control of nestin [21] promoter and harboring floxed Cx45 alleles that induce GFP expression after recombination, suggested the expression of Cx45 in renin-expressing cells [21]. These mice also showed moderate elevations of plasma renin concentrations and blood pressure, suggesting that Cx45 might play a similar role for the function of renin-secreting cells as Cx40. A study with renin cell-specific deletion of Cx45, however, revealed no abnormalities in the regulation of renin secretion and blood pressure [30]. The difference of findings between the two studies still awaits explanation. One possibility could be that Cre recombinase driven by the nestin promoter acts more globally than renin promoter-driven Cre and could therefore induce indirect effects on renin-secreting cells.
Summary and perspectives
Almost 50 years after their first discovery, a number of functions can now be attributed to the strong gap junction coupling between cells in the juxtaglomerular area, in particular in renin-secreting cells. Renin-secreting cells mainly form gap junctions or possibly hemichannels composed of connexin 40. Connexin 40 likely is important for the calcium spreading in and between renin-secreting cells and by that it plays a fundamental role for the renal baroreceptor mechanism that links renin secretion to the renal perfusion pressure. Defective Cx40 function interrupts the baroreceptor mechanism and renin secretion runs out of physiological negative feedback control leading to hyperreninemia and hypertension.
Future experiments will have to define the interaction of calcium and connexin 40 in the control of renin secretion in more detail. Moreover, it will be of interest to see which changes of the renin system in Cx40-defective kidneys are developmentally defined and which ones can be induced later in the otherwise normally differentiated kidney.
References
Alonso F, Boittin FX, Beny JL, Haefliger JA (2010) Loss of connexin40 is associated with decreased endothelium-dependent relaxations and eNOS levels in the mouse aorta. Am J Physiol Heart Circ Physiol 299:H1365–1373
Arensbak B, Mikkelsen HB, Gustafsson F, Christensen T, Holstein-Rathlou NH (2001) Expression of connexin 37, 40, and 43 mRNA and protein in renal preglomerular arterioles. Histochem Cell Biol 115:479–487
Baek EB, Kim SJ (2011) Mechanisms of myogenic response: Ca(2+)-dependent and -independent signaling. J Smooth Muscle Res 47:55–65
Barajas L, Liu L, Tucker M (1994) Localization of connexin43 in rat kidney. Kidney Int 46:621–626
Barrio LC, Capel J, Jarillo JA, Castro C, Revilla A (1997) Species-specific voltage-gating properties of connexin-45 junctions expressed in Xenopus oocytes. Biophys J 73:757–769
Beblo DA, Wang HZ, Beyer EC, Westphale EM, Veenstra RD (1995) Unique conductance, gating, and selective permeability properties of gap junction channels formed by connexin40. Circ Res 77:813–822
Bukauskas FF, Elfgang C, Willecke K, Weingart R (1995) Biophysical properties of gap junction channels formed by mouse connexin40 in induced pairs of transfected human HeLa cells. Biophys J 68:2289–2298
Castrop H, Hocherl K, Kurtz A, Schweda F, Todorov V, Wagner C (2010) Physiology of kidney renin. Physiol Rev 90:607–673
Davis JO, Freeman RH (1976) Mechanisms regulating renin release. Physiol Rev 56:1–56
De Vriese AS, Van de Voorde J, Lameire NH (2002) Effects of connexin-mimetic peptides on nitric oxide synthase- and cyclooxygenase-independent renal vasodilation. Kidney Int 61:177–185
de Wit C, Roos F, Bolz SS, Kirchhoff S, Kruger O, Willecke K, Pohl U (2000) Impaired conduction of vasodilation along arterioles in connexin40-deficient mice. Circ Res 86:649–655
de Wit C, Roos F, Bolz SS, Pohl U (2003) Lack of vascular connexin 40 is associated with hypertension and irregular arteriolar vasomotion. Physiol Genomics 13:169–177
Evans WH, De Vuyst E, Leybaert L (2006) The gap junction cellular internet: connexin hemichannels enter the signalling limelight. Biochem J 397:1–14
Figueroa XF, Duling BR (2008) Dissection of two Cx37-independent conducted vasodilator mechanisms by deletion of Cx40: electrotonic versus regenerative conduction. Am J Physiol Heart Circ Physiol 295:H2001–2007
Fray JC, Park CS (1986) Forskolin and calcium: interactions in the control of renin secretion and perfusate flow in the isolated rat kidney. J Physiol 375:361–375
Gollob MH (2006) Cardiac connexins as candidate genes for idiopathic atrial fibrillation. Curr Opin Cardiol 21:155–158
Haefliger JA, Demotz S, Braissant O, Suter E, Waeber B, Nicod P, Meda P (2001) Connexins 40 and 43 are differentially regulated within the kidneys of rats with renovascular hypertension. Kidney Int 60:190–201
Haefliger JA, Krattinger N, Martin D, Pedrazzini T, Capponi A, Doring B, Plum A, Charollais A, Willecke K, Meda P (2006) Connexin43-dependent mechanism modulates renin secretion and hypertension. J Clin Invest 116:405–413
Haefliger JA, Nicod P, Meda P (2004) Contribution of connexins to the function of the vascular wall. Cardiovasc Res 62:345–356
Hanner F, Sorensen CM, Holstein-Rathlou NH, Peti-Peterdi J (2010) Connexins and the kidney. Am J Physiol Regul Integr Comp Physiol 298:R1143–1155
Hanner F, von Maltzahn J, Maxeiner S, Toma I, Sipos A, Kruger O, Willecke K, Peti-Peterdi J (2008) Connexin45 is expressed in the juxtaglomerular apparatus and is involved in the regulation of renin secretion and blood pressure. Am J Physiol Regul Integr Comp Physiol 295:R371–380
Harris AL (2001) Emerging issues of connexin channels: biophysics fills the gap. Q Rev Biophys 34:325–472
Hellmann P, Winterhager E, Spray DC (1996) Properties of connexin40 gap junction channels endogenously expressed and exogenously overexpressed in human choriocarcinoma cell lines. Pflugers Arch 432:501–509
Hillis GS, Duthie LA, Mlynski R, McKay NG, Mistry S, MacLeod AM, Simpson JG, Haites NE (1997) The expression of connexin 43 in human kidney and cultured renal cells. Nephron 75:458–463
Hwan Seul K, Beyer EC (2000) Heterogeneous localization of connexin40 in the renal vasculature. Microvasc Res 59:140–148
Ichihara A, Suzuki H, Murakami M, Naitoh M, Matsumoto A, Saruta T (1995) Interactions between angiotensin II and norepinephrine on renin release by juxtaglomerular cells. Eur J Endocrinol 133:569–577
Imanishi M, Tsuji T, Nakamura S, Takamiya M (2001) Prostaglandin I(2)/E(2) ratios in unilateral renovascular hypertension of different severities. Hypertension 38:23–29
Krattinger N, Capponi A, Mazzolai L, Aubert JF, Caille D, Nicod P, Waeber G, Meda P, Haefliger JA (2007) Connexin40 regulates renin production and blood pressure. Kidney Int 72:814–822
Kruger O, Plum A, Kim JS, Winterhager E, Maxeiner S, Hallas G, Kirchhoff S, Traub O, Lamers WH, Willecke K (2000) Defective vascular development in connexin 45-deficient mice. Development 127:4179–4193
Kurt B, Kurtz L, Sequeira-Lopez ML, Gomez RA, Willecke K, Wagner C, Kurtz A (2011) Reciprocal expression of connexin 40 and 45 during phenotypical changes in renin-secreting cells. Am J Physiol Renal Physiol 300:F743–748
Kurtz A (2012) Renal connexins and blood pressure. Biochim Biophys Acta 1818(8):1903–1908
Kurtz A, Penner R (1989) Angiotensin II induces oscillations of intracellular calcium and blocks anomalous inward rectifying potassium current in mouse renal juxtaglomerular cells. Proc Natl Acad Sci U S A 86:3423–3427
Kurtz A, Pfeilschifter J, Hutter A, Buhrle C, Nobiling R, Taugner R, Hackenthal E, Bauer C (1986) Role of protein kinase C in inhibition of renin release caused by vasoconstrictors. Am J Physiol 250:C563–571
Kurtz L, Gerl M, Kriz W, Wagner C, Kurtz A (2009) Replacement of connexin 40 by connexin 45 causes ectopic localization of renin-producing cells in the kidney but maintains in vivo control of renin gene expression. Am J Physiol Renal Physiol 297:F403–409
Kurtz L, Janssen-Bienhold U, Kurtz A, Wagner C (2009) Connexin expression in renin-producing cells. J Am Soc Nephrol 20:506–512
Kurtz L, Madsen K, Kurt B, Jensen BL, Walter S, Banas B, Wagner C, and Kurtz A. High-level connexin expression in the human juxtaglomerular apparatus. Nephron Physiol 116: p1-8
Kurtz L, Schweda F, de Wit C, Kriz W, Witzgall R, Warth R, Sauter A, Kurtz A, Wagner C (2007) Lack of connexin 40 causes displacement of renin-producing cells from afferent arterioles to the extraglomerular mesangium. J Am Soc Nephrol 18:1103–1111
Lai EY, Wang Y, Persson AE, Manning RD Jr, Liu R (2011) Pressure induces intracellular calcium changes in juxtaglomerular cells in perfused afferent arterioles. Hypertens Res 34:942–948
Li A, Banerjee J, Leung CT, Peterson-Yantorno K, Stamer WD, Civan MM (2011) Mechanisms of ATP release, the enabling step in purinergic dynamics. Cell Physiol Biochem 28:1135–1144
Liao Y, Day KH, Damon DN, Duling BR (2001) Endothelial cell-specific knockout of connexin 43 causes hypotension and bradycardia in mice. Proc Natl Acad Sci U S A 98:9989–9994
Liu F, Arce FT, Ramachandran S, Lal R (2006) Nanomechanics of hemichannel conformations: connexin flexibility underlying channel opening and closing. J Biol Chem 281:23207–23217
Lubkemeier I, Machura K, Kurtz L, Neubauer B, Dobrowolski R, Schweda F, Wagner C, Willecke K, Kurtz A (2011) The connexin 40 A96S mutation causes renin-dependent hypertension. J Am Soc Nephrol 22:1031–1040
Moreno AP, Laing JG, Beyer EC, Spray DC (1995) Properties of gap junction channels formed of connexin 45 endogenously expressed in human hepatoma (SKHep1) cells. Am J Physiol 268:C356–365
Peti-Peterdi J (2006) Calcium wave of tubuloglomerular feedback. Am J Physiol Renal Physiol 291:F473–480
Ravier MA, Guldenagel M, Charollais A, Gjinovci A, Caille D, Sohl G, Wollheim CB, Willecke K, Henquin JC, Meda P (2005) Loss of connexin36 channels alters beta-cell coupling, islet synchronization of glucose-induced Ca2+ and insulin oscillations, and basal insulin release. Diabetes 54:1798–1807
Saez JC, Berthoud VM, Branes MC, Martinez AD, Beyer EC (2003) Plasma membrane channels formed by connexins: their regulation and functions. Physiol Rev 83:1359–1400
Saez JC, Connor JA, Spray DC, Bennett MV (1989) Hepatocyte gap junctions are permeable to the second messenger, inositol 1,4,5-trisphosphate, and to calcium ions. Proc Natl Acad Sci U S A 86:2708–2712
Sauter A, Machura K, Neubauer B, Kurtz A, Wagner C (2008) Development of renin expression in the mouse kidney. Kidney Int 73:43–51
Scholz H, Hamann M, Gotz KH, Kurtz A (1994) Role of calcium ions in the pressure control of renin secretion from the kidneys. Pflugers Arch 428:173–178
Schweda F, Kurtz L, de Wit C, Janssen-Bienhold U, Kurtz A, Wagner C (2009) Substitution of connexin40 with connexin45 prevents hyperreninemia and attenuates hypertension. Kidney Int 75:482–489
Schweda F, Riegger GA, Kurtz A, Kramer BK (2000) Store-operated calcium influx inhibits renin secretion. Am J Physiol Renal Physiol 279:F170–176
Sipos A, Vargas SL, Toma I, Hanner F, Willecke K, Peti-Peterdi J (2009) Connexin 30 deficiency impairs renal tubular ATP release and pressure natriuresis. J Am Soc Nephrol 20:1724–1732
Sorensen CM, and Holstein-Rathlou NH. Cell–cell communication in the kidney microcirculation. Microcirculation 2012
Spray DC, Stern JH, Harris AL, Bennett MV (1982) Gap junctional conductance: comparison of sensitivities to H and Ca ions. Proc Natl Acad Sci U S A 79:441–445
Takenaka T, Inoue T, Kanno Y, Okada H, Hill CE, Suzuki H (2008) Connexins 37 and 40 transduce purinergic signals mediating renal autoregulation. Am J Physiol Regul Integr Comp Physiol 294:R1–11
Takenaka T, Inoue T, Kanno Y, Okada H, Meaney KR, Hill CE, Suzuki H (2008) Expression and role of connexins in the rat renal vasculature. Kidney Int 73:415–422
Takenaka T, Inoue T, Okada H, Ohno Y, Miyazaki T, Chaston DJ, Hill CE, Suzuki H (2011) Altered gap junctional communication and renal haemodynamics in Zucker fatty rat model of type 2 diabetes. Diabetologia 54:2192–2201
Taugner R, Schiller A, Kaissling B, Kriz W (1978) Gap junctional coupling between the JGA and the glomerular tuft. Cell Tissue Res 186:279–285
Theis M, de Wit C, Schlaeger TM, Eckardt D, Kruger O, Doring B, Risau W, Deutsch U, Pohl U, Willecke K (2001) Endothelium-specific replacement of the connexin43 coding region by a lacZ reporter gene. Genesis 29:1–13
Toma I, Bansal E, Meer EJ, Kang JJ, Vargas SL, Peti-Peterdi J (2008) Connexin 40 and ATP-dependent intercellular calcium wave in renal glomerular endothelial cells. Am J Physiol Regul Integr Comp Physiol 294:R1769–1776
Van Dongen R, Peart WS (1974) Calcium dependence of the inhibitory effect of angiotensin on renin secretion in the isolated perfused kidney of the rat. Br J Pharmacol 50:125–129
van Veen TA, van Rijen HV, Jongsma HJ (2000) Electrical conductance of mouse connexin45 gap junction channels is modulated by phosphorylation. Cardiovasc Res 46:496–510
Wagner C (2008) Function of connexins in the renal circulation. Kidney Int 73:547–555
Wagner C, de Wit C, Kurtz L, Grunberger C, Kurtz A, Schweda F (2007) Connexin40 is essential for the pressure control of renin synthesis and secretion. Circ Res 100:556–563
Wagner C, Jobs A, Schweda F, Kurtz L, Kurt B, Lopez ML, Gomez RA, van Veen TA, de Wit C, Kurtz A (2010) Selective deletion of Connexin 40 in renin-producing cells impairs renal baroreceptor function and is associated with arterial hypertension. Kidney Int 78:762–768
Wagner C, Kurtz L, Schweda F, Simon AM, Kurtz A (2009) Connexin 37 is dispensable for the control of the renin system and for positioning of renin-producing cells in the kidney. Pflugers Arch 459:151–158
Yao J, Suwa M, Li B, Kawamura K, Morioka T, Oite T (2003) ATP-dependent mechanism for coordination of intercellular Ca2+ signaling and renin secretion in rat juxtaglomerular cells. Circ Res 93:338–345
Zhang J, Hill CE (2005) Differential connexin expression in preglomerular and postglomerular vasculature: accentuation during diabetes. Kidney Int 68:1171–1185
Acknowledgments
The authors’ work is financially supported by grants from the German Research Foundation (Sonderforschungsbereich 699).
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of the special issue on the Renin–Angiotensin System.
Rights and permissions
About this article
Cite this article
Wagner, C., Kurtz, A. Distribution and functional relevance of connexins in renin-producing cells. Pflugers Arch - Eur J Physiol 465, 71–77 (2013). https://doi.org/10.1007/s00424-012-1134-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-012-1134-7