Abstract
The SLC7 family is divided into two subgroups, the cationic amino acid transporters (the CAT family, SLC7A1–4) and the glycoprotein-associated amino acid transporters (the gpaAT family, SLC7A5–11), also called light chains or catalytic chains of the hetero(di)meric amino acid transporters (HAT). The associated glycoproteins (heavy chains) 4F2hc (CD98) or rBAT (D2, NBAT) form the SLC3 family. Members of the CAT family transport essentially cationic amino acids by facilitated diffusion with differential trans-stimulation by intracellular substrates. In some cells, they may regulate the rate of NO synthesis by controlling the uptake of l-arginine as the substrate for nitric oxide synthase (NOS). The heterodimeric amino acid transporters are, in contrast, quite diverse in terms of substrate selectivity and function (mostly) as obligatory exchangers. Their selectivity ranges from large neutral amino acids (system L) to small neutral amino acids (ala, ser, cys-preferring, system asc), negatively charged amino acid (system xc −) and cationic amino acids plus neutral amino acids (system y+L and b0,+-like). Cotransport of Na+ is observed only for the y+L transporters when they carry neutral amino acids. Mutations in b0,+-like and y+L transporters lead to the hereditary diseases cystinuria and lysinuric protein intolerance (LPI), respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cationic amino acid transporters (CAT, SLC7A1–4) subfamily members have 14 putative transmembrane (TM) segments and are glycosylated, whereas the glycoprotein-associated amino acid transporters (gpaAT, SLC7A5–11) have two TM segments less, are not glycosylated, and need to associate with a glycoprotein of the SLC3 family [heavy chains 4F2hc or rBAT (related to b0,+AT-type amino acid transporter, where b0,+AT is the basic and neutral amino acid transporter)] for surface expression (Figs. 1 and 2).
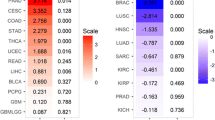
Phylogenetic tree of the SLC7 family proteins. The SLC7 family is composed of two subfamilies formed by the cationic amino acid transporters (CAT, SLC1–4) and the glycoprotein-associated amino acid transporters [gpaAT, light chains of heterodimeric amino acid transporters (HAT-lc), SLC5–11 and mouse neutral amino acid, ala, ser, cys-preferring transporter-2 (mAsc-2) and aspartate/glutamate transporter-1 (AGT1)]. SLC7A4 as well as Asc-2 and AGT1 differ slightly from the other subfamily members
Putative structure of SLC7 amino acid transporters. A A model of mCAT-1 in the membrane with 14 predicted transmembrane domains (TM I–XIV). The two confirmed glycosylation sites in the third extracellular loop of mCAT-1 are indicated. Although all CAT proteins are glycosylated, the positions of the glycosylation sites vary between isoforms and between species. Glu107 and the protein area that determine the transport properties are marked in red. B Model of HAT consisting of a light chain (SLC7A5–11) with 12 putative transmembrane helices associated with the heavy chain 4F2hc (CD98, SLC3A2) or rBAT (SLC3A1) through a conserved disulphide bridge. The COOH-terminus is localized intracellularly. The 12 TM of the light chains show considerable similarity to the first 12 TM of the CAT transporters. Only the heavy chain appears to be glycosylated
The homologous region of the two SLC7 subfamilies corresponds to the first 12 putative TM segments of the CATs and is ~20% identical and ~60% similar to gpaAT. Within each subfamily, the lowest level of identity is around 40%. It is noteworthy that among the CAT members, CAT-1 to CAT-3 are more closely related to each other (~60% identity) than to CAT-4 (~40% identity). There are also two additional gpaAT-related transporters, the murine ala, ser, cys-preferring transporter (mAsc-2) and the murine aspartate-glutamate transporter-1 (mAGT1), that, to date, have been described only in the mouse and do not interact with either 4F2hc or rBAT. They share ~45% identical residues with each other and only 24–29% with the other gpaATs. These two transporters need probably also the association with a heavy chain that, however, has not yet been identified.
CAT proteins: general aspects
The first family member of the SLC7 family (mCAT-1, for mouse cationic amino acid transporter) was originally identified by Albritton and coworkers as the receptor for murine ecotropic leukaemia viruses. Three additional related proteins, CAT-2A, -2B, and -3 (SLC7A2 and 3), have since been identified in different mammalian species, with CAT-2A and -2B being splice variants that differ only in a stretch of 42 amino acids (for review see: [14, 15, 18]). The function of the more distantly related isoform SLC7A4 (also referred to as CAT-4) has remained elusive [58, 66]. All other CAT proteins mediate Na+-independent transport of cationic l-amino acids.
The transport properties of CAT-1, -2B and -3 are consistent with those attributed originally to the classic cationic amino acid transporter system y+, with the most pronounced trans-stimulation being observed for CAT-1. In contrast, CAT-2A, a low-affinity carrier for cationic amino acids, is relatively insensitive to trans-stimulation (apparent K m for cationic amino acids: 2–5 mM, compared with 0.1–0.4 mM for the other CAT isoforms). In its protonated form (at pH 5.5), l-histidine is a good substrate for CAT-1, but not for CAT-3 [63]. Some other neutral amino acids are reportedly recognized by the CAT proteins, however, with rather low affinity (for review see: [14]). For CAT-1 and CAT-2A voltage dependence of cationic amino acid transport has been described, with membrane hyperpolarization increasing the V max for influx (for review see: [14, 15]).
Glu107 has been shown to be essential for the transport activity of mCAT-1 (for review see: [14, 15]). Located in TM III and conserved in all other known CAT isoforms, this Glu residue is likely to be part of the substrate translocation pathway. A region of 80 amino acids spanning from the fourth intracellular loop to TM X has been shown to determine the apparent substrate affinity of the CAT proteins and the sensitivity to trans-stimulation. This region contains the stretch of 42 amino acids that differs in the two splice variants, CAT-2A and -2B. The low substrate affinity of human CAT-2A (hCAT-2A) is determined by two amino acid residues within the stretch of 42 amino acids: Arg369 and a missing His at position 381 [27].
Glycoprotein-associated amino acid transporters (gpaAT): general aspects
The first hint for the existence of the gpaAT transporters came from expression cloning of the type-II glycoprotein rBAT in Xenopus laevis oocytes and the subsequent demonstration that the related 4F2hc protein induces amino acid transport in this expression system as well (see review by Palacin and Kanai on the SLC3 family in this issue). From the fact that 4F2hc (heavy chain) was known to associate covalently with a hydrophobic polytopic "light chain", it was deduced that the amino acid transport observed in Xenopus oocytes upon expression of heavy chains was due to their association with endogenous oocyte light chains (gpaATs) leading to the surface expression of heterodimeric amino acid transporters (HATs). The first member of this gpaAT family, LAT1, was identified in 1998 [30, 37].
Six of the known light chains associate with the widely distributed 4F2hc that is expressed strongly in growing cells and found basolaterally in polarized transporting cells of kidney and small intestine. One light chain, b0,+AT, associates with the related rBAT, localizing to the apical pole of epithelial cells in kidney proximal tubule and small intestine. The association with these type-II glycoproteins is covalent, via a disulphide bridge that links the extracellular neck of the glycoprotein with the second putative extracellular loop of the gpaAT (Fig. 2B) [46]. It appears that the glycoprotein does not play an active role in the actual amino acid transport function, since transport can be mediated by the gpaAT b0,+AT reconstituted in liposomes without its heavy chain [50]. The possible role of the glycoprotein heavy chain in modulating the transport properties of the light chain remains to be investigated in more detail.
Transport selectivity and ion coupling differ among gpaATs (see Abstract and below). A common functional feature of the heteromeric transporters is that they apparently function as (nearly) obligatory exchangers. This transport mode has been well documented in the case of the mouse system L transporters LAT1-4F2hc and LAT2-4F2hc, the anionic amino acid transporter system, cystine preferring system x− c xCT-4F2hc and the rBAT-induced Xenopus oocyte system b0,+-like [13, 39, 54]. For the L-type transporters, it has been shown that the selectivity of influx and efflux are similar (with some differences) but that the apparent substrate affinities are much lower for efflux (inside).
The amino acid transporters described in this review all correspond, with the exception of AGT1 to transport systems that had been described functionally before their cloning. Thus, the current nomenclature of these proteins is based to some extent on the names of the previously described systems. The features of the transporters are summarised in Table 1.
SLC7A1/CAT-1
CAT-1 is expressed almost ubiquitously with the exception of adult liver but its expression level varies considerably in different tissues and cell types. CAT-1 co-localizes with caveolin in endothelial cells (for review, see [36]) and is restricted to the basolateral membrane in epithelial cells, [10, 34]. Besides its expression in the plasma membrane, CAT-1 has also been found in intracellular vesicles in glioblastoma cells [66].
CAT-1 seems to be the major system y+ transporter in most cells (including NO-producing cells) (Fig. 3A, B). Homozygous CAT-1 knockout mice die on day 1 after birth, are 25% smaller than their wild-type littermates and suffer from severe anaemia, while the heterozygous mice exhibit no phenotypic abnormalities [45]. The relatively normal development of most tissues in the homozygous CAT-1 knockout mice up to birth is probably due to the expression of CAT-3 during embryogenesis and fetal development [42].
Physiological roles of SLC7 family amino acid transporters. A, B Outline of the role of CAT proteins in the substrate supply of endothelial (eNOS) and inducible nitric oxide synthase (iNOS). CAT proteins feed arginine into a pool of cationic amino acids (CAA) that is freely exchangeable with the extracellular space (pool I). In addition, an l-arginine pool that is not freely exchangeable with the extracellular space seems to exist in most cells (pool II). The eNOS in endothelial cells has access to pool II (A). In contrast, iNOS can only be fed from the exchangeable pool I (B). Macrophages seem to have two separated exchangeable l-arginine pools, pools IA and B, that are replenished by CAT-1 and CAT-2B, respectively, with iNOS receiving its substrate only from pool IB (further explanations and references, see text). C Concerted action of HAT proteins for vectorial transport of CAA and neutral amino acids (NAA) across epithelial cells of kidney proximal tubule and small intestine. For further explanation see paragraph on SLC7A9 (CssC cystine). D Role of the HAT protein LAT1 in non-polarized cells. Some neutral amino acids (NAA x ) taken up by Na+-dependent transporters (i.e. system A) can then be exchanged by LAT1-4F2hc for other extracellular neutral amino acids (NAA y )
CAT-1 expression can be modulated by a variety of stimuli including cell proliferation, growth factors, cytokines and hormones. In contrast to the "normal" cap-dependent protein synthesis, translation of the CAT-1 mRNA is increased during nutrient limitation [22]. In addition, the CAT-1 mRNA is stabilized under these conditions [67]. Independent of its protein expression, transport activity of human CAT-1 is decreased after activation of protein kinase C (PKC) in human endothelial cells, indicating posttranslational regulation [26]. CAT-1 activity can also be modulated by interaction with cytoskeletal proteins [69].
SLC7A2/CAT-2
The two CAT-2 splice variants (see above) exhibit quite distinct expression patterns. The low affinity CAT-2A is most abundant in liver, but is also expressed in skeletal muscle, pancreas, cardiomyocytes, cardiac microvascular endothelial cells and vascular smooth muscle. Significant expression of CAT-2B is only found after cytokine or lipopolysaccharide (LPS) treatment in most cell types. It is often induced together with the inducible isoform of NO-synthase (iNOS) and is generally co-expressed with CAT-1.
Surprisingly, homozygous CAT-2 −/− mice show no apparent phenotypic abnormalities, indicating that the expression of both CAT-2 splice variants is primarily dispensable [43]. However, the sustained NO production in peritoneal macrophages from these mice is almost abolished, underlining the important role of CAT-2B for the substrate supply of iNOS. Neither the expression of iNOS nor the intracellular l-arginine concentrations are reduced in these cells. The latter strongly indicates the presence of different exchangeable l-arginine pools in macrophages (see Fig. 3B).
SLC7A3/CAT-3
CAT-3 is expressed in mesoderm and in many developing tissues of mid-streak mouse embryos [29], but seems to be confined to central neurons in adult mice and rats [5, 28, 29]. In humans, strong CAT-3 expression has been observed in thymus, moderate expression in uterus, testis, mammary gland and brain and weak expression in ovary and stomach [63]. There is no correlation between the expression of CAT-3 and the neuronal NOS (nNOS). CAT-3 is thought to play a major role during embryogenesis. There have been no gene knockout studies reported to date.
SLC7A4/(CAT-4)
The SLC7A4 product is only ~40% identical to the CAT-1–3 proteins and its function is not known. The name CAT-4, which implies a function as cationic amino acid transporter, might thus be incorrect. SLC7A4 is expressed in brain, testis and placenta [58]. Besides its expression in the plasma membrane, SLC7A4 has also been found in intracellular vesicles in glioblastoma cells [66]. No gene knockout studies have yet been performed for SLC7A4.
SLC7A5/LAT1
LAT1 (L-type amino acid transporter-1) was identified on the basis of its capability to transport large neutral amino acids into Xenopus oocytes when expressed with 4F2hc (see above) [30, 37]. As expected for system L, this HAT protein also transports 2-(−)-endoamino-bicycloheptane-2-carboxylic acid (BCH) and its function is not Na+ sensitive. Its uptake selectivity range is relatively broad and the apparent affinity for the uptake of branched and aromatic amino acids is quite high (micromolar range) [30, 37, 39]. LAT1-4F2hc is an obligatory exchanger that does not mediate any measurable amino acid efflux in the absence of extracellular amino acids (no facilitated diffusion). Its uptake function is strongly trans-stimulated by intracellular amino acids and the stoichiometry of this exchange is 1:1 [39]. The apparent affinity for extracellular amino acids is as much as 100-fold higher than for intracellular ones, the concentration of the latter, thus, controls the transport rate [39]. The selectivity of the efflux function resembles that of uptake, but with some differences: in particular l-leucine, l-isoleucine and l-methionine are relatively better efflux than influx substrates [39]. Taken together, these functional data indicate that LAT1-4F2hc does not mediate net uptake of amino acids but rather that it is designed to equilibrate the relative concentrations of different amino acids across a membrane. Thus, it functions as a tertiary-active uptake transporter for amino acids that it exchanges against intracellular amino acids accumulated, for instance, via a Na+ cotransporter (Fig. 3D) [39, 64].
Interestingly, the first partial cDNAs for LAT1 were identified in activated human lymphocytes (E16) and in rat hepatoma cells (TA1). This, together with later observations that LAT1 is expressed in most tested tumours and tumour cell lines, suggests that LAT1-4F2hc may play an important role in many growing cells [65, 68].
SLC7A6/y+LAT2
The transporter(s) mediating y+L-type amino acid transport, i.e. the Na+-independent transport of cationic amino acids and the Na+-dependent uptake of neutral amino acids, was first described in erythrocytes and the expression of 4F2hc in Xenopus oocytes led to the expression of such a transport [17] (see review on SLC3 by Palacin and Kanai in this issue). The function of y+LAT2-4F2hc was first characterized briefly in papers describing the closely related epithelial y+LAT1-4F2hc transporter [48, 60]. In contrast to y+LAT1, y+LAT2 is widely expressed in non-epithelial and epithelial tissues. It mediates, as a heterodimer with 4F2hc, obligatory amino acid exchange of neutral and cationic amino acids with a stoichiometry of 1:1. The transport of neutral amino acids is coupled to Na+ [7]. Interestingly, whilst y+LAT2 mediates efficient influx of several neutral and cationic amino acids, the efflux of cationic amino acids is much more efficient than that of neutral ones [7]. The physiological role of this transporter is not clear at present.
SLC7A7/y+LAT1
The y+LAT1 cDNA was identified on the basis of its homology to LAT1 and was shown to function as system y+L when co-expressed with 4F2hc in Xenopus laevis oocytes [48, 60]. Detailed functional experiments showed that this heteromeric transporter mediates the uptake of neutral amino acids together with Na+ with a high apparent affinity, preferentially exchanging these neutral amino acids for intracellular cationic amino acids [31, 48, 60]. Its cationic amino acid efflux function and its high expression in kidney and small intestine suggested that it is the transporter defective in the hereditary disease lysinuric protein intolerance (LPI) (see below). Later experiments have confirmed its expected basolateral localization in kidney proximal tubule and small intestine and have shown that its expression follows a decreasing axial gradient along the proximal kidney tubule similar to LAT2 and b0,+AT [3].
SLC7A8/LAT2
LAT2 was also discovered by homology and functional experiments performed in Xenopus oocytes have demonstrated that its cell-surface amino acid uptake function depends on the association with 4F2hc and corresponds to system L but with a wider selectivity than LAT1-4F2hc (it accepts also smaller amino acids) [49, 52]. Its tissue distribution resembles that of y+LAT1, its major sites of expression being the basolateral membrane of the proximal kidney tubule (segment S1>S2>>S3) and small intestine [3, 52]. Functionally, it exchanges neutral amino acids across the basolateral membrane and thereby equilibrates their relative concentrations. Interestingly, it is a quite efficient exporter of l-cysteine, an amino acid that is imported into proximal kidney tubule cells mainly via the apical b0,+AT-rBAT transporter (defective in cystinuria) as l-cystine [39]. The role of LAT2-4F2hc in the basolateral efflux of l-cysteine has been substantiated recently in cell culture models [3, 21].
Similar to LAT1, LAT2 also displays a much lower apparent affinity for intracellular amino acids than for extracellular ones (exception for glycine). Taken together, LAT2 extends the selectivity range of a putative unidirectional basolateral efflux pathway (Fig. 3C) [64].
SLC7A9/b0,+AT
System b0,+ was first described as a Na+-independent transport system for cationic and neutral amino acids. Subsequently, a b0,+-like system that also transports l-cystine was described on the luminal side of renal proximal tubule and small intestine. Identification of rBAT and of b0,+AT as the heavy and light subunits of this transporter led to the identification of mutations in both subunits resulting in cystinuria (see review by Palacin and Kanai in this issue) [9, 11, 19, 47].
The b0,+AT protein has been shown to be covalently linked to rBAT and expressed in the brush border of the initial part of the proximal tubule and of jejunum and ileum (M. Dave, C. Wagner, F. Verrey, unpublished results) and thus has a similar tissue distribution to basolateral y+LAT1 and LAT2 [3, 20, 47]. Heterologous co-expression of rBAT and b0,+AT induces Na+-independent, high-affinity transport of l-cystine and cationic amino acids, and slightly lower affinity transport of neutral amino acids, by an obligatory exchange mechanism [8, 13, 47]. Under physiological conditions, luminal l-cystine and the cationic amino acids are taken up preferentially because of their high apparent extracellular affinity, the intracellular reduction of cystine to cysteine and the membrane potential (for cationic substrates), whereas the neutral amino acids are transported outwards because of their intracellular accumulation via an as yet unidentified, apical, B0-type Na+ cotransporter [13]. The basolateral efflux of the b0,+-like uptake of substrates is mediated mainly by LAT2- and y+LAT1-4F2hc in exchange for extracellular neutral amino acids [3, 64] (see below and Fig. 3C).The light chain b0,+AT is the catalytic subunit and has been shown recently to function alone as a transporter after reconstitution in liposomes [50]. The heavy chain rBAT is required for trafficking to the cell membrane [2].
SLC7A10/Asc-1
Asc-1 (asc-type amino acid transporter-1) was identified by homology and is linked to 4F2hc via a disulphide bond [25, 41]. It mediates Na+-independent transport of small neutral amino acids such as Gly, L-Ala, L-Ser, L-Thr, L-Cys, α-aminoisobutyric acid and β-alanine. Asc-1-4F2hc also transports d-isomers including D-Ser with high apparent affinity. It functions preferentially, but not exclusively, in an exchange mode. These functional properties appear consistent with those of system asc. Heterogeneity in substrate selectivity has been described for this transport system and the existence of at least two subtypes has been proposed. Asc-1 corresponds to the subtype that was characterized originally in trout peripheral blood lymphocytes, which is less stereospecific and transports α-aminoisobutyric acid and β-alanine.
Asc-1 exhibits the highest structural similarity to the L-type transporter light chain LAT2 (66% identity). In contrast to LAT2-4F2hc, which takes neutral amino acids of all sizes, and to LAT1-4F2hc, which transports only large ones, Asc-1 transports only small neutral amino acids and is not inhibited by BCH. This suggests an interesting transition in the spatial configuration of the substrate binding site between these gpaATs.
Asc-1 mRNA is expressed in the brain, lung, small intestine and placenta. Although the functional significance of Asc-1 has not yet been determined, it is notable that it transports d-serine, a putative endogenous modulator of NMDA-type glutamate receptors, and thus might play a role in regulating synaptic transmission.
SLC7A11/xCT
In many cell types system x− c provides cystine for the synthesis of glutathione (GSH: reducing agent, buffer for free radicals) and has been identified by expression cloning as a heterodimer composed of 4F2hc and the light chain xCT (SLC7A11) [54]. Under normal conditions, system x− c is found mainly in native brain (hypothalamic area, meninges) and in macrophages, as well as in most cell culture lines [1, 55]. It is Na+ independent and electroneutral and obeys an obligatory exchange mode, exchanging extracellular anionic cystine (pH dependence) for glutamate with a stoichiometry of 1:1. The driving force for this exchange is generated by the cystine concentration gradient (intracellular reduction) and the high intracellular concentration of glutamate. As cystine uptake and reduction are rate-limiting for GSH synthesis, system x− c activity directly controls intracellular GSH levels. Consequently, xCT expression is elevated in cells requiring high GSH synthesis, for instance activated macrophages, neuronal and glial cells and other cells after GSH depletion [6, 33, 54, 55]. Electrophile response element-like sequences mediate an increase in gene transcription in response to chemical stress agents in the presence of Nrf2, a transcription factor that is involved in the induction of several phase-II detoxifying enzymes [53].
Asc-2
Asc-2 (asc-type amino acid transporter-2) has been identified as a SLC7 family member. It exhibits relatively low, but significant, sequence similarity to other light chains [12]. The cysteine residue involved in the disulphide bond formation with the heavy chain is conserved in Asc-2, although Asc-2 does not induce functional activity when co-expressed either with 4F2hc or rBAT. Asc-2 was characterized functionally using fusion proteins of Asc-2 and 4F2hc or rBAT that were sorted to the plasma membrane. They expressed a transport function corresponding to the Na+-independent transport system asc. Unlike the other system asc transporter Asc-1-4F2hc, Asc-2 is stereoselective and does not accept some of the high-affinity substrates of Asc-1 such as α-aminoisobutyric acid and β-alanine. Asc-2 is expressed in kidney collecting duct cells, placenta, spleen, lung and skeletal muscle. In Western blot analysis, Asc-2 is detected as multiple bands under non-reducing conditions, whereas under reducing conditions it appears as a single band with a lower molecular mass, suggesting that it is linked to (an) unknown heavy chain(s) by a disulphide bond.
AGT1
AGT1 (aspartate/glutamate transporter-1) was identified as a SLC7 family member with 48% identity to Asc-2 [38]. As for Asc-2, fusion proteins either with 4F2hc or rBAT have been used for its functional characterization [38]. The AGT1 fusion protein expressed a Na+-independent transport activity for anionic amino acids that is distinct from that of xCT, since it does not accept cystine, homocysteate or l-α-aminoadipate, but exhibits high affinity for aspartate and glutamate. AGT1 is expressed predominantly in kidney where it localizes to basolateral membrane of the proximal straight tubules and distal convoluted tubules. As for Asc-2, Western blot analysis suggests association with an unknown heavy chain via a disulphide bond. The identification of AGT1 and Asc-2 has established a new subgroup of the heterodimeric amino acid transporters that do not associate with 4F2hc or rBAT, but rather with (an)other, as yet unknown heavy chain(s) (Fig. 1).
SLC7 transporters and inherited aminoacidurias
Mutations in b0,+AT or its heavy chain rBAT cause inherited, autosomal recessive cystinuria, a disease characterized by urinary hyperexcretion of cystine and cationic amino acids. Mutations in y+LAT1 cause lysinuric protein intolerance (LPI) that is manifested by urinary hyperexcretion of cationic amino acids [4, 19, 61]. Cystinuria is the most common primary inherited aminoaciduria and its associated pathology is due to the renal cystine lithiasis, whereas LPI is rare (<200 cases) with multi-system pathology.
Cystinuria has been classified into two phenotypic subtypes: type I, in which heterozygous relatives have normal urine amino acids, as is the case with all rBAT mutations and with 14% of the 40 cystinuria-specific b0,+AT mutations (including 18 missense mutations), and type non-I, in which heterozygotes with b0,+AT mutations have moderate-to-high aminoaciduria [16, 35]. In contrast to cystinuria, LPI is a monogenic disease. Twenty-five y+LAT1 mutations have been described worldwide in the 96 LPI patients that have been studied, and account for >98% of the cases [44].
Genotype/phenotype correlations have not been established in cystinuria or LPI patients due to extensive clinical differences of patients sharing the same genotype [16, 44]. In contrast, patients that are heterozygous for b0,+AT mutations show a genotype/phenotype correlation: the higher the loss of transport function of their mutated b0,+AT, the higher the hyperexcretion of amino acids [23].
Functional analyses of some disease-associated missense mutations of b0,+AT and y+LAT-1 [40, 50, 59] have revealed transport-inactivating defects, whereas all analysed rBAT mutations induce a trafficking defect. This agrees with the notion of a "catalytic" role of the light chain and a role for routing of the heavy chain.
In contrast to cystinuria, LPI is characterized also by a low plasma concentration of some amino acids that actually may be the main cause of failure to thrive of children [44, 56]. In cystinuria, other apical intestinal transporters, including that for oligopeptides, compensate the defect, whereas in LPI, the basolateral defect in cationic amino acid release is not sufficiently compensated. The low plasma concentration of cationic amino acids might be the cause of a defective urea cycle as well. Some LPI patients have furthermore symptoms that may be related to immune system defects such as erythroblastophagia, lung alveolar proteinosis and glomerulonephritis [44, 56]. Further research is needed to understand the aetiology of these LPI-associated alterations.
Pharmacological and pharmaceutical aspects of CAT transporters
Some derivatives of cationic l-amino acids are also substrates for the CAT proteins, including several inhibitors of nitric oxide synthase (NOS), e.g. l-N 5-(1-iminoethyl)-ornithine (L-NIO), N G-monomethylarginine (L-NMMA) or asymmetrical dimethylarginine (L-NMMA, L-ADMA), but not N G-nitroarginine (L-NNA) (for review see [14]). The CAT substrates not only compete with l-arginine for transport, but also drive the efflux of intracellular l-arginine, due to trans-stimulation. Other CAT substrates that are not NOS inhibitors (such as symmetrical dimethylarginine, L-SDMA), can also provoke depletion of intracellular arginine and therefore inhibit NO synthesis indirectly.
Due to its specific role for the substrate supply of iNOS in macrophages, CAT-2B represents a potential drug target in pathological situations where sustained iNOS activity may be detrimental, e.g. during sepsis or chronic inflammation. However, so far no inhibitors for the CAT proteins are available.
Pharmacological and pharmaceutical aspects of LAT1-4F2hc
A high level of LAT1 expression is observed in tumour cells of various tissue origins. Because LAT1-4F2hc transports into cells essential amino acids that are indispensable for protein synthesis, it is proposed that the inhibition of this transporter in tumour cells may be of some therapeutic benefit.
Another possible strategy in cancer therapeutics that involves LAT1 is the use of anti-tumour agents that are transported by LAT1-4F2hc and are, thus, delivered efficiently and relatively selectively into target tumour cells. For instance, the phenylalanine mustard melphalan is transported by LAT1-4F2hc and accumulates in cancer cells. It would, therefore, be possible to generate LAT1-4F2hc-permeable anti-tumour drugs considering its broad substrate selectivity [32, 62].
The transport of modified amino acids by LAT1-4F2hc has also many other (patho)physiological, pharmacological and diagnostic implications. This transporter has been shown to transport e.g. thyroid hormones, methylmercury-l-cysteine complexes and substances used for tumour labelling [24, 51, 57].
References
Bassi MT, Gasol E, Manzoni M, Pineda M, Riboni M, Martin R, Zorzano A, Borsani G, Palacin M (2001) Identification and characterisation of human xCT that co-expresses, with 4F2 heavy chain, the amino acid transport activity system xc. Pflugers Arch 442:286–296
Bauch C, Verrey F (2002) Apical heterodimeric cystine and cationic amino acid transporter expressed in MDCK cells. Am J Physiol 283:F181–F189
Bauch C, Forster N, Loffing-Cueni D, Summa V, Verrey F (2003) Functional cooperation of epithelial heteromeric amino Acid transporters expressed in Madin-Darby canine kidney cells. J Biol Chem 278:1316–1322
Borsani G, Bassi MT, Sperandeo MP, De Grandi A, Buoninconti A, Riboni M, Manzoni M, Incerti B, Pepe A, Andria G, Ballabio A, Sebastio G (1999) SLC7A7, encoding a putative permease-related protein, is mutated in patients with lysinuric protein intolerance. Nat Genet 21:297–301
Braissant O, Gotoh T, Loup M, Mori M, Bachmann C (1999) L-arginine uptake, the citrulline-NO cycle and arginase II in the rat brain: an in situ hybridization study. Brain Res Mol Brain Res 70:231–241
Bridges CC, Kekuda R, Wang H, Prasad PD, Mehta P, Huang W, Smith SB, Ganapathy V (2001) Structure, function, and regulation of human cystine/glutamate transporter in retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 42:47–54
Broer A, Wagner CA, Lang F, Broer S (2000) The heterodimeric amino acid transporter 4F2hc/y+LAT2 mediates arginine efflux in exchange with glutamine. Biochem J 349 Pt 3:787–795
Busch AE, Herzer T, Waldegger S, Schmidt F, Palacin M, Biber J, Markovich D, Murer H, Lang F (1994) Opposite directed currents induced by the transport of dibasic and neutral amino acids in Xenopus oocytes expressing the protein rBAT. J Biol Chem 269:25581–25586
Calonge MJ, Gasparini P, Chillaron J, Chillon M, Gallucci M, Rousaud F, Zelante L, Testar X, Dallapiccola B, Di Silverio F, Barcelo P, Estivill X, Zorzano A, Nunes V, Palacin M (1994) Cystinuria caused by mutations in rBAT, a gene involved in the transport of cystine. Nat Genet 6:420–425
Cariappa R, Heath-Monnig E, Furesz TC, Kamath SG, Smith CH (2002) Stable polarized expression of hCAT-1 in an epithelial cell line. J Membr Biol 186:23–30
Chairoungdua A, Segawa H, Kim JY, Miyamoto K, Haga H, Fukui Y, Mizoguchi K, Ito H, Takeda E, Endou H, Kanai Y (1999) Identification of an amino acid transporter associated with the cystinuria-related type II membrane glycoprotein. J Biol Chem 274:28845–28848
Chairoungdua A, Kanai Y, Matsuo H, Inatomi J, Kim DK, Endou H (2001) Identification and characterization of a novel member of the heterodimeric amino acid transporter family presumed to be associated with an unknown heavy chain. J Biol Chem 276:49390–49399
Chillaron J, Estevez R, Mora C, Wagner CA, Suessbrich H, Lang F, Gelpi JL, Testar X, Busch AE, Zorzano A, Palacin M (1996) Obligatory amino acid exchange via systems bo,+-like and y+L-like. A tertiary active transport mechanism for renal reabsorption of cystine and dibasic amino acids. J Biol Chem 271:17761–17770
Closs EI, Mann GE (2000) Membrane transport of L-arginine and cationic amino acids analogs. In: Ignarro LJ (ed) Nitric oxide: biology and pathobiology. Academic Press, San Diego, pp 225–241
Closs EI (2002) Expression, regulation and function of carrier proteins for cationic amino acids. Curr Opin Nephrol Hypertens 11:99–107
Dello Strologo L, Pras E, Pontesilli C, Beccia E, Ricci-Barbini V, de Sanctis L, Ponzone A, Gallucci M, Bisceglia L, Zelante L, Jimenez-Vidal M, Font M, Zorzano A, Rousaud F, Nunes V, Gasparini P, Palacin M, Rizzoni G (2002) Comparison between SLC3A1 and SLC7A9 cystinuria patients and carriers: a need for a new classification. J Am Soc Nephrol 13:2547–2553
Deves R, Chavez P, Boyd CA (1992) Identification of a new transport system (y+L) in human erythrocytes that recognizes lysine and leucine with high affinity. J Physiol (Lond) 454:491–501
Deves R, Boyd CAR (1998) Transporters for cationic amino acids in animal cells: discovery, structure, and function. Physiol Rev 78:487–545
Feliubadalo L, Font M, Purroy J, Rousaud F, Estivill X, Nunes V, Golomb E, Centola M, Aksentijevich I, Kreiss Y, Goldman B, Pras M, Kastner DL, Pras E, Gasparini P, Bisceglia L, Beccia E, Gallucci M, de Sanctis L, Ponzone A, Rizzoni GF, Zelante L, Bassi MT, George AL, Manzoni M, De Grandi A, Riboni M, Endsley JK, Ballabio A, Borsani G, Reig N, Fernandez E, Estevez R, Pineda M, Torrents D, Camps M, Lloberas J, Zorzano A, Palacin M (1999) Non-type I cystinuria caused by mutations in SLC7A9, encoding a subunit (bo,+AT) of rBAT. Nat Genet 23:52–57
Fernandez E, Carrascal M, Rousaud F, Abian J, Zorzano A, Palacin M, Chillaron J (2002) rBAT-b0,+AT heterodimer is the main apical reabsorption system for cystine in the kidney. Am J Physiol 283:F540–F548
Fernández E, Torrents D, Chillarón J, Martín del Río R, Zorzano A, Palacín M (2003) Basolateral LAT-2 has a major role in the transepithelial flux ofl-cystine in the renal proximal tubule cell line OK. J Am Soc Nephrol 14:837–847
Fernandez J, Bode B, Koromilas A, Diehl JA, Krukovets I, Snider MD, Hatzoglou M (2002) Translation mediated by the internal ribosome entry site of the CAT-1 mRNA is regulated by glucose availability in a PERK kinase-dependent manner. J Biol Chem 277:11780–11787
Font MA, Feliubadalo L, Estivill X, Nunes V, Golomb E, Kreiss Y, Pras E, Bisceglia L, d'Adamo AP, Zelante L, Gasparini P, Bassi MT, George AL Jr, Manzoni M, Riboni M, Ballabio A, Borsani G, Reig N, Fernandez E, Zorzano A, Bertran J, Palacin M (2001) Functional analysis of mutations in SLC7A9, and genotype-phenotype correlation in non-Type I cystinuria. Hum Mol Genet 10:305–316
Friesema EC, Docter R, Moerings EP, Verrey F, Krenning EP, Hennemann G, Visser TJ (2001) Thyroid hormone transport by the heterodimeric human system L amino acid transporter. Endocrinology 142:4339–4348
Fukasawa Y, Segawa H, Kim JY, Chairoungdua A, Kim DK, Matsuo H, Cha SH, Endou H, Kanai Y (2000) Identification and characterization of a Na+-independent neutral amino acid transporter that associates with the 4F2 heavy chain and exhibits substrate selectivity for small neutrald- and l-amino acids. J Biol Chem 275:9690–9698
Gräf P, Förstermann U, Closs EI (2001) The transport activity of the human cationic amino acid transporter hCAT-1 is downregulated by activation of protein kinase C. Br J Pharmacol 132:1193–1200
Habermeier A, Wolf S, Martine U, Graf P, Closs EI (2003) Two amino acid residues determine the low substrate affinity of the human cationic amino acid transporter-2A (hCAT-2A). J Biol Chem (In press)
Hosokawa H, Ninomiya H, Sawamura T, Sugimoto Y, Ichikawa A, Fujiwara K, Masaki T (1999) Neuron-specific expression of cationic amino acid transporter 3 in the adult rat brain. Brain Res 838:158–165
Ito K, Groudine M (1997) A new member of the cationic amino acid transporter family is preferentially expressed in adult mouse brain. J Biol Chem 272:26780–26786
Kanai Y, Segawa H, Miyamoto K, Uchino H, Takeda E, Endou H (1998) Expression cloning and characterization of a transporter for large neutral amino acids activated by the heavy chain of 4F2 antigen (CD98). J Biol Chem 273:23629–23632
Kanai Y, Fukasawa Y, Cha SH, Segawa H, Chairoungdua A, Kim DK, Matsuo H, Kim JY, Miyamoto K, Takeda E, Endou H (2000) Transport properties of a system y+L neutral and basic amino acid transporter. Insights into the mechanisms of substrate recognition. J Biol Chem 275:20787–20793
Kanai Y, Endou H (2001) Heterodimeric amino acid transporters: molecular biology and pathological and pharmacological relevance. Curr Drug Metab 2:339–354
Kim JY, Kanai Y, Chairoungdua A, Cha SH, Matsuo H, Kim DK, Inatomi J, Sawa H, Ida Y, Endou H (2001) Human cystine/glutamate transporter: cDNA cloning and upregulation by oxidative stress in glioma cells. Biochim Biophys Acta 1512:335–344
Kizhatil K, Albritton LM (2002) System y+ localizes to different membrane subdomains in the basolateral plasma membrane of epithelial cells. Am J Physiol 283:C1784–C1794
Leclerc D, Boutros M, Suh D, Wu Q, Palacin M, Ellis JR, Goodyer P, Rozen R (2002) SLC7A9 mutations in all three cystinuria subtypes. Kidney Int 62:1550–1559
Mann GE, Yudilevich DL, Sobrevia L (2003) Regulation of amino acid and glucose transporters in endothelial and smooth muscle cells. Physiol Rev 83:183–252
Mastroberardino L, Spindler B, Pfeiffer R, Skelly PJ, Loffing J, Shoemaker CB, Verrey F (1998) Amino acid transport by heterodimers of 4F2hc/CD98 and members of a permease family. Nature 395:288–291
Matsuo H, Kanai Y, Kim JY, Chairoungdua A, Kim do K, Inatomi J, Shigeta Y, Ishimine H, Chaekuntode S, Tachampa K, Choi HW, Babu E, Fukuda J, Endou H (2002) Identification of a novel Na+-independent acidic amino acid transporter with structural similarity to the member of a heterodimeric amino acid transporter family associated with unknown heavy chains. J Biol Chem 277:21017–21026
Meier C, Ristic Z, Klauser S, Verrey F (2002) Activation of system L heterodimeric amino acid exchangers by intracellular substrates. EMBO J 21:580–589
Mykkanen J, Torrents D, Pineda M, Camps M, Yoldi ME, Horelli-Kuitunen N, Huoponen K, Heinonen M, Oksanen J, Simell O, Savontaus ML, Zorzano A, Palacin M, Aula P (2000) Functional analysis of novel mutations in y+LAT-1 amino acid transporter gene causing lysinuric protein intolerance (LPI). Hum Mol Genet 9:431–438
Nakauchi J, Matsuo H, Kim DK, Goto A, Chairoungdua A, Cha SH, Inatomi J, Shiokawa Y, Yamaguchi K, Saito I, Endou H, Kanai Y (2000) Cloning and characterization of a human brain Na+-independent transporter for small neutral amino acids that transports d-serine with high affinity. Neurosci Lett 287:231–235
Nicholson B, Sawamura T, Masaki T, MacLeod CL (1998) Increased CAT3-mediated cationic amino acid transport functionally compensates in CAT1 knockout cell lines. J Biol Chem 273:14663–14666
Nicholson B, Manner CK, Kleeman J, MacLeod CL (2001) Sustained nitric oxide production in macrophages requires the arginine transporter CAT2. J Biol Chem 276:15881–15885
Palacin M, Borsani G, Sebastio G (2001) The molecular bases of cystinuria and lysinuric protein intolerance. Curr Opin Genet Dev 11:328–335
Perkins CP, Mar V, Shutter JR, delCastillo J, Danilenko DM, Medlock ES, Ponting IL, Graham M, Stark KL, Zuo Y, Cunningham JM, Bosselman RA (1997) Anemia and perinatal death result from loss of the murine ecotropic retrovirus receptor mCAT-1. Genes Dev 11:914–925
Pfeiffer R, Spindler B, Loffing J, Skelly P, Shoemaker C, Verrey F (1998) Functional heterodimeric amino acid transporters lacking cysteine residues involved in disulfide bond. FEBS Lett 439:157–162
Pfeiffer R, Loffing J, Rossier G, Bauch C, Meier C, Eggermann T, Loffing-Cueni D, Kuhn LC, Verrey F (1999) Luminal heterodimeric amino acid transporter defective in cystinuria. Mol Biol Cell 10:4135–4147
Pfeiffer R, Rossier G, Spindler B, Meier C, Kuhn L, Verrey F (1999) Amino acid transport of y+L-type by heterodimers of 4F2hc/CD98 and members of the glycoprotein-associated amino acid transporter family. EMBO J 18:49–57
Pineda M, Fernandez E, Torrents D, Estevez R, C L, Camps M, Lloberas J, Zorzano A, Palacin M (1999) Identification of a membrane protein, LAT-2, that co-expresses with 4F2 heavy chain, an L-type amino acid transport activity with broad specificity for small and large zwitterionic amino acids. J Biol Chem 274:19738–19744
Reig N, Chillaron J, Bartoccioni P, Fernandez E, Bendahan A, Zorzano A, Kanner B, Palacin M, Bertran J (2002) The light subunit of system b0,+ is fully functional in the absence of the heavy subunit. EMBO J 21:4906–4914
Ritchie JW, Peter GJ, Shi YB, Taylor PM (1999) Thyroid hormone transport by 4F2hc-IU12 heterodimers expressed in Xenopus oocytes. J Endocrinol 163:R5–R9
Rossier G, Meier C, Bauch C, Summa V, Sordat B, Verrey F, Kuhn LC (1999) LAT2, a new basolateral 4F2hc/CD98-associated amino acid transporter of kidney and intestine. J Biol Chem 274:34948–34954
Sasaki H, Sato H, Kuriyama-Matsumura K, Sato K, Maebara K, Wang H, Tamba M, Itoh K, Yamamoto M, Bannai S (2002) Electrophile response element-mediated induction of the cystine/glutamate exchange transporter gene expression. J Biol Chem 277:44765–44771
Sato H, Tamba M, Ishii T, Bannai S (1999) Cloning and expression of a plasma membrane cystine/glutamate exchange transporter composed of two distinct proteins. J Biol Chem 274:11455–11458
Sato H, Tamba M, Okuno S, Sato K, Keino-Masu K, Masu M, Bannai S (2002) Distribution of cystine/glutamate exchange transporter, system xc −, in the mouse brain. J Neurosci 22:8028–8033
Simell O (2001) Lysinuric protein intolerance and other cationic amino acidurias. In: Scriver CR, Beaudet AL, Sly SW, Valle D (eds) Metabolic and molecular bases of inherited diseases, 8th Edn. McGraw-Hill, New York, pp 4933–4956
Simmons-Willis TA, Koh AS, Clarkson TW, Ballatori N (2002) Transport of a neurotoxicant by molecular mimicry: the methylmercury-l-cysteine complex is a substrate for human L-type large neutral amino acid transporter (LAT) 1 and LAT2. Biochem J 367:239–246
Sperandeo MP, Borsani G, Incerti B, Zollo M, Rossi E, Zuffardi O, Castaldo P, Taglialatela M, Andria G, Sebastio G (1998) The gene encoding a cationic amino acid transporter (SLC7A4) maps to the region deleted in the velocardiofacial syndrome. Genomics 49:230–236
Toivonen M, Mykkanen J, Aula P, Simell O, Savontaus ML, Huoponen K (2002) Expression of normal and mutant GFP-tagged y+L amino acid transporter-1 in mammalian cells. Biochem Biophys Res Commun 291:1173–1179
Torrents D, Estevez R, Pineda M, Fernandez E, Lloberas J, Shi Y, Zorzano A, Palacin M (1998) Identification and characterization of a membrane protein (y+L amino acid transporter-1) that associates with 4F2hc to encode the amino acid transport activity y+L—a candidate gene for lysinuric protein intolerance. J Biol Chem 273:32437–32445
Torrents D, Mykkanen J, Pineda M, Feliubadalo L, Estevez R, de Cid R, Sanjurjo P, Zorzano A, Nunes V, Huoponen K, Reinikainen A, Simell O, Savontaus ML, Aula P, Palacin M (1999) Identification of SLC7A7, encoding y+LAT-1, as the lysinuric protein intolerance gene. Nat Genet 21:293–296
Uchino H, Kanai Y, Kim do K, Wempe MF, Chairoungdua A, Morimoto E, Anders MW, Endou H (2002) Transport of amino acid-related compounds mediated by L-type amino acid transporter 1 (LAT1): insights into the mechanisms of substrate recognition. Mol Pharmacol 61:729–737
Vékony N, Wolf S, Boissel JP, Gnauert K, Closs EI (2001) Human cationic amino acid transporter hCAT-3 is preferentially expressed in peripheral tissues. Biochemistry 40:12387–12394
Verrey F (2003) System L: heteromeric exchanger of large neutral amino acids involved in directional transport. Pflugers Arch445:529–533
Wolf DA, Wang S, Panzica MA, Bassily NH, Thompson NL (1996) Expression of a highly conserved oncofetal gene, TA1/E16, in human colon carcinoma and other primary cancers: homology to Schistosoma mansoni amino acid permease and Caenorhabditis elegans gene products. Cancer Res 56:5012–5022
Wolf S, Janzen A, Vékony N, Martiné U, Strand D, Closs EI (2002) Expression of solute carrier 7A4 (SLC7A4) in the plasma membrane is not sufficient to mediate an amino acid transport activity. Biochem J 364:767–775
Yaman I, Fernandez J, Sarkar B, Schneider RJ, Snider MD, Nagy LE, Hatzoglou M (2002) Nutritional control of mRNA stability is mediated by a conserved AU-rich element that binds the cytoplasmic shuttling protein HuR. J Biol Chem 277:41539–41546
Yanagida O, Kanai Y, Chairoungdua A, Kim DK, Segawa H, Nii T, Cha SH, Matsuo H, Fukushima J, Fukasawa Y, Tani Y, Taketani Y, Uchino H, Kim JY, Inatomi J, Okayasu I, Miyamoto K, Takeda E, Goya T, Endou H (2001) Human L-type amino acid transporter 1 (LAT1): characterization of function and expression in tumor cell lines. Biochim Biophys Acta 1514:291–302
Zharikov SI, Sigova AA, Chen S, Bubb MR, Block ER (2001) Cytoskeletal regulation of thel-arginine/NO pathway in pulmonary artery endothelial cells. Am J Physiol 280:L465–L473
Acknowledgements
The laboratory of FV is supported by the Swiss National Science Foundation grant 31-59141.99. The laboratory of MP is supported by the Spanish Dirección General de Investigación Científica y Técnica Research Grant PM 99/0172 and by the support of the Comissionat per a Universitats i Recerca de la Generalitat de Catalunya (Spain). The laboratory of EIC is supported by grants Cl 100/3-4 and the Collaborative Research Centre SFB 553 (project B4) from the Deutsche Forschungsgemeinschaft, Bonn, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verrey, F., Closs, E.I., Wagner, C.A. et al. CATs and HATs: the SLC7 family of amino acid transporters. Pflugers Arch - Eur J Physiol 447, 532–542 (2004). https://doi.org/10.1007/s00424-003-1086-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-003-1086-z