Abstract
The SLC19 gene family of solute carriers is a family of three transporter proteins with significant structural similarity, transporting, however, substrates with different structure and ionic charge. The three members of this gene family are expressed ubiquitously and mediate the transport of two important water-soluble vitamins, folate and thiamine. The concentrative transport of substrates mediated by the members of this gene family is energized by transcellular H+/OH− gradient. SLC19A1 is expressed at highest levels in absorptive cells where it is located in a polarized manner either in the apical or basal membrane, depending on the cell type. It mediates the transport of reduced folate and its analogs, such as methotrexate, which are anionic at physiological pH. SLC19A2 is expressed ubiquitously and mediates the transport of thiamine, a cation at physiological pH. SLC19A3 is also widely expressed and is capable of transporting thiamine. This review summarizes the current knowledge on the structural, functional, molecular and physiological aspects of the SLC19 gene family.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
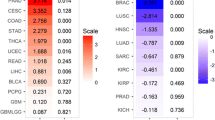
There are three members within the SLC19 family of solute carriers: a folate transporter (SLC19A1) and two thiamine transporters (SLC19A2 and SLC19A3). The folate transporter also mediates the transport of methotrexate, an antineoplastic and immunosuppressive agent. Since antifolates such as methotrexate have significant therapeutic potential, SLC19A1 has received considerable interest as a drug delivery system in cancer chemotherapy. Mutations in SLC19A1 in cancer cell lines result in resistance to antifolates. Despite the significant structural similarity among the three members of the gene family at the level of amino acid sequence (Table 1), there is very little structural similarity among their substrates. BLAST (basic local alignment search tool) search indicates that there are no additional, heretofore unidentified, members of the SLC19 gene family in the human genome. It is also evident that all three members are represented in lower organisms including Drosophila and C. elegans, but the substrate specificity and transport function of these putative transporters have not yet been established.
SLC19A1 transports folate and its derivatives that exist as anions at physiological pH, whereas SLC19A2 and SLC19A3 transport thiamine, which exists as a cation at physiological pH. One functional feature is, however, common among these three transporters. All are energized by a transmembrane pH gradient but with different mechanisms (Fig. 1). Folate influx into cells via SLC19A1 is stimulated by an inwardly directed H+ gradient (i.e., pHout<pHin), suggesting either folate/H+ symport or folate/OH− antiport as the transport mechanism. In contrast, thiamine influx into cells via SLC19A2 and SLC19A3 is enhanced by an outwardly directed H+ gradient (pHout>pHin), suggesting thiamine/H+ antiport as the transport mechanism. The members of this gene family are expressed ubiquitously, although at variable levels in different tissues. As a general pattern, the expression of these transporters is very high in absorptive tissues such as the intestine, kidney and placenta. Since folate and thiamine play vital roles in cellular metabolism, the transporters of the SLC19 gene family are of biological importance, and, consequently, disruptions of the functions of these transporters by genetic mutations can be expected to lead to serious clinical complications. The salient features of these three transporters and their corresponding genes are summarized in Table 2.
SLC19A1
The cloning of SLC19A1 was first accomplished by functional complementation, in which methotrexate-resistant human breast cancer cells (MTXR ZR-75-1) were transfected with cDNAs from a mouse cDNA library as a means of screening for the cDNA that could restore methotrexate-sensitivity in these cells [5]. Subsequently, SLC19A1 was cloned from other animal species either by a similar functional complementation approach or by homology screening [17, 22, 37, 39, 40]. The transporter is known as RFC (reduced folate carrier), RFT (reduced folate transporter), or FOLT (folate transporter). The open reading frame (ORF) of human SLC19A1 cDNA codes for a protein with 12 transmembrane domains and a single N-glycosylation site [17, 22, 37, 40]. The presence of 12 transmembrane domains has been confirmed experimentally by epitope insertion analysis [8]. However, alternative topological models have been proposed [14]. Site-directed mutagenesis studies have confirmed the glycosylation of SLC19A1 at the putative N-glycosylation site and also the noninvolvement of the carbohydrate moiety in the transport function [41]. The murine ortholog differs from its counterparts in other species in that it lacks the N-glycosylation site [5].
SLC19A1 mediates the cellular influx of folate and its derivatives. The carrier prefers reduced folates over non-reduced folates. Tetrahydrofolate and its derivatives N 5-methyltetrahydrofolate, N 5-formyltetrahydrofolate, and methotrexate exhibit much higher affinity for transport via this transporter compared with folate [30]. Interestingly, even though thiamine itself is not recognized by SLC19A1 as a substrate, the phosphate esters of thiamine are transported to some extent by this transporter [44, 46]. A common feature among the substrates of SLC19A1 is that all exist predominantly as anions at physiological pH. The transport function of SLC19A1 is sensitive to classical organic anion transport inhibitors such as probenecid. There is convincing evidence that SLC19A1 is energized by a transmembrane pH gradient (pHout<pHin) [24]. This suggests that the transport mechanism involves the influx of the anionic substrates that is coupled to either symport of H+ into cells or antiport of OH− out of the cells. Studies with native tissue preparations have shown, however, that the pH gradient-dependent transport activity of SLC19A1 is electroneutral [28]. This suggests that the monovalent anionic forms of folate and its derivatives are the preferred substrates for this transporter. This transport model is however equivocal because in certain cell types the transport function of SLC19A1 is not enhanced by a transmembrane pH gradient [24].
SLC19A1 mRNA is detectable in all human tissues. However, the expression is markedly higher in absorptive tissues such as the intestine, kidney, and placenta compared with tissues such as skeletal muscle and heart. In all cell types, the transporter is localized to the plasma membrane [35]. Interestingly, the transporter has also been detected in mitochondrial membranes where it may play a role in the trafficking of folate derivatives between cytoplasm and mitochondrial matrix [34].
The slc19a1 gene, located on human chromosome 21q22.3 [42], has five exons that contain the entire ORF [33, 38, 43]. In addition, there are multiple 5′-non-coding exons, which undergo variable splicing giving rise to different transcripts differing in their 5′untranslated region (UTR) [33, 38, 43]. Three TATA-less promoters with binding sites for several different transcription factors regulate the transcription of the gene [36]. Studies of the structure-function relationship in SLC19A1 show that the C-terminal cytoplasmic tail is important for the stability and membrane trafficking of the protein [26, 29] and that the intracellular loop between the transmembrane domains 6 and 7 is important for the function of the transporter [15]. Gene knockout studies in mice have shown that homozygous deletion of the gene leads to embryonic lethality [45]. Heterozygotes are viable. There is substantial interest in the activity of the transporter and homocysteinemia. N 5-Methyltetrahydrofolate is the donor of the CH3- group needed for the conversion of homocysteine to methionine catalyzed by the enzyme homocysteine-methyltransferase and thus folate deficiency results in elevated homocysteine levels [12]. Since homocysteinemia is associated with increased incidence of neural tube defects and cardiovascular complications, it is possible that, at least in some cases, mutations in the slc19a1 gene may contribute to the etiology of these clinical diseases.
The regulation of SLC19A1 expression and function has been investigated under various physiological and pathological conditions. Evidence indicates that the expression of the transporter in the intestine is subject to adaptive regulation in response to folate status [27]. Increased folate availability suppresses the transporter expression whereas folate deficiency enhances the transporter expression. The expression of the transporter is also cell cycle-dependent, with highest level of expression seen at the G1-to-S transition [11]. The transcription factor p53 also suppresses SLC19A1 expression [4]. In addition, the activity and expression of the transporter are decreased by nitric oxide and hyperglycemia [18, 31].
SLC19A2
The gene responsible for the disease thiamine-responsive megaloblastic anemia (TRMA or Rogers syndrome), located on human chromosome 1q23, was long believed to code for a thiamine transporter [32]. Subsequent studies by positional cloning and homology screening led to the successful isolation of the cDNA and establishment of its functional identity as a thiamine transporter [3, 6, 9, 13]. The SLC19A2 gene codes for a protein of 12 transmembrane domains and two N-glycosylation sites [3, 6, 9, 13]. The transporter has also been cloned from mouse tissues [20]. A splice variant, lacking 38 amino acids in the intracellular loop between the transmembrane domains 6 and 7, has been identified in certain tissues in mouse. This variant is functional, indicating the non-involvement of this protein region in transport function [16]. The N-glycosylation is also not essential for transport function [1].
SLC19A2 mediates the transport of thiamine [6]. The transport process is stimulated by a transmembrane pH gradient (pHout>pHin), suggesting that the transport mechanism most likely involves thiamine/H+ antiport. The transporter is very specific for thiamine and no other organic cations are recognized as substrates by the transporter [6]. SLC19A2 is expressed ubiquitously in human tissues [6]. Western analyses and immunohistochemical localization studies in mice indicate that the SLC19A2 protein is widely distributed and that the protein is expressed both on the cell surface and intracellular locations [10]. The slc19a2 gene consists of six exons. Targeted deletion of the gene results in diabetes, sensorineural deafness, and megaloblastosis in mice on thiamine-free diet [21]. The deletion of the gene has no effect on mice when supplemented with thiamine. Several mutations in the human slc19a2 gene have been identified that result in TRMA [19, 25]. Patients with TRMA are effectively treated with thiamine supplementation [19]. It is interesting to note that nutritional thiamine deficiency, known as beriberi, is associated with cardiovascular and/or neurological complications, symptoms not seen in patients with TRMA or in mice homozygous for slc19a2 gene deletion. This indicates that there are additional transporters for thiamine in humans and other mammals. Accordingly, SLC19A2 is referred to as ThTr1 (thiamine transporter 1).
SLC19A3
The third member of the SLC19 gene family was cloned recently by homology screening [7]. SLC19A3 also codes for a thiamine transporter and the transport process most likely involves thiamine/H+ antiport, as in the case of SLC19A2 [23]. SLC19A3 is therefore referred to as ThTr2 (thiamine transporter 2). As evidenced from the functional relationship between SLC19A2 and SLC19A3, there is a significant structural similarity between the two transporters. Since SLC19A3 is also expressed ubiquitously in humans and other mammals, it is possible that the intact function of this transporter is responsible for the lack of cardiovascular and neurological complications in humans and mice lacking the function of the slc19a2 gene. The slc19a3 gene is located on human chromosome 2q37 and consists of five exons coding for the ORF and additional 5′- and 3′-non-coding exons [7]. The murine slc19a3 gene maps to a region on chromosome 1 defined as a seizure susceptibility locus in the DBA/2J mouse strain [7]. Whether such a connection between seizure susceptibility and slc19a3 exists in humans is not known.
Role of SLC19 gene family members in the homeostasis of folate and thiamine
The SLC19 gene family plays an important role in the transport and homeostasis of folate and thiamine in the body. Since SLC19A1 has also been shown to transport mono- and pyro-phosphate derivatives of thiamine [44, 46], all three members of the SLC19 gene family may play a role in the homeostasis of thiamine. It is quite evident that the role of these transporters in non-polarized cells is to mediate the influx of folate and thiamine into the cells. However, in cells that mediate the transcellular transfer of these vitamins (e.g., the absorptive cells of the intestine and kidney, the syncytiotrophoblast in the placenta, and the retinal pigment epithelium), the exact role of these transporters is dependent on their polarized distribution in the apical membrane versus the basolateral/basal membrane. The distribution of SLC19A2 and SLC19A3 in these polarized cells has not yet been investigated and therefore it is difficult to predict their exact role in the transcellular movement of thiamine and consequently in thiamine homeostasis of the whole organism. On the other hand, recent advances in the area of subcellular localization of SLC19A1 in polarized cells have enhanced our understanding of the role of this transporter in the transcellular movement of folate (Fig. 2). Interestingly, folate homeostasis in most of these cells involve not only SLC19A1 but also folate receptor α (FRα), a glycosylphosphatidylinositol-anchored protein. In cells that express both FRα and SLC19A1, the two proteins are invariably polarized in a differential manner [2, 35]. Since FRα is capable of mediating only the influx of folate into the cells, this transport mechanism is located exclusively in the membrane where the entry of folate into the cells occurs as the initial step in the transcellular movement of this vitamin. Thus, FRα is located in the apical membrane of the renal tubular cell and the placental syncytiotrophoblast and in the basolateral membrane of the retinal pigment epithelium. The entry of folate via FRα involves receptor-mediated endocytosis and a hitherto unidentified transporter in the endosomal membrane. In contrast to FRα, SLC19A1 is capable of bidirectional transport and thus is located in the membrane where the exit of folate occurs from the cells to complete the transcellular transfer. Thus, SLC19A1 is located in the basolateral/basal membrane of the renal tubular cell and the placental syncytiotrophoblast and in the apical membrane of the retinal pigment epithelium. Interestingly, FRα does not seem to be expressed in the intestinal epithelium, an important site of transcellular transfer of folate involved in the absorption of this vitamin from dietary sources. SLC19A1 is expressed in the apical membrane of this epithelium and mediates the initial step (i.e., cellular entry of folate from the intestinal lumen) of the transcellular transfer. The molecular identity of the transport mechanism responsible for the exit of folate across the basolateral membrane of this epithelium has not yet been established.
References
Balamurugan K, Said HM (2002) Functional role of specific amino acid residues in human thiamine transporter SLC19A2: mutational analysis. Am J Physiol 283:G37–G43
Chancy CD, Kekuda R, Huang W, Prasad PD, Kuhnel JM, Sirotnak FM, Roon P, Ganapathy V, Smith SB (2000) Expression and differential polarization of the reduced-folate transporter-1 and the folate receptor alpha in mammalian retinal pigment epithelium. J Biol Chem 275:20676–20684
Diaz GA, Banikazemi M, Oishi K, Desnick RJ, Gelb BD (1999) Mutations in a new gene encoding a thiamine transporter cause thiamine-responsive megaloblastic anaemia syndrome. Nat Genet 22:309–312
Ding BC, Whetstine JR, Witt TL, Schuetz JD, Matherly LH (2001) Repression of human reduced folate carrier gene expression by wild type p53. J Biol Chem 276:8713–8719
Dixon KH, Lampher BC, Chiu J, Kelley K, Cowan KH (1994) A novel cDNA restores reduced folate carrier activity and methotrexate sensitivity to transport deficient cells. J Biol Chem 269:17–20
Dutta B, Huang W, Molero M, Kekuda R, Leibach FH, Devoe LD, Ganapathy V, Prasad PD (1999) Cloning of the human thiamine transporter, a member of the folate transporter family. J Biol Chem 274:31925–31929
Eudy JD, Spiegelstein O, Barber RC, Wlodarczyk BJ, Talbot J, Finnell RH (2000) Identification and characterization of the human and mouse SLC19A3 gene: a novel member of the reduced folate family of micronutrient transporter genes. Mol Genet Metab 71:581–590
Ferguson PL, Flintoff WF (1999) Topological and functional analysis of the human reduced folate carrier by hemagglutinin epitope insertion. J Biol Chem 274:16269–16278
Fleming JC, Tartaglini E, Steinkamp MP, Schorderet DF, Cohen N, Neufeld EJ (1999) The gene mutated in thiamine-responsive anaemia with diabetes and deafness (TRMA) encodes a functional thiamine transporter. Nat Genet 22:305–308
Fleming JC, Steinkamp MP, Kawatsuji R, Tartaglini E, Pinkus JL, Pinkus GS, Fleming MD, Neufeld EJ (2001) Characterization of a murine high-affinity thiamine transporter, Slc19a2. Mol Genet Metab 74:273–280
Gong M, Cowan KH, Gudas J, Moscow JA (1999) Isolation and characterization of genomic sequences involved in the regulation of the human reduced folate carrier gene (RFC1). Gene 233:21–31
Kang SS, Wong PW, Norusis M (1987) Homocysteinemia due to folate deficiency. Metabolism 36:458–462
Labay V, Raz T, Baron D, Mandel H, Williams H, Barrett T, Szargel R, McDonald L, Shalata A, Nosaka K, Gregory S, Cohen N (1999) Mutations in SLC19A2 cause thiamine-responsive megaloblastic anaemia associated with diabetes mellitus and deafness. Nat Genet 22:300–304
Liu XY, Matherly LH (2002) Analysis of membrane topology of the human reduced folate carrier protein by hemagglutinin epitope insertion and scanning glycosylation insertion mutagenesis. Biochim Biophys Acta 1564:333–342
Liu XY, Witt TL, Matherly LH (2003) Restoration of high-level transport activity by human reduced folate carrier/ThTr1 thiamine transporter chimaeras: role of the transmembrane domain 6/7 linker region in reduced folate carrier function. Biochem J 369:31–37
Lo PK, Wang FF (2002) Identification of transcriptional start sites and splicing of mouse thiamine transporter gene THTR-1 (Slc19a2). Biochim Biophys Acta 1576:209–213
Moscow JA, Gong M, He R, Sgagias MK, Dixon KH, Anzick SL, Meltzer PS, Cowan KH (1995) Isolation of a gene encoding a human reduced folate carrier (RFC1) and analysis of its expression in transport-deficient, methotrexate-resistant human breast cancer cells. Cancer Res 55:3790–3794
Naggar H, Ola MS, Moore P, Huang W, Bridges CC, Ganapathy V, Smith SB (2002) Downregulation of reduced-folate transporter by glucose in cultured RPE cells and in RPE of diabetic mice. Invest Ophthalmol Vis Sci 43:556–563
Neufeld EJ, Fleming JC, Tartaglini E, Steinkamp MP (2001) Thiamine-responsive megaloblastic anemia syndrome: a disorder of high-affinity thiamine transport. Blood Cells Mol Dis 27:135–138
Oishi K, Hirai T, Gelb BD, Diaz GA (2001) Slc19a2: cloning and characterization of the murine thiamin transporter cDNA and genomic sequence, the orthologue of the human TRMA gene. Mol Genet Metab 73:149–159
Oishi K, Hofmann S, Diaz GA, Brown T, Manwani D, Ng L, Young R, Vlassara H, Ioannou YA, Forrest D, Gelb BD (2002) Targeted disruption of Slc19a2, the gene encoding the high-affinity thiamin transporter Thtr-1, causes diabetes mellitus, sensorineural deafness and megaloblastosis in mice. Hum Mol Genet 11:2951–2960
Prasad PD, Ramamoorthy S, Leibach FH, Ganapathy V (1995) Molecular cloning of the human placental folate transporter. Biochem Biophys Res Commun 206:681–687
Rajgopal A, Edmondnson A, Goldman ID, Zhao R (2001) SLC19A3 encodes a second thiamine transporter ThTr2. Biochim Biophys Acta 1537:175–178
Rajgopal A, Sierra EE, Zhao R, Goldman ID (2001) Expression of the reduced folate carrier SLC19A1 in IEC-6 cells results in two distinct transport activities. Am J Physiol 281:C1579–C1586
Raz T, Labay V, Baron D, Szargel R, Anbinder Y, Barrett T, Rabl W, Viana MB, Mandel H, Baruchel A, Cayuela JM, Cohen N (2000) The spectrum of mutations, including four novel ones, in the thiamine-responsive megaloblastic anemia gene SLC19A2 of eight families. Hum Mutat 16:37–42
Sadlish H, Williams FM, Flintoff WF (2002) Cytoplasmic domains of the reduced folate carrier are essential for trafficking, but not function. Biochem J 364:777–786
Said HM, Chatterjee N, Haq RU, Subramanian VS, Ortiz A, Matherly LH, Sirotnak FM, Halsted C, Rubin SA (2000) Adaptive regulation of intestinal folate uptake: effect of dietary folate deficiency. Am J Physiol 279:C1889–C1895
Schron CM, Washington C Jr, Blitzer BL (1985) The transmembrane pH gradient drives uphill folate transport in rabbit jejunum. Direct evidence for folate/hydroxyl exchange in brush border membrane vesicles. J Clin Invest 76:2030–2033
Sharina IG, Zhao R, Wang Y, Babani S, Goldman ID (2002) Role of the C-terminus and the long cytoplasmic loop in reduced folate carrier expression and function. Biochem Pharmacol 63:1717–1724
Sierra E, Goldman ID (1999) Recent advances in the understanding of the mechanism of membrane transport of folates and antifolates. Semin Oncol 26:11–23
Smith SB, Huang W, Chancy C, Ganapathy V (1999) Regulation of the reduced-folate transporter by nitric oxide in cultured human retinal pigment epithelial cells. Biochem Biophys Res Commun 257:279–283
Stagg AR, Fleming JC, Baker MA, Sakamoto M, Cohen N, Neufeld EJ (1999) Defective high-affinity thiamine transporter leads to cell death in thiamine-responsive megaloblastic anemia syndrome fibroblasts. J Clin Invest 103:723–729
Tolner B, Roy K, Sirotnak FM (1998) Structural analysis of the human RFC-1 gene encoding a folate transporter reveals multiple promoters and alternatively spliced transcripts with 5′ end heterogeneity. Gene 211:331–341
Trippett TM, Garcia S, Manova K, Mody R, Cohen-Gould L, Flintoff W, Bertino JR (2001) Localization of a human reduced folate carrier protein in the mitochondrial as well as the cell membrane of leukemia cells. Cancer Res 61:1941–1947
Wang Y, Zhao R, Russell RG, Goldman ID (2001) Localization of the murine reduced folate carrier as assessed by immunohistochemical analysis. Biochim Biophys Acta 1513:49–54
Whetstine JR, Flatley RM, Matherly LH (2002) The human reduced folate carrier gene is ubiquitously and differentially expressed in normal human tissues: identification of seven non-coding exons and characterization of a novel promoter. Biochem J 367:629–640
Williams FM, Flintoff WF (1995) Isolation of a human cDNA that complements a mutant hamster cell defective in methotrexate uptake. J Biol Chem 270:2987–2992
Williams FM, Flintoff WF (1998) Structural organization of the human reduced folate carrier gene: evidence for 5′ heterogeneity in lymphoblast mRNA. Somat Cell Mol Genet 24:143–156
Williams FM, Murray RC, Underhill TM, Flintoff WF (1994) Isolation of a hamster cDNA clone coding for a function involved in methotrexate uptake. J Biol Chem 269:5810–5816
Wong SC, Proefke SA, Bhushan A, Matherly LH (1995) Isolation of human cDNAs that restore methotrexate sensitivity and reduced folate carrier activity in methotrexate transport-defective Chinese hamster ovary cells. J Biol Chem 270:17468–17475
Wong SC, Zhang L, Proefke SA, Matherly LH (1998) Effects of the loss of capacity for N-glycosylation on the transport activity and cellular localization of the human reduced folate carrier. Biochim Biophys Acta 1375:6–12
Yang-Feng TL, Ma YY, Liang R, Prasad PD, Leibach FH, Ganapathy V (1995) Assignment of the human folate transporter gene to chromosome 21q22.3 by somatic cell hybrid analysis and in situ hybridization. Biochem Biophys Res Commun 210:874–879
Zhang L, Wong SC, Matherly LH (1998) Structure and organization of the human reduced folate carrier gene. Biochim Biophys Acta 1442:389–393
Zhao R, Gao F, Wang Y, Diaz GA, Gelb BD, Goldman ID (2001) Impact of the reduced folate carrier on the accumulation of active thiamin metabolites in murine leukemia cells. J Biol Chem 276:1114–1118
Zhao R, Russell RG, Wang Y, Liu L, Gao F, Kneitz B, Edelmann W, Goldman ID (2001) Rescue of embryonic lethality in reduced folate carrier-deficient mice by maternal folic acid supplementation reveals early neonatal failure of hematopoietic organs. J Biol Chem 276:10224–10228
Zhao R, Gao F, Goldman ID (2002) Reduced folate carrier transports thiamine monophosphate: an alternative route for thiamine delivery into mammalian cells. Am J Physiol 282:C1512–C1517
Acknowledgements
This work was supported by National Institutes of Health Grants HD37150 (PDP) and EY12830 (SBS).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganapathy, V., Smith, S.B. & Prasad, P.D. SLC19: the folate/thiamine transporter family. Pflugers Arch - Eur J Physiol 447, 641–646 (2004). https://doi.org/10.1007/s00424-003-1068-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-003-1068-1