Abstract
Purpose
Pancreatic body/tail cancer commonly invades the hepatic artery or celiac artery, making surgical resection difficult. Distal pancreatectomy with celiac axis resection (DP-CAR) has recently been performed to achieve curative resection of these tumors. However, the safety and efficacy remain unclear. This study aimed to clarify the efficacy and safety of DP-CAR, mainly focusing on the combination with neoadjuvant therapy (NAT).
Methods
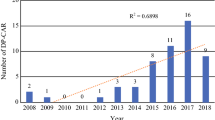
We retrospectively reviewed 31 consecutive patients with pancreatic ductal adenocarcinoma who underwent DP-CAR between 2010 and 2016. Data from 7 patients who underwent DP-CAR without NAT were used as a reference (upfront surgery, US).
Results
Gemcitabine + S-1 (GS) (n = 17) and gemcitabine + albumin-bound paclitaxel (GnP) (n = 8) were frequently used as NAT. DP-CAR following NAT was performed safely with 1 death, resulting in a mortality rate of 3%. The median survival time (MST) in the NAT group was 38.6 months, while that in the US group was 15.6 months. The NAT group had a high R0 resection rate (74%), while only 1 of 7 cases in the US group achieved R0 resection. Within the NAT group, patients treated with GS showed favorable overall survival with 39.5 months of MST, while that of patients treated with GnP was 19.8 months.
Conclusion
The combination of NAT and DP-CAR was feasible and safe for pancreatic body/tail cancer invading the celiac artery and/or hepatic artery. This strategy should be further assessed for the optimal regimen and duration of NAT in prospective studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic body/tail cancer is usually diagnosed at an advanced stage. Even without distant metastasis, it commonly invades the hepatic artery (HA) and/or celiac artery (CA), making surgical resection difficult. According to National Comprehensive Cancer Network (NCCN) guidelines [1], contact of a tumor with the HA and/or CA is defined as borderline resectable (BR), with a higher likelihood of incomplete resection, or unresectable (UR). Distal pancreatectomy with celiac axis resection (DP-CAR), or modified Appleby procedure, may be the only option for tumor eradication in patients with such advanced pancreatic cancer.
This procedure was originally performed by Appleby in a patient with advanced gastric cancer involving nodal metastases and the CA [2] and was modified by omitting gastrectomy for resection of advanced pancreatic body cancer [3,4,5]. Since Hirano and the Hokkaido University group reported long-term results for this procedure in 2007 [6], several reports have demonstrated its safety and efficacy [7,8,9]. However, the survival benefit for this procedure is still limited. Recent meta-analyses revealed that the median survival time of patients who underwent DP-CAR was 14.4–17.0 months [10, 11]. However, safety remains a concern. The Hokkaido University group reported a post-DP-CAR mortality rate of 5% in their long-term follow-up analysis [12]. Due to these problems, DP-CAR has not been widely accepted.
Recently, multidisciplinary treatment combining surgical resection and chemo(radio)therapy for pancreatic cancer has been widely accepted for the improvement of survival, especially in advanced cancer. For BR or UR pancreatic cancer, several guidelines or expert consensus statements, such as those from the NCCN [1], International Study Group of Pancreatic Surgery (ISGPS) [13], or European Organization for Research and Treatment of Cancer [14], recommend neoadjuvant therapy (NAT) or preoperative treatment. However, reports regarding the combination of DP-CAR and preoperative treatment are limited. To the best of our knowledge, in this study, we report the largest single-institution experience using this combination. The objective of this study was to clarify the efficacy and safety of DP-CAR, focusing on the combination with NAT.
Materials and methods
Patients
This study included 31 consecutive patients who underwent DP-CAR for pancreatic body/tail cancer without distant metastasis following neoadjuvant chemo(radio)therapy in Chiba University Hospital between 2010 and 2016. Clinicopathologic data from these patients were collected retrospectively and analyzed in this study. All 31 patients had invasive ductal adenocarcinoma of the pancreas, diagnosed with histological analysis. Cases with incidental para-aortic lymph node metastasis that was detected only on postoperative histological analysis were included in this study. The stages of pancreatic carcinoma were based on the TNM Classification of Malignant Tumors 8th edition of the Union for International Cancer Control (UICC) [15]. Resectability status (R, resectable; BR, borderline resectable; UR, unresectable) was defined using the NCCN guidelines [1]. Resection margin status (R) was also defined according to the UICC TNM classification [15]: resection margin positivity was defined as 1 or more cancer cells at any tumor surface (R1). Pathological responses to NAT were defined with the Evans grading system [16]. Completion of adjuvant therapy was defined as treatment for 4 months or more. Postoperative complications were graded according to the Clavien-Dindo classification [17]. Postoperative pancreatic fistula and delayed gastric emptying were defined according to the classification of the ISGPS [18, 19]. Response rate was defined as the ratio of cases in which computed tomography (CT) images obtained before surgery showed a partial response (PR) or complete response (CR) with NAT, according to the revised Response Evaluation Criteria in Solid Tumors (RECIST) guideline (ver. 1.1) [20]. Data of 7 patients who underwent DP-CAR without NAT between 2004 and 2016, including 5 patients who underwent DP-CAR before we started to use NAT (2004–2009) and 2 patients who refused to have NAT, were used as a reference.
This study was conducted in accordance with the ethical standards of the Committee on Human Experimentation and was approved by the Institutional Ethics Committee of our institution (Chiba University, Graduate School of Medicine #2732). The methods were carried out in accordance with the approved guidelines.
Indication for DP-CAR, preoperative treatment, and operative procedure
DP-CAR was indicated in patients with pancreatic body cancer possibly involving or contacting the CA, common hepatic artery (CHA), or origin of the splenic artery, based on imaging diagnosis or intraoperative findings. Preoperative coil embolization of the CHA and left gastric artery (LGA) was performed except in cases with the replacement of the HA by the superior mesenteric artery (SMA) [12, 21]. Multidetector-row CT was usually repeated every 3 months after initiation of NAT. Surgery was performed if patient status and organ function were well maintained and CT images met the following criteria, even when a response to NAT was not observed: (1) without distant metastasis, (2) without SMA or gastroduodenal artery (GDA) stenosis or deformity due to tumor invasion, and (3) without tumor contact or invasion of the aorta.
From 2010 to 2014, we used gemcitabine and S-1 (GS) for combined NAT (n = 17), according to the protocol of Nakamura et al. [22]: briefly, we treated patients with 60 mg/m2/day S-1 on days 1–14 and 1000 mg/m2 gemcitabine on days 8 and 15 of a 21-day cycle. After 2015, we changed the neoadjuvant treatment protocol to gemcitabine and albumin-bound paclitaxel (nab-PTX) combined therapy (GnP) (n = 8). We administered 1000 mg/m2 gemcitabine and 125 mg/m2 nab-PTX on days 1 and 8 of a 21-day cycle. Six patients were referred to our hospital after receiving chemo or chemoradiation therapy other than GS or GnP.
The DP-CAR procedure basically included en bloc resection of the celiac axis including the celiac plexus, CHA, and left gastric artery. Arterial flow to the liver through the GDA was confirmed using Doppler ultrasonography or confirmation of pulsation in the proper hepatic artery during the operation. Reconstruction of the HA was not required in all cases. We performed regional lymph node dissection, but not extensive dissection of the SMA plexus, adrenal gland, ganglions, or Gerota’s fascia, except for cases in which direct invasion to these regions was suspected on preoperative imaging or intraoperative findings. Resection and reconstruction of the portal vein or superior mesenteric vein were performed when necessary. Patients were treated with adjuvant therapy using either gemcitabine, S-1, or GS therapy, if the performance status was acceptable.
Statistical analysis
Cumulative survival was estimated using the Kaplan-Meier method, and the differences in survival were examined using the log-rank test. P < 0.05 was considered significant. Statistical analyses were performed using JMP 12 software (SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
Table 1 shows the characteristics of 31 patients who received NAT. Median age was 66 years and 68% of patients were male. Average serum carbohydrate antigen 19-9 (CA19-9) level was relatively high at 1164 IU/ml. As we only performed DP-CAR for tumor contacting the CA and/or CHA, most patients were classified as BR (87%). Four patients were classified as UR due to tumor contact with the GDA or aorta at the time of diagnosis. The background of these patients was comparable to that of the 7 patients who underwent upfront surgery (US).
Effects of neoadjuvant therapy
We then analyzed the effects of NAT. Starting in 2010, we used NAT for BR and UR pancreatic cancer patients. GS was most frequently used as NAT (n = 17), followed by GnP (n = 8). The duration between the initiation of NAT and surgery was a median of 90 days (range, 33–699). The response rate with NAT was 39%, and the median serum CA19-9 level decreased from 1164 to 241 IU/ml (P = 0.006) (Table 1).
Surgical, short-term, and long-term outcomes
Table 2 shows surgical and perioperative outcomes. Preoperative coil embolization was generally performed before surgery. Embolization was performed safely without any complications, such as coil dislocation in the proper hepatic artery. CHA and LGA coil embolization was performed in 24 of 31 patients who underwent NAT. Embolization was not performed in 4 patients due to a replacement of the right or common HA by the SMA, and in 3 patients due to technical difficulties. The median duration between coil embolization and surgery was 49 days (range, 3–369).
The mean operative time and blood loss were 350 min and 1274 ml, respectively. Portal vein resection was performed in 12 cases (39%). Grade III or higher Clavien-Dindo complications occurred in 13 patients (42%), most of which were postoperative pancreatic fistulas. Ischemic complications were limited, but there were 3 cases of gastritis and 1 case of liver abscess. One patient who previously underwent distal gastrectomy for gastric cancer and had preoperative CHA coil embolization died 47 days after surgery due to gastric perforation followed by sepsis. The in-hospital mortality rate was 3%.
These surgical and postoperative factors were similar to those of 7 patients with US. We did not perform a statistical comparison between patients who underwent NAT and US, because most of the 7 patients in the US group underwent DP-CAR during a time period (2004–2010) when we were on the learning curve for this procedure. However, these results at least indicated that NAT did not affect the operative and postoperative courses.
Histopathological analysis (Table 2) revealed that the majority of patients (84%) had limited pathological effects (Evans grade I or IIa) from NAT. R0 resection was achieved in 23 patients (74%). In contrast, R0 resection was achieved in only 1 of 7 patients in the US group.
Survival of patients who underwent DP-CAR following NAT
In 31 patients who underwent NAT, the median observation period was 29.6 months. Even with limited pathological effects, survival in patients who underwent NAT was favorable. The median overall survival time (MST) and 3-year survival rate from initiation of therapy were 38.6 months and 50.7%, respectively. In contrast, those of US patients were 15.6 months and 14.3%, respectively (Fig. 1a), similar to the values in a previous report [11]. R0 resection was the key to long-term survival after DP-CAR in patients who underwent NAT. MST after surgery in R0 patients (n = 23) was 31.8 months, while MST in R1 or 2 patients (n = 8) was 17.5 months (P = 0.03) (Fig. 1b).
Overall survival (OS) of patients who underwent DP-CAR. a OS from initiation of therapy in patients who underwent DP-CAR with neoadjuvant therapy (NAT) (n = 31) and upfront surgery (US) (n = 7). b OS from surgery, stratified by residual tumor status (R) in patients with NAT. Patients with R0 resection survived significantly longer than patients with R1 or 2 resection (P = 0.03)
We investigated whether a treatment regimen with NAT affected the prognosis of patients who underwent DP-CAR. As described previously, we used GS for NAT until 2014. After 2015, we mainly used GnP. We analyzed the data of patients who received GS (n = 17) and GnP (n = 8) as NAT (Table 3). Due to the small sample size, we did not perform a statistical comparison between these two groups. Patient background, tumor size, serum CA19-9 level, and resectability were comparable between the two groups. The histopathological factors in the two groups were also similar, except for the pathological UICC T stage. The GnP group showed a relatively high response rate (4 of 8 cases had a partial response [PR]) and R0 resection was achieved in all cases; in contrast, the GS group showed a 35% response rate (6 of 17 cases had a PR) and 65% R0 resection rate. Unexpectedly, even though R0 resection was achieved in all GnP cases, the GnP group showed lesser overall survival time than the GS group. MST was 19.8 months in the GnP group and 38.6 months in the GS group (Fig. 2a). The liver was the most frequent site of primary recurrence in the GnP group, while local recurrence was most frequent in the GS group (Fig. 2b). However, due to the small patient numbers and different treatment periods, no statistical conclusion was drawn in a comparison between the two groups.
Comparison of overall survival (OS) and recurrence pattern between patients who received neoadjuvant therapy with gemcitabine and S-1 combination (GS) and gemcitabine and albumin-bound paclitaxel combination (GnP). a Comparison of OS from initiation of therapy. b Primary recurrence site. GnP group showed the tendency to have hepatic recurrence
Discussion
The safety and efficacy of DP-CAR for pancreatic body cancer remain controversial. We have aggressively used this procedure to achieve curative resection for pancreatic body/tail cancer invading the CHA and/or CA.
In our study, mortality occurred in only 1 of 31 patients who underwent DP-CAR following NAT. Life-threatening complications (Clavien-Dindo grades IVa and b) occurred in 1 case (3%). These results indicated that DP-CAR was relatively safe. However, a high mortality rate with DP-CAR has been reported. A recent European multicenter cohort analysis showed a 16% mortality rate [23]. Nakamura et al. [12] reported a relatively high mortality rate of 5%. They also reported that severe gastropathy with stomach perforation occurred in 5 of 80 DP-CAR cases. Preoperative coil embolization of the CHA and LGA is reportedly useful for preventing ischemic complications in the liver and stomach [21, 24]. We also routinely performed CHA and LGA coil embolization, except in cases with a replaced HA. Coil embolization might have contributed to the relatively low incidence of ischemic complications in our series. However, several other reports did not support the usefulness of coil embolization [23]. Nakamura et al. also routinely performed preoperative coil embolization, but the incidence of ischemic complications and the mortality rate were relatively high [12]. The effectiveness of coil embolization should be examined in a future prospective study.
The high complication rate reported by Nakamura et al. may be attributed to extended resection. They performed en bloc excision of retroperitoneal tissue including the celiac plexus, bilateral ganglions, the total nerve plexus around the SMA, the left adrenal grand, and Gerota’s fascia to achieve microscopically curative resection (R0). Although this extended retroperitoneal resection resulted in a high R0 resection rate (92.5%), local recurrence was still seen in 14 of 80 DP-CAR cases. This indicates that extended resection has a limited role in local tumor eradication. Although we did not routinely perform extended resection, our data showed a favorable survival rate in patients who underwent DP-CAR. Accordingly, we think that extended resection is not necessary if curative resection is secured.
Meanwhile, it should be noted that 1 patient in our study who previously underwent distal gastrectomy died due to gastric perforation that led to severe sepsis. A reduced arterial supply to the remnant stomach might be the cause of this complication. In such cases, combined total gastrectomy may avoid the complication, as Yamamoto et al. suggested [8].
The MST with DP-CAR in this study was among the longest reported [11]. We think that this favorable survival outcome was mainly due to NAT in our series. Many recent reports showed the efficacy of NAT for BR or UR pancreatic cancer. However, only a few reports showed the efficacy and safety of NAT combined with DP-CAR. Nakamura et al. reported extremely good prognoses in 12 patients who underwent preoperative therapy and DP-CAR; the 5-year survival rate was 78.8% [12]. Baumgartner et al. also reported a retrospective analysis of 11 patients who underwent DP-CAR following NAT and showed a median estimated overall survival of 31 months from the time of original diagnosis [7]. The NAT group showed a higher R0 rate than the US group. This high R0 rate in the NAT group probably contributed to prolonged survival.
Unexpectedly, patients receiving GS NAT showed longer survival than those receiving GnP NAT. GS showed a high response rate (29.3%) in the GEST study, which compared gemcitabine, S-1, and GS for UR pancreatic cancer [25]. GnP also showed a high response rate (23%) in the MPACT study, which compared gemcitabine monotherapy and GnP for metastatic pancreatic cancer [26]. Because of these high response rates, we used these treatment regimens for NAT. It is worth mentioning that patients with GnP NAT showed higher hepatic recurrence rates than those with GS NAT. This may account for the shorter survival in the GnP group. However, due to the limited patient numbers and retrospective nature of this study, it is very hard to determine the reasons for shorter survival duration in the GnP group.
The main limitation of this study was its retrospective nature. The treatment policy changed during the study period. As a result, patients in each group were treated using different treatment policies and each group included a relatively small number of patients, making statistical analysis difficult. Moreover, this study did not include patients who were scheduled for but did not undergo surgical resection after NAT. Several patients in this study were referred to our institution after chemotherapy or chemoradiation therapy. This is one reason why we could not perform intent-to-treat analysis for all patients who were scheduled for DP-CAR at diagnosis. In addition, it was very difficult to determine inclusion criteria, especially in UR pancreatic cancer patients. UR cancer includes a wide variety of cases, ranging from those with cancer surrounding the CA with limited extent to cancer spreading to the aorta, adrenal gland, and retroperitoneal tissues. The former cases have a high likelihood of resectability, while the latter cases have very limited resectability, even after NAT. Prospective trials with precisely defined inclusion criteria are necessary to estimate the resection rates after NAT. A multi-institutional study will be needed to determine the effectiveness and limitations of combined DP-CAR and NAT, as each institution will have a limited number of cases.
Conclusion
In conclusion, DP-CAR was feasible and safe for patients with pancreatic body cancer contacting the CA and/or CHA. The combination of NAT and DP-CAR can provide a survival benefit for these patients. A prospective trial is needed to identify an adequate NAT regimen.
References
Tempero MA, et al. (2018) NCCN clinical practice guideline in oncology Pancreatic adenocarcinoma ver. 2.2018. https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed 6 Aug 2018
Appleby LH (1953) The coeliac axis in the expansion of the operation for gastric carcinoma. Cancer 6:704–707
Mayumi T, Nimura Y, Kamiya J, Kondo S, Nagino M, Kanai M, Miyachi M, Hamaguchi K, Hayakawa N (1997) Distal pancreatectomy with en bloc resection of the celiac artery for carcinoma of the body and tail of the pancreas. Int J Surg 22:15–21. https://doi.org/10.1007/BF02803900
Gagandeep S, Artinyan A, Jabbour N, Mateo R, Matsuoka L, Sher L, Genyk Y, Selby R (2006) Extended pancreatectomy with resection of the celiac axis: the modified Appleby operation. Am J Surg 192:330–335. https://doi.org/10.1016/j.amjsurg.2006.05.010
Hishinuma S, Ogata Y, Tomikawa M, Ozawa I (2007) Stomach-preserving distal pancreatectomy with combined resection of the celiac artery: radical procedure for locally advanced cancer of the pancreatic body. J Gastrointest Surg 11:743–749. https://doi.org/10.1007/s11605-007-0143-x
Hirano S, Kondo S, Hara T, Ambo Y, Tanaka E, Shichinohe T, Suzuki O, Hazama K (2007) Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long-term results. Ann Surg 246:46–51. https://doi.org/10.1097/01.sla.0000258608.52615.5a
Baumgartner JM, Krasinskas A, Daouadi M, Zureikat A, Marsh W, Lee K, Bartlett D, Moser AJ, Zeh HJ 3rd (2012) Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic adenocarcinoma following neoadjuvant therapy. J Gastrointest Surg 16:1152–1159. https://doi.org/10.1007/s11605-012-1839-0
Yamamoto Y, Sakamoto Y, Ban D, Shimada K, Esaki M, Nara S, Kosuge T (2012) Is celiac axis resection justified for T4 pancreatic body cancer? Surgery 151:61–69. https://doi.org/10.1016/j.surg.2011.06.030
Okada K, Kawai M, Tani M, Hirono S, Miyazawa M, Shimizu A, Kitahata Y, Yamaue H (2014) Preservation of the left gastric artery on the basis of anatomical features in patients undergoing distal pancreatectomy with celiac axis en-bloc resection (DP-CAR). World J Surg 38:2980–2985. https://doi.org/10.1007/s00268-014-2702-0
Gong H, Ma R, Gong J, Cai C, Song Z, Xu B (2016) Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic cancer: a systematic review and meta-analysis. Medicine (Baltimore) 95:e3061. https://doi.org/10.1097/MD.0000000000003061
Klompmaker S, de Rooij T, Korteweg JJ, van Dieren S, van Lienden KP, van Gulik TM, Busch OR, Besselink MG (2016) Systematic review of outcomes after distal pancreatectomy with coeliac axis resection for locally advanced pancreatic cancer. Br J Surg 103:941–949. https://doi.org/10.1002/bjs.10148
Nakamura T, Hirano S, Noji T, Asano T, Okamura K, Tsuchikawa T, Murakami S, Kurashima Y, Ebihara Y, Nakanishi Y, Tanaka K, Shichinohe T (2016) Distal pancreatectomy with en bloc celiac axis resection (modified Appleby procedure) for locally advanced pancreatic body CANCER: a single-center review of 80 consecutive patients. Ann Surg Oncol 23:969–975. https://doi.org/10.1245/s10434-016-5493-8
Bockhorn M, Uzunoglu FG, Adham M, Imrie C, Milicevic M, Sandberg AA, Asbun HJ, Bassi C, Büchler M, Charnley RM, Conlon K, Cruz LF, Dervenis C, Fingerhutt A, Friess H, Gouma DJ, Hartwig W, Lillemoe KD, Montorsi M, Neoptolemos JP, Shrikhande SV, Takaori K, Traverso W, Vashist YK, Vollmer C, Yeo CJ, Izbicki JR, International Study Group of Pancreatic S (2014) Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 155:977–988. https://doi.org/10.1016/j.surg.2014.02.001
Lutz MP, Zalcberg JR, Ducreux M, Aust D, Bruno MJ, Büchler MW, Delpero JR, Gloor B, Glynne-Jones R, Hartwig W, Huguet F, Laurent-Puig P, Lordick F, Maisonneuve P, Mayerle J, Martignoni M, Neoptolemos J, Rhim AD, Schmied BM, Seufferlein T, Werner J, van Laethem JL, Otto F (2017) 3rd St. Gallen EORTC Gastrointestinal Cancer Conference: consensus recommendations on controversial issues in the primary treatment of pancreatic cancer. Eur J Cancer 79:41–49. https://doi.org/10.1016/j.ejca.2017.03.022
Brierley JD, Gospodarowicz MK, Wittekind C (2016) The TNM classification of malignant tumours, 8th eddition edn. Wiley, Hoboken
Evans DB, Rich TA, Byrd DR, Cleary KR, Connelly JH, Levin B, Charnsangavej C, Fenoglio CJ, Ames FC (1992) Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas. Arch Surg 127:1335–1339. https://doi.org/10.1001/archsurg.1992.01420110083017
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Büchler M, International Study Group on Pancreatic S (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591. https://doi.org/10.1016/j.surg.2016.11.014
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768. https://doi.org/10.1016/j.surg.2007.05.005
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Kondo S, Katoh H, Shimizu T, Omi M, Hirano S, Ambo Y, Okushiba S, Morikawa T (2000) Preoperative embolization of the common hepatic artery in preparation for radical pancreatectomy for pancreas body cancer. Hepato-gastroenterology 47:1447–1449
Nakamura K, Yamaguchi T, Ishihara T, Sudo K, Kato H, Saisho H (2006) Phase II trial of oral S-1 combined with gemcitabine in metastatic pancreatic cancer. Br J Cancer 94:1575–1579. https://doi.org/10.1038/sj.bjc.6603168
Klompmaker S, van Hilst J, Gerritsen SL, Adham M, Teresa Albiol Quer M, Bassi C, Berrevoet F, Boggi U, Busch OR, Cesaretti M, Dalla Valle R, Darnis B, De Pastena M, Del Chiaro M, Grutzmann R, Diener MK, Dumitrascu T, Friess H, Ivanecz A, Karayiannakis A, Fusai GK, Labori KJ, Lombardo C, Lopez-Ben S, Mabrut JY, Niesen W, Pardo F, Perinel J, Popescu I, Roeyen G, Sauvanet A, Prasad R, Sturesson C, Lesurtel M, Kleeff J, Salvia R, Besselink MG, group EAD-Cs (2018) Outcomes after distal pancreatectomy with celiac axis resection for pancreatic cancer: a pan-European retrospective cohort study. Ann Surg Oncol 25:1440–1447. https://doi.org/10.1245/s10434-018-6391-z
Abo D, Hasegawa Y, Sakuhara Y, Terae S, Shimizu T, Tha KK, Tanaka E, Hirano S, Kondo S, Shirato H (2012) Feasibility of a dual microcatheter-dual interlocking detachable coil technique in preoperative embolization in preparation for distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer. J Hepatobiliary Pancreat Sci 19:431–437. https://doi.org/10.1007/s00534-011-0455-9
Ueno H, Ioka T, Ikeda M, Ohkawa S, Yanagimoto H, Boku N, Fukutomi A, Sugimori K, Baba H, Yamao K, Shimamura T, Sho M, Kitano M, Cheng AL, Mizumoto K, Chen JS, Furuse J, Funakoshi A, Hatori T, Yamaguchi T, Egawa S, Sato A, Ohashi Y, Okusaka T, Tanaka M (2013) Randomized phase III study of gemcitabine plus S-1, S-1 alone, or gemcitabine alone in patients with locally advanced and metastatic pancreatic cancer in Japan and Taiwan: GEST study. J Clin Oncol 31:1640–1648. https://doi.org/10.1200/JCO.2012.43.3680
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369:1691–1703. https://doi.org/10.1056/NEJMoa1304369
Acknowledgements
The authors thank the members of the Department of General Surgery, Chiba University Hospital, Chiba, Japan, for helping this study.
Funding
This research was partly supported by the Grant-in-Aid for scientific research (B:Grant No.: JP17H04287 and C: Grant No.: JP15K10180) of JSPS (Japan Society for the Promotion of Science) KAKENHI.
Author information
Authors and Affiliations
Contributions
Study conception and design: HY and MO; acquisition of data: HY, NS, SK, AU, and TT; analysis and interpretation of data: HY, KF, SK, and AK; drafting of the manuscript: HY and ST; critical revision of the manuscript: MM and MO.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoshitomi, H., Sakai, N., Kagawa, S. et al. Feasibility and safety of distal pancreatectomy with en bloc celiac axis resection (DP-CAR) combined with neoadjuvant therapy for borderline resectable and unresectable pancreatic body/tail cancer. Langenbecks Arch Surg 404, 451–458 (2019). https://doi.org/10.1007/s00423-019-01775-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01775-0