Abstract
Purpose
We describe a “left-posterior approach” in which the important steps in laparoscopic distal pancreatectomy (LDP) for left-sided pancreatic cancer are accomplished in the direction caudal and dorsal to the pancreas.
Methods
The patients who underwent LDP with a left-posterior approach at our hospital from January 2016 to April 2020 were reviewed to evaluate the short-term postoperative outcomes. In LDP, we first dissected retroperitoneal tissues above the left renal vein and superior mesenteric artery, yielding the mobilization of the pancreatic body widely. Then, the splenic artery was divided behind the ventrally lifted pancreas as an artery-first approach. The regional lymphadenectomy was performed in an en bloc manner consecutively in the same operative field. The neck of the pancreas was transected with a linear stapler after mobilization of the spleen.
Results
In nine patients (five men and four women) aged 76 years (range: 64–82 years), the operative time was 398 min (276–482 min) with the estimated blood loss of 40 ml (0–80 ml). No patients developed grade B/C pancreatic fistula or delayed gastric emptying. Postoperative complications classified as grade III in the Clavien–Dindo classification occurred in one patient (abdominal abscess). The pathology confirmed R0 resection in all patients who had pancreatic cancer (n = 5), IPMNs (n = 3), and high-grade pancreatic intraepithelial neoplasia (PanIN) (n = 1). The number of retrieved lymph nodes was 35 (11–49).
Conclusion
The procedure with a left-posterior approach is a rational surgical technique in LDP for left-sided pancreatic cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical resection is the only treatment with potential to cure pancreatic cancer or to achieve long-term survival [1]. Surgery takes the form of pancreatoduodenectomy for cancers of the head of the pancreas, and distal pancreatectomy for left-sided pancreatic cancers. For benign and low-grade malignant pancreatic tumors, recent studies have reported the advantages of minimally invasive surgery including laparoscopic distal pancreatectomy (LDP) over open surgery with respect to hospital stays and blood loss [2, 3]. LDP for pancreatic cancer has been reported to be safe and oncologically equivalent, although prospective comparative studies are lacking [3,4,5]. In centers with substantial experience with pancreatic surgery, LDP for pancreatic cancer has been increasingly performed. Nevertheless, standard procedures for LDP have not yet been established because LDP is a technically demanding operation that requires a pancreatectomy with adequate surgical margins and regional lymphadenectomy to achieve complete R0 resection.
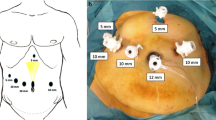
In the present paper, we describe a “left-posterior approach” to achieve adequate surgical margins with regional lymphadenectomy in LDP. In this approach, the important steps of the surgical procedures are all accomplished in the caudal and dorsal (i.e., posterior) direction to the pancreas mainly from the left side of the patient; the procedures enable the division of the splenic artery (SPA) behind the ventrally lifted pancreas before pancreatic transection as an artery-first approach, and the dissection of retroperitoneal tissues and regional lymphadenectomy in an en bloc manner consecutively, all in the same operative field (Fig. 1a, b). This approach allows determination of resectability of the disease, because direct exposure of the celiac axis with the origin of the SPA as well as the superior mesenteric artery (SMA) is possible before pancreatic transection, one of the points of no-return in pancreatic surgery.
Schematic illustrations of the left-posterior approach and trocar placement. a Schematic illustrations of the left-posterior approach for an artery-first en bloc resection in laparoscopic distal pancreatectomy. b Anterior view after the completion of the left-posterior approach. Retroperitoneal dissection with an “artery-first” division of the splenic artery and suprapancreatic lymphadenectomy are completed in an en bloc manner. c Trocar placement and the position for the insertion of a Nathanson liver retractor. The red arrows indicate the sutures for the stomach to be retracted upward to the abdominal wall. d The position of the surgeon and camera assistant holding a scope inserted into the left lower port during the left-posterior approach. CHA common hepatic artery, DC diaphragmatic crus, IMV inferior mesenteric vein, IVC inferior vena cava, LGA left gastric artery, LGV left gastric vein, LNs lymph nodes in the suprapancreatic lesion (station numbers 7, 8a, 8p, and 9), LRV left renal vein, SMA superior mesenteric artery, SMV superior mesenteric vein, SPA splenic artery, SPV splenic vein
Here, we describe our technique for LDP with an artery-first left-posterior approach for left-sided pancreatic cancers, and report the surgical outcomes of the procedure.
Patients and methods
The patients who underwent LDP with a left-posterior approach at Kyoto University Hospital from January 2016 to April 2020 were reviewed to document patient characteristics and short-term outcomes after surgery. We indicated a left-posterior approach in LDP for a left-sided pancreatic tumor which was preoperatively assumed to be potentially invasive, requiring retroperitoneal dissection to various extents with regional lymphadenectomy. Postoperative pancreatic fistula (POPF) and delayed gastric emptying (DGE) were defined according to the definitions of the International Study Group of Pancreatic Surgery (ISGPS) [6, 7]. All postoperative complications were graded according to the Clavien–Dindo classification [8]. We compared surgical outcomes between LDP with a left-posterior approach and LDP with a conventional “anterior” approach, in which the division of the splenic artery and lymphadenectomy were performed anteriorly, or an open distal pancreatectomy for a left-sided pancreatic tumor. The patients who underwent distal pancreatectomy with combined resection of the celiac axis or other organs, except for the spleen and left adrenal gland, were excluded in this study. Numbering and locations of lymph node stations are described according to the definition in the English edition of Classification of Pancreatic Carcinoma, edited by the Japan Pancreas Society [9]. Tumor staging was performed according to the International Union against Cancer (UICC) TNM classification (8th Edition) [10]. For statistical analysis, the comparison between two groups was performed with the Mann–Whitney U test using GraphPad Prism version 7.05 (GraphPad Software, San Diego, CA, USA). A p value < 0.05 was considered statistically significant.
Surgical procedures for laparoscopic distal pancreatectomy with a left-posterior approach
-
1.
The patient is placed in the supine position with the legs apart. During the operation, the patient is placed in reverse-Trendelenburg with a right-lateral tilt.
-
2.
The surgeon first stands to the right side of the patient, and the first assistant is on the left. The second assistant holds a flexible laparoscope between the patient’s legs.
-
3.
The initial umbilical trocar is placed using an open technique, and CO2 pneumoperitoneum is created with 10 mmHg of intraabdominal pressure. Five trocars are used in addition to the initial umbilical port: two ports on the right side with three on the left (Fig. 1c). A 12-mm trocar is placed on the right side of the umbilicus with a 5-mm trocar at around 5 cm above the 12-mm port. A 12-mm trocar is then placed in the subcostal left flank with a 5-mm trocar around 5 cm below the 12-mm one. An additional 15-mm trocar is then placed in the left lower quadrant of the abdomen. The left lower port is used for the insertion of a flexible scope during the left-posterior approach (Fig. 1d) and for a linear stapler to transect the neck of the pancreas, as mentioned below.
-
4.
The round ligament of the liver is held upward to the abdominal wall with a 2-0 silk thread inserted through an 18-gauge catheter. A Nathanson hook liver retractor, fixed with OCTOPUS (Yufu Itonaga Co., Ltd., Tokyo, Japan), is placed in the epigastric portion and used to gently hold the lateral segment of the liver.
-
5.
After inspection of the abdominal cavity, the gastrocolic ligament is divided and the lesser sac is opened. The splenocolic ligament is dissected so that the splenic flexure of the colon is mobilized. This procedure should be limited to the minimum extent necessary for tumors invading the mesocolon to avoid exposure of the tumor.
When combined resection of the Gerota fascia and left adrenal gland is planned, part of the upper pole of the renal fascia is also exposed (Fig. 2a).
At this moment, the left gastroepiploic vessels and the short gastric vessels in the gastrosplenic ligament are preserved.
-
6.
The stomach is hung upward to the abdominal wall by retracting the two sutures that are made directly to the back of the upper part of the stomach body and the antrum. The Nathanson liver retractor placed in the epigastric portion is also used to hold the back wall of the stomach upward to the abdominal wall. The pancreatic tail and the spleen are also slightly elevated upward by the traction together with the gastrosplenic ligament attached to the stomach (Fig. 2b).
-
7.
The transverse colon is lifted cranially by the assistant. The retroperitoneum is divided along the lateral margin of the ascending portion of the duodenum and the origin of the jejunum. The inferior vena cava and the left renal vein are exposed. The attachment of the origin of the jejunum to the mesocolon is dissected. The origin of the jejunum is mobilized, and the anterolateral surface of the SMA is exposed (Fig. 2c). The inferior mesenteric vein (IMV) is divided and the retroperitoneum is dissected to the left along the left renal vein to open a retroperitoneal window back of the pancreas (Fig. 2d).
-
8.
The transverse colon is retracted caudally, and the transverse mesocolon is divided along the inferior margin of the pancreas body and tail (Fig. 2e). The arcade of marginal vessels of the colon is preserved. The division line of the mesocolon is connected to the plane on which the splenocolic ligament is dissected.
-
9.
The pancreas is mobilized from the surface of the left adrenal gland and the anterior aspect of the fascia of left diaphragmatic crus is exposed.
When combined resection of the left adrenal gland is planned, the division line of the mesocolon is connected to the surface of the renal fascia exposed beforehand. The left adrenal vein is divided and retroperitoneal tissues behind the adrenal gland are dissected together with perirenal fat along the upper pole of left the kidney, followed by the exposure of the lateral aspect of the left crus fascia.
The operative field below the pancreas is now widely opened, and the main part of “the left-posterior approach” (procedures nos. 10–15 as mentioned below) is prepared to start (Fig. 2f).
-
10.
The surgeon moves to the patient’s left side with the assistant on the right. A laparoscope is inserted through the left lower port with the tip of the scope deflected laterally to the left up to the maximum extent (around 90°) to make a co-axial setting (Fig. 1d), and the main part of the left-posterior approach is initiated. The fascia of the diaphragmatic crus is exposed widely with the lymph nodes in the gastropancreatic fold (station number 9) lifted ventrally to the pancreas body and tail.
-
11.
The lymph nodes along the anterolateral aspect of the SMA are dissected with preservation of its surrounding nerve plexus. The superior mesenteric vein (SMV) is exposed above the pancreatic head plexus II [9] on the right side to the SMA. The spleno-portal junction and the confluence of the IMV and the SMV are also exposed.
-
12.
The shape of the origin of the celiac artery, surrounded with the dense nerve tissues and the celiac ganglion, appears between the anterior surface of the diaphragmatic crus and the anterior aspect of the origin of the SMA (Fig. 2f). The left and anterior wall of the portal vein is exposed upward into the hepatoduodenal ligament such that the inferior wall of the common hepatic artery (CHA) is exposed, just proximal to the bifurcation of the CHA and the gastroduodenal artery. The nerve tissues between the origin of the SPA and the CHA are dissected. The lymph nodes along the CHA (station number 8) attached to the pancreas are detached from the CHA.
-
13.
The origin of the SPA is isolated by dissecting the nerve tissues around the SPA, and secured with a 10-cm tape (Fig. 3a). The SPA is ligated with a 2-0 silk thread and a metal clip, and then divided.
-
14.
The IMV and SPV are divided at the confluence of the SMV with a metal clip or a linear stapler. When the IMV drains into the SPV, there is no need to divide the proximal side of the IMV.
-
15.
The lymph nodes along the CHA and LGA are dissected as a result of a skeletonization of both arteries, and lymph node station numbers 7–9 are anatomically separated off from the fascia of the diaphragmatic crus. The inferior side of the left caudate lobe of the liver and the infrahepatic vena cava are exposed behind the pancreas containing the dissected lymph nodes, which are elevated ventrally by the assistant (Fig. 3b). The left gastric vein is also divided at its junction to the PV or SPV during the procedure of the lymphadenectomy. All retroperitoneal tissues and lymph nodes intended to be resected are then anatomically separated off in an en bloc manner from the dorsal aspect, and “the left-posterior approach” is completed (Fig. 3c, d).
-
16.
The surgeon moves to the right side of the patient with the assistant on the left. The lymph nodes along the CHA (station numbers 8a and 8p) and around the LGA (station numbers 7 and 9) are already dissected in an en bloc manner and freed from the relevant arteries and the diaphragmatic crus, and they are all attached to the body-tail of the pancreas (Fig. 3e).
-
17.
The Nathanson liver retractor is replaced and the tension of the sutures to the stomach is also adjusted if needed to hold the stomach properly to obtain a good surgical field around the gastropancreatic fold. The anterior aspect of the gastropancreatic fold is cut at the intentional borderline of the lymph node station number 7 dissection directed to the upper edge of the gastrosplenic membrane along the stomach wall, and the LGA is liberated. The left gastric vein at the stomach side is divided.
-
18.
The attachment of the spleen to the retroperitoneum is divided, and the spleen is then mobilized from the retroperitoneum.
-
19.
The gastrosplenic ligament including the short gastric and the left gastroepiploic vessels is divided along the stomach wall. The specimen is then connected only by the neck of the pancreas.
-
20.
An intraoperative ultrasound is performed to determine and mark a planned pancreatic transection line with an adequate margin. The neck of the pancreas is transected with the linear stapler (Covidien Signia Tri-Staple 2.0 Reinforced Intelligent Reload, 60-mm extra-thick, black) inserted through the left lower 15-mm trocar after a sufficient compression using an intestinal clamp, followed by peri-firing compression with the stapler. The operative field after a pancreatectomy is shown in Fig. 3f.
-
21.
The specimen placed in a plastic bag is retrieved through the umbilical incision with a minimal extension.
-
22.
A closed drain is placed along the pancreatic transected margin through the right inferior port site with the tip of the drain located in the left subphrenic space.
Representative intraoperative view of the procedure. a Part of the upper pole of the renal fascia is exposed after a mobilization of the splenic flexure of the colon when an extensive retroperitoneal dissection is needed. b The stomach is retracted upward to the abdominal wall by the sutures and a Nathanson liver retractor. c The origin of the jejunum is mobilized, and the anterolateral surface of the SMA is exposed. d The inferior mesenteric vein is divided and the retroperitoneum is dissected to the left along the left renal vein. e The transverse mesocolon is divided along the inferior border of the pancreas body and tail. f The operative view of the left-posterior approach. The anterior aspect of SMA and the diaphragmatic crus are widely exposed. DC diaphragmatic crus, IMV inferior mesenteric vein, LGA left gastric artery, LRV left renal vein, SMA superior mesenteric artery, SMV superior mesenteric vein
Representative intraoperative view of the procedure. a The splenic artery is secured at its origin. b Suprapancreatic lymph nodes (station numbers 7, 8a, 8p, 9) are dissected from the diaphragmatic crus and relevant arteries, i.e., a skeletonization of the common hepatic artery and left gastric artery. c The operative view after the completion of the left-posterior approach. d The lymph nodes around the common hepatic artery (station numbers 8a and 8p) are anatomically dissected, exposing the inferior vena cava and the caudate lobe of the liver. e The anterior view after the completion of the left-posterior approach. Retroperitoneal dissection with the division of the splenic artery and suprapancreatic lymphadenectomy are completed in an en bloc manner. f The operative field after a pancreatectomy is shown. CHA common hepatic artery, CL caudate lobe, DC diaphragmatic crus, IMV inferior mesenteric vein, IVC inferior vena cava, LGA left gastric artery, LNs lymph nodes in the suprapancreatic lesion (station numbers 7, 8a, 8p, and 9), LRV left renal vein, SMA superior mesenteric artery, SMV superior mesenteric vein, SPA splenic artery, SPV splenic vein
Results
We performed LDP via the left-posterior approach for nine patients (five men and four women) with the median age of 76 years (range: 64–82 years) who had a left-sided pancreatic tumor. The procedure was completed laparoscopically in all patients except for one patient with pancreatic cancer who underwent planned minimal laparotomy only for a pancreatic transection by electrocautery at the last step of the operation because the tumor was close to the pancreas head. Patient demographics and clinical characteristic are summarized in Table 1. During the same period, we performed LDP with a conventional “anterior” approach for 16 patients, and open distal pancreatectomy for 30 patients.
In the nine patients undergoing LDP with a left-posterior approach, the preoperative diagnoses were pancreatic ductal adenocarcinoma (PDAC) in six patients (T1 in four patients and T2 in two patients) and intraductal papillary mucinous neoplasms (IPMNs) with undeniable invasive components in three patients (all T2). The median tumor size was 22 mm (range: 10–36 mm). The location of the tumor was the body and tail of the pancreas in four patients, the body in four patients, and the tail in one patient. Of the six patients with preoperative diagnosis of PDAC, five had received a definitive diagnosis of PDAC by endoscopic ultrasound-guided fine-needle aspiration biopsy; four patients received preoperative treatment in a neoadjuvant setting (Gemcitabine-based concurrent chemoradiotherapy for three patients and combination chemotherapy with Gemcitabine plus S-1 for one patient); while one patient was treated with modified FOLFIRINOX for 8 months because of suspected multiple lymph node metastases followed by LDP with lymphadenectomy. The remaining patient had a severe stricture in the main pancreatic duct of the pancreas body with adjacent parenchymal atrophy and dilated distal duct. The pancreatic juice cytology and brush cytology revealed atypical epithelial cells. We strongly suspected an invasive carcinoma in the surrounding area of the stricture; the pathological examination of the specimen revealed high-grade pancreatic intraepithelial neoplasia (PanIN) in the duct with stricture. For the three patients with IPMNs, we could not preoperatively rule out the possibility of the tumors having invasive components, all of which were pathologically proven to contain low- to intermediate-grade dysplasia.
The median operative time was 398 min (range: 276–482 min), which was not different from LDP with a conventional approach (368 min [146–496 min], p = 0.67) or open distal pancreatectomy (305 min [152–572 min], p = 0.06). The estimated blood loss was 40 ml (range: 0–80 ml), significantly lesser than that in LDP with a conventional approach (90 ml [0–1640 ml], p = 0.046) or open distal pancreatectomy (386 ml [94–8940 ml], p < 0.001). No patient required perioperative blood transfusions. There was no postoperative mortality. No patients developed clinically relevant (grade B or C) POPF or DGE, although biochemical leak was observed in two patients (22.2%). Postoperative complications of grade III or higher in the Clavien–Dindo classification occurred in one patient (IIIa, abdominal abscess). The pathology confirmed complete R0 resection in all patients in this study. The median number of retrieved lymph nodes was 35 (range: 11–49), which was significantly greater compared with LDP via a conventional approach (14 [2–44], p = 0.07), or open distal pancreatectomy (14 [1–44], p = 0.007).
The median postoperative hospital stay was 15 days (range: 8–36 days) and no patients required readmission. This was slightly short but not statistically different from that in open distal pancreatectomy (19 days [11–59 days], p = 0.07). Adjuvant chemotherapy was given to five patients with PDAC. The median time to adjuvant chemotherapy was 40 days (23–78 days). This was not different compared with LDP via a conventional approach (41 days [23–64 days], p = 0.81) or open distal pancreatectomy (41 days [24–84 days], p = 0.71).
Discussion
As a surgical treatment of pancreatic cancer, the tumor should be removed with sufficient surgical margins and adequate lymphadenectomy. Especially in the case of pancreatic body cancer, safe division of the splenic artery, both oncologically and surgically, with an adequate regional lymphadenectomy poses technical problems.
The division of the splenic vessels and lymphadenectomy in LDP are generally performed anteriorly (ventrally) to the pancreas [11,12,13]; little has been reported regarding the advantage of the dorsal approach [14, 15]. The idea of this “anterior approach” probably comes from the procedures in open distal pancreatectomy and laparoscopic gastrectomy that share a similar operative field with LDP. In open distal pancreatectomy, the concept of radical antegrade modular pancreatosplenectomy (RAMPS) has become widely used to obtain negative tangential margins [16,17,18,19]. Recently, several reports on laparoscopic RAMPS procedure have been published [11, 20]. In RAMPS, the dissection commences from right to left with early transection of the pancreas neck, followed by the division of splenic vessels and then retroperitoneal dissection posterolaterally [18]. Therefore, resectability based on arterial involvement is evaluated after pancreatic transection, which is a point of no-return in pancreatic surgery.
By contrast, our procedure with a left-posterior approach in LDP directly reaches the origin of the celiac axis and SMA consecutively after retroperitoneal dissection in the same direction of the same operative field. Determining resectability and division of the SPA are, therefore, possible before pancreatic transection in an “artery-first approach.” In pancreatoduodenectomy, the concept and importance of an artery-first approach is well accepted [21]; it consists of early determination of resectability based on the evaluation of arterial involvement before performing irreversible steps, and a precise dissection around the SMA and its branches to ensure negative surgical margins. Other potential benefits of an artery-first approach in pancreatoduodenectomy include shorter operative time, and reduction in intraoperative blood loss due to early ligation of the inferior pancreatoduodenal artery. An artery-first approach is, however, not common in distal pancreatectomy [22], possibly because of the anatomical difficulty. Because the origin of the SPA is often located behind the tumor or the pancreas itself, the difficulty of reaching the SPA before pancreatic transection with an “anterior approach” largely depends on the anatomy and tumor factor in each case. An anterior procedure in deep parts such as the lesion around the celiac axis would become more difficult with restriction of free motion of the forceps in laparoscopic surgery. On the other hand, our “left-posterior approach” is rational from the viewpoint of favorable forceps movement. The concept is similar to a caudal approach in laparoscopic liver surgery [23] or a medial-to-lateral approach in laparoscopic colorectal surgery [24] which enables early division of the feeding vessels with minimal tumor manipulation and favorable forceps movement with good views. Another advantage of our approach pertains to lymphadenectomy. As shown in the schematic illustration (Fig. 1a, b), suprapancreatic lymphadenectomy (station numbers 7, 8a, 8p, 9, and 11) can be anatomically performed in an en bloc manner in the same operative field behind a ventrally lifted pancreas. Because lymphadenectomy involves skeletonization of the corresponding arteries from the dorsal side of their axes, it can be accomplished at a distance from the tumor even in case of a tumor that is close to the origin of the CHA or SPA. In our experience, the number of retrieved lymph nodes was greater with this left-posterior approach than that in LDP with a conventional “anterior” approach or open distal pancreatectomy.
The limitations of our procedures are the technical demand for an assistant surgeon in obtaining an adequate surgical field at each surgical step and the difficulty in understanding the anatomy at the dorsal side of the pancreas. In the step with the infracolic approach, the transverse mesocolon and retroperitoneum around the IMV need to be stretched by an assistant surgeon. The exposure of the anterior aspect of the diaphragmatic crus and the SMA should be finished prior to the part approaching the SPA, because branches of the celiac artery, which are covered with dense nerve tissue and thus are not visible at first, must exist between the diaphragmatic crus and the SMA. Then, the pancreas should be lifted ventrally so that the SPA runs vertically from the origin to the pancreas. Confirmation of the anatomical landmarks at each surgical step is therefore crucial to understand the surgical anatomy, and thereby standardize the procedure to enable a safe and meticulous en bloc dissection.
Conclusion
Procedures with a left-posterior approach are a rational surgical technique that achieves artery-first LDP with anatomically en bloc retroperitoneal and lymph node dissection in left-sided pancreatic cancer.
Data availability
All data for this study are available as part of the article and no additional source data were required.
References
Ryan DP, Hong TS, Bardeesy N (2014) Pancreatic adenocarcinoma. N Engl J Med 371(11):1039–1049. https://doi.org/10.1056/NEJMra1404198
de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, van Dam R, Dejong C, van Duyn E, Dijkgraaf M, van Eijck C, Festen S, Gerhards M, Groot Koerkamp B, de Hingh I, Kazemier G, Klaase J, de Kleine R, van Laarhoven C, Luyer M, Patijn G, Steenvoorde P, Suker M, Abu Hilal M, Busch O, Besselink M (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg 269(1):2–9. https://doi.org/10.1097/SLA.0000000000002979
Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, D’Angelica MI, Balduzzi A, Bassi C, Bjornsson B, Boggi U, Callery MP, Del Chiaro M, Coimbra FJ, Conrad C, Cook A, Coppola A, Dervenis C, Dokmak S, Edil BH, Edwin B, Giulianotti PC, Han HS, Hansen PD, van der Heijde N, van Hilst J, Hester CA, Hogg ME, Jarufe N, Jeyarajah DR, Keck T, Kim SC, Khatkov IE, Kokudo N, Kooby DA, Korrel M, de Leon FJ, Lluis N, Lof S, Machado MA, Demartines N, Martinie JB, Merchant NB, Molenaar IQ, Moravek C, Mou YP, Nakamura M, Nealon WH, Palanivelu C, Pessaux P, Pitt HA, Polanco PM, Primrose JN, Rawashdeh A, Sanford DE, Senthilnathan P, Shrikhande SV, Stauffer JA, Takaori K, Talamonti MS, Tang CN, Vollmer CM, Wakabayashi G, Walsh RM, Wang SE, Zinner MJ, Wolfgang CL, Zureikat AH, Zwart MJ, Conlon KC, Kendrick ML, Zeh HJ, Hilal MA, Besselink MG (2019) The Miami International Evidence-Based Guidelines on Minimally Invasive Pancreas Resection. Ann Surg. https://doi.org/10.1097/SLA.0000000000003590
Riviere D, Gurusamy KS, Kooby DA, Vollmer CM, Besselink MG, Davidson BR, van Laarhoven CJ (2016) Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database Syst Rev 4:CD011391. https://doi.org/10.1002/14651858.CD011391.pub2
van Hilst J, Korrel M, de Rooij T, Lof S, Busch OR, Groot Koerkamp B, Kooby DA, van Dieren S, Abu Hilal M, Besselink MG (2019) Oncologic outcomes of minimally invasive versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a systematic review and meta-analysis. Eur J Surg Oncol 45(5):719–727. https://doi.org/10.1016/j.ejso.2018.12.003
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. surgery 161(3):584–591. https://doi.org/10.1016/j.surg.2016.11.014
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Buchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142(5):761–768. https://doi.org/10.1016/j.surg.2007.05.005
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Japan Pancreas Society (2017) Classification of Pancreatic Carcinoma. Fourth English edn. Kanehara & Co. Ltd, Tokyo
Brierley JD, Gospodarowicz MK, Wittekind C (2017) TNM Classification of Malignant Tumours, 8th edn. Wiley Blackwell, Oxford
Kim EY, Hong TH (2017) Initial experience with laparoscopic radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer in a single institution: technical aspects and oncological outcomes. BMC Surg 17(1):2. https://doi.org/10.1186/s12893-016-0200-z
de Rooij T, van Hilst J, Vogel JA, van Santvoort HC, de Boer MT, Boerma D, van den Boezem PB, Bonsing BA, Bosscha K, Coene PP, Daams F, van Dam RM, Dijkgraaf MG, van Eijck CH, Festen S, Gerhards MF, Groot Koerkamp B, Hagendoorn J, van der Harst E, de Hingh IH, Dejong CH, Kazemier G, Klaase J, de Kleine RH, van Laarhoven CJ, Lips DJ, Luyer MD, Molenaar IQ, Nieuwenhuijs VB, Patijn GA, Roos D, Scheepers JJ, van der Schelling GP, Steenvoorde P, Swijnenburg RJ, Wijsman JH, Abu Hilal M, Busch OR, Besselink MG (2017) Minimally invasive versus open distal pancreatectomy (LEOPARD): study protocol for a randomized controlled trial. Trials 18(1):166. https://doi.org/10.1186/s13063-017-1892-9
Hong S, Song KB, Madkhali AA, Hwang K, Yoo D, Lee JW, Youn WY, Alshammary S, Park Y, Lee W, Kwon J, Lee JH, Hwang DW, Kim SC (2019) Robotic versus laparoscopic distal pancreatectomy for left-sided pancreatic tumors: a single surgeon’s experience of 228 consecutive cases. Surg Endosc 34:2465–2473. https://doi.org/10.1007/s00464-019-07047-8
Ome Y, Seyama Y, Doi M, Muto J (2019) Laparoscopic distal pancreatectomy for left-sided pancreatic cancer using the “caudo-dorsal artery-first approach”. Ann Surg Oncol 26:4464–4465. https://doi.org/10.1245/s10434-019-07789-8
Wada Y, Aoki T, Murakami M, Fujimori A, Koizumi T, Kusano T, Matsuda K, Nogaki K, Hakozaki T, Shibata H, Tomioka K (2020) Individualized procedures for splenic artery dissection during laparoscopic distal pancreatectomy. BMC Surg 20(1):32. https://doi.org/10.1186/s12893-020-00694-y
Grossman JG, Fields RC, Hawkins WG, Strasberg SM (2016) Single institution results of radical antegrade modular pancreatosplenectomy for adenocarcinoma of the body and tail of pancreas in 78 patients. J Hepatobiliary Pancreat Sci 23(7):432–441. https://doi.org/10.1002/jhbp.362
Mitchem JB, Hamilton N, Gao F, Hawkins WG, Linehan DC, Strasberg SM (2012) Long-term results of resection of adenocarcinoma of the body and tail of the pancreas using radical antegrade modular pancreatosplenectomy procedure. J Am Coll Surg 214(1):46–52. https://doi.org/10.1016/j.jamcollsurg.2011.10.008
Strasberg SM, Drebin JA, Linehan D (2003) Radical antegrade modular pancreatosplenectomy. Surgery 133(5):521–527. https://doi.org/10.1067/msy.2003.146
Strasberg SM, Linehan DC, Hawkins WG (2007) Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg 204(2):244–249. https://doi.org/10.1016/j.jamcollsurg.2006.11.002
Kim S, Yoon YS, Han HS, Cho JY (2019) Laparoscopic subtotal pancreatectomy with radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer. Surg Oncol 28:150. https://doi.org/10.1016/j.suronc.2018.12.006
Sanjay P, Takaori K, Govil S, Shrikhande SV, Windsor JA (2012) ‘Artery-first’ approaches to pancreatoduodenectomy. Br J Surg 99(8):1027–1035. https://doi.org/10.1002/bjs.8763
Takaori K, Uemoto S (2016) Artery-First Distal Pancreatectomy. Dig Surg 33(4):314–319. https://doi.org/10.1159/000445016
Cho JY, Han HS, Wakabayashi G, Soubrane O, Geller D, O’Rourke N, Buell J, Cherqui D (2018) Practical guidelines for performing laparoscopic liver resection based on the second international laparoscopic liver consensus conference. Surg Oncol 27(1):A5–a9. https://doi.org/10.1016/j.suronc.2017.12.003
Veldkamp R, Gholghesaei M, Bonjer HJ, Meijer DW, Buunen M, Jeekel J, Anderberg B, Cuesta MA, Cuschierl A, Fingerhut A, Fleshman JW, Guillou PJ, Haglind E, Himpens J, Jacobi CA, Jakimowicz JJ, Koeckerling F, Lacy AM, Lezoche E, Monson JR, Morino M, Neugebauer E, Wexner SD, Whelan RL (2004) Laparoscopic resection of colon cancer: consensus of the European Association of Endoscopic Surgery (EAES). Surg Endosc 18(8):1163–1185. https://doi.org/10.1007/s00464-003-8253-3
Author information
Authors and Affiliations
Contributions
Study conception and design: KN, GK, AY, TA, SY, K. Taura, K. Takaori, TM. Acquisition of data: KN. Analysis and interpretation of data: KN, TM. Drafting of manuscript: KN, TM. Critical revision of manuscript: KN, GK, AY, TA, SY, K. Taura, K. Takaori, TM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This study was approved by the Ethics Committee of Kyoto University (R0455). Since this was a retrospective study, formal consent for the study was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
(MP4 202943 kb)
Rights and permissions
About this article
Cite this article
Nagai, K., Kiguchi, G., Yogo, A. et al. Left-posterior approach for artery-first en bloc resection in laparoscopic distal pancreatectomy for left-sided pancreatic cancer. Langenbecks Arch Surg 405, 1251–1258 (2020). https://doi.org/10.1007/s00423-020-02021-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-02021-8